Back to Journals » Journal of Multidisciplinary Healthcare » Volume 10
General practitioners' and primary care nurses' care for people with disabilities: quality of communication and awareness of supportive services
Authors Storms H , Marquet K, Claes N
Received 3 May 2017
Accepted for publication 12 July 2017
Published 20 September 2017 Volume 2017:10 Pages 367—376
DOI https://doi.org/10.2147/JMDH.S140962
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Hannelore Storms,1 Kristel Marquet,1,2 Neree Claes1,3
1Faculty of Medicine and Life Sciences, Hasselt University, Hasselt, Belgium; 2Quality and Safety Department, Jessa Hospital, Hasselt, Belgium; 3vzw Wit-Gele Kruis Limburg, Genk, Belgium
Background: General practitioners (GPs) and primary-care nurses (PCNs) often feel inexperienced or inadequately educated to address unmet needs of people with disabilities (PDs). In this research, GPs’ and PCNs’ communication with PDs and health care professionals, as well as their awareness of supportive measures relevant to PDs (sensory disabilities excluded), was examined.
Materials and methods: An electronic questionnaire was sent out to 545 GPs and 1,547 PCNs employed in Limburg (Belgium). GPs and PCNs self-reported about both communication with parties involved in care for PDs (scale very good, good, bad, very bad) and their level of awareness of supportive measures relevant for PDs (scale unaware, inadequately aware, adequately aware).
Results: Of the questionnaire recipients, 6.6% (36 of 545) of GPs and 37.6% (588 of 1,547) of PCNs participated: 68.8% of 32 GPs and 45.8% of 443 PCNs categorized themselves as communicating well with PDs, and attributed miscommunication to limited intellectual capacities of PDs. GPs and PCNs reported communicating well with other health care professionals. Inadequate awareness was reported for tools to communicate (88.3% of GPs, 89% of PCNs) and benefits for PDs (44.1% of GPs, 66.9% of PCNs).
Conclusion: GPs’ and PCNs’ lacking awareness of communication aids is problematic. Involvement in a multidisciplinary, expert network might bypass inadequate awareness of practical and social support measures.
Keywords: nursing care, disability, primary care, family medicine, networks, integrated care, unmet needs, quality, accessibility
Background
The unmet needs of people with disabilities (PDs) are significant in comparison to the general population.1–3 Although article 25 of the UN Convention on the Rights of Persons with Disabilities states the right of persons with disabilities to attain the highest standard of health care, PDs often experience health inequalities.4 Several studies have demonstrated the likelihood to have poorer health status and less chance of receiving preventive services when disabled.2,5,6 Tackling PDs’ health disparities is even more important, as the risk of developing secondary or comorbid conditions for this population is higher than for the general population: coronary heart diseases, urinary tract infections, and unhealthy lifestyles (smoking, sedentary lifestyle, malnutrition) are more prevalent in PDs in general.6–9 Moreover, the age of onset and degree of severity of disorders presented in PDs are different than can be expected in the general population.6–9
Because of the worldwide movement to deinstitutionalize care for PDs, primary-care services are becoming more important to organize the necessary health care this population needs.10 In Belgium, this shift from institutions toward more community-based services can be illustrated by the number of PDs contacting primary-care services. Despite efforts of the government to provide necessary care for PDs in a community-setting, eg, through benefits like a personal assistance budget, approximately 21,518 PDs (16%) of the 129,021 Dutch-speaking PDs (<65 years old) were waiting to be admitted to residential care facilities in 2013.11–13 This hampered accessibility of primary care is a major problem: care organized on this level has been shown to have important positive effects on health outcomes; moreover, it also decreases mortality for PDs.14,15 As formal primary care in Belgium – provided by general practitioners (GPs) and primary-care nurses (PCNs), among other care professionals – is lagging behind, PDs turn to informal (family) caregivers to receive the care they need. However, the emphasis should be on formal care, with informal care being complementary. After all, the role of informal caregiver can be very demanding, and burdening should be prevented.16–20
Inaccessibility of care has been illustrated in numerous reports.4,6,14,15,21–23 Mainstream health services are often unprepared to respond to this shift toward primary care.10 Primary-care professionals are suddenly expected to address PDs’ specific needs, even though they might not have sufficient (clinical) knowledge or might not have the skills to interact with this population.24,25 Previous research has described (primary) care professionals feeling insufficiently educated about the prevalence of diseases in PDs, being doubtful on how to respond to behavioral problems, not knowing how to communicate with PDs, finding it challenging to assess PDs, or having certain perceptions about this often-stigmatized population.26–29 Consequently, primary-care professionals might feel overwhelmed or anxious and might be more reluctant to treat PDs.29,30 If health care professionals fail to adapt to the needs of PDs, access to necessary care is jeopardized, potentially leading to major health problems in the form of hospital admissions and increased health care costs.31
Besides having sufficient clinical knowledge, primary-care professionals ought to make referrals to other care services, as well as provide support to PDs and their informal caregivers regarding practical and social issues, depending on their living situation.2,24,32,33 In order to act accordingly, interacting with PDs and their informal caregivers is required, as well as collaborating with other care professionals and agencies specialized in care for PDs. In general, communication with patients and the exchange of health care information among health care professionals is vital.34–37 To facilitate communication with PDs, several tools are available, eg, Tellus, sign language, and visualization (Picto).38 Primary-care professionals would benefit from being aware of these tools, because it would not only enable them to improve their therapeutic relationship with PDs by means of their communication, but when being able to guide PDs to these aids by informing them about their existence, they can actively contribute to PDs’ quality of life. To enable primary-care professionals to refer PDs to specialized services, they need to be aware of the agencies specialized in the organization of care for PDs. Consequently, primary-care professionals will then support PDs in their care management, as these agencies can provide accurate information and might offer necessary assistance with all forms and regulations. When primary-care professionals are unaware of tools to support PDs, unaware of agencies specialized in the organization of care for PDs, or when communication with other care professionals is hampered, management of care is often shifted to informal caregivers.39 The goal of this research was to examine GPs’ and PCNs’ self-reported quality of communication with PDs, informal caregivers, and care professionals, as well as to determine their awareness regarding supportive tools and procedures and agencies relevant in the care for PDs.
Materials and methods
Design
In this research, primary-care professionals self-reported about both the quality of their communication with other stakeholders in the care for PDs and the level of awareness regarding supportive measures available to this population. The online survey was distributed to all GPs and PCNs in one region in Belgium (Limburg).
Setting and participants
Participants were primary-care professionals employed as GPs or PCNs in home and/or residential care in Limburg. All these GPs and self-employed PCNs, as well as all PCNs employed by the regional nursing organization, were sent an email with a hyperlink to the questionnaire, via the umbrella organization of GPs and of self-employed PCNs and via the regional nursing organization, respectively. The online survey was sent to 545 GPs and 1,547 PCNs (September and December 2015).
Informed consent was acquired by proceeding to the first question after reading the introduction-section of the survey. This introduction stated clearly that in this research, PDs were regarded as everyone with a disability, except those who experience only sensory disabilities or impairments due to the normal aging process. Broadly stated, PDs are people with a congenital or noncongenital physical, intellectual, or developmental disability, eg, Down syndrome, oxygen deprivation at birth, acquired brain injury due to trauma or disease, spina bifida, and muscular diseases.
Questionnaire
The questionnaire was developed by a team of four GPs and 20 PCNs. These experts’ opinions on the organization of care and supportive measures for PDs shaped the content of the questionnaire. Several meetings were organized to discuss and review the questionnaire until consensus was reached on the final version. The questionnaire consisted of closed-ended questions addressing the following items. Some characteristics of GPs’ and PCNs’ patients were surveyed, more specifically about the care setting (home or residential care) in which they delivered care to PDs, the kinds of disabilities their patients had (physical, intellectual, or both), their contact with informal caregivers, and problems they perceive informal caregivers to be experiencing (overload of tasks, finding suitable care, coping with disability of their relatives/friends, difficulties in communicating with their relatives/friends with disabilities, hampered [para]medical follow-up).
Quality of communication was assessed on a scale of very good–good–bad–very bad. In particular, GPs and PCNs were asked to self-report about their communication with health care professionals (in home-care setting; in residential care setting, with GPs [to be answered by PCNs], with specialists [to be answered by GPs]) and with PDs. GPs and PCNs could also report about possible causes of hampered communication (limited intellectual capacity, lack of communication aids, cultural differences).
Awareness of supportive services was examined on a scale of unaware–inadequately aware–adequately aware: four supportive measures (communication aids [Tellus, sign language, visualizations [Picto], adjustments and tools to improve mobility of PDs, adjustments to their home, and adjustments and tools to improve PDs’ daily living) and four relevant procedures or agencies for PDs (benefits PDs might be entitled to, the responsibilities of VAPH [Flemish Agency for Disabled Persons], procedures for admission to residential care facilities, [residential] care facilities in the region) (Figure 1).
  | Figure 1 Quality of communication of GPs and primary-care nurses and their awareness regarding measures relevant to people with disabilities. |
Analysis
The questionnaire was developed with Qualtrics software. Quantitative analysis (mean, standard deviation, Fisher’s exact test) was performed using SPSS 22.0. Respondents with missing values for one or more variables were excluded from analyses that included those variables.
Ethics
As this research concerned perceptions of medical professionals, rather than data from patient surveys or medical records, it was exempt from review-board approval under Belgian law.
Results
A total of 2,092 questionnaires were sent: 36 GPs (response rate 6.6%) and 588 PCNs (response rate 38%) participated. In Table 1, the age distribution of the 624 respondents is listed. The majority (41.5%) was aged 46–60 years.
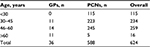  | Table 1 Age distribution of GPs and PCNs Abbreviations: GPs, general practitioners; PCNs, primary-care nurses. |
Characteristics of PDs and their informal caregivers
GPs (n=36) treated on average 20.3 (SD 25.4) PDs, and PCNs (n=588) treated 5.1 (SD 7.1) PDs. The majority of GPs (86.1%) and PCNs (64.6%) had all sorts of disabilities represented in their patients. Table 2 lists the three most frequently represented disabilities in patients of GPs and PCNs. The majority of GPs (47.2%) deliver care to PDs in residential care settings exclusively, the majority of PCNs (54.3%) exclusively in home care (Table 3). Sixteen (44.4.%) GPs and 200 PCNs (34%) reported a burdening of at least half of the informal caregivers. GPs and PCNs reported informal caregivers to be experiencing problems finding suitable care (88.9% of GPs, 48.3% of PCNs), overload of tasks (77.8% of GPs, 77.3% of PCNs), and coping with situations of disability (66.7% of GPs, 56.5% of PCNs).
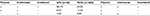  | Table 2 Top three disability types among patients of GPs and PCNs Abbreviations: GPs, general practitioners; PCNs, primary-care nurses. |
  | Table 3 Settings in which GPs and PCNs deliver care to people with disabilities Abbreviations: GPs, general practitioners; PCNs, primary-care nurses. |
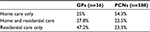
Communication of GPs and PCNs with PDs and health care professionals
Of the 34 GPs and 475 PCNs, two GPs and 32 PCNs reported experiencing hampered communication with PDs. In Figure 2, quality of communication is illustrated with a link to possible reasons for hampered communication from participants’ point of views. Difficulties in communication are frequently reported to be attributable to limited intellectual capacities of disabled patients of primary-care professionals. About half of the GPs and PCNs reported experiencing miscommunication with PDs, and a lack of communication aids was mentioned as the root of these communication problems. Overall, cultural differences are almost never reported to be a reason for miscommunication: only one GP (2.9%) and 72 PCNs (15.2%) reported this.
  | Figure 2 Reasons for hampered communication according to GPs and PCNs. Abbreviations: GPs, general practitioners; PCNs, primary-care nurses. |
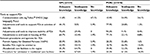
GPs’ (n=34) and PCNs’ (n=475) self-rating of their communication with health care professionals in home versus residential care as (very) good comprised 97.1% of GPs and 93.3% of PCNs versus 85.2% of GPs and 89.7% of PCNs (Table 4). In Figure 3, dichotomized quality of communication is depicted for GPs and PCNs delivering care to PDs in home- or residential care settings exclusively. None of the GPs working exclusively in home care or exclusively in residential care facilities self-reported communication with health care professionals in home care to be (very) bad.
  | Table 4 GPs’ and PCNs’ self-rating of communication with other health care professionals as (very) good Abbreviation: GPs, general practitioners; PCNs, primary-care nurses. |
  | Figure 3 Dichotomized quality of communication of GPs and PCNs across different settings. Abbreviations: GPs, general practitioners; PCNs, primary-care nurses. |
GPs and PCNs working in both home- and residential care settings (nine GPs, 100 PCNs) self-rated their communication as (very) good with professionals in home care (88.9% of GPs, 93% of PCNs), residential care (77.8% of GPs, 95% PCNs), and specialists (77.8% of GPs, 94% of PCNs). Fisher’s exact test was performed to detect differences in communication with health professionals in home or residential care among GPs and PCNs working either exclusively in home care or in residential care only, and no significant differences were found.
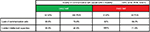
GP and PCN awareness of supportive tools, procedures, and agencies relevant to PDs
With regard to supportive tools, most GPs (n=34) and PCNs (n=484) reported being aware of adjustments and tools to improve the mobility of PDs (70.6% of GPs, 90.5% of PCNs). Little or no awareness was reported regarding communication aids: 41.2% of GPs and 54.9% of PCNs rated their awareness as inadequate, and 47.1% of GPs and 34.1% of PCNs rated it unaware (Table 5). Table 5 also illustrates how GPs and PCNs categorized their awareness of procedures and agencies relevant to PDs: 55.9% of GPs were adequately aware of the responsibilities of VAPH, 39.4% of PCNs were adequately aware of the (residential) care facilities in the region, 67.6% of GPs were inadequately unaware of procedures for admission in residential care facilities, and 66.9% of PCNs were inadequately aware of benefits PDs might be entitled to.
  | Table 5 Knowledge of tools, procedures, and agencies among GPs and PCNs Abbreviations: PCNs, primary-care nurses; PDs, people with disabilities; SMOG, Spreken met Ondersteuning van Gebaren. |
Discussion
The aim of this research was to examine the quality of communication of GPs and PCNs with different stakeholders in the care for PDs, as well as their awareness regarding practical and social issues in terms of tools, procedures, and agencies to support PDs in the management of their care. Findings of this study indicated self-reported communication of high quality of GPs and PCNs with their PDs and with care professionals in home and residential care. The awareness of supportive tools for PDs varied across the different domains: the most profoundly limited awareness concerned communication aids, in contrast to adjustments to enhance mobility of PDs, which are known to most GPs and PCNs. Regarding relevant procedures and agencies, GPs were most acquainted with the role of the agency authorized for the organization of welfare and health care targeting of PDs (VAPH), in contrast to PCNs, who most frequently reported being informed about (residential) care facilities in the region and their admission procedures.
Communicating with PDs and informal caregivers
A relatively small proportion of GPs and PCNs experienced difficulties when interacting with PDs. In the event of miscommunication, GPs and PCNs most frequently attributed this to limited intellectual capacities of their patients and seldom to a lack of tools to communicate. Remarkably, both GPs and PCNs reported being inadequately aware of tools to support PDs in their communication. However, it is unclear if this means that they did not know about the tools’ existence or were unaware of their availability to PDs. Research examining communication of GPs and PCNs with people with (intellectual) disabilities is limited. However, in a qualitative study performed by Wullink et al, needs regarding communication with people with an intellectual disability were compared to criteria used to train GPs on how to communicate with patients.40 PDs stated that they liked to be listened to and talked to by their GP (instead of talking to the informal caregiver); they also viewed the duration of consultation as too short, even though GPs often reserved twice the time of a regular consultation of 10 minutes to talk to them.40,41 A lack of time to communicate effectively with PDs is also a challenge for PCNs, which was demonstrated by Hemsley et al in a hospital setting.20,42 Experiences reported by these nurses were similar to those of GPs: taking time to communicate with PDs was most often compromised due to the workload of care professionals. These results were also underpinned by Mastebroek et al. Moreover, their findings highlighted the importance of a personal connection with care professionals.43 In order to enable PDs to engage in their care, primary-care professionals should invest in their therapeutic relationship with patients (with a disability).9,44,45
One way to facilitate or improve interaction with PDs is to be aware and use tools to support communication between care professionals and PDs.3,9,44,45 Publications that stipulate a series of tools designed for PDs to help them communicate include an Australian management book in which guidelines are formulated to support health care professionals in their interaction with people with (developmental) disabilities and a review by Lantman-de Valk and Walsh.3,46 Competent communication is an essential part of the therapeutic relationship. Therefore, tools to support communication can be considered a reasonable adjustment to make sure PDs can take part in decisions about their care.24 Because different kinds of communication deficits exist among PDs, communication should always be tailored. In a person-centered approach, communication aids to support PDs in the management of their care should thus be top of mind. As these tools improve the quality of a (medical) conversation, their use is not only beneficial for PDs and primary care professionals but also for informal caregivers, because they are often consulted or even requested to make decisions for PDs.
Being responsible for the management of care for PDs can result in burdening of informal caregivers: in accordance with previous research, the majority of GPs and PCNs in this study reported a burdening of at least half the informal caregivers.20,47 In their opinion, the two most frequent underlying causes were an overload of tasks and difficulties in finding suitable care. These findings indicate a reliance on informal care, as well as difficulties regarding accessibility of care services. Both professions reported being frequently in contact with informal caregivers. This could be an illustration of the complementarity of or tendency to (have to) rely on informal care, although it might also be a reflection of a good relationship with the informal, supportive network of PDs. These data should be interpreted prudently, as they voice GPs’ and PCNs’ opinions on problems experienced by informal caregivers. Consequently, it should not necessarily be surprising that only a limited number of GPs and PCNs adjudicated burdening to hamper (para)medical follow-up.
Communication with health care professionals
The majority of GPs and PCNs in this research perceived interdisciplinary communication with care professionals in both home care and residential care as (very) good, in contrast to other research.26 However, focusing on GPs and PCNs working exclusively in a home- or residential care setting, it is apparent that GPs’ communication with specialists was reported to be (very) bad. This result is an important indicator. However, it should be interpreted cautiously, as the larger percentages were based on a limited number of GPs. On a descriptive level, a slightly higher proportion of GPs communicated better with professionals in residential care than PCNs with home-care professionals. Differences in PDs residing more frequently in residential care facilities (GPs) or in a home-care setting (PCNs) is a possible explanation, as it enhances the likelihood of having (good) contact with professionals working in these respective settings, although no significant differences could be found. Remarkably, despite their communication with professionals in residential care facilities, GPs frequently reported being inadequately aware of the procedures involved in admission to residential care facilities, as opposed to PCNs, who reported adequate awareness. As the exchange of health care information is a prerequisite for high-quality care, the categorization of well-communicating health care professionals is promising.48–50
Collaboration, advice, referral
GPs’ and PCNs’ communication with PDs and their informal caregivers and health care professionals is important, as is the collaboration with care services and agencies specialized in care for PDs. In a more person-centered approach to health care, it is vital for GPs and PCNs that they are able to rely on a network of health care professionals.7,39 Moreover, they need to be aware of specialized agencies to which to refer PDs. Although primary-care professionals should, for instance, have a general awareness of measures to improve PDs’ quality of life, gaps in information can be bypassed when involved in a network of (specialized) care services and agencies. Consequently, the workload, which is inevitably affected by taking into account the needs of PDs, will be “shared” among all network members.32
In this study, for both GPs and PCNs, reported awareness of communication aids is problematic. As explained, being able to communicate is vital, as high-quality care requires insight into the needs of patients. However, both profession groups reported being adequately aware of measures to support PDs in their daily life (routines, being mobile, adjustments to their home). GPs reported being aware of the role of the agency specialized in the organization of care for PDs, which was not the case for PCNs: they were most frequently aware of care facilities in the region. These results illustrate how a multidisciplinary approach is beneficial to PDs: primary-care professionals might lack information on practical and social measures targeting PDs, but they can assume a coordinating role and make referrals to other care services and specialized agencies who have accurate information at their disposal.32,33
Previous research has shown that care professionals themselves value and would like to be more educated about collaboration with other services.51 Presumably, addressing PCNs’ inadequate knowledge on the responsibilities of VAPH will give them the opportunity to refer PDs to this organization. Indirectly, it can help PDs and informal caregivers navigate to the health care system and maybe steer them toward alternative care solutions. Consequently, this would reduce burdening of informal caregivers by targeting their search toward finding suitable care. Otherwise, as mentioned earlier, management of care is often shifted to informal caregivers, in particular when primary-care professionals’ communication with PDs is poor and informal caregivers are increasingly expected to make health care decisions for them, when interdisciplinary communication is poor, when there is no awareness of supportive measures for PDs, and when agencies specialized in the organization of care for PDs are unknown.39
Limitations
This study examined GPs’ and PCNs’ quality of communication with PDs and health care professionals. Moreover, it provided insight into GPs’ and PCNs’ awareness of supportive services relevant in the care of PDs. Because the questionnaire was developed based on expert opinion of a multidisciplinary team, it was only face-validated. This study has potential selection and response bias. It was based on a purposive sample in one Belgian region because of the access to all email addresses of these primary-care professionals. There is no indication that findings are specific for primary-care professionals employed in this region (as opposed to other Belgian areas) or relate to delivering care to a certain subsection of PDs. These hypotheses were not explored; therefore, findings should be interpreted cautiously. Although the sample size of GPs was small, valuable information was able to be collected from the PCNs. The primary goal was not to generalize findings, although to some extent this would probably be justified, as certain needs reported in this research were similar to previous studies.29,30 The questionnaire was distributed broadly in the targeted region. Response bias can be presumed, particularly for GPs, when only those with a specific interest participated, eg, those who frequently encounter problems in their care for PDs or who feel inexperienced. Results should be interpreted prudently, because of the lack of data from nonrespondents.
Recommendations
In order to meet the needs of PDs and their informal caregivers, primary-care professionals should be aware of the importance of being involved in a network of care services and specialized agencies. Although clinical knowledge prevails in their prequalification training, being informed about measures improving PDs’ quality of life is beneficial, in particular for this population.52 As PDs might be at greater risk of experiencing difficulties navigating through the health care system than the general population, both GPs and PCNs have a key role in giving advice and making referrals to other care professionals, as well as specialized agencies.1–3 As information regarding tools to support PDs and benefits PDs are entitled to is dynamic and changes over time, the focus should be on how to be up to date or how to organize a multidisciplinary network. A first step to achieve both would be to keep every stakeholder in the loop, thus sharing information. When documentation is being integrated, interprofessional collaboration is within reach. In order to exchange information successfully, all stakeholders should be onboard and there should be consensus about the medium to facilitate the exchange. Moreover, the tool enabling the flow of information should be adapted to all stakeholders’ working routines.53,54 However, sharing information face to face (or orally) and being part of a team are other prerequisites that should not be overlooked.
The development of multidisciplinary, on-the-job training to tackle common, everyday challenges primary-care professionals come across in their care for PDs should be explored.55 It is feasible to design a training package that can be deployed in different settings and for different health care professions, as has been demonstrated in a review by Hemm et al.56 Zooming in on future primary-care professionals, prequalification training could be reorganized. A program could be developed in resemblance of a project by Bollard et al, exposing (mental health) nurses to PDs by involving them in nursing education. This has been shown to be beneficial, as students improved their knowledge of disabilities, as well as their understanding of the need for different ways to communicate with PDs.57 An alternative approach is teaching students from the point of view of service users and their experiences in trying to get access to necessary health care, which might also be an innovative and intriguing way to educate health care professionals.58
In general, these educational programs will have to integrate knowledge, skills, and attitudes to turn out equipped primary-care professionals. In particular, topics regarding mental health should be included: it not only influences PDs’ physical state but also can shed light on the underlying mechanisms of what is perceived as “challenging behavior”.59–62 Besides disseminating knowledge, care professionals should have the opportunity to practice. Important skills to be acquired would be those regarding interpersonal communication, with a specific and extensive focus on doctor–patient communication and relationship (trust) building with PDs.
Although delivering care to PDs can be very challenging, it also allows care professionals to be creative: to meet the needs of PDs, a “one size fits all” approach is not feasible. Instead, person-centered care with tailored interventions will be necessary.
Conclusion
Both GPs and PCNs self-reported the quality of their communication with PDs as good. However, these primary-care professionals’ lack of awareness of tools to support communication is problematic. Being involved in a multidisciplinary network seems vital for both these professional groups, given their inadequate awareness of practical and social support measures, procedures, and specialized agencies relevant to PDs.
Disclosure
The authors report no conflicts of interest in this work.
References
Lennox TN, Nadkarni J, Moffat P, Robertson C. Access to services and meeting the needs of people with learning disabilities. J Learn Disabil. 2003;7(1):34–50. | ||
Emerson E, Baines S, Allerton L, Welch V. Health inequalities and people with learning disabilities in the UK: 2012. 2012. Available from: http://webarchive.nationalarchives.gov.uk/20160704153108/http://www.improvinghealthandlives.org.uk/securefiles/160704_1635//IHAL%202012-11%20Health%20Inequalities_r1.pdf. Accessed August 14, 2017. | ||
Lantman-de Valk HM, Walsh PN. Managing health problems in people with intellectual disabilities. BMJ. 2008;337(7683):1408–1412. | ||
United Nations. Convention on the Rights of Persons with Disabilities. New York: UN; 2006. | ||
Reichard A, Stolzle H, Fox MH. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disabil Health J. 2011;4(2):59–67. | ||
World Health Organization. World Report on Disability. Geneva: WHO; 2011. | ||
Sullivan WF, Berg JM, Bradley E, et al. Primary care of adults with developmental disabilities: Canadian consensus guidelines. Can Fam Physician. 2011;57:541–553. | ||
de Winter CF, Bastiaanse LP, Hilgenkamp TI, Evenhuis HM, Echteld MA. Overweight and obesity in older people with intellectual disability. Res Dev Disabil. 2012;33(2):398–405. | ||
Kerr M, Fraser W, Felce D. Primary health care for people with a learning disability: a keynote review. Br J Learn Disabil. 1996;24(1):2–8. | ||
Doostan D, Wilkes M. Evidence-based case review: treating the developmentally disabled. West J Med. 1999;171(2):92–96. | ||
Vlaams Agentschap voor Personen met een Handicap [website on the Internet]. The Flemish agency for people with a disability (VAPH). Available from: http://www.vaph.be/vlafo/view/nl/204713-en.html. Accessed September 25, 2015. | ||
Vlaams Agentschap voor Personen met een Handicap. Zorgregierapport: gegevens 31 December 2014 – tweede jaarhelft 2014. 2014. Available from: https://www.vaph.be/sites/default/files/documents/zorgregierapport-31-december-2014/zorgregierapport_2014-12-31.pdf. Dutch. Accessed August 14, 2017. | ||
Federale Overheidsdienst Sociale Zekerheid. Jaarverslag 2014 – In goede handen: DG personen met een handicap. 2014. Available from: http://handicap.belgium.be/docs/nl/jaarverslag-2014.pdf. Dutch. Accessed August 14, 2017. | ||
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. | ||
Starfield B. Primary care: an increasingly important contributor to effectiveness, equity, and efficiency of health services: SESPAS report 2012. Gac Sanit. 2012;26 Suppl 1:20–26. | ||
Maes B, Broekman TG, Došen A, Nauts J. Caregiving burden of families looking after persons with intellectual disability and behavioural or psychiatric problems. J Intellect Disabil Res. 2003;47(Pt 6):447–455. | ||
Carretero S, Garcés J, Ródenas F, Sanjosé V. The informal caregiver’s burden of dependent people: theory and empirical review. Arch Gerontol Geriatr. 2009;49(1):74–79. | ||
Harkness KI, Tranmer JE. Measurement of the caregiving experience in caregivers of persons living with heart failure: a review of current instruments. J Card Fail. 2007;13(7):577–587. | ||
Snyder B, Keefe K. The unmet needs of family caregivers for frail and disabled adults. Soc Work Health Care. 1985;10(3):1–14. | ||
Reinhard SC, Given B, Petlick NH, Bemis A. Supporting family caregivers in providing care. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality; 2008. | ||
Scottish Government. Strengthening the Commitment: The Report of the UK Modernising Learning Disabilities Nursing Review. Edinburgh: Scottish Government; 2012. | ||
McGrath A. Annual health checks for people with learning disabilities. Nurs Stand. 2010;24(50):35–40. | ||
Scheepers M, Kerr M, O’Hara D, et al. Reducing health disparity in people with intellectual disabilities: a report from Health Issues Special Interest Research Group of the International Association for the Scientific Study of Intellectual Disabilities. J Policy Pract Intellect Disabil. 2005;2(3–4):249–255. | ||
MacArthur J, Brown M, McKechanie A, Mack S, Hayes M, Fletcher J. Making reasonable and achievable adjustments: the contributions of learning disability liaison nurses in “getting it right” for people with learning disabilities receiving general hospitals care. J Adv Nurs. 2015;71(7):1552–1563. | ||
Claes N, Storms H, Moermans V. Care, communication and educational needs of primary care nurses to treat disabled patients. J Nurs Educ Pract. 2016;6(7):109–115. | ||
Lennox N, Diggens J, Ugoni A. The general practice care of people with intellectual disability: barriers and solutions. J Intellect Disabil Res. 1997;41(5):380–390. | ||
Baxter H, Lowe K, Houston H, Jones G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J Gen Pract. 2006;56(523):93–98. | ||
Lennox N, Van Driel ML, van Dooren K. Supporting primary healthcare professionals to care for people with intellectual disability: a research agenda. J Appl Res Intellect Disabil. 2015;28(1):33–42. | ||
Wilkinson J, Dreyfus D, Cerreto M, Bokhour B. “Sometimes I feel overwhelmed”: educational needs of family physicians caring for people with intellectual disability. Intellect Dev Disabil. 2012;50(3):243–250. | ||
McDermott S, Moran R, Platt T, Dasari S. Variation in health conditions among groups of adults with disabilities in primary care. J Community Health. 2006;31(3):147–159. | ||
Yee S, Breslin ML. Achieving accessible health care for people with disabilities: why the ADA is only part of the solution. Disabil Health J. 2010;3(4):253–261. | ||
McColl MA, Forster D, Shortt SE, et al. Physician experiences providing primary care to people with disabilities. Healthc Policy. 2008;4(1):e129–e147. | ||
Esbensen AJ. Families of individuals with intellectual disability and comorbid mental health problems. J Ment Health Res Intellect Disabil. 2011;4(3):140–157. | ||
Kripalini S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. | ||
Claes N, Nele J, van Mierlo J. The implementation costs of an electronic prevention programme in Belgian general practice. Eur J Gen Pract. 2010;16(1):12–17. | ||
Geurts MM, Talsma J, Brouwers JR, de Gier JJ. Medication review and reconciliation with cooperation between pharmacist and general practitioner and the benefit for the patient: a systematic review. Br J Clin Pharmacol. 2012;74(1):16–33. | ||
Mastebroek M, Naaldenberg J, Lagro-Janssen AL, Lantman-de Valk HM. Health information exchange in general practice care for people with intellectual disabilities: a qualitative review of the literature. Res Dev Disabil. 2014;35(9):1978–1987. | ||
Jabbla. Tellus 5. Available from: http://www.jabbla.com/products.asp?itemID=10. Accessed August 14, 2017. | ||
Butters A, Webster M, Hill M. Literature Review: Understanding the Needs of People with Mental Health Conditions and/or Learning Disabilities and the Implications for the Pension, Disability and Carers Service. London: Department for Work and Pensions; 2010. | ||
Wullink M, Veldhuijzen W, Lantman-de Valk HM, Metsemakers JF, Dinant GJ. Doctor-patient communication with people with intellectual disability: a qualitative study. BMC Fam Pract. 2009;10:82. | ||
Morrison EH, George V, Mosqueda L. Primary care for adults with physical disabilities: perceptions from consumer and provider focus groups. Fam Med. 2008;40(9):645–651. | ||
Hemsley B, Balandin S, Worrall L. Nursing the patient with complex communication needs: time as a barrier and a facilitator to successful communication in hospital. J Adv Nurs. 2012;68(1):116–126. | ||
Mastebroek M, Naaldenberg J, Mareeuw FA, Lagro-Janssen AL, Lantman-de Valk HM. Experiences of patients with intellectual disabilities and carers in GP health information exchanges: a qualitative study. Fam Pract. 2016;33(5):543–550. | ||
Chant S, Jenkinson T, Randle J, Russell G. Communication skills: some problems in nursing education and practice. J Clin Nurs. 2002;11(1):12–21. | ||
Olney MF. Communication strategies of adults with severe disabilities: supporting self-determination. Rehabil Couns Bull. 2001;44(2):87–94. | ||
Australian Government. Communicating with People with Disability: National Guidelines for Emergency Managers. Canberra: Australian Emergency Management Institute; 2013. | ||
Vecchio N, Cybinski P, Stevens S. The effect of disability on the needs of caregivers. Int J Soc Econ. 2009;36(7):782–796. | ||
Elliott RA, Tran T, Taylor SE, et al. Gaps in continuity of medication management during the transition from hospital to residential care: an observational study (MedGap study). Australas J Ageing. 2012;31(4):247–254. | ||
Paulus D, Van den Heede K, Mertens R. Organisation of care for chronic patients in Belgium: development of a position paper. 2012. Available from: https://kce.fgov.be/sites/default/files/page_documents/KCE_190C_organisation_care_chronic_patients_0.pdf. Accessed August 14, 2017. | ||
Gröne O, Garcia-Barbero M. Integrated care: a position paper of the WHO European office for integrated health care services. Int J Integr Care. 2001;1:e21. | ||
Phillips A, Morrison J, Davis R. General practitioners’ educational needs in intellectual disability health. J Intellect Disabil Res. 2004;48(2):142–149. | ||
Hahn JE. Addressing the need for education: curriculum development for nurses about intellectual and developmental disabilities. Nurs Clin North Am. 2003;38(2):185–204. | ||
Atwal A, Caldwell K. Do multidisciplinary integrated care pathways improve interprofessional collaboration? Scand J Caring Sci. 2002;16(4):360–367. | ||
Storms H, Marquet K, Nelissen K, et al. Implementing an electronic medication overview in Belgium. BMC Res Notes. 2014;7:915. | ||
Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008;(1):CD002213. | ||
Hemm C, Dagnan D, Meyer TD. Identifying training needs for mainstream healthcare professionals, to prepare them for working with individuals with intellectual disabilities: a systematic review. J Appl Res Intellect Disabil. 2015;28(2):98–110. | ||
Bollard M, Lahiff J, Parkes N. Involving people with learning disabilities in nurse education: towards an inclusive approach. Nurse Educ Today. 2012;32(2):173–177. | ||
Smith P, Ooms A, Marks-Maran D. Active involvement of learning disabilities service users in the development and delivery of a teaching session to pre-registration nurses: students’ perspectives. Nurse Educ Pract. 2016;16(1):111–118. | ||
Phelan M, Stradins L, Morrison S. Physical health of people with severe mental illness. BMJ. 2001;322(7284):443–444. | ||
World Health Organization. Integrating Mental Health into Primary Care: A Global Perspective. Geneva: WHO;2008. | ||
Kerwick S, Jones R, Mann A, Goldberg D. Mental health care training priorities in general practice. Br J Gen Pract. 1997;47(417):225–227. | ||
McConkey R, Truesdale M. Reactions of nurses and therapists in mainstream health services to contact with people who have learning disabilities. J Adv Nurs. 2000;32(1):158–163. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
