Back to Journals » Infection and Drug Resistance » Volume 16
Genomic Analysis of Carbapenem-Resistant Hypervirulent Klebsiella pneumoniae in a Chinese Tertiary Hospital
Authors Chen L, Zhou Y, Wang S, Wu C, Zhou P, Wang B, Chen Z, Yu F
Received 18 July 2023
Accepted for publication 21 September 2023
Published 27 September 2023 Volume 2023:16 Pages 6385—6394
DOI https://doi.org/10.2147/IDR.S425949
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Lan Chen,1,* Ying Zhou,2,* Shanshan Wang,1 Chunyang Wu,3 Peiyao Zhou,4 Bingjie Wang,2 Zhu Chen,5 Fangyou Yu2
1Department of Clinical Laboratory Medicine, The First Affiliated Hospital of Ningbo University, Ningbo, Zhejiang, 315010, People’s Republic of China; 2Department of Clinical Laboratory Medicine, Shanghai Pulmonary Hospital, Tongji University School of Medicine, Shanghai, 200082, People’s Republic of China; 3Department of Respiratory Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, 325000, People’s Republic of China; 4Department of Laboratory Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 5Department of Clinical Laboratory Medicine, Ningbo No. 2 Hospital, Ningbo, Zhejiang, 315010, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhu Chen; Fangyou Yu, Email [email protected]; [email protected]
Background: Carbapenem-resistant hypervirulent Klebsiella pneumoniae (CR-hvKP) has become a clinical crisis and is associated with significant morbidity and mortality. The prevalence of CR-hvKP has trended upward since 2010. This study aims to describe the clinical and genomic characteristics of CR-hvKP collected from a tertiary hospital in eastern China, from August 2020 to October 2021.
Methods: We tested the susceptibility to common antibiotics in these isolates to feature the antibiotic-resistant phenotypes. We also applied whole-genome sequencing and core-genome phylogenetic to analysis the genetic features of these isolates. Plasmid replicons were identified by using the PlasmidFinder database, and core-genome phylogenetic analysis by Parsnp database.
Results: All these strains isolated from the patients with serious underlying diseases and poor prognosis. We found all CR-hvKp isolates exhibited a multidrug-resistant (MDR) phenotype. These results revealed that blaKPC-2 was the predominant carbapenemases gene (n = 53, 84.1%), and ST11-KL64 CR-hvKP strains dominated, forming a single cluster, and differed by an average of 26 core SNPs. We only found eight ST15 isolates containing KL24 and KL112 type capsules, with the main carbapenem resistance genes being blaOXA-232 and blaKPC-2. All ST11-KL64 strains had a series of resistance and virulence genes, along with IncHIB-FIB virulence plasmids and IncFII resistance plasmids, while the prevalence of resistance plasmids like the IncFII plasmid was absence in ST15 isolates.
Conclusion: This suggests that ST11-KL64 CR-hvKP has emerged as the most prevalent hypervirulence and carbapenem-resistant K. pneumoniae and may contribute to hospital outbreaks of infection, which required most clinical attention.
Keywords: carbapenem-resistant, hypervirulence, Klebsiella pneumoniae, whole-genome sequencing, antimicrobial resistance, virulence genes
Introduction
Klebsiella pneumoniae (KP) is a common opportunistic pathogen in clinical practice, capable of causing infectious diseases in the urinary tract, respiratory tract, blood, and soft tissues.1 Hypervirulent Klebsiella pneumoniae (hvKp) has a higher virulence than KP2 and can cause severe infectious diseases, including pyogenic liver abscess, endophthalmitis, and meningitis.3,4
Although multidrug resistance and hypervirulence were previously thought to follow distinct evolutionary directions with non-overlapping genomic signatures for each phenotype,5 hvKp has recently garnered more attention due to its increased likelihood of acquiring antimicrobial resistance (AMR) genes, particularly those that code for carbapenemases.2,6 Carbapenem-resistant hvKp (CR-hvKp) exhibits both hypervirulence and carbapenem resistance phenotypes, making infections caused by these strains difficult to treat with current antibiotics, and should therefore receive greater attention.7
CR-hvKP emerged in the early 2010s and is primarily prevalent in Asia, especially China, but cases have been reported worldwide.8 In 2016, a lethal outbreak of ST11 CR-hvKP occurred in a Chinese intensive care unit, with 21 ST11 KPC-2-producing CR-hvKP strains isolated from five patients who died during hospitalization.7 CR-hvKP has spread globally and poses a significant human public health threat.9 Therefore, the early recognition of these hypervirulent strains, including their resistance determinants, is a priority concern.
The aim of our study was to determine the current occurrence of CR-hvKp in a tertiary hospital in eastern China. We analyzed the clinical outcomes through reviewing medical history and identified different serotypes, virulence-associated markers, and antimicrobial drug resistance genes among the CR-hvKp isolates by using whole genome sequencing (WGS).
Materials and Methods
Bacterial Strains
To explore the characteristics of the carbapenem-resistant hypervirulent K. pneumoniae (CR-hvKP) isolates, we collected 63 CR-hvKP isolates from 54 patients with underlying diseases and poor prognosis in a tertiary hospital in Ningbo, Zhejiang Province, China, from August 2020 to October 2021. The strains from different isolation sites of the same patient were included in this study. All the information about the patients were listed in Table 1. The speciation was determined by Matrix-Assisted Laser Flight Desorption/ Ionisation Time of (MALDI-TOF MS). Based on the antibiotic susceptibility results and the patient’s prognosis, we initially determined whether the infected bacteria were CR-hvKP, and then further confirmed based on the results of whole-genome sequencing.
 |
Table 1 Characteristics of Clinical Cases and Isolates |
Antimicrobial Susceptibility Test
We performed bacterial antimicrobial susceptibility testing using VITEK2 system. MICs were measured for cefoxitin, ceftriaxone, aztreonam, cefepime, imipenem, tobramycin, gentamicin, amikacin, ciprofloxacin, levofloxacin, piperacillin/tazobactam, amoxicillin/clavulanic acid and trimethoprim/sulfamethoxazole. For MIC determination, E. coli ATCC 25922 was used as a quality control strain, which was purchased from National Center for Clinical Laboratories and kept by our laboratory. CLSI2022-M100-ED31was used to determine the interpretative breakpoints.10
Whole-Genome Sequencing and Bioinformatics Analysis
The genomic DNA of these CR-hvKP was extracted using a commercial DNA extraction kit (Qiagen, Germany). The genome sequencing was then performed by the Illumina NovaSeq 6000 platform, with 2×150 bp paired-end reads. The multilocus sequence typing (MLST), capsular type, resistance and virulence determinants were determined by the Kleborate (version 0.3.0) (https://github.com/katholt/Kleborate/). Plasmid replicons were identified using the PlasmidFinder database using the minimum coverage and minimum identities of 90% (https://cge.cbs.dtu.dk/services/PlasmidFinder/).
Results
Clinical Characteristics of Patients Infecting with CR-hvKp
We collected 63 isolates of carbapenem-resistant hypervirulent K. pneumoniae (CR-hvKP) from 54 patients at a tertiary hospital in China. This study included strains from different isolation sites of the same patient, with 9 patients having 2 isolates from different specimens (Table 1). The patients were predominantly males (81.5%, n = 44) with a median age of 66 years. They were mainly from different ICU wards in the hospital (23/54 42.6%), followed by the emergency intensive care unit (EICU; 6/54, 11.1%), gerontology (5/54; 9.3%), hematology (4/54; 7.4%), neurosurgery (3/54; 5.5%), emergency ward (3/54; 5.5%) and other wards (10/54; 18.6%). Among the 63 CR-hvKP isolates, a variety of clinical specimens were involved, including sputum (37/63, 58.7%), blood (11/63, 17.5%), urine (4/63, 6.3%), stool (4/63, 6.3%), and other specimens (7/63, 11.2%). Notably, some patients had poor prognoses, with 20 patients (37.0%) experiencing delirium during discharge, 4 patients still requiring treatment, and 2 patients dying during their hospitalization. Due to the multidrug resistance and higher virulence of infections caused by CR-hvKP isolates, distressing clinical outcomes were more likely to occur.
Antimicrobial Resistance Phenotype of the CR-hvKp Isolates
To clarify the antibiotic-resistant phenotype of these CR-hvKp isolates, we tested their susceptibility to 13 antibiotics (Table 2). We found that CR-hvKp was resistant to multiple antibiotic classes, with most isolates showing high-level resistance to carbapenems and all β-lactam antibiotics, including ceftriaxone, cefepime, cefoxitin, and aztreonam (Table 2). Resistance to fluoroquinolones was also frequent, with 92.1% and 88.9% of isolates resistant to ciprofloxacin and levofloxacin, respectively. However, the isolates were relatively susceptible to three antimicrobials: gentamicin, tobramycin, and amikacin, with resistance rates of 23.8%, 22.2%, and 15.9%, respectively. All CR-hvKp exhibited a multidrug-resistant (MDR) phenotype showing resistant to three or more antibiotic classes and 27.0% were resistant to all six antimicrobial classes.
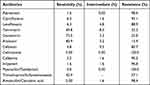 |
Table 2 Antibiotic Susceptibilities of 63 Carbapenem-Resistant K. pneumoniae |
Genomic Phylogeny of CR-hvKp Isolates
To gain a deeper understanding of the molecular mechanisms behind these strains, we conducted whole-genome sequencing and core-genome phylogenetic analysis (Figure 1). The results showed that the ST11 CR-hvKP strains dominated, forming a single cluster, and differed by an average of 26 core SNPs, indicating clonal expansion. These ST11 strains contained the KL64 capsule type and had a series of resistance and virulence genes, along with IncHI1B-FIB virulence plasmids and IncFII resistance plasmids (Figure 1). This suggests that ST11-KL64 CR-hvKP has emerged as the most prevalent hypervirulence and carbapenem-resistant K. pneumoniae and may contribute to hospital outbreaks of infection.
While ST15 K. pneumoniae was identified as the second most frequent CRKP clone in hospital infections after ST11 K. pneumoniae, hypervirulent ST15 CRKP was uncommon. We found eight ST15 isolates containing KL24 and KL112 type capsules, with the main carbapenem resistance genes being blaOXA-232 and blaKPC-2. The prevalence of resistance plasmids like the IncFII plasmid did not observed in ST15 isolates, but only the IncHI1B-FIB virulence plasmid in these ST15 clusters.
In addition to the ST11 and ST15 CR-hvKP prevalence clones, we found several hypervirulent clones like ST412 and ST65 that obtained resistance elements to generate hypervirulent CRKP (Figure 1). Although the classical hypervirulent clone ST412 isolates contained the blaKPC-2 gene, we observed no plasmids, indicating that the gene may have been obtained through other mobile elements. For the ST65 strains, the resistance phenotype mainly attributed to another resistance plasmid, the IncX plasmid, harboring blaNDM-1 and blaKPC-3 genes. The co-existence of different plasmids and the diversity of plasmids simultaneously contributed to the transmission of both resistant and hypervirulent phenotypes in CR-hvKP isolates.
The Distribution of Antibiotic Resistance Genes and Virulence Factors
The presence of carbapenem-resistant genes in all 63 isolates is concerning, as it limits the options for effective antimicrobial treatment. Most of the isolates carried the blaKPC gene, particularly blaKPC-2, but other carbapenemase genes such as blaOXA and blaNDM were also found. A small proportion of isolates carried multiple carbapenemase genes, which further complicates treatment options. Additionally, a significant proportion of isolates carried beta-lactamase genes.
The hypervirulence of hvKp is due to its unique characteristics, including capsule, lipopolysaccharide, siderophores, and allantoin metabolism. Genetic biomarkers such as iucA, iroB, rpmA, and rmpA2 can be used to identify hvKp strains. All isolates in the study carried the iucA gene, which is a critical factor contributing to the high pathogenicity of hvKP. The iroB gene was detected in 11 isolates, and the rpmA (26/63, 41.3%) and rmpA2 (55/63, 87.3%) genes were present in a significant proportion of isolates. The combination of these virulence determinants varied among different ST types, leading to different hypervirulence phenotypes.
Overall, the emergence of CR-hvKP strains with limited treatment options and high virulence is a significant public health concern, and further studies are needed to understand the molecular mechanisms behind these strains and develop effective prevention and treatment strategies.
Discussion
HvKp is an emerging pathogen that has been reported in the community setting and has recently caused infections in healthcare settings, with higher virulence and mortality rates.11,12 In this study, we used whole-genome sequencing (WGS) in conjunction with phenotypic surveillance to characterize CR-hvKP isolates collected from a large tertiary public health hospital in eastern China. This study aims to complement and update the growing body of epidemiological findings on this pathogen.
The majority of CR-hvKP isolates in our study were recovered from patients hospitalized in the ICU, EICU, and hematology departments. Patients hospitalized in these departments are at a greater risk of CR-hvKP infections, mainly due to immune status alterations, the use of broad-spectrum antibiotics, frequent comorbidities, and the use of invasive devices.13–16 These CR-hvKP isolates showed 27.0% resistance to all six antimicrobial classes. Due to their multidrug resistance and higher virulence, the prognosis of some patients was poor, with 37.0% of patients experiencing delirium at discharge. Therefore, to prevent transmission, we should screen for CRE carriage to enable early detection and implementation of eradication measures.
Our study revealed a high diversity of STs (n=8), with ST11-KL64 K. pneumoniae being the predominant blaKPC clone in China. ST11-KL64 CR-hvKP has been identified as a cause of bacterial liver abscess,17 bacteremia, and other infections, and it is a high-risk clinical pathogen that has gained worldwide attention.18 Notably, a Chinese report linked pneumonia with high mortality to ST11-KL64 CR-hvKP.19 Our study results are consistent with these findings, with ST11-KL64 (n=37, 58.7%) accounting for most of the strains. In a multicenter study, ST11 also accounted for most infections (66.6%), followed by ST45 (8.2%), ST15, and ST290 (5.4% each).20 KPC-producing ST15 K. pneumoniae have caused outbreaks.21 However, a recent Chinese surveillance study reported a lower frequency of ST15 clones,20 In our study, ST15 was the second most frequent CR-hvKP clone in hospital infections after ST11. Interestingly, we found that ST15-KL112 only carried OXA-232 genes, instead of blaKPC-2. All in all, ST11-KL64 CR-hvKP poses a significant challenge for clinicians in various clinical settings and warrants further attention.
The 63 CR-hvKP isolates posed multi-drug-resistant features that exhibited high-level resistance to all β-lactam antibiotics and carbapenems, but remained susceptible to aminoglycosides. All the isolates harboring carbapenemases gene, which make the major contribution to the MDR phenotype. In this study, blaKPC-2 genes were predominant among CR-hvKP isolates (84.1%, n = 53), similar finding was noted in Asia and America where blaKPC-2 is class A enzymes highly prevalent in CR-hvKP isolates.22 Moreover, the blaKPC-2 genes were distributed across almost all STs, while the diversity of strains carrying OXA-48-like genes was lower. In other countries, such as India, Iran, Russia, and Italy, the majority of CR-hvKP isolates were OXA-48-positive strains.22 It is important to note that global immigration may lead to changes in the linkages between bacterial resistance mechanisms and regions or cities.23 Therefore, surveillance of AMR trends should be maintained, and areas with low prevalence cannot be ignored. Furthermore, CR-hvKP strains simultaneously producing two or more carbapenemases can cause serious infectious diseases with high mortality.22 In our study, two CR-hvKP strains producing blaKPC-2 and blaNDM-5 carbapenem resistance genes were reported.
All these 63 strains were found to carry virulence genes, including aerobactin (iucA), salmochelin (iroB), and regulators of mucoid phenotype (rmpA and rmpA2). Siderophore systems are crucial for bacterial pathogenicity, enabling them to scavenge iron from host transport proteins, allowing them to survive and proliferate in the host.24 Aerobactin plays a crucial role in both in vivo and vivo survival of hvKp, compared to other siderophores.2 Aerobactin has been identified as the most prevalent siderophore in hvKp.2 These investigations indicate that aerobactin (iucA) is the primary determinant of the virulence of hvKP. Our study showed the presence of iucA universally among all isolates, and all 63 isolates harbored carbapenemase-encoding genes, indicating the convergence of hypervirulence and multidrug resistance.
While salmochelin (iroB) was detected in only 5.4% of bacteremia isolates,20 it was present in 17.5% of isolates in our study. We also observed a higher frequency of rmpA in isolates (41.3%) compared to bacteremia isolates in a previous study (25.2%).20 The gene encoding aerobactin (iucA) was detected in 10.3% of isolates in Singapore, while the remaining virulence genes (iro, rmpA, and rmpA2) were far less prevalent, occurring in only 2.4% to 4.5% of the isolates.25 The regulators of mucoid phenotype genes, rmpA/A2, were associated with hypermucoviscosity.26 Strains with rmpA/A2 were mainly enriched in KL1/KL2 and ST23/ST86/ST65 hypervirulent clones.26 However, rmpA/A2 was distributed across most strains in our study, except for the ST37-KL25 strains. The most pandemic linage observed in our study was ST11-KL64, which harbored iucA, rpmA, and rmpA2.
The copresence of iucA, iroB, rmpA, and rmpA2 was observed in most isolates of ST412-KL57 and ST65-KL2 in our study, except for FK3104. Twenty-seven of the 63 CR-hvKP isolates (42.9%) harbored three or more hypervirulence genes. K. pneumoniae isolates carrying hypervirulence genes pose a risk of transmission and constitute a significant public health threat once they exhibit hypervirulence in vitro and vivo.
Conclusion
ST11-KL64 CR-hvKP has emerged as the most prevalent hypervirulence and carbapenem-resistant K. pneumoniae and contribute to the transmission of both resistance and hypervirulence phenotype, which required most clinical attention.
Ethics Statement
The research protocol was approved by the Ethics Committee of The First Affiliated Hospital of Ningbo University (2023019A). We confirm that all adult participants gave their informed consent. Guidelines outlined in the Declaration of Helsinki were followed.
Funding
This research is supported by Medical Scientific Research Foundation of Zhejiang Province, Grant No.2023KY1072. This research is also supported by Medical Scientific Research Foundation of Zhejiang Province, Grant No.2022KY1124.
Disclosure
The authors report that there are no competing interests to declare for this work.
References
1. Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11(4):589–603. doi:10.1128/CMR.11.4.589
2. Shon AS, Bajwa RP, Russo TA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: a new and dangerous breed. Virulence. 2013;4(2):107–118. doi:10.4161/viru.22718
3. Wang JH, Liu Y-C, Lee SS-J, et al. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin Infect Dis. 1998;26(6):1434–1438. doi:10.1086/516369
4. Xu M, Fu Y, Fang Y, et al. High prevalence of KPC-2-producing hypervirulent Klebsiella pneumoniae causing meningitis in Eastern China. Infect Drug Resist. 2019;12:641–653. doi:10.2147/IDR.S191892
5. Bialek-Davenet S, Criscuolo A, Ailloud F, et al. Genomic definition of hypervirulent and multidrug-resistant Klebsiella pneumoniae Clonal Groups. Emerg Infect Dis. 2014;20(11):1812–1820. doi:10.3201/eid2011.140206
6. Catalan-Najera JC, Garza-Ramos U, Barrios-Camacho H. Hypervirulence and hypermucoviscosity: two different but complementary Klebsiella spp. phenotypes? Virulence. 2017;8(7):1111–1123. doi:10.1080/21505594.2017.1317412
7. Gu D, Dong N, Zheng Z, et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect Dis. 2018;18(1):37–46. doi:10.1016/S1473-3099(17)30489-9
8. Zhang R, Lin D, Chan EW-C, et al. Emergence of carbapenem-resistant serotype K1 hypervirulent Klebsiella pneumoniae strains in China. Antimicrob Agents Chemother. 2016;60(1):709–711. doi:10.1128/AAC.02173-15
9. Wozniak JE, Band VI, Conley AB, et al. A nationwide screen of carbapenem-resistant Klebsiella pneumoniae reveals an isolate with enhanced virulence and clinically undetected colistin heteroresistance. Antimicrob Agents Chemother. 2019;63(5). doi:10.1128/AAC.00107-19
10. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, 26th Informational Supplement (M100-S26). Clinical and Laboratory Standards Institute; 2022.
11. Liu C, Guo J. Characteristics of ventilator-associated pneumonia due to hypervirulent Klebsiella pneumoniae genotype in genetic background for the elderly in two tertiary hospitals in China. Antimicrob Resist Infect Control. 2018;7(1):95. doi:10.1186/s13756-018-0371-8
12. Zhang Y, Zhao C, Wang Q, et al. High prevalence of hypervirulent Klebsiella pneumoniae infection in china: geographic distribution, clinical characteristics, and antimicrobial resistance. Antimicrob Agents Chemother. 2016;60(10):6115–6120. doi:10.1128/AAC.01127-16
13. Akturk H, Sutcu M, Somer A, et al. Carbapenem-resistant Klebsiella pneumoniae colonization in pediatric and neonatal intensive care units: risk factors for progression to infection. Braz J Infect Dis. 2016;20(2):134–140. doi:10.1016/j.bjid.2015.12.004
14. Borer A, Saidel-Odes L, Eskira S, et al. Risk factors for developing clinical infection with carbapenem-resistant Klebsiella pneumoniae in hospital patients initially only colonized with carbapenem-resistant K pneumoniae. Am J Infect Control. 2012;40(5):421–425. doi:10.1016/j.ajic.2011.05.022
15. Wang Z, Qin -R-R, Huang L, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection and mortality of Klebsiella pneumoniae infection. Chin Med J. 2018;131(1):56–62. doi:10.4103/0366-6999.221267
16. Zhang Y, Guo L-Y, Song W-Q, et al. Risk factors for carbapenem-resistant K. pneumoniae bloodstream infection and predictors of mortality in Chinese paediatric patients. BMC Infect Dis. 2018;18(1):248. doi:10.1186/s12879-018-3160-3
17. Yang Q, Jia X, Zhou M, et al. Emergence of ST11-K47 and ST11-K64 hypervirulent carbapenem-resistant Klebsiella pneumoniae in bacterial liver abscesses from China: a molecular, biological, and epidemiological study. Emerg Microbes Infect. 2020;9(1):320–331. doi:10.1080/22221751.2020.1721334
18. Wu H, Li D, Zhou H, et al. Bacteremia and other body site infection caused by hypervirulent and classic Klebsiella pneumoniae. Microb Pathog. 2017;104:254–262. doi:10.1016/j.micpath.2017.01.049
19. Yang X, Sun Q, Li J, et al. Molecular epidemiology of carbapenem-resistant hypervirulent Klebsiella pneumoniae in China. Emerg Microbes Infect. 2022;11(1):841–849. doi:10.1080/22221751.2022.2049458
20. Cienfuegos-Gallet AV, Zhou Y, Ai W, et al. Multicenter Genomic Analysis of Carbapenem-Resistant Klebsiella pneumoniae from Bacteremia in China. Microbiol Spectr. 2022;10(2):e0229021. doi:10.1128/spectrum.02290-21
21. Vubil D, Figueiredo R, Reis T, et al. Outbreak of KPC-3-producing ST15 and ST348 Klebsiella pneumoniae in a Portuguese hospital. Epidemiol Infect. 2017;145(3):595–599. doi:10.1017/S0950268816002442
22. Han YL, Wen X-H, Zhao W, et al. Epidemiological characteristics and molecular evolution mechanisms of carbapenem-resistant hypervirulent Klebsiella pneumoniae. Front Microbiol. 2022;13:1003783. doi:10.3389/fmicb.2022.1003783
23. Bonomo RA, Burd EM, Conly J, et al. Carbapenemase-producing organisms: a global scourge. Clin Infect Dis. 2018;66(8):1290–1297. doi:10.1093/cid/cix893
24. Lee C-R, Lee JH, Park KS, et al. Antimicrobial resistance of hypervirulent Klebsiella pneumoniae: epidemiology, hypervirulence-associated determinants, and resistance mechanisms. Front Cell Infect Microbiol. 2017;7:483. doi:10.3389/fcimb.2017.00483
25. Teo JQ, Tang CY, Tan SH, et al. Genomic surveillance of carbapenem-resistant Klebsiella pneumoniae from a Major Public Health Hospital in Singapore. Microbiol Spectr. 2022;10(5):e0095722. doi:10.1128/spectrum.00957-22
26. Du Q, Pan F, Wang C, et al. Nosocomial dissemination of hypervirulent Klebsiella pneumoniae with high-risk clones among children in Shanghai. Front Cell Infect Microbiol. 2022;12:984180. doi:10.3389/fcimb.2022.984180
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

