Back to Journals » Open Access Emergency Medicine » Volume 15
Geographical Association Between Basic Life Support Courses and Bystander Cardiopulmonary Resuscitation and Survival from OHCA in Denmark
Authors Jensen TW, Ersbøll AK, Folke F, Andersen MP , Blomberg SN, Holgersen MG, Andersen LB, Lippert F , Torp-Pedersen C , Christensen HC
Received 21 February 2023
Accepted for publication 20 May 2023
Published 15 June 2023 Volume 2023:15 Pages 241—252
DOI https://doi.org/10.2147/OAEM.S405397
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Theo Walther Jensen,1– 3 Annette Kjær Ersbøll,3,4 Fredrik Folke,2,3,5 Mikkel Porsborg Andersen,6 Stig Nikolaj Blomberg,1– 3 Mathias Geldermann Holgersen,2,7 Lars Bredevang Andersen,1 Freddy Lippert,2,3 Christian Torp-Pedersen,6,8 Helle Collatz Christensen1,2,9
1Emergency Medical Services Region Zealand, Naestved, Denmark; 2Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark; 3Copenhagen Emergency Medical Services, University of Copenhagen, Copenhagen, Denmark; 4National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark; 5Department of Cardiology, Herlev Gentofte University Hospital, Gentofte, Denmark; 6Department of Cardiology, Nordsjaellands Hospital, Hilleroed, Denmark; 7Paediatric Pulmonary Service, Department of Paediatrics and Adolescent Medicine, Copenhagen University Hospital, Copenhagen, Denmark; 8Aalborg University Hospital, Aalborg & Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark; 9Danish Clinical Quality Program (RKKP), National Clinical Registries & Department of Clinical Medicine, Copenhagen, Denmark
Correspondence: Theo Walther Jensen, Emergency Medical Services, Region Zealand and University of Copenhagen, Ringstedgade 61, 13. etage, Naestved, 4700, Denmark, Tel +45 51 21 10 06, Email [email protected]
Introduction: Annually, approximately 4% of the entire adult population of Denmark participate in certified basic life support (BLS) courses. It is still unknown whether increases in BLS course participation in a geographical area increase bystander cardiopulmonary resuscitation (CPR) or survival from out-of-hospital cardiac arrest (OHCA). The aim of the study was to examine the geographical association between BLS course participation, bystander CPR, and 30-day survival from OHCA.
Methods: This nationwide register-based cohort study includes all OHCAs from the Danish Cardiac Arrest Register. Data concerning BLS course participation were supplied by the major Danish BLS course providers. A total of 704,234 individuals with BLS course certificates and 15,097 OHCA were included from the period 2016– 2019. Associations were examined using logistic regression and Bayesian conditional autoregressive analyses conducted at municipality level.
Results: A 5% increase in BLS course certificates at municipality level was significantly associated with an increased likelihood of bystander CPR prior to ambulance arrival with an adjusted odds ratio (OR) of 1.34 (credible intervals: 1.02;1.76). The same trends were observed for OHCAs in out-of-office hours (4pm-08am) with a significant OR of 1.43 (credible intervals: 1.09;1.89). Local clusters with low rate of BLS course participation and bystander CPR were identified.
Conclusion: This study found a positive effect of mass education in BLS on bystander CPR rates. Even a 5% increase in BLS course participation at municipal level significantly increased the likelihood of bystander CPR. The effect was even more profound in out-of-office hours with an increase in bystander CPR rate at OHCA.
Keywords: basic life support, survival, geography, epidemiology, conditional autoregressive regression
Background
Cardiac arrest is a common cause of sudden death in Europe, with an annual incidence of out-of-hospital cardiac arrest (OHCA) at 67–170 per 100,000 inhabitants.1–3 OHCA is a condition with a poor prognosis, with survival to discharge from hospital, in Europe around 8%.4 There are approximately 5000 cases of OHCA in Denmark annually. There has been a significant increase in survival after OHCA in Denmark in the last two decades. The 30-day survival rate after a hospital discharge increased from around 4% in 2001 to 16% in 2018.5,6 This is partly due to a significant increase in bystander cardiopulmonary resuscitation (CPR) prior to the arrival of emergency medical services (EMS) personnel.7–9 Similar trends have been seen in other countries demonstrating a clear positive relation between bystander CPR prior to arrival of EMS and survival.9–11
From 2001, the bystander CPR rate increased from 20% to 77% in 20185,6,12 in Denmark. This increase in bystander CPR rate might be due to several central initiatives targeted at engaging more laypersons. CPR courses have been made mandatory in all primary schools since January 2005 and when taking driver’s license since October 2006.6,12 The annual BLS course participation rate in Denmark is 3.6% of all adults. Since the implementation of mandatory BLS course participation for acquiring driver’s license was fully implemented (in 2009) more than 44% of the entire Danish adult population has attended BLS courses. Most BLS courses (>97%) are provided by one of the organizations of the Danish First Aid Council.13 The providers aim to follow the ERC guidelines for recognizing the OHCA alerting EMS, providing CPR, and using an AED (automatic external defibrillator).14,15 It is a supported assumption that those educated in BLS are more willing to act and to provide CPR in cases of OHCA.16–19 Meta studies indicate an increase in survival following the implementation of large-scale BLS education.16,20 A recent study from Denmark found a positive association between BLS course participation rate and 30-day survival from OHCA rate per 100,000 inhabitants. In addition, the effect of BLS course participation rate on 30-day survival was mediated by the bystander CPR rate. However, BLS course participation rate is not evenly distributed geographically. Hence, it is expected that some geographical areas benefit more and less from national efforts in mass education BLS.
A recent French study examined regional differences in BLS education and survival from OHCA. The study showed a positive association between BLS education and survival, though there was substantial variation.21 In recent years, there has generally been a large improvement in geodata availability and increasing accessibility of geospatial modelling. Analysis of geographical data has recently been utilized in similar fields to compare AED location and rurality’s effect in survival via the Danish Cardiac Arrest register.22–24 Having long-term whole-population annual BLS training rates can contribute to fill-out this knowledge gap by answering questions about geographical association at a national level. To explore the geographical association between mass education in BLS and survival, geospatial regression analysis can be used.
The aim of this study was to analyze the association between BLS course participation and bystander CPR rate and 30-day survival at municipality level. Second, we aim to identify geographical clusters with low frequency of BLS education and low level of bystander CPR.
Methods
This is a municipal level register-based cohort study comprising all OHCA in Denmark between January 1 2016 and December 31 2019.
Setting
Denmark has a population of approximately 5.85 million.25 Health care is free of charge and is publicly funded by taxation. The Danish administration and health-care system is managed by the central government, regional administrations, and the municipalities. There are 98 municipalities with varying geographical size, population, and socio-economic conditions and cover 42,933 km2. There are approximately 400.000 immigrants,26 these are included in municipal data and are included in the current study.
Data
OHCA Data
The study population included all verified OHCA in the Danish Cardiac Arrest Register in the period between January 1 2016 and December 31 2019.27 Characteristics of each OHCA included geolocation, bystander-initiated CPR, and survival. OHCAs were assigned to the municipality where the event took place. OHCAs occurring at locations with health-care staff present (ie nursing homes, handicap and dementia facilities, hospices, doctors’ offices, staffed elderly homes, etc.) were identified by manual examination and excluded.
BLS Education Data
All data concerning BLS education were derived from the Danish First Aid Council Digital database on course certificates from early 2016 to early December 31 2019 and from the Danish Heart Foundation “Give Life” campaign. All certificates include data on the time of issuing, personal identification number, and certificate type. Each individual certificate holder was included with the first certificate, despite the potential for several certificates per person. The number of individuals has been verified in a previous study.13 The current address of each certificate holder was identified in the Danish Civil Registration System and linked with the relevant municipality at Statistics Denmark. Data regarding BLS certificates were assigned to the municipality were the persons have their residence. Participation rates per municipality were based on 2019 population size.
Municipality Level Data
Municipal data on population mean disposable income, educational level, age, and several additional variables were publicly available in Denmark through Statistics Denmark.28 The analysis in this study requires all geographical units (the municipalities) to have a clearly specified connecting unit ie a neighboring unit with borders. However, Denmark consists of a number of islands and some of these islands are not naturally connected with borders. Hence, the mathematical connections among municipalities [whether they were considered neighbors] was manually corrected so islands were connected to closest land-based municipality.
Statistical Analysis and Models
Exposure, Outcomes, and Confounders
The exposure variable was the proportion of the municipal population attending BLS courses (proportion 0–1). There are two models with two different outcome measures. In model 1 the outcome measure is the proportion of OHCAs with 30-day survival. In model 2 the outcome measure is the proportion of OHCAs with bystander CPR. Exposure and outcomes were aggregated annually at municipality level. The models were based on the most relevant meta-analysis.29 Directed acyclic graphs (DAGs) were used to illustrate the relationship between the included variables (Supplementary Materials). Model 1 was adjusted for mean age in the municipality, mean disposable income per person in the municipality, mean municipal Charlson Comorbidity Index (CCI) (0–24) and initial rhythm at OHCA [shockable or non-shockable] (see Supplementary Materials). Model 2 was adjusted for mean age in the municipality, mean disposable income per person in the municipality and mean response time for EMS arrival at OHCA (minutes) (see Supplementary Materials). The difference in models is based on the difference in outcome measure, ie initial rhythm measured by EMS is less relevant in model 2 as bystanders CPR will have been initiated prior to EMS measuring cardiac rhythms with an electrocardiogram.
Non-Spatial Regression
Initially, a descriptive analysis was performed of the distribution of incidence proportions for key indicators of exposure and outcome measures such as overall OHCA, bystander CPR prior to arrival of EMS, 30-day survival from OHCA and BLS course participation rate. Municipal level non-spatial association between BLS course participation rate and the two outcomes was analyzed in a logistic regression model. Results are presented as odds ratios (OR) and 95% confidence intervals (95% CI) for an increase in the outcome, following a 5% municipal increase in the proportion of the population with a course certificate. Subgroup analysis was conducted stratified by the location of OHCA in public locations and on all OHCAs in out-of-office hours (4.00pm-08.00am). Quantitative confounding variables were inspected for linearity in the models (parameter estimates of a categorized version of each variable should indicate linearity). If the assumption about linearity was not fulfilled, the variable was transformed to a categorical variable. Models were inspected for dispersion, and the dispersion parameters are displayed. Over dispersion was considered, when the residual deviance divided by the degrees of freedom was above 1.5. If models were under or over dispersed, the model was adjusted by applying quasi binomial distribution presumptions to the modeling. Logistic regression was conducted using the package GLM with a logit link in R.
Geo-Spatial Illustrations and Cluster Analysis
Geo-spatial cluster analysis and illustrations were guided by a similar analysis conducted in a different study.30 The Global and the Local Moran’s Index was used to identify and illustrate spatial clustering.31 Neighboring spatial units (municipalities) can correlate leaving data to present in clusters or areas with similar values, complicating the possibility for meaningful analysis of association. The global Moran’s I was used to test whether variables in geospatial neighboring units were correlated. The values can vary between +1 and −1 indicating the strength of the autocorrelation with a value of 0 indicating no correlation. Positive values indicate a positive correlation between neighboring unit higher than expected by chance.31 The local Moran’s I show the individual geographical clusters and was used to visualize clusters by making a local indicator of spatial association (LISA) map.31 The LISA map indicates “hot spots” (red) and “cold spots” (blue) of local geographical correlation in incidence proportions. Using Moran’s I requires making a choice about neighborhood topology, that is how “far” units (municipalities) should be to be considered “neighboring.” This is labelled spatial weights matrix (wij).31 Like other studies, the row-standardized spatial weights matrix (wij) was calculated with a distance band of 200 km.30,31 A two-sided p-value <0.05 was considered statistically significant. A package of spatial analytical tool in R statistical software calculates both global and local Moran’s I and corresponding Z-values.32
Geo-Spatial Regression
Spatial data were included from the period between January 1 2016 and December 31 2019. Neighboring spatial units tend to have similar values that often violate the assumption of independence common in many regression models. Standard logistic regression needed to be supplemented with analysis that overcomes this. A Bayesian spatial conditional autoregressive (CAR) analysis was conducted to evaluate the significance of the spatial autocorrelation between neighboring municipalities.33 The CAR analysis uses the presumed associations as other models while adjusting for spatial similarities. Bayesian modelling creates estimates for each individual variable by using information from other variables in the model.33 Like similar analysis of Danish municipalities, the CAR model suggested by Leroux was used.30 The weights matrix used in the Morans Index analysis was used in the CAR model as well. CAR analyses were conducted with the CARBayes package in R.34 Results are presented as odds ratios (OR) and 95% confidence intervals (95% CI) for an increase in the outcome following a 5% municipal increase in the proportion of the population with a course certificate. Subgroup analysis was conducted stratified by the location of OHCA in public locations and on all OHCAs in out-of-office hours (4.00pm-08.00am).
Data Storage and Ethics
In Denmark, no ethical approval is required for the analysis of aggregated data from official registers as in the current study. The study is approved by the data responsible institute, the regional data protection agency (Approval number: P-2020-259) in accordance with the General Data Protection Regulation (GDPR).
Results
In the period between January 1 2016 and December 31 2019 704,234 individuals with BLS course certificates and 15,097 OHCA were included (Table 1). Figure 1 shows a modified CONSORT diagram presenting inclusion and exclusions of EMS witnessed OHCAs, health care staffed cases, and duplicates. The subgroup population on out-of-office hours included 7449 OHCAs with 7648 exclusions and the subgroup population on in OHCA’s public places included 3375 OHCA with 11,722 excluded cases (Figure 1).
 |
Table 1 Summary Statistics of Out-of-Hospital Cardiac Arrest and Basic Life Support Course Participation in Denmark, from 2016 to 2019 |
 |
Figure 1 Modified Consort Flow Diagram. Notes: *Daytime – working hours is defined as 08.00–16.00. Night-time – out of offices hours is defined as 16.00–08.00. CONSORT figure adapted from Falci SGM, Marques LS. CONSORT: when and how to use it. Dental Press J. Orthod. 2015;20(3):13-15. Copyright: © 2015 Falci and Marques. Creative Commons Attribution License.35 |
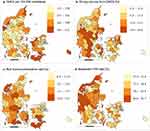
Municipal Incidence Proportions
Figure 2 shows incidence proportions between 2016 and 2019 of; OHCA per 100,000 inhabitants; 30-day survival from OHCA; BLS course participation rate and rates of bystander CPR at OHCA at municipal level. An uneven distribution of OHCA per 100,000 inhabitants is seen with areas of relatively higher rates of OHCA in rural areas of Denmark (Figure 2a). The distribution of 30-day survival rates differs greatly from 0% to approximately 40%, with a tendency to higher rates in densely populated municipalities (Figure 2b). The distribution of BLS course participation rates was seemingly even distributed with some local clusters, notably with lower rates in the greater Copenhagen area (capital) and Aarhus, the second-largest city of Denmark (Figure 2c). Bystander CPR rates were generally high in Denmark, ranging from 57.9% to 91.7% with a tendency for higher rates in the western part of the country (Figure 2d).
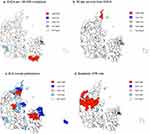
Spatial Clustering and Over Dispersion
Table 2 shows global Moran’s Index summary statistics. The Global Moran’s I analysis on all four incidence proportions showed that data were not geographically randomly distributed. This suggests tendencies to geographical clusters (Table 2). Figure 3 presents local Moran’s maps and shows areas significantly different from random distribution. Both significant “hot” and “cold” spots were identified in all analyses. The map of OHCA per 100,000 inhabitants shows a major hot spot of high frequency of OHCA in the south-eastern municipalities of Denmark (Figure 3a). The distribution of 30-day survival illustrated on LISA map shows two minor unrelated hot spots (Figure 3b). The map of BLS course participation rates shows several local clusters with significant hot and cold spots (Figure 3c). The LISA map for bystander CPR rates shows one large connected hot spot in the western part and one cold spot in the eastern part of Denmark (Figure 3d).
 |
Table 2 Global Moran’s I Summary Statistics |
Non-Spatial Regression Analysis
Table 3 presents results of the non-spatial and spatial regression models.
 |
Table 3 Odds Ratios and Summary Statistics from Non-Spatial and Spatial Analysis |
Crude analysis shows tendencies towards positive association between bystander CPR and an increase in course proportion on a municipal level. The association between 30-day survival and an increase in course proportion showed no clear tendencies. CAR analysis generally showed stronger association between exposure and outcome and hence limited spatial over-dispersion in the associations.
Spatial Regression Analysis
The CAR analysis showed that a 5% increase in municipal BLS course participation rate was significantly associated with an increased rate of bystander CPR prior to arrival of ambulance. The adjusted OR of bystander CPR rate was 1.34 (credible intervals: 1.02;1.76, ρ: 0.052, τ2: 0.063) when BLS course participation rate increased by 5%. The same results were observed on OHCAs in out-of-office hours with a significant OR of 1.43 (credible intervals: 1.09;1.89). Similar non-significant trend was seen in OHCA in public locations. There was no significant association with 30-day survival rates and BLS course participation rates in CAR regression (Table 3).
Discussion
This paper shows that even a 5% increase in BLS course participation rate on municipal level significantly increases the likelihood of bystander CPR rates with a factor 1.34. The municipal effect was even more profound in the out-of-office hours, with a rise in bystander CPR rates of a factor 1.43. Spatial analysis shows that several municipalities together formed clusters with significantly higher or lower BLS course participation rates.
The possibilities for direct comparison of result is limited by the lack of similar literature. No prior studies have conducted similar full population and whole country investigations examining all OHCAs in the period with spatial corrections. Several studies have found similar results indicating a positive relationship between BLS course participation rate and survival.20,21 However, the results are not completely compatible.
A study by Karam et al adjusted for many of the same variables as the current paper. Our current paper also incorporates socio-demographic confounders to survival, spatial dispersion, and adjusted full population as well as all types of OHCA. The inclusion of socio-demographic variables can seemingly limit some of the residual confounding in geographical analysis. Figure 2 in this study does not visualize the association in an intuitive equal colored prevalences. Nevertheless, there was a clear tendency in both studies showing that mass education in BLS was correlated with positive outcome for OHCA.
The analysis in the current paper expands the understanding of the impact of BLS mass education by showing that the effect of BLS mass education can be seen even on the relatively small spatial unit of Danish municipalities. This supports the assumption that bystanders trained in BLS were more willing to act and perform CPR.16–19 In terms of the chain of survival, this is the first link labeled early recognition.36 The importance of earlier recognition as a result of BLS education and training has been stressed by many in the resuscitation society37–40 and several key publications suggest this to impact survival.41,42 This might explain some of the remaining residual variance in the models.
It has been shown in several settings that social disparities impact survival from OHCA with a clear tendency for low-income areas to have lower bystander CPR rates, lower usage of AED, and hence lower survival rates.24,43,44 Further, it was shown that rurality does not decrease the chance of survival from OHCA with a shockable rhythm in Denmark.24 Similar to the disparities in the factors associated with survival from OHCA, many social disparities have been shown in the distribution of BLS education. It is known that people who have lower education and income levels, living in rural areas, and older age generally have lower BLS course participation rates.45–49 However, further research needs to be conducted to conclude on association between the models in this study and population density. The authors hypothesize that one contributing factor to a lower impact of social factors in the Danish setting might be the broad distribution of BLS education in all parts of society.13 This is in part due to mandated course participation when acquiring driver’s license.13
The choice of spatial unit, the Danish municipalities, was a result of two factors. First, most analyses considering modeling with known confounders require a minimum amount of data from all variables in all units. Choosing smaller available administrative units was not possible as this would render too many units empty and hence disable analysis. Second, the clinical implications of different results from smaller or larger units would potentially be severely limited. Conclusions based on geographical units smaller than municipalities were not much used as the units get too small. Further, choosing larger units renders the conclusion so broad that spatial differentiation is increasingly meaningless.
Limitation
Denmark is a relatively small country with 5,8 million inhabitants. The population is relatively homogeneous in terms of educational status, social status, and habitation. This limits the direct comparative value of the results.
This paper has several limitations. First, this paper does not address the fact that the quality of BLS is known to decrease rapidly after course participation.40,50,51 Hence, during the period of 4 years for municipal analysis it is to be expected that many participants will have loss of BLS skills. Second, we cannot be sure that BLS courses have been attained prior to the relevant OHCA. Therefore, the conclusions in the current paper describe the tendencies of mass education in BLS in municipalities. Third, this paper has not included analysis of individuals changing residence. The residency of all individuals is based on 2019 residency. The results cannot be interpreted at an individual level (ecological fallacy). Fourth, this paper measures education in BLS only through certified courses. Thus, other means of achieving skills within BLS are not included.
Conclusion
This study found a positive effect of mass education in BLS on bystander CPR rates. Even a 5% an increase in BLS course participation rate at municipal level significantly increased the likelihood of bystander CPR rates with a factor 1.34 at municipal level. The effect was even more profound in out-of-office hours with a rise in bystander CPR rates at OHCA. The results should be considered when designing and evaluating campaign to increase survival from OHCA. When designing strategies for improving survival, mass education in BLS should be considered, even at a municipal level.
Abbreviations
AED, automatic external defibrillator; CAR, conditional autoregressive; CPR, cardiopulmonary resuscitation; BLS, basic life support; OHCA, out-of-hospital cardiac arrest; OR, odds ratio; GLM, generalized linear model; LISA, local indicators of spatial association.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Professor Christian Torp-Pedersen reports grants from Novo Nordisk and grants from Bayer, outside the submitted work. The authors report no other conflicts of interest in this work
References
1. Grasner JT, Wnent J, Herlitz J, et al. Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa TWO study. Resuscitation. 2020;148:21826. doi:10.1016/j.resuscitation.2019.12.042
2. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. 2019;321:120010. doi:10.1001/jama.2019.1696
3. Kiguchi T, Okubo M, Nishiyama C, et al. Out-of-hospital cardiac arrest across the world: first report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020;152:3949. doi:10.1016/j.resuscitation.2020.02.044
4. Gräsner JT, Herlitz J, Tjelmeland IBM, et al. European Resuscitation Council Guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61–79. PMID: 33773833. doi:10.1016/j.resuscitation.2021.02.007
5. Dansk Hjertestopsregister [Danish Cardiac Arrest Registry]; 2021. Available from: http://hjertestopregister.dk/wp-content/uploads/2019/11/Dansk-Hjertestopregister-2018.pdf.
6. Wissenberg M, Lippert FK, Folke F, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377–1384. doi:10.1001/jama.2013.278483
7. Eisenberg M, Lippert FK, Castren M, et al. Acting on the call; 2019. Available from: http://www.globalresuscitationalliance.org/wp-content/pdf/acting_on_the_call.pdf.
8. Eisenberg M. A call to establish a global resuscitation alliance; 2018. Available from: https://foundation915.files.wordpress.com/2016/07/a-call-to-establish-a-global-resuscitation-alliance-2016.pdf.
9. Nakahara S, Tomio J, Ichikawa M, et al. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA. 2015;314:247–254.
10. Hallstrom AP, Ornato JP, Weisfeldt M, et al; Public Access Defibrillation Trial Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637–646.
11. Weisfeldt ML, Sitlani CM, Ornato JP, et al.; ROC Investigators. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55(16):1713–1720. doi:10.1016/j.jacc.2009.11.077
12. Hansen SM, Hansen CM, Folke F, et al. Bystander defibrillation for out-of-hospital cardiac arrest in public vs residential locations. JAMA Cardiol. 2017;2:507–514. doi:10.1001/jamacardio.2017.0008
13. Jensen TW, Folke F, Andersen MP, et al. Socio-demographic characteristics of basic life support course participants in Denmark. Resuscitation. 2022;170:167–177. doi:10.1016/j.resuscitation.2021.11.006
14. Perkins GD, Handley AJ, Koster RW, et al. European resuscitation council guidelines for resuscitation 2015: section 2. adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi:10.1016/j.resuscitation.2015.07.015
15. Jensen TW, Møller TP, Viereck S, et al. A nationwide investigation of CPR courses, books, and skill retention. Resuscitation. 2019;134:110–121. PMID: 30385384. doi:10.1016/j.resuscitation.2018.10.029
16. Swor R, Khan I, Domeier R, et al. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(6):596–601. PMID: 16614455. doi:10.1197/j.aem.2005.12.021
17. Cho GC, Sohn YD, Kang KH, et al. The effect of basic life support education on laypersons’ willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81(6):691–694. PMID: 20347208. doi:10.1016/j.resuscitation.2010.02.021
18. Taniguchi T, Omi W, Inaba H, et al. Attitudes toward the performance of bystander cardiopulmonary resuscitation in Japan. Resuscitation. 2007;75(1):82–87. PMID: 17420082. doi:10.1016/j.resuscitation.2007.02.019
19. Hamasu S, Morimoto T, Kuramoto N, et al. Effects of BLS training on factors associated with attitude toward CPR in college students. Resuscitation. 2009;80(3):359–364. PMID: 19181430. doi:10.1016/j.resuscitation.2008.11.023
20. Malta Hansen C, Kragholm K, Pearson DA, et al. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314(3):255–264. PMID: 26197186. doi:10.1001/jama.2015.7938
21. Karam N, Narayanan K, Bougouin W, et al. Major regional differences in automated external defibrillator placement and basic life support training in France: further needs for coordinated implementation. Resuscitation. 2017;118:49–54. doi:10.1016/j.resuscitation.2017.07.002
22. Karlsson L, Malta Hansen C, Wissenberg M, et al. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: a registry-based study. Resuscitation. 2019;136:30–37. doi:10.1016/j.resuscitation.2019.01.014
23. Sondergaard KB, Hansen SM, Pallisgaard JL, et al. Out-of-hospital cardiac arrest: probability of bystander defibrillation relative to distance to nearest automated external defibrillator. Resuscitation. 2018;124:138–144. doi:10.1016/j.resuscitation.2017.11.067
24. Ringgren KB, Kragholm KH, Lindgren FL, et al. Out-of-hospital cardiac arrest: does rurality decrease chances of survival? Resusc Plus. 2022;9:100208. doi:10.1016/j.resplu.2022.100208
25. Population and population projections in Denmark [Internet/ English]; 2021. Available from: www.dst.dk/en/Statistik/emner/befolkning-og-valg/befolkning-og-befolkningsfremskrivning.
26. Immigrants and their descendants [Internet/ English]; 2023. Available from: https://www.dst.dk/en/Statistik/emner/borgere/befolkning/indvandrere-og-efterkommere.
27. Lindskou TA, Mikkelsen S, Christensen EF, et al. The Danish prehospital emergency healthcare system and research possibilities. Scand J Trauma Resusc Emerg Med. 2019;27(1):100. doi:10.1186/s13049-019-0676-5
28. Statistics Denmark, Income for people (14 years +) by region, unit, sex and type of income [Internet/ English]; 2021. Available from: https://www.statistikbanken.dk/INDKP101.
29. Al-Dury N, Ravn-Fischer A, Hollenberg J, et al. Identifying the relative importance of predictors of survival in out of hospital cardiac arrest: a machine learning study. Scand J Trauma Resusc Emerg Med. 2020;28(1):60. doi:10.1186/s13049-020-00742-9
30. Madsen KB, Ersbøll AK, Olsen J, Parner E, Obel C. Geographic analysis of the variation in the incidence of ADHD in a country with free access to healthcare: a Danish cohort study. Int J Health Geogr. 2015;14:24. doi:10.1186/s12942-015-0018-4 PMID: 26297014; PMCID: PMC4546292.
31. Fischer MM, Getis A. Handbook of Applied Spatial Analysis: Soft- Ware Tool, Methods and Applications. Berlin: Springer; 2010.
32. Rgeoda package, vignette [Internet/ English]; 2022; Available from: https://raw.githubusercontent.com/GeoDaCenter/rgeoda/master/vignettes/rgeoda_tutorial.Rmd.
33. Lee D. CARBayes: an R package for Bayesian spatial modeling with condi- tional autoregressive priors. J Stat Softw. 2013;55(13):1–24. doi:10.18637/jss.v055.i13
34. Lee D. CARBayes: an R package for bayesian spatial modeling with conditional autoregressive priors. J Stat Softw. 2013;55:1–2.
35. Falci SGM, Marques LS CONSORT: when and how to use it. Dental Press J Orthod. 2015;20(3):13–15.
36. Olasveengen TM, Semeraro F, Ristagno G, et al. European resuscitation council guidelines 2021 Basic Life Support. Resuscitation. 2021;161:98–114. doi:10.1016/j.resuscitation.2021.02.009
37. Cobb LA, Hallstrom AP. Community-based cardiopulmonary resuscitation: what have we learned? Ann N Y Acad Sci. 1982;382:330–342. doi:10.1111/j.1749-6632.1982.tb55228.x
38. Koster RW. Modern BLS, dispatch and AED concepts. Best Pract Res Clin Anaesthesiol. 2013;27(3):327–334. doi:10.1016/j.bpa.2013.07.005
39. Jarrah S, Judeh M, AbuRuz ME. Evaluation of public awareness, knowledge and attitudes towards basic life support: a cross-sectional study. BMC Emerg Med. 2018;18(1):37. doi:10.1186/s12873-018-0190-5
40. Partiprajak S, Thongpo P. Retention of basic life support knowledge, self-efficacy and chest compression performance in Thai undergraduate nursing students. Nurse Educ Pract. 2016;16(1):235–241. doi:10.1016/j.nepr.2015.08.012
41. Strömsöe A, Svensson L, Axelsson ÅB, et al. Improved outcome in Sweden after out-of-hospital cardiac arrest and possible association with improvements in every link in the chain of survival. Eur Heart J. 2015;36(14):863–871. doi:10.1093/eurheartj/ehu240
42. Viereck S, Møller TP, Ersbøll AK, et al. Recognising out-of-hospital cardiac arrest during emergency calls increases bystander cardiopulmonary resuscitation and survival. Resuscitation. 2017;115:141–147. doi:10.1016/j.resuscitation.2017.04.006
43. Dahan B, Jabre P, Karam N, et al. Impact of neighbourhood socio-economic status on bystander cardiopulmonary resuscitation in Paris. Resuscitation. 2017;110:107–113. doi:10.1016/j.resuscitation.2016.10.028
44. Andersen LW, Holmberg MJ, Granfeldt A, et al. Neighborhood characteristics, bystander automated external defibrillator use, and patient outcomes in public out-of-hospital cardiac arrest. Resuscitation. 2018;126:72–79. doi:10.1016/j.resuscitation.2018.02.021
45. Bakke HK, Steinvik T, Angell J, Wisborg T. A nationwide survey of first aid training and encounters in Norway. BMC Emerg Med. 2017;17(1):6. doi:10.1186/s12873-017-0116-7
46. Cartledge S, Saxton D, Finn J, Bray JE. Australia’s awareness of cardiac arrest and rates of CPR training: results from the Heart Foundation’s HeartWatch survey. BMJ Open. 2020;10(1):e033722. doi:10.1136/bmjopen-2019-033722
47. Blewer AL, Ibrahim SA, Leary M, et al. Cardiopulmonary resuscitation training disparities in the United States. J Am Heart Assoc. 2017;6(5):e006124. doi:10.1161/JAHA.117.006124
48. Axelsson AB, Herlitz J, Holmberg S, Thorén AB. A nationwide survey of CPR training in Sweden: foreign born and unemployed are not reached by training programmes. Resuscitation. 2006;70(1):90–97. doi:10.1016/j.resuscitation.2005.11.009
49. Abdulhay NM, Totolos K, McGovern S, et al. Socioeconomic disparities in layperson CPR training within a large U.S. city. Resuscitation. 2019;141:13–18. doi:10.1016/j.resuscitation.2019.05.038
50. Anderson R, Sebaldt A, Lin Y, Cheng A. Optimal training frequency for acquisition and retention of high-quality CPR skills: a randomized trial. Resuscitation. 2019;135:153–161. doi:10.1016/j.resuscitation.2018.10.033
51. Madden C. Undergraduate nursing students’ acquisition and retention of CPR knowledge and skills. Nurse Educ Today. 2006;26(3):218–227. doi:10.1016/j.nedt.2005.10.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.