Back to Journals » Cancer Management and Research » Volume 15
Gender Differences in Symptom Burden, Functional Performance and Global Quality of Life of Lung Cancer Patients Receiving Inpatient versus Outpatient Treatment
Authors Koch M, Rothammer T, Rasch F, Müller K, Braess J, Koller M, Schulz C
Received 14 November 2022
Accepted for publication 1 February 2023
Published 21 February 2023 Volume 2023:15 Pages 175—183
DOI https://doi.org/10.2147/CMAR.S397198
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Seema Singh
Myriam Koch,1 Tobias Rothammer,1 Frederike Rasch,1 Karolina Müller,2 Jan Braess,3 Michael Koller,2 Christian Schulz1
1Department of Internal Medicine 2, University Hospital Regensburg, Regensburg, Germany; 2Center for Clinical Studies, University Hospital Regensburg, Regensburg, Germany; 3Clinic for Oncology and Hematology, Hospital Barmherzige Brüder, Regensburg, Germany
Correspondence: Myriam Koch, Klinik und Poliklinik für Innere Medizin II, Universitätsklinikum Regensburg, Franz-Josef-Strauß Allee 11, Regensburg, D-93053, Germany, Tel +49 941 9440, Email [email protected]
Background: Lung cancer may cause severe impairment of quality of life. An increasing number of lung cancer patients are receiving outpatient chemotherapy. However, little is known about gender aspects in the areas of impaired QoL in outpatient versus inpatient lung cancer patients. The aim of the study was to investigate this.
Methods: We report from a prospective, multicenter study to analyze the EORTC QLQ-LC29, a new designed module to assess the QoL of lung cancer patients. The participants filled out the EORTC QLQ-C30 and the recently updated lung cancer module QLQ-LC29.
Results: A total of 198 lung cancer patients (73 female and 125 male, mean 64.5 age years) during first-line therapy were enrolled in this study by completing the both questionnaires. Women showed higher symptom scores, when being inpatient. Significant results were found regarding nausea/vomiting (mean women = 17.6 and mean men = 9.3, p = 0.037) and hair loss (mean women = 40.0 and mean men = 21.7, p = 0.010), although women received fewer chemotherapy treatments than their male counterparts (women n = 47, 64.4% and men n = 86, 68.8%). When it comes to global QoL, men report a significant worse QoL than women (mean women = 57.5 and mean men = 46.1, p = 0.016), when being inpatient. As outpatients, men report significant results regarding sore mouth and tongue (mean women = 1.2 and mean men = 13.5, p = 0.012).
Conclusion: This study adds to the literature in showing the typical gender difference effect on QoL, suggesting men suffer less than women, is not a universal phenomenon irrespective of being inpatient or outpatient. It also confirms the hypothesis that the symptom burden is higher with inpatients than outpatients.
Keywords: gender differences, lung cancer, quality of life, EORTC QLQ-C30/EORTC QLQ-LC29, outpatient versus inpatient treatment
Introduction
Lung cancer, a life-threatening disease, is worldwide one of the most leading cancer type for women and men.1–5 Patients suffer from numerous symptoms, which result in impaired quality of life (QoL).4,6 New therapies with a positive impact on overall survival are introduced with high dynamics in the field of lung cancer. With a longer overall survival, quality of life becomes an even more important issue in this life threatening disease.
An increasing number of lung cancer patients are receiving outpatient chemotherapy treatment.7 By comparing out- and inpatients, inpatients suffer more from symptoms than outpatients as could be shown in a German study in 4020 cancer patients.8 However, further studies were not able to confirm these results.7
Another current topic in lung cancer patients is gender aspects according to various studies.1,2,9 The number of female patients has risen due to changes in smoking habits, the leading risk factor for lung cancer.10 But women face not only a rising incidence, they are also more likely than men to develop adenocarcinoma of the lung.1,9,11 Furthermore, relevant mutations like TP53 have been found more frequently in female patients and women respond differently to various therapies in NSCLC with benefits in overall survival.1,11,12 Women, for example, respond better to pembrolizumab combined with chemotherapy treatment than men.13 In contrast, men better respond to immunotherapy with Pembrolizumab than women.14 When it comes to QoL women, in large-scale Dutch, German, Norwegian and Swedish studies, consistently showed a higher symptom burden and lower levels of QoL than men by means of the EORTC (European Organization for Research and Treatment of Cancer) QLQ-C30, a well-established questionnaire used to assess QoL of cancer patients in oncological trials.15–21 In contrast an international, multicenter study on lung cancer patients of any tumor stage, using the QLQ-C30 questionnaire and the recently updated lung cancer-specific module the QLQ-LC29, could not find any relevant gender difference regarding QoL.22–24
The goal of the present project was, to use the EORTC QLQ-C30 plus the QLQ-LC29 in a cohort of lung cancer patients and to investigate gender aspects in the areas of QoL in lung cancer patients treated as inpatient or outpatients, because to our knowledge this is the first study examining this issue.
Method
Study Design
The current report is based on a prospective, multicenter study to analyze the EORTC QLQ-LC29, a new designed module to assess the QoL of lung cancer patients. The study recruitment for this satellite project took place from October 2019 to February 2021 at the University Hospital Regensburg and the Hospital Barmherzige Brüder in Regensburg.
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was registered with the Deutsches Register Klinischer Studien – DRKS (https://drks.de/drks_web/setLocale_EN.do) (reference number DRKS00023355). Approval from the Ethical Committee of the University of Regensburg was obtained (reference number 19–1418-101).
Patients
The following eligibility criteria applied: histologically proven non-small cell lung cancer (NCSLC) or small cell lung cancer (SCLC) during first-line therapy, 18 years of age or older, no other previous or recurrent tumor, ability to fill in a questionnaire and written informed consent. Patients were excluded from the study if any of the above criteria were not fulfilled.
Procedure
Before participation, inpatients and outpatients were informed about the study. After providing written informed consent, patients filled out the paper-and-pencil version of the EORTC QLQ-C30 and the recently updated lung cancer module QLQ-LC29. Tumor histology, age, comorbidities and therapies were collected from the medical records.
Questionnaires
The EORTC QLQ-C30 (version 3.0), a questionnaire designed for the use in international clinical trials for cancer patients of any tumor type, consists of 15 scales: five multi-item function scales (emotional, cognitive, social, physical and role functioning), three multi-item symptom scales (nausea, fatigue, pain), five single items (appetite loss, diarrhea, constipation, insomnia, dyspnea) and one two-item scale to assess global quality of life. Items are accompanied by four-item Likert scales with the response options labeled (1)” not at all”, (2) “a little”, (3) “quite a bit” and (4) “very much”. The two global QoL items are to be completed using a seven-item Likert scale (1 = very bad to 7 = very good). According to the EORTC scoring manual, all scores are subjected to linear transformation and are presented on scales ranging from 0 to 100. In the case of functional scores, a high score denotes good functioning, whereas a high score in symptom scales denotes for a high symptom burden.
The updated EORTC lung cancer module consists of 29 items. According to the calling results of the Phase 3 study, it consists of five multi-item symptom scales (coughing, shortness of breath, side effects, fear of progression, surgery-related symptoms) and five single-item scales (coughing blood, pain in the chest, pain in the shoulder, bodily pain, problems with weight loss).
Statistical Analyses
Basic descriptive statistics included counts, percentages, medians/ranges, and means and confidence intervals.
Gender differences in all QoL aspects were analyzed using univariate (t-test) and multivariable (analyses of covariance, ANCOVA) models. ANCOVAs were adjusted for the following covariates: age, gender, tumor type (NSCLC vs SCLC), stage (NSCLC stage IV vs other stages) comorbidity (yes/no) and administration site (inpatient/outpatient). Estimated marginal means with corresponding 95%-confidence intervals were presented as effect estimates. A p-value <0.05 was considered to be the threshold of statistical significance. Due to the exploratory nature of all analyses, corrections for alpha-error were not applied.
The smallest difference a patient recognizes as an important change in QoL without being of significant value is defined as the minimal important difference (MID).25 In oncological trials, MIDs help to interpret quality of life scores.25 A study on patients with breast cancer and small-cell lung cancer suggested that changes in scores more than 20 represent a large difference, a change of 10–20 represents a moderate difference and a score of 5–10 represent a small difference by means of a subjective significance questionnaire and the QLQ-C30 questionnaire.26 In accordance with that study, we defined in our study changes in scores of ≥ 5 as representing a perceivable and clinically important difference with respect to cancer-related changes in QoL.
All analyses were performed using the software packages SPSS Statistics 23.0 (IBM Corporation, Armonk, NY, USA) and SAS 9.4 (SAS Institute, Cary, NC, USA).
Results
Patient Characteristics
A total of 198 patients (73 female and 125 male) were enrolled (Table 1). Median age was 64.5 years. Non-small cell lung cancer was the predominant histological type (SCLC n = 48, 24.2% vs NSCLC n = 150, 75.8%). A total of 167 patients suffered from comorbidities (84.3%). Table 2 shows the administered first-line therapies.
 |
Table 1 Baseline Characteristics |
 |
Table 2 First-Line Therapy |
Gender Differences Regarding Functional and Symptom Scores
Table 3 presents the estimated marginal means (EMM) of QoL for women and men and the respective p-values.
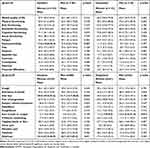 |
Table 3 Estimated Marginal Means of the EORTC QLQ-C30 and the QLQ-LC29 |
Figure 1 shows cumulated symptom scores of women and men by comparing outpatient and inpatient (median women outpatient = 691.67, median women inpatient = 905.56 and median men outpatient = 638.89, median men inpatient = 747.22). Women show higher symptom scores, when being inpatient. Significant results were found regarding nausea/vomiting (mean women = 17.6 and mean men = 9.3, p = 0.037) hair loss (mean women = 40.0 and mean men = 21.7, p = 0.010) and dizziness (mean women = 32.4 and mean men = 22.7, p = 0.01).
Figure 2 shows cumulated function scores of women and men by comparing outpatient and inpatient (median women outpatient = 340.83, median women inpatient = 270 and median men outpatient = 323.75, median men inpatient = 320). Women show lower functional scores when being inpatient, significantly in physical functioning (women inpatient = 60.0, women outpatient = 78.2, p-value = 0.001) and role functioning (women inpatient = 49.2, women outpatient = 65.8, p-value=0.034).
When it comes to global QoL, men report a poorer quality of life compared to women (mean women = 57.5 and mean men = 46.1, p = 0.016) when being treated as an inpatient (Figure 3). Furthermore, male inpatients have a significantly worse QoL than male outpatients (p < 0.001). As outpatients, men reported a significantly higher symptom burden with respect to sore mouth and tongue (mean women = 1.2 and mean men = 13.5, p = 0.012).
Based on descriptive analytics minimal important differences in the inpatient group were found in role functioning (mean women = 49.2, mean men = 54.7, p-value = 0.419), pain (mean women = 29.0, mean men = 35.6, p-value = 0.328) and financial difficulties (mean women = 16.9, mean men = 24.3, p-value= 0.248), insomnia (mean women = 42.1, mean men = 36.4, p-value = 0.435). The three largest minimal important differences in the outpatient group were found in hair loss (mean women = 44.9, mean men = 37.2, p-value = 0.288), fear of progression (mean women = 60.8, mean men = 49.3, p-value = 0.104) and shoulder pain (mean women = 28.8, mean men = 18.0 and p-value = 0.111). For more details see Table 1.
Discussion
Gender differences have been a subject of many analyses in QoL research.15–21 Based on the hypothesis that gender differences in QoL of lung cancer patients depend on the treatment conditions as an outpatient or inpatient, we conducted this study.
Our study clearly proves that inpatients suffered more symptoms than outpatients independent of gender. Moreover, the function scales show higher scores for outpatients than for inpatients, also independent of gender. This expresses that the therapy conditions have a decisive influence on the quality of life of lung cancer patients, whereby this observation applies to both genders. This is in line with another German study on 4020 cancer patients demonstrating that inpatients report the biggest impairments of QoL.8 However, another study on outpatient versus inpatient lung cancer patients prior to hospital discharge came to the conclusion that quality of life was not significantly different and better physical, social and emotional well-being before discharge were signs for better QoL during outpatient chemotherapy treatment.7
We observed three statistically significant and clinically important differences to the disadvantage of women (nausea/vomiting, hair loss and dizziness) as inpatients. Nausea/vomiting and alopecia are common side effects of lung cancer patients treated with chemotherapy, which worsens quality of life.5,27 When compared to the EORTC reference sample of lung cancer patients,19 our inpatients report similar impaired symptom scores for nausea/vomiting as inpatients. This is in line with two other Canadian studies, demonstrating that women with advanced cancer face significantly more nausea than men.28,29
The present study underlines that women suffer more from alopecia which most likely can be explained by the fact that women care more about their appearance than men. In our cohort, women received fewer chemotherapy treatments than their male counterparts. This means that differences in the quality of life between genders cannot be explained by a higher intensity of therapy in women.
In contrast to the inpatients, we observed only one significant difference in QoL in outpatients with lung cancer (sore mouth or throat) to the disadvantage of men, which is a well-known side effect of chemotherapy that deteriorates QoL.27 This is well explained by the higher amount of chemotherapy treatment given to the male participants in the present study.
Although women suffered more from symptoms when being inpatient in our study, men reported significantly worse global QoL. This is a striking finding since an investigation on the QoL of the general German population as well as an investigation of the general Norwegian population using the EORTC QLQ-C30 showed men reporting consistently better QoL than women.15,18 This may be due to the observation that men have more problems with the diagnosis itself than with cancer associated symptoms. However, since a significantly worse QoL could only be found in male inpatients, it could be an effect of hospitalization. But when it comes to the MIDs, the inpatient study group shows the largest MIDs in financial difficulties, pain and insomnia, with a higher symptom burden in men concerning financial difficulties and pain. Male cancer patients more often face financial difficulties because they are usually the main breadwinners for their families.30 Financial difficulties themselves can result in worse global QoL, an explanation for the worse QoL of men despite fewer symptoms.
Limitations
The present analysis has several limitations. First of all, it has only a small number of participants. Second, experience suggests that patients with advanced stages are less likely to complete questionnaires. Hence, the present sample may be biased toward a better performance status. Furthermore, the study has a disproportion in participation of women and men.
Conclusion
This study confirms the hypothesis that the symptom burden is higher with inpatients than outpatients. It also adds to the literature in showing the typical gender difference effect on QoL, suggesting that men suffer less than women, is not a universal phenomenon irrespective of being inpatient or outpatient.
Abbreviations
EORTC, European Organization for Research and Treatment of Cancer; MID, minimal important difference; N, number; NSCLC, non-small cell lung cancer; QoL, Quality of life; SCLC, small cell lung cancer; UICC, Union for International Cancer Control.
Data Sharing Statement
Dr. Myriam Koch will respond to data sharing requests under the premise that an adequate research question is formulated. Original anonymized data will be made available up to one year after the publication of the paper.
Disclosure
Dr. Myriam Koch, Tobias Rothammer, Frederike Rasch, Karolina Müller, Prof. Dr. Jan Braess and Prof. Dr. Christian Schulz have nothing to disclose. Prof. Dr. Michael Koller reports a grant from EORTC (Reference number: Koller Lung 03/2016).
References
1. Ulas A, Tokluoglu S, Kos M, et al. Lung cancer in women, a different disease, survival differences by sex in Turkey. Asian Pac J Cancer. 2015;16(2):815–822.
2. Kim HR, Kim SY, Kim CH, et al. Sex-specific incidence of EGFR mutation and its association with age and obesity in lung adenocarcinomas, a retrospective analysis. J Cancer Res Clin Oncol. 2017;143(11):2283–2290. doi:10.1007/s00432-017-2473-8
3. Rauma V, Salo J, Sintonen H, Rasanen J, Ilonen I. Patient features predicting long-term survival and health-related quality of life after radical surgery for non-small cell lung cancer. Thoracic Cancer. 2016;7(3):333–339. doi:10.1111/1759-7714.12333
4. Larsson M, Ljung L, Johansson BB. Health-related quality of life in advanced non-small cell lung cancer, correlates and comparisons to normative data. Eur J Cancer Care. 2012;21(5):642–649. doi:10.1111/j.1365-2354.2012.01346.x
5. de Oliveira PI, Pereira CA, Belasco AG, Bettencourt AR. Comparison of the quality of life among persons with lung cancer, before and after the chemotherapy treatment. Rev Lat Am Enfermagem. 2013;21(3):787–794. doi:10.1590/S0104-11692013000300019
6. Wang B, Hao N, Zhang X. Factors influencing the psychology and quality of life in lung cancer patients. Saudi Med J. 2017;38(9):948–951. doi:10.15537/smj.2017.9.18532
7. Matsuda A, Kobayashi M, Sakakibara Y, et al. Quality of life of lung cancer patients receiving outpatient chemotherapy. Exp Ther Med. 2011;2(2):291–294. doi:10.3892/etm.2011.185
8. Hinz A, Weis J, Faller H, et al. Quality of life in cancer patients-a comparison of inpatient, outpatient, and rehabilitation settings. Support Thorac Cancer Ther. 2018;26(10):3533–3541. doi:10.1007/s00520-018-4211-4
9. Sakurai H, Asamura H, Goya T, et al. Survival differences by gender for resected non-small cell lung cancer, a retrospective analysis of 12,509 cases in a Japanese Lung Cancer Registry study. J Thorac Oncol. 2010;5(10):1594–1601. doi:10.1097/JTO.0b013e3181f1923b
10. Tolwin Y, Gillis R, Peled N. Gender and lung cancer-SEER-based analysis. Ann Epidemiol. 2020;46:14–19. doi:10.1016/j.annepidem.2020.04.003
11. Stapelfeld C, Dammann C, Maser E. Sex-specificity in lung cancer risk. Int J Cancer. 2020;146(9):2376–2382. doi:10.1002/ijc.32716
12. Pinto JA, Vallejos CS, Raez LE, et al. Gender and outcomes in non-small cell lung cancer, an old prognostic variable comes back for targeted therapy and immunotherapy? ESMO open. 2018;3(3):e000344. doi:10.1136/esmoopen-2018-000344
13. Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–2092. doi:10.1056/NEJMoa1801005
14. Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–1833. doi:10.1056/NEJMoa1606774
15. Schwarz R, Hinz A. Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer. 2001;37(11):1345–1351. doi:10.1016/S0959-8049(00)00447-0
16. Hinz A, Singer S, Brahler E. European reference values for the quality of life questionnaire EORTC QLQ-C30, Results of a German investigation and a summarizing analysis of six European general population normative studies. Acta oncologica. 2014;53(7):958–965. doi:10.3109/0284186X.2013.879998
17. Waldmann A, Schubert D, Katalinic A. Normative data of the EORTC QLQ-C30 for the German population, a population-based survey. PLoS One. 2013;8(9):e74149. doi:10.1371/journal.pone.0074149
18. Hjermstad MJ, Fayers PM, Bjordal K, Kaasa S. Health-related quality of life in the general Norwegian population assessed by the European Organization for research and treatment of cancer core quality-of-life questionnaire, the QLQ=C30 (+ 3). J Clin Oncol. 1998;16(3):1188–1196. doi:10.1200/JCO.1998.16.3.1188
19. Scott Neil WFPM, Aaronson Neil K, Andrew B, et al. Spangers Mirjam AG on behalf of the EORTC quality of life group. EORTC QLQ-C30 Reference Values; 2008.
20. Derogar M, van der Schaaf M, Lagergren P. Reference values for the EORTC QLQ-C30 quality of life questionnaire in a random sample of the Swedish population. Acta oncologica. 2012;51(1):10–16. doi:10.3109/0284186X.2011.614636
21. van de Poll-Franse LV, Mols F, Gundy CM, et al. Normative data for the EORTC QLQ-C30 and EORTC-sexuality items in the general Dutch population. Eur J Cancer. 2011;47(5):667–675. doi:10.1016/j.ejca.2010.11.004
22. Koch M, Hjermstad MJ, Tomaszewski K, et al. Gender effects on quality of life and symptom burden in patients with lung cancer, results from a prospective, cross-cultural, multi-center study. J Thorac Dis. 2020;12(8):4253–4261. doi:10.21037/jtd-20-1054
23. Koller M, Hjermstad MJ, Tomaszewski KA, et al. An international study to revise the EORTC questionnaire for assessing quality of life in lung cancer patients. Ann Oncol. 2017;28(11):2874–2881. doi:10.1093/annonc/mdx453
24. Koller M, Warncke S, Hjermstad MJ, et al. Use of the lung cancer-specific Quality of Life Questionnaire EORTC QLQ-LC13 in clinical trials, A systematic review of the literature 20 years after its development. Cancer. 2015;121(24):4300–4323. doi:10.1002/cncr.29682
25. Maringwa JT, Quinten C, King M, et al. Minimal important differences for interpreting health-related quality of life scores from the EORTC QLQ-C30 in lung cancer patients participating in randomized controlled trials. Support Thorac Cancer Ther. 2011;19(11):1753–1760. doi:10.1007/s00520-010-1016-5
26. Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16(1):139–144. doi:10.1200/JCO.1998.16.1.139
27. Daroszewski C, Stasiewicz M, Jaźwińska-Tarnawska E, et al. Quality of life in patients with advanced non-small-cell lung cancer receiving palliative Chemotherapy. Adv Exp Med Biol. 2019;1160:11–18.
28. Cheung WY, Le LW, Gagliese L, Zimmermann C. Age and gender differences in symptom intensity and symptom clusters among patients with metastatic cancer. Support Thorac Cancer Ther. 2011;19(3):417–423. doi:10.1007/s00520-010-0865-2
29. Chow S, Ding K, Wan BA, et al. Gender differences in pain and patient reported outcomes, a secondary analysis of the NCIC CTG SC. 23 randomized trial. Ann Palliat Med. 2017;6(Suppl 2):S185–S194. doi:10.21037/apm.2017.08.12
30. Syse A, Tretli S, Kravdal O. The impact of cancer on spouses’ labor earnings, a population-based study. Cancer. 2009;115(18 Suppl):4350–4361. doi:10.1002/cncr.24582
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.