Back to Journals » International Journal of General Medicine » Volume 15
Gender Differences in Prolonged Mechanical Ventilation Patients – A Retrospective Observational Study
Authors Huang C
Received 5 April 2022
Accepted for publication 7 June 2022
Published 14 June 2022 Volume 2022:15 Pages 5615—5626
DOI https://doi.org/10.2147/IJGM.S368881
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chienhsiu Huang
Department of Internal Medicine, Division of Chest Medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chiayi County, Taiwan
Correspondence: Chienhsiu Huang, Department of Internal medicine, Division of Chest medicine, Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Chiayi County, Taiwan, Tel +886-9-21552418, Email [email protected]; [email protected]
Background: The gender differences in patients requiring prolonged mechanical ventilation are not understood. We investigated the effects of gender differences in terms of age, causes of respiratory failure, discharge status, successful weaning, mortality rate and long-term survival outcomes in patients receiving prolonged mechanical ventilation.
Methods: We conducted a six-year retrospective study of patients requiring prolonged mechanical ventilation. Survival curves for all patients requiring prolonged mechanical ventilation and those who were very old (aged ≥ 80 years) were compared based on gender.
Results: Among the 574 patients enrolled. There was no statistically significant difference between male and female patients regarding successful weaning, ventilator dependence, or in-hospital mortality. We gathered long-term follow-up data on 296 patients, including 70 very old male patients and 41 very old female patients. The 6-month, 3-year, and 5-year mortality rates for the 189 male patients were 75.1%, 85.2%, and 89.9%, respectively; the corresponding rates for the 107 female patients were 66.4%, 86.0%, and 88.8%, respectively. There was no statistically significant difference between two groups regarding mortality rates. The five-year survival curve of male patients was similar to that of female patients. The 6-month, 1-year, and 5-year mortality rates for the 70 very old male patients were 90.0%, 95.7%, and 97.1%, respectively; the corresponding rates for the 41 very old female patients were 63.4%, 90.2%, and 95.1%, respectively. There was a statistically significant difference between very old male and very old female patients in the 6-month mortality rate and the five-year survival curve.
Conclusion: There were no gender differences in weaning status, ventilator dependence, in-hospital mortality, or survival outcomes among patients requiring prolonged mechanical ventilation. Among very old patients requiring prolonged mechanical ventilation, the risk of death was 34% lower in very old female patients than in very old male patients for a period of five years.
Keywords: prolonged mechanical ventilation, respiratory care center, gender medicine, long-term survival
Introduction
Men and women differ biologically and in lifestyle factors, such as nutrition, physical activity, work, education, and stress. In many diseases, the incidence, causes, risk factors, clinical presentations, diagnoses, treatments, responses to treatment and prognoses differ significantly between women and men. Gender medicine is a new discipline that explores gender influences on the pathophysiology, clinical symptoms and signs, prevention, therapy and prognosis of diseases. The development of gender-specific medicine is important to understand the differences in the prevention, care, treatment, and outcomes of diseases in both genders. The aim of gender medicine is to recognize the differences arising from gender in several aspects, including anatomical, physiological, biological, functional, and social aspects, as well as the response between genders to pharmacological treatment.1 Many studies discuss gender differences in medical diseases such as cancer, coronary heart disease, diabetes mellitus, stroke, Alzheimer’s disease, dementia, depression, chronic kidney disease, liver disease, and autoimmune disease.2–18 The studies discussing gender differences in pulmonary diseases have mainly focused on asthma, cancer, chronic obstructive pulmonary disease (COPD), cystic fibrosis, and tuberculosis.19–26 The extent of gender differences in disease cause, course, and prognosis in patients on prolonged mechanical ventilation (PMV) is unknown and may vary based on many factors. The purpose of this study was to investigate the effects of gender differences according to age, causes of respiratory failure leading to PMV, comorbidities, respiratory care center (RCC; a weaning unit within an acute-care hospital) discharge status, successful weaning, mortality rate and long-term survival outcomes in patients with PMV in a RCC.
Methods
Details of the Hospital
The Dalin Tzu Chi Hospital is a tertiary-level teaching hospital with 600 acute-care beds and an intensive care unit (ICU) containing 59 beds. A 10-bed ventilator weaning unit (RCC) is available within Dalin Tzu Chi Hospital (an acute-care hospital), and this unit provides care for patients on PMV.
Patient Details
We conducted a retrospective single-center study and enrolled all patients consecutively admitted to the RCC of Dalin Tzu Chi Hospital between January 1, 2012, and December 31, 2017. Patients included those who received PMV for >21 days and patients who were eligible for RCC admission if they met the Taiwan National Health Insurance requirements.27
The long-term survival of all participants was calculated from the date of admission to the RCC until death or December 31, 2021. We collected data on all patients requiring PMV, including age, gender, comorbidities, causes of acute respiratory failure leading to PMV, receipt or not of tracheostomy, RCC discharge status, weaning status, and long-term outcomes. Data were extracted retrospectively for all participants from their medical records. Survival curves for all patients requiring PMV and for very old (aged ≥ 80 years) patients requiring PMV were compared separately based on gender.
Definition of Outcomes
A PMV patient was defined as using a mechanical ventilator for at least six hours daily for 21 or more consecutive days. A successfully weaned patient was defined as a patient who was independent of the ventilator for 5 consecutive days and nights, and these patients were transferred to the general ward for further care. We classified the successfully weaned patients requiring PMV into two groups: (1) ward mortality patients who died in the ward before hospital discharge and (2) discharged PMV patients who discharged from the hospital after weaning from PMV. Ventilator dependence was defined as an inability to be weaned from the ventilator, which necessitated transfer to a long-term care hospital (LTCH) for long-term ventilator support (LTCH is a respiratory care ward in Taiwan). Unsuccessfully weaned patients included patients who died during the RCC hospitalization, hospice patients in the RCC, and ventilator-dependent patients in the LTCH. The in-hospital mortality patients included patients who died during RCC hospitalization, successfully weaned patients who died in the general ward before hospital discharge, and hospice patients in the RCC. Patients aged ≥ 80 years were defined as very old patients.
Causes of acute respiratory failure leading to PMV were classified into the following 11 categories: (1) pneumonia, (2) intracranial hemorrhage, (3) sepsis, (4) postoperative condition, (5) COPD, (6) cardiac disease (including decompensated heart failure, coronary atherosclerotic disease, and acute myocardial infarction), (7) underlying malignant disease, (8) cervical spine disease, (9) postcardio-pulmonary-cerebral resuscitation (CPCR) hypoxic encephalopathy, (10) cerebral infarction, and (11) other miscellaneous causes.
Statistical Analysis
Continuous variables are expressed as the mean ± standard deviation or median, whereas categorical variables are expressed as frequencies and percentages. The differences in baseline characteristics, causes of acute respiratory failure, RCC discharge status, weaning status, the receipt or not of tracheostomy, and comorbidities were evaluated using Student’s t test for continuous variables and Pearson’s chi-square test or Fisher’s exact test for categorical variables. The differences in 6-month, 1-year, 3-year and 5-year mortality rates were evaluated using Fisher’s exact test between male and female patients requiring PMV. Univariate analysis was used to analyze differences in variables for male and female patients requiring PMV. Multivariate stepwise logistic regression models were used to evaluate the impact of each variable in male and female patients requiring PMV. Kaplan–Meier method was used to estimate the cumulative probability of survival as a function of the number of months in log-term follow-up male patients requiring PMV and long-term follow-up female patients requiring PMV. The Log rank test was used to compare survival rates between the two groups. Cox proportional hazards models were used to determine whether there was a relationship between the survival rates of the two groups. The Kaplan–Meier method was also used to estimate the cumulative probability of survival as a function of the number of months in very old male patients requiring PMV and very old female patients requiring PMV. The Log rank test was used to compare survival rates between the two groups. Cox proportional hazards models were used to determine the relationship between the survival rates of the two groups. All statistical analyses were conducted using the statistical package SPSS for Windows (Version 17.0, SPSS, Inc., Chicago, IL), and a P value<0.05 was considered to show statistical significance.
Results
Over six years, 574 patients were admitted to the RCC (Figure 1). Of these, 357 (62.2%) were men, and 217 (37.8%) were women. Three hundred ninety-one patients (68.1%) were successfully weaned from the ventilator, including 242 men and 149 women.28 The mean age was statistically significantly difference between male and female patients (71.46 vs 73.88 years, P=0.046). Table 1 shows the differences in clinical variables between male and female patients requiring PMV. There was no statistically significant difference between male and female patients in successful weaning, ventilator dependence, RCC mortality, general ward mortality, or in-hospital mortality. In terms of comorbidities, there was a statistically significant difference between male and female patients only for cardiovascular comorbidities. In terms of causes of respiratory failure leading to PMV, sepsis and cardiac disease were reported more often in female patients, and pneumonia was reported more often in male patients. A multivariate analysis between male and female patients requiring PMV showed that sepsis and cardiac disease were statistically significant difference between two groups (Table 2).
 |
Table 1 Comparison of Clinical Variables Between Male and Female in 574 PMV Patients |
 |
Table 2 Difference in Clinical Characteristics Variables Between Male and Female in 574 Prolonged Mechanical Ventilation Patients |
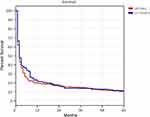
We further gathered long-term follow-up data on 296 patients requiring PMV up to December 31, 2021. Of these, 189 (63.9%) were men, and 107 (36.1%) were women. In terms of comorbidities, there was a statistically significant difference between male and female patients for malignant disease. In terms of causes of respiratory failure leading to PMV, sepsis was reported more often in female patients, and pneumonia was reported more often in male patients (Table 3). A multivariate analysis between long-term follow-up male patients requiring PMV and long-term follow-up female patients requiring PMV showed there was no statistically significant difference between two groups (Table 4). The 6-month, 1-year, 3-year, and 5-year mortality rates for the 189 male patients were 75.1%, 80.4%, 85.2%, and 89.9%, respectively; the corresponding rates for the 107 female patients were 66.4%, 78.5%, 86.0%, and 88.8%, respectively. There was no statistically significant difference between male and female patients in any of the above mortality rates. Kaplan–Meier analysis showed that the five-year survival curve of male patients requiring PMV was similar to that of female patients requiring PMV (P = 0.477; Log rank test). According to a Cox proportional hazards regression analysis of the 296 patients requiring PMV, no factors were determined to be related to survival in male patients or female patients (Figure 2).
 |
Table 3 Comparison of Clinical Variables Between Male and Female in 296 Long-Term Follow-Up Prolonged Mechanical Ventilation Patients |
 |
Table 4 Difference in Clinical Characteristics Variables Between Male and Female in 296 Long-Term Follow-Up Prolonged Mechanical Ventilation Patients |
These 296 patients requiring PMV included 70 very old male patients and 41 very old female patients. In terms of comorbidities, malignant disease was reported more often in very old male patients (Table 5). A multivariate analysis between very old male patients and very old female patients showed that only malignancy comorbidity was statistically significantly difference between two groups (Table 6). The 6-month, 1-year, 3-year, and 5-year mortality rates for the 70 very old male patients were 90.0%, 92.9%, 95.7%, and 97.1%, respectively; the corresponding rates for the 41 very old female patients were 63.4%, 80.5%, 90.2%, and 95.1%, respectively. A statistically significant difference between very old male patients and very old female patients was found only in the 6-month mortality rate (P=0.001, odds ratio (OR)=5.192). Kaplan–Meier analysis showed a statistically significant difference in survival between very old male patients and very old female patients (P = 0.038; Log rank test). According to Cox proportional hazards regression analysis of the 111 very old patients requiring PMV, the risk of death was 34% lower in the very old female patients than in the very old male patients (P = 0.045; hazard ratio (HR) = 0.66; 95% confidence interval (CI) 0.442–0.991) (Figure 3).
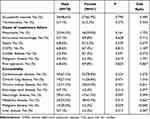 |
Table 5 Comparison of Clinical Variables Between Male and Female in 111 Very Old Long-Term Follow-Up Prolonged Mechanical Ventilation Patients |
 |
Table 6 Difference in Clinical Characteristics Variables Between Male and Female in 111very Old Long-Term Follow-Up Prolonged Mechanical Ventilation Patients |
Discussion
We did not find any studies in the international literature related to gender differences in patients requiring PMV. To our knowledge, this study is the only study to focus on gender differences in patients requiring PMV in the literature. Therefore, we can analyze only our research results, and we hope that these results can inspire similar research.
There were 256 (71.7%) male patients requiring PMV aged ≥ 65 years and 172 (79.3%) female patients requiring PMV aged ≥ 65 years (P=0.048, OR= 0.663). Therefore, the mean age of women was older than that of men in our study. In a study by Corrao et al, a retrospective observational study included 1380 hospitalized elderly patient. Coronary artery disease was more frequent in men, but hypertension was more frequent in women.29 Motiejunaite et al demonstrated that hypertension was more frequent in women in the studies of 22,523 acute heart failure patients.30 There were 35 cases (9.8%) of coronary artery disease in male patients requiring PMV and 12 cases (5.5%) of coronary artery disease in female patients requiring PMV (P=0.084, OR=1.857). There were 166 cases (46.5%) of hypertension in male patients requiring PMV and 134 cases (61.8%) of hypertension in female patients requiring PMV (P<0.001, OR=0.538, 95% CI 0.382–0.759). The comparison of the clinical demographic profiles between male and female patients requiring PMV showed more cardiovascular comorbidities in female patients requiring PMV in our study, similar to the literature. The analysis of causes of respiratory failure leading to PMV showed gender differences in pneumonia, sepsis and cardiac disease. Female patients had more cardiovascular comorbidities resulting in more respiratory failure secondary to cardiac disease. There were 3 cases (0.8%) of urosepsis in male patients and 10 cases (4.6%) of urosepsis in female patients (P=0.006, OR=0.175, 95% CI 0.048–0.645). Female patients have a higher risk of urinary tract infection than male patients. Among women aged 18 years and older, the estimated incidence was 12.6%; for men, this incidence was only 3%.31 Female patients have a higher risk of urinary tract infection than male patients. This clinical phenomenon explains why there were more urosepsis cases in female patients in this study. Some studies showed that the male gender was associated with an increased risk of pneumonia.32–35 In our patients requiring PMV, we found that pneumonia was predominant in males as the cause of respiratory disease.
In this study, RCC discharge statuses, including successful weaning, ventilator dependence, and in-hospital mortality, were similarly distributed across both genders. This finding means that there was no statistically significant difference in short-term outcomes between male and female patients requiring PMV. In terms of long-term survival outcomes, there was no statistically significant difference in five-year survival outcomes between male and female patients requiring PMV. Few studies have explored very old patients requiring PMV.36–38 These studies mainly focused on the clinical characteristics, weaning outcomes and long-term outcomes of patients requiring PMV. No study discusses gender differences in long-term survival outcomes. We explored whether there were gender differences in long-term survival outcomes in very old patients requiring PMV. There were 14 cases (20.0%) of malignancy comorbidity in very old male patients requiring PMV and 1 case (2.4%) of malignancy comorbidity in very old female patients requiring PMV (P=0.029, OR=10.00, 95% CI 1.263–79.164). Very old male patients were more number of malignancy comorbidity patients than very old female patient. A comparison of very old patients requiring PMV between males and females with 6-month mortality rate showed that there was a statistically significant difference between two groups (P=0.001, OR= 5.192). The 5-year survival rate analysis showed that very old male patients requiring PMV had a worse five-year survival rate than very old female patients requiring PMV in our study. The poorer survival outcome of the very old male patients requiring PMV was related to the high 6-month mortality rate and a higher percentage of malignancy comorbidity. The importance of this study is that it is a pioneering report on gender differences in PMV. We hope this study will inspire more medical experts to research gender differences in PMV.
Limitations of Our Study
Our findings on the gender differences in patients requiring PMV must be interpreted with caution since they are derived from a 6-year retrospective single-center study and there is a possibility of changing the management strategy. The gender differences in patients requiring PMV in terms of causes of respiratory failure, clinical characteristics, treatment outcomes, weaning status, and long-term survival outcomes need further prospective study by medical experts in the future. We expect additional studies on gender differences in patients requiring PMV to yield additional insights.
Conclusion
Among all patients requiring PMV, there were no gender differences in terms of weaning status, ventilator dependence, in-hospital mortality or survival outcomes. Among very old (aged ≥ 80 years) patients requiring PMV, very old female patients requiring PMV had better survival outcomes than very old male patients requiring PMV, related to the high 6-month mortality rate and a higher percentage of malignancy comorbidity in very old male patients requiring PMV.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There was no funding for this study.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Mauvais-Jarvis F, Merz NB, Barnes PJ, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396(10250):565–582. doi:10.1016/S0140-6736(20)31561-0
2. Wagner AD, Oertelt-Prigione S, Adjei A, et al. Gender medicine and oncology: report and consensus of an ESMO workshop. Ann Oncol. 2019;30:1912–1924. doi:10.1093/annonc/mdz414
3. Clocchiatti A, Cora E, Zhang Y, Dotto GP. Sexual dimorphism in cancer. Nat Rev Cancer. 2016;16:330–339. doi:10.1038/nrc.2016.30
4. Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018;363:k4247. doi:10.1136/bmj.k4247
5. Regitz-Zagrosek V, Oertelt-Prigione S, Prescott E, et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37:24–34.
6. Mauvais-Jarvis F. Gender differences in glucose homeostasis and diabetes. Physiol Behav. 2018;187:20–23. doi:10.1016/j.physbeh.2017.08.016
7. Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316. doi:10.1210/er.2015-1137
8. Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–926. doi:10.1016/S1474-4422(08)70193-5
9. Bots SH, Peters SAE, Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health. 2017;2:e000298. doi:10.1136/bmjgh-2017-000298
10. Sheth SA, Lee S, Warach SJ, et al. Sex differences in outcome after endovascular stroke therapy for acute ischemic stroke. Stroke. 2019;50:2420–2427. doi:10.1161/STROKEAHA.118.023867
11. Ferretti MT, Iulita MF, Cavedo E, et al. Sex differences in Alzheimer disease—the gateway to precision medicine. Nat Rev Neurol. 2018;14:457–469. doi:10.1038/s41582-018-0032-9
12. Canevelli M, Quarata F, Remiddi F, et al. Sex and gender differences in the treatment of Alzheimer’s disease: a systematic review of randomized controlled trials. Pharmacol Res. 2017;115:218–223. doi:10.1016/j.phrs.2016.11.035
13. Zhu L, Rochon PA, Gruneir A, et al. Sex differences in the prevalent use of oral formulations of cholinesterase inhibitors in older adults with dementia. Drugs Aging. 2019;36:875–884. doi:10.1007/s40266-019-00690-9
14. Marcus SM, Kerber KB, Rush AJ, et al. Sex differences in depression symptoms in treatment-seeking adults: confirmatory analyses from the Sequenced Treatment Alternatives to Relieve Depression study. Compr Psychiatry. 2008;49:238–246. doi:10.1016/j.comppsych.2007.06.012
15. Carrero JJ, Hecking M, Chesnaye NC, Jager KJ. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol. 2018;14:151–164. doi:10.1038/nrneph.2017.181
16. Guy J, Peters MG. Liver disease in women: the influence of gender on epidemiology, natural history, and patient outcomes. Gastroenterol Hepatol (N Y). 2013;9:633–639.
17. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi:10.1002/hep.28431
18. Whitacre CC. Sex differences in autoimmune disease. Nat Immunol. 2001;2:777–780. doi:10.1038/ni0901-777
19. Casimir GJ, Lefèvre N, Corazza F, Duchateau J. Sex and inflammation in respiratory diseases: a clinical viewpoint. Biol Sex Differ. 2013;4:16. doi:10.1186/2042-6410-4-16
20. Pinkerton KE, Harbaugh M, Han MK, et al. Women and lung disease. Sex differences and global health disparities. Am J Respir Crit Care Med. 2015;192:11–16. doi:10.1164/rccm.201409-1740PP
21. Stolz D, Kostikas K, Loefroth E, et al. Differences in COPD exacerbation risk between women and men: analysis from the UK Clinical Practice Research Datalink data. Chest. 2019;156:674–684. doi:10.1016/j.chest.2019.04.107
22. Han MK, Postma D, Mannino DM, et al. Gender and chronic obstructive pulmonary disease: why it matters. Am J Respir Crit Care Med. 2007;176:1179–1184. doi:10.1164/rccm.200704-553CC
23. Zein JG, Denson JL, Wechsler ME. Asthma over the adult life course: gender and hormonal influences. Clin Chest Med. 2019;40:149–161. doi:10.1016/j.ccm.2018.10.009
24. Shah R, Newcomb DC. Sex bias in asthma prevalence and pathogenesis. Front Immunol. 2018;9:2997. doi:10.3389/fimmu.2018.02997
25. Hamid Salim MA, Declercq E, Van Deun A, Saki KAR. Gender differences in tuberculosis: a prevalence survey done in Bangladesh. Int J Tuberc Lung Dis. 2004;8:952–957.
26. Singh PP, Sharma PP, Kumar A. A study of gender differentials in the prevalence of tuberculosis based on NFHS-2 and NFHS-3 data. Indian J Community Med. 2010;35(2):230–237. doi:10.4103/0970-0218.66869
27. Huang C, Chen JC. The Long-Term Survival of Intracranial Hemorrhage Patients Successfully Weaned from Prolonged Mechanical Ventilation. Int J Gen Med. 2021;14:1197–1203. doi:10.2147/IJGM.S304228
28. Huang C. The Long-Term Survival of Successfully Weaned Prolonged Mechanical Ventilation Patients. Int J Gen Med. 2021;14:3981–3988. doi:10.2147/IJGM.S287529
29. Corrao S, Santalucia P, Argano C, et al. REPOSI Investigators. Gender-differences in disease distribution and outcome in hospitalized elderly: data from the REPOSI study. Eur J Intern Med. 2014;25:617–623. doi:10.1016/j.ejim.2014.06.027
30. Motiejūnaitė J, Akiyama E, Cohen-Solal A, et al. The association of long-term outcome and biological sex in patients with acute heart failure from different geographic regions. Eur Heart J. 2020;41:1357–1364. doi:10.1093/eurheartj/ehaa071
31. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7:653–660. doi:10.1038/nrurol.2010.190
32. Moss M, Mannino DM. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979–1996). Crit Care Med. 2002;30:1679–1685. doi:10.1097/00003246-200208000-00001
33. Kaplan V, Angus DC, Griffin MF, Clermont G, Scott Watson R, Linde-Zwirble WT. Hospitalized community-acquired pneumonia in the elderly: age and sex-related patterns of care and outcome in the United States. Am J Respir Crit Care Med. 2002;165:766–772. doi:10.1164/ajrccm.165.6.2103038
34. Neupane B, Walter SD, Krueger P, Marrie T, Loeb M. Predictors of inhospital mortality and re-hospitalization in older adults with community-acquired pneumonia: a prospective cohort study. BMC Geriatr. 2010;10:22. doi:10.1186/1471-2318-10-22
35. Gutiérrez F, Masiá M, Mirete C, et al. The influence of age and gender on the population-based incidence of community-acquired pneumonia caused by different microbial pathogens. J Infect. 2006;53:166–174. doi:10.1016/j.jinf.2005.11.006
36. Su J, Lin CY, Chen SK, Peng MJ, Wu CL. Characteristics and Outcome for Very Elderly Patients (> 80 years) Admitted to a Respiratory Care Center in Taiwan. Int J Gerontol. 2012;6:262–266. doi:10.1016/j.ijge.2012.01.030
37. Frengley JD, Sansone GR, Shakya K, Kaner RJ. Prolonged mechanical ventilation in 540 seriously ill older adults: effects of increasing age on clinical outcomes and survival. J Am Geriatr Soc. 2014;62:1–9. doi:10.1111/jgs.12597
38. Lai CC, Ko SC, Chen CM, Weng SF, Tseng KL, Cheng KC. The Outcomes and Prognostic Factors of the Very Elderly Requiring Prolonged Mechanical Ventilation in a Single Respiratory Care Center. Medicine. 2016;95:e2479. doi:10.1097/MD.0000000000002479
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.