Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Glial Fibrillary Acidic Protein Levels in Post-Stroke Depression: A Prospective Ischemic Stroke Cohort
Authors Shan W, Zhao J, Qiu C, Xu G, Feng J
Received 11 August 2023
Accepted for publication 12 October 2023
Published 18 October 2023 Volume 2023:19 Pages 2171—2178
DOI https://doi.org/10.2147/NDT.S435006
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Richard J Porter
Wanying Shan,1,* Jie Zhao,2,* Chunfang Qiu,1 Guoli Xu,1 Jie Feng1
1Department of Neurology, Suzhou Ninth People’s Hospital, Soochow University, Suzhou, Jiangsu, 215200, People’s Republic of China; 2Department of Gerontology, Suzhou Ninth People’s Hospital, Soochow University, Suzhou, Jiangsu, 215200, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jie Feng, Department of Neurology, Suzhou Ninth People’s Hospital, Soochow University, No. 2666 Ludang Road, Suzhou, Jiangsu, 215200, People’s Republic of China, Tel/Fax +86 051282881332, Email [email protected]
Background and Purpose: Increased glial fibrillary acidic protein (GFAP) levels were found in cerebrovascular disease patients. The pathogenesis of depression after ischemic stroke remains largely unknown. Here, we aim to determine whether GFAP concentrations were associated with post-stroke depression (PSD) at 3 months.
Methods: From March 2022 to September 2022, patients with first-ever ischemic stroke were prospectively recruited. GFAP concentrations were detected within 24 h using an enzyme-linked immunosorbent assay. The PSD was defined as a Hamilton Depression Rating Scale 24-Item score ≥ 8.
Results: A total of 206 subjects with ischemic stroke (mean age: 63.6 years; 49.0% female) were enrolled. During the 90-day follow-up, 57 participants (27.7%) were observed in PSD. The median serum GFAP concentrations were 0.67 ng/mL. After adjustment for the covariates, higher increased GFAP levels were associated with increased risk of PSD (odds ratio [OR], 7.12; 95% confidence interval [CI], 3.29– 15.44; P < 0.001). Also, the multivariate-adjusted OR of PSD associated with the fourth quartile of GFAP was 10.89 (95% CI, 3.53– 33.60; P < 0.001) compared with the first quartile. Furthermore, the restricted cubic spline confirmed a linear association between GFAP and the risk of PSD (P for linearity < 0.001).
Conclusion: Our results indicated that increased circulating GFAP concentrations were significantly correlated with the risk of PSD at 3 months. Measuring the GFAP levels after ischemic stroke may add some values for the risk stratifying of PSD.
Keywords: post-stroke depression, ischemic stroke, prognosis, glial fibrillary acidic protein, prospective study
Introduction
Stroke is estimated to be the leading cause of acquired disability and mortality worldwide.1 Post-stroke depression (PSD) is a common complication that affects approximately one-third of ischemic stroke survivors.2–4 PSD may negatively affect the quality of life after ischemic stroke, and impair recovery of cognitive and motor function.5,6 Also, a meta-analysis included 15 prospective cohort studies with 250,294 participants suggesting that PSD is significantly correlated with an increased risk of mortality in ischemic stroke patients.7 Therefore, it is essential to identify the predictor and specific pathophysiology of PSD, in order to stratify the PSD risk and improve stroke prognosis.
Glial Fibrillary Acidic Protein (GFAP) is a cytoskeletal protein with a 50–52 KDa molecular mainly secreted by the astrocytes.8,9 It plays an important role in the mediating shape and motility of astrocytic processes and contributes to blood-brain barrier (BBB) integrity and white matter architecture.10,11 When astrocytes and the BBB are broken down, GFAP molecules may release into the blood and become detectable Elevated GFAP levels in peripheral blood and cerebrospinal fluid have been found in several central nervous system diseases.12–14 It has been reported that Alzheimer’s disease dementia patients with increased GFAP levels show worse cognitive function.15 Also, significant correlations were found between infarction size, stroke severity, and serum GFAP concentrations in ischemic stroke patients.16 However, the correlation between circulating GFAP concentrations and depressive symptoms after ischemic stroke is still unclear.
We therefore prospectively recruited the ischemic stroke patients and evaluated whether the serum GFAP levels were correlated with the risk of 3-month PSD.
Materials and Methods
Study Patients and Design
Between March 2022 to September 2022, the first-ever ischemic stroke subjects with symptoms onset to hospitalization less than 7 days were consecutively enrolled at Suzhou Ninth People’s Hospital. Ischemic stroke was confirmed by the World Health Organization criteria combined with brain computed tomography or magnetic resonance imaging results.17 The exclusion standards were: 1) age less than 18 years; 2) unable to complete the psychological measurement; 3) had a history of psychiatric illness, Alzheimer’s disease, Parkinson’s disease, traumatic brain injury, central nervous system infection, hematological or immunological diseases, thyroid diseases, malignant tumor, and serious organ dysfunction. This study was approved by the Ethics Committee of Suzhou Ninth People’s Hospital. Written consent was obtained from all participants before entering this study. All the participants were informed about the purpose of the study. All procedures were in accordance with the 1964 Helsinki Declaration and its later amendments.
Baseline Data Collection
Baseline variables were recorded after admission, including demographic characteristics (age, gender, and educational background), traditional risk factors (hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, and smoking), clinical data (blood pressure, neurological deficits, side of infarction, and stroke subtypes) and laboratory data (total cholesterol, triglyceride, baseline glucose levels, and Hyper-sensitive C-reactive protein). Baseline neurological deficits were measured using the National Institutes of Health Stroke Scale (NIHSS).18 Stroke subtypes were classified as large artery atherosclerosis, small artery occlusion, cardioembolism, and others according to the Trial of Org 10,172 in Acute Stroke Treatment (TOAST).19
Measurements of GFAP Levels
Blood samples in all patients were collected within 24 hours after admission by trained nurses and tested by technicians who were blinded to clinical data. The blood was centrifuged, aliquoted, and kept at –80°C for later analysis. Serum GFAP concentrations were detected by an enzyme-linked immunosorbent assay kit.
Psychological Measurement
During the 3-month follow-up, the psychological measurement was performed using the validated version of the 24-item Hamilton Depression Rating Scale (HRSD-24).20 According to previous studies, PSD was defined as a Hamilton Depression Rating Scale 24-Item score ≥ 8.21–23
Statistical Analysis
The continuous variables were expressed as means ± standard deviation (SD) or medians with interquartile ranges (IQR). Univariate analysis for continuous variables was conducted using the Student’s t-test or Mann–Whitney U-test. Categorical variables were shown as percentages and compared using the Fisher exact test or χ2 test. Binary logistic regression analysis was performed to estimate the odds ratios (OR) and 95% confidence intervals (CI). Multivariate analyses were first controlled for demographic characteristics and educational status (Model 1) and additionally controlled for all variables (including demographic characteristics, educational status, and P value < 0.1 in the univariate analysis).
Additionally, we utilized the restricted cubic splines to estimate and explore the shape of the correlation between GFAP levels and PSD, with 3 knots placed at the 5th, 50th, and 95th percentiles of GFAP, and the reference point was the median GFAP levels (0.67 ng/mL) among all patients. Furthermore, we used the receiver operating characteristic curve (ROC) to assess the overall predicted accuracy of GFAP. All statistical analyses were conducted with SPSS (version 24.0, SPSS Inc., Chicago, IL, USA) and R statistical software (version 4.0.0, R Foundation, Vienna, Austria). All analyses were two-tailed, and statistical significance was determined by P < 0.05.
Results
Baseline Data
In this study, 294 patients with ischemic stroke were screened for analysis. We excluded 62 patients unable to complete the psychological measurement, 19 patients previously diagnosed with psychiatric illness, Alzheimer’s disease, Parkinson’s disease, traumatic brain injury, central nervous system infection, hematological or immunological diseases, thyroid diseases, malignant tumor, and serious organ dysfunction, and 7 patients lost to follow-up. Finally, a total of 206 patients were finally included in the study. The average age was 63.6 years and 101 (49.0%) were male. Further details of baseline data are presented in Table 1. The median circulating GFAP concentrations were 0.67 ng/mL. According to the median GFAP levels, patients were divided into the higher GFAP levels group and the lower GFAP levels group. As shown in Table 1, as compared with patients with lower GFAP levels, those with higher GFAP levels had a higher prevalence of diabetes mellitus (P = 0.017) and PSD (P < 0.001) and had a higher Hs-CRP levels (P = 0.049). However, there was no significant difference between the 2 groups in terms of age, sex, baseline NIHSS score, and stroke etiology.
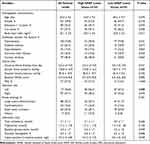 |
Table 1 Baseline Data of the Ischemic Stroke Patients According to the GFAP Levels |
Comparison of Baseline Data in Patients with or Without PSD
At the 3-month follow-up, PSD was observed in 57 patients (27.7%). The comparison of baseline data is shown in Table 2. The GFAP concentrations in subjects with PSD were higher than those in patients without PSD (median, 0.92 ng/mL versus. 0.48 ng/mL; P = 0.001). In addition, compared with patients without PSD, those with it were older (66.0 ± 9.9 versus. 62.7 ± 8.7 years, P = 0.018), more likely to live alone (40.4% versus. 22.8%, P = 0.012), and have education <12 years (68.4% versus. 52.3%, P = 0.037) and diabetes mellitus (36.8% versus. 21.5%, P = 0.024), and have a higher NIHSS score (median, 5.0 versus. 4.0, P = 0.011), glucose levels (5.9 ± 2.2 mmol/L versus. 5.3 ± 1.5 mmol/L, P = 0.041) and Hs-CRP levels (median, 6.0 mg/L versus. 4.0 mg/L; P = 0.046).
 |
Table 2 Clinical and Sociodemographic Characteristics of Patients Stratified by PSD at 3 Months |
Association GFAP Levels and PSD
The cut-off values of the GFAP levels in the 4 quartiles were: (first quartile) < 0.23 ng/mL, (second quartile) 0.23–0.66 ng/mL, (third quartile) 0.67–1.00 ng/mL and (fourth quartile) >1.00 ng/mL. Patients in the fourth quartile of GFAP had the highest incidence of PSD (49.1%; P < 0.002). After adjustment for potential confounders (including age, sex, education, and P value < 0.1 in the univariate analysis) in multivariate regression analysis, the OR of PSD associated with the fourth quartile of GFAP levels was 10.89 (compared with the first quartile; 95% CI, 3.53–33.60; P< 0.006; Table 3). In continuous analysis, higher GFAP levels were confirmed to have an increased risk of PSD (OR, 7.12; 95% CI, 3.29–15.44; P < 0.001). Furthermore, the results of restricted cubic spline regression analysis demonstrated that there was a linear relationship between GFAP levels and PSD (P < 0.001; Figure 1) after adjustment for the covariates. In addition, the AUC of GFAP in predicting the presence of PSD was 0.735 (95% CI, 0.657–0.812, P = 0.001). The optimal cutoff point of circulating GFAP levels was 0.45 ng/mL, with a sensitivity of 87.7% and a specificity of 51.7%.
 |
Table 3 Multivariate Analysis for the Relationship Between GFAP Levels and PSD |
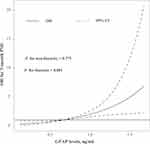 |
Figure 1 Association of serum GFAP levels with risk of post-stroke depression. Odds ratios and 95% confidence intervals derived from restricted cubic spline regression, with knots placed at the 5th, 50th, and 95th percentiles of GFAP. Odds ratios were controlled for the same variables as model 2 in Table 3. |
Discussion
This is the first prospective study to evaluate the predictive value of serum GFAP levels in 3-month PSD in ischemic stroke patients. The results found that even after controlling for demographic characteristics, stroke severity, and other potential confounders, patients with increased GFAP concentrations have a higher risk of PSD.
PSD is the most frequent and burdensome neuropsychiatric complication after ischemic stroke.24 This discrepancy in the prevalence of PSD occurs because studies were performed in different settings, instruments assessing PSD, and the distinct time intervals between the PSD assessments and stroke symptoms onset. In this study, we found that 27.7% of ischemic stroke patients experience PSD at 90 days follow-up, which is similar to previous literature.2–4 We found that age and educational background were predictors of PSD. Older patients with low educational status were more likely to have a depressive response when dealing with the stress of stroke, possibly due to a lack of sufficient social security.25 The significant correlation between stroke severity and PSD was also consistent with earlier studies.26,27 Due to the pathophysiology, prognosis, and clinical features of subcortical lacunar strokes being different from other acute cerebrovascular diseases,28 some researchers might suppose that lacunar stroke is associated with the risk of PSD. However, our data did not confirm a significant correlation between stroke subtypes and PSD. Further studies are recommended to detect this association.
GFAP is a monomeric intermediate filament protein of the astroglia skeleton, which is considered brain-specific.8 GFAP is involved in several cellular processes in astrocytes, such as vesicle trafficking, neuron-astrocyte interactions, and blood-brain barrier integrity.29 The GFAP molecules will be released into circulation through the damaged BBB in several central nervous system diseases. Circulating GFAP has recently been indicated as a promising biomarker for disease diagnosis.12–14 Our data further extended the predictive value of GFAP in cerebrovascular diseases and showed that patients with increased serum GFAP levels have a higher PSD risk at 3 months after ischemic stroke.
PSD is a heterogeneous condition, and no individual pathophysiological processes can fully explain PSD. Recently, some processes have been confirmed to induce PSD including neuroinflammation, glutamate-mediated excitotoxicity, and abnormal neurotrophic response to stroke.2,24 The precise mechanisms underlying the observed relationship between serum GFAP and PSD are unknown, but several pathophysiological processes may explain the association. Firstly, reactive astrocytes after central nervous system injury may induce the expression of GFAP and the release of several pro-inflammatory cytokines. Also, reactive astrocytes increase the excitotoxicity of glutamate to neurons and other brain cells by regulating the extracellular glutamate.30,31 We, therefore, assume that GFAP may mediate the depressive symptoms after ischemic stroke by inducing neuroinflammation and glutamate excitotoxicity. Secondly, GFAP−/− mice display abnormalities of the BBB and endothelial function.11 As the BBB plays a pivotal role in the pathogenesis of depression, GFAP is involved in the presence of PSD by mediating the integrity of the BBB. Thirdly, GFAP has also been reported to be correlated with small cerebral vessel disease, including lacunar infarction and white matter hyperintensity burden,15 which might induce neuropsychological alterations.32 Further basic experiments are needed to clarify the detailed mechanism of GFAP on depression after ischemic stroke.
The strengths of our study include prospective design, comprehensive assessment of PSD, and recruiting a homogeneous population of ischemic stroke patients. However, this study had some inevitable limitations. Firstly, this study was based on Asian ethnicity patients, it cannot be generalized to other populations. Secondly, GFAP levels were tested once at a time after admission. We therefore could not assess the correlation between GFAP changes and PSD. Thirdly, ischemic stroke patients with severe neurological deficits, a history of psychiatric illness, and other serious illnesses were excluded, which might underestimate the incidence of PSD. Finally, several potential confounders were not recorded in this study, such as home care, medication compliance, and use of sedative and hypnotic drugs post-discharge. Therefore, these results should be interpreted with caution.
In conclusion, increased GFAP levels were associated with a significant augmentation of the proportion of patients with 3-month PSD after stroke. The results of the present report suggested that circulating GFAP levels could be a promising biomarker for PSD risk stratification. Further studies using more representative nationwide-based samples are needed to confirm our findings. Furthermore, whether the management of GFAP within the appropriate range could improve functional outcome after ischemic stroke is a possible future area of inquiry.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Johnson CO, Nguyen M, Roth GA. Collaborators. GS. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(5):439–458. doi:10.1016/S1474-4422(19)30034-1
2. Robinson R, Jorge R. Post-stroke depression: a review. Am J Psychiatry. 2016;173(3):
3. Towfighi A, Ovbiagele B, El Husseini N, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(2):e30–e43. doi:10.1161/STR.0000000000000113
4. Schöttke H, Giabbiconi C. Post-stroke depression and post-stroke anxiety: prevalence and predictors. Int Psychogeriatr. 2015;27(11):1805–1812. doi:10.1017/S1041610215000988
5. Parikh R, Robinson R, Lipsey J, Starkstein S, Fedoroff J, Price T. The impact of poststroke depression on recovery in activities of daily living over a 2-year follow-up. Arch Neurol. 1990;47(7):785–789. doi:10.1001/archneur.1990.00530070083014
6. Chemerinski E, Robinson R, Kosier J. Improved recovery in activities of daily living associated with remission of poststroke depression. Stroke. 2001;32(1):113–117. doi:10.1161/01.STR.32.1.113
7. Cai W, Mueller C, Li Y, Shen W, Stewart R. Post stroke depression and risk of stroke recurrence and mortality: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:102–109. doi:10.1016/j.arr.2019.01.013
8. Yang Z, Wang K. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci. 2015;38(6):364–374. doi:10.1016/j.tins.2015.04.003
9. Middeldorp J, Hol E. GFAP in health and disease. Prog Neurobiol. 2011;93(3):421–443. doi:10.1016/j.pneurobio.2011.01.005
10. Gomi H, Yokoyama T, Itohara S. Role of GFAP in morphological retention and distribution of reactive astrocytes induced by scrapie encephalopathy in mice. Brain Res. 2010;1312:156–167. doi:10.1016/j.brainres.2009.11.025
11. Pekny M, Stanness K, Eliasson C, Betsholtz C, Janigro D. Impaired induction of blood-brain barrier properties in aortic endothelial cells by astrocytes from GFAP-deficient mice. Glia. 1998;22(4):390–400. doi:10.1002/(SICI)1098-1136(199804)22:4<390::AID-GLIA8>3.0.CO;2-7
12. Wunderlich M, Wallesch C, Goertler M. Release of glial fibrillary acidic protein is related to the neurovascular status in acute ischemic stroke. Eur J Neurol. 2006;13(10):1118–1123. doi:10.1111/j.1468-1331.2006.01435.x
13. Katsanos A, Makris K, Stefani D, et al. Plasma glial fibrillary acidic protein in the differential diagnosis of intracerebral hemorrhage. Stroke. 2017;48(9):2586–2588. doi:10.1161/STROKEAHA.117.018409
14. Amalia L. Glial Fibrillary Acidic Protein (GFAP): neuroinflammation biomarker in acute ischemic stroke. J Inflamm Res. 2021;14:7501–7506. doi:10.2147/JIR.S342097
15. Elahi FM, Casaletto KB, La Joie R, et al. Plasma biomarkers of astrocytic and neuronal dysfunction in early- and late-onset Alzheimer’s disease. Alzheimers Dement. 2020;16(4):681–695. doi:10.1016/j.jalz.2019.09.004
16. Herrmann M, Vos P, Wunderlich M, Lamers K. Release of glial tissue-specific proteins after acute stroke: a comparative analysis of serum concentrations of protein S-100B and glial fibrillary acidic protein. Stroke. 2000;31(11):2670–2677. doi:10.1161/01.STR.31.11.2670
17. Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke. 1989;20(10):1407–1431. doi:10.1161/01.STR.20.10.1407
18. Brott T, Adams HJ, Olinger C, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–870. doi:10.1161/01.STR.20.7.864
19. Adams HJ, Bendixen B, Kappelle L, Biller J, Love B, Gordon D. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi:10.1161/01.STR.24.1.35
20. Zimmerman M, Martinez J, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton depression rating scale. J Affect Disord. 2013;150(2):384–388. doi:10.1016/j.jad.2013.04.028
21. Wang G, Zhou Y, Bu X, et al. Antiphospholipid antibodies predict post-stroke depression after acute ischemic stroke. J Affect Disord. 2019;257:160–165. doi:10.1016/j.jad.2019.07.013
22. Chen Y, Qu J, Xiao W, et al. Intracranial atherosclerosis and poststroke depression in Chinese patients with ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25(4):998–1004. doi:10.1016/j.jstrokecerebrovasdis.2015.12.038
23. Zhu Z, Guo D, Shi M, et al. Effect of immediate blood pressure reduction on post-stroke depression in ischemic stroke patients: a substudy of CATIS trial. J Affect Disord. 2022;300:195–202. doi:10.1016/j.jad.2021.12.120
24. Medeiros G, Roy D, Kontos N, Beach S. Post-stroke depression: a 2020 updated review. Gen Hosp Psychiatry. 2020;66:70–80. doi:10.1016/j.genhosppsych.2020.06.011
25. De Ryck A, Brouns R, Geurden M, Elseviers M, De Deyn PP, Engelborghs S. Risk factors for poststroke depression: identification of inconsistencies based on a systematic review. J Geriatr Psychiatry Neurol. 2014;27(3):147–158. doi:10.1177/0891988714527514
26. Zhang Y, Cheng L, Chen Y, Yang G, Liu J, Zeng L. Clinical predictor and circulating microRNA profile expression in patients with early onset post-stroke depression. J Affect Disord. 2016;193:51–58. doi:10.1016/j.jad.2015.12.061
27. Chi C, Huang Y, Ye S, et al. Interleukin-10 level is associated with post-stroke depression in acute ischaemic stroke patients. J Affect Disord. 2021;293:254–260. doi:10.1016/j.jad.2021.06.037
28. Rudilosso S, Rodríguez-Vázquez A, Urra X, Arboix A. The potential impact of neuroimaging and translational research on the clinical management of lacunar stroke. Int J Mol Sci. 2022;23(3):1497. doi:10.3390/ijms23031497
29. Garwood C, Ratcliffe L, Simpson J, Heath P, Ince P, Wharton S. Review: astrocytes in Alzheimer’s disease and other age-associated dementias: a supporting player with a central role. Neuropathol Appl Neurobiol. 2017;43(3):281–298. doi:10.1111/nan.12338
30. Oppenheim R, Houenou L, Parsadanian A, Prevette D, Snider W, Shen L. Glial cell line-derived neurotrophic factor and developing mammalian motoneurons: regulation of programmed cell death among motoneuron subtypes. J Neurosci. 2000;20(13):5001–5011. doi:10.1523/JNEUROSCI.20-13-05001.2000
31. Struzyńska L. A glutamatergic component of lead toxicity in adult brain: the role of astrocytic glutamate transporters. Neurochem Int. 2009;55(1–3):151–156. doi:10.1016/j.neuint.2009.01.025
32. Blanco-Rojas L, Arboix A, Canovas D, Grau-Olivares M, Oliva Morera JC, Parra O. Cognitive profile in patients with a first-ever lacunar infarct with and without silent lacunes: a comparative study. BMC Neurol. 2013;13(1):203. doi:10.1186/1471-2377-13-203
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
