Back to Journals » Orthopedic Research and Reviews » Volume 12
Functional Outcomes Following Surgical Fixation of Paediatric Lateral Condyle Fractures of the Elbow – A Systematic Review
Authors Birkett N , Al-Tawil K, Montgomery A
Received 15 May 2019
Accepted for publication 11 February 2020
Published 6 March 2020 Volume 2020:12 Pages 45—52
DOI https://doi.org/10.2147/ORR.S215742
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Nicholas Birkett,1 Karam Al-Tawil,1 Alexander Montgomery2
1Princess Alexandra Hospital, Harlow, Essex CM20 1QX, UK; 2Royal London Hospital, London E1 1FR, UK
Correspondence: Nicholas Birkett
Princess Alexandra Hospital, Hamstel Road, Harlow, Essex CM20 1QX, UK
Tel +44 79 6188 0429
Email [email protected]
Objective: Lateral humeral condyle fractures are the second most common elbow fractures in children. Both K-wire fixation and screw fixation have been advocated as suitable treatment options for displaced fractures. This study aimed to identify which fixation method was associated with the best functional outcomes.
Methods: A systematic review was conducted. Studies reporting functional outcomes following surgical fixation of lateral condyle fractures were included for review. The primary outcome measure was functional outcome. The secondary outcome measure was major complications. A narrative analysis was undertaken, as meta-analysis was felt to be inappropriate due to the differences between included studies.
Results: Ten retrospective non-randomised, comparative studies were eligible and included. No randomised-controlled trials were identified. The highest rate of excellent functional outcomes was seen with screw fixation (120/126 [95%]), compared with K-wire fixation (135/162 [86%]). The incidence of major complications was comparable, with complications in 6/95 (6%) of screw fixations and 6/141 (4%) K-wire fixations. A small sample of data on closed reduction demonstrated excellent functional results in 73 of 76 (96%) of patients. Closed reduction of displaced fractures is associated with a significant learning curve however.
Conclusion: The evidence was of poor quality and comprised of retrospective case series. This prevented meta-analysis and any firm conclusions being drawn from the available data. Screw fixation may be associated with improved functional outcomes. Complication rates between the two methods are comparable. Further prospective studies are recommended.
Keywords: lateral condyle fracture, paediatric, functional outcome, systematic review, K-wire fixation, screw fixation
Introduction
Fractures of the lateral condyle are the second most frequent elbow fracture in children after supracondylar fracture, comprising 10–20% of all paediatric elbow fractures.1,2 Despite this, the injury remains relatively rare, with a reported incidence of 1.6/10,000.3,4 The mechanism of injury is either through an avulsion of the condyle due to a varus force on a supinated forearm or through radial head impaction on the capitellum following a fall onto an outstretched hand.5,6
Multiple treatment options are available for these fractures, ranging from immobilisation for non-displaced or minimally displaced fractures to open reduction and fixation for displaced fractures. There is broad consensus that displaced fractures require surgical fixation, with most studies using >2 mm of articular displacement as indication for fixation.7,8 This consensus derives from the high-reported rates of secondary displacement and non-union following conservative treatment of displaced fractures.9,10
The most commonly used classification system is that developed by Milch.11 The author divided lateral condyle fractures into two subtypes. Type 1 fractures are lateral to the trochlear groove and are considered more mechanically stable. Type 2 fractures run through the trochlea and are considered less stable.
There is no clinical consensus regarding the best method of fixation, and many studies lack sufficient power to draw firm conclusions regarding functional outcomes of what is a relatively rare injury. Traditionally, fixation is achieved either using K-wires or through screw fixation. Reduction is traditionally achieved with an open approach, although closed reduction has been reported, and is discussed in this study. K-wire fixation has the advantages of a minimal risk of physeal damage and the opportunity for wire removal in an outpatient setting. Complications include pin site infection and loss of fixation.6,12 Screw fixation is thought to provide superior fixation through compression of the fracture site and to have a lower risk of infection.13 Damage to the physis and the long-term effects of this are not well understood however. Furthermore, the screws must be removed at a later date under general anaesthetic.
This study aims to systematically analyse the available literature to determine what the functional outcomes are and whether they differ based on method of fixation.
Materials and Methods
A PRISMA compliant systematic review was conducted to determine which surgical fixation method resulted in the best functional outcome and the fewest complications.14 The Embase and MEDLINE databases were searched, along with the Cochrane Library.
Search Strategy
A systematic literature search was performed on April 21st 2018. The Embase and MEDLINE databases, along with the Cochrane library were searched. The resulting papers were then manually searched to determine whether they met the inclusion criteria stated below (Table 1). This was performed independently by 2 authors (NB and KA-T). In the case of only one author including a paper, it was included in the review nonetheless. The search strategies and results are presented in Tables 2 and 3.
 |
Table 1 Full Inclusion and Exclusion Criteria |
 |
Table 2 MEDLINE and Embase Search Strategy and Results |
 |
Table 3 Cochrane Search Strategy and Results |
Study Selection
Study Designs
Unpublished studies, guidelines, protocols, and editorials were not considered. All other study designs were considered.
Types of Participants
Children who have sustained a lateral condyle fracture of the elbow.
Exclusion criteria include complex fractures (bicondylar fractures, associated supracondylar fractures) and pathological fractures. Studies involving animal or cadaveric models were not considered.
Interventions
Interventions eligible for consideration were children who have undergone surgical fixation of their fractures.
The full inclusion and exclusion criteria are summarised below:
Outcomes of Interest
The primary outcome measure of interest was functional outcome as measured through an established scoring system. Examples of these include the Mayo Elbow Performance Score (MEPS) and that developed by Hardacre et al.15,16
Secondary outcomes were major complications (non-union, deep infection, metalwork failure, re-fracture, re-operation, malunion, delayed union, neurovascular injury, compartment syndrome).
Literature Appraisal
The critical appraisal checklist for cohort studies developed by the Critical Appraisal Skills Programme (CASP) was used to evaluate the studies’ methodology and determine the value of the research, as this was the study design of all included papers.17
Data Collection and Results
The methodologies and data extracted were reviewed. Meta-analysis was felt to be inappropriate due to the heterogeneity in both treatment modalities and outcome measurements. A narrative review was conducted in order to best answer the research question.
Results
Search Results
A total of 226 studies were identified from the literature search (123 MEDLINE, 101 Embase, 2 Cochrane). Twenty-five studies were selected for full-text review following assessment of their abstracts. Of these 25, 10 met the inclusion criteria and were deemed eligible for this review. Many studies did not meet the inclusion criteria as their only outcome measurement was range of motion. Functional scoring systems can more accurately assess the impact of any reduced range of motion or clinical deformity on the patient themselves and are reliable and accurate.18 The full results of the literature search are presented in Tables 2 and 3, and in Figure 1.
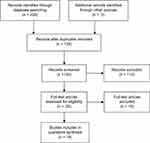 |
Figure 1 PRISMA flow diagram illustrating literature search. |
Critical Appraisal Results
Table 4 summarises the critical appraisal, assessed using the CASP critical appraisal tool. The tool comprises 12 questions to help systematically review a cohort study and determine any bias. Questions 7–9 “What are the Results” relate to the results of the individual study so are excluded (individual study findings can be seen in Table 5). All studies were retrospective comparative studies of level IV evidence. Many of the studies share the same limitations. They have small sample sizes with retrospectively collected data, which raises the risk of other variables impacting on the results and limits their power.
 |
Table 4 Results of the CASP Questionnaire for Cohort Studies for Each Included Paper |
 |
Table 5 Summary of Included Studies |
Findings
Of the ten studies, eight reported outcomes of K-wire fixation,19–28 four reported the outcomes of screw fixation,21,27,20,24 one reported outcomes of fixation with bioabsorbable materials19 and one of screw-wire fixation.28 In addition, three studies looked exclusively at closed reduction.23–26 The findings of the studies are summarised in Table 5.
Primary Outcome – Functional Outcomes
K-wire fixation had excellent functional outcomes in 52%28 to 100%19 of patients. Screw fixation had excellent functional outcomes in 89%27 to 100%20 of patients. Fixation with bioabsorbable materials had excellent functional outcomes in 100% of the five patients treated with this method. Screw-wire fixation was associated with an excellent functional outcome in 48% of patients.
Secondary Outcome – Complications
K-wire fixation was associated with a 0–9% risk of major complications. Screw fixation was associated with a 3–8% risk of major complications. The five patients treated with bioabsorbable materials suffered no major complications. The rate of complications following screw-wire fixation was not reported.
Discussion
The findings of this review demonstrate low-quality evidence from which it is hard to draw firm results as to whether K-wire fixation or screw fixation is associated with better functional outcomes. The sample size regarding other fixation methods is simply too small to draw any meaningful conclusions.
The studies were all of Level IV evidence, with a variety of methodologies that could lead to bias. Included studies did show similar basic demographics that are in keeping with existing epidemiological data on this injury.3,4 Therefore, the findings could be applicable to the wider population.
K-Wire vs Screw Fixation
Combining the available data shows excellent outcomes in 135 (83%) of 162 k-wire fixations and 120 (95%) of 126 screw fixations. Poor outcomes are reported in 6 (4%) of 162 k-wire fixations. No poor functional outcomes are reported following screw fixation. These results must be interpreted with caution; however, as the follow-up period varies greatly between studies (range 4.3–66.45 months, mean 20.7 months). There was no correlation between shorter follow up time and worse outcomes.
The worst functional outcomes for k-wiring were reported by Wirmer et al, with only 52% of their 21 participants having an excellent outcome.28 The authors used the scoring system developed by Dhillon et al, which grades even a 1° loss of range of motion from the contralateral side as “good” and not “excellent”.29 This will lead to patients with no true functional deficit being downgraded and could lead to poorer results than if they had used a scoring system such as MEPS, which gives any range of motion above 100° the highest functional score.
The two studies that directly compare k-wire fixation to screw fixation both report improved functional outcomes with screw fixation compared with k-wire fixation.21,27
Gilbert et al reported excellent functional outcomes of 94% in their screw group, compared with 86% in their k-wire group.21 Their study is limited however by the short follow up period (7.2 and 6.4 months). Their screw group was also treated at an earlier stage post-injury than the k-wire group, which may have influenced the results.
Stein et al reported excellent functional outcomes in 89% of their screw group, compared with 57% in their k-wire group.27 The study is again limited by the short follow up period (4.3 months for k-wiring) and the small sample size. As per Gilbert et al, the screw cohort was treated more recently than the k-wire cohort. Improved experience of the individual surgeons and improved orthopaedic knowledge could account for the improved results. Furthermore, the time post procedure at which patients were examined varied, which makes comparison of individual cases difficult, and limits the power of the study.
Complications were not reported as accurately as functional outcomes throughout the literature. Frongia et al and Wirmer et al did not accurately report their complications.28,20 Combining the available data on complications shows a major complication rate of 6 (4%) in 141 K-wire fixations and 6 (6%) in 95 screw fixations. From the available data, the complication rates of the two procedures appear to be comparable. No study found a statistically significant difference in the rate of major complications between the two methods.
Gilbert et al reported a significant difference in complications between k-wire and screw (13 to 3 – p=0.0074).21 They included asymptomatic lateral condylar overgrowth and capitellar irregularity as complications, however, unlike other studies.
One potential benefit of screw fixation is that it provides more stable fixation than with k-wires. It is a common practice to immobilise patients for 6–8 weeks in plaster following k-wire fixation,12,30 which will inevitably lead to stiffness. Patients treated with screw fixation do not require such a long period in plaster. This in turn permits earlier physiotherapy, which could account for the improved functional outcomes seen in the included studies.
Screw-Wire Fixation
Results were only reported by Wirmer et al, who suggest that screw-wires are used in favour of k-wires following their retrospective cohort study.28 Their functional results between the two methods were comparable; 48% excellent for screw-wire and 52% excellent for k-wire. One major drawback of the study is that the screw wires were inserted in a different configuration to the k-wires, a possible contributing factor not acknowledged by the authors. The small sample size and potential for bias in the study means that no firm conclusions can be drawn regarding screw-wire fixation.
Bioabsorbable Materials
The perceived benefit of using bioabsorbable materials for fixation is that no further procedure for metalwork removal is required. Previous studies have shown nonspecific inflammatory reactions such as seroma formation with this type of fixation.31 The study by Andrey et al showed no such effect, and excellent functional outcomes in all 5 of their patients.19 The small sample limits the power of the study. The authors also note that “using bioabsorbable pins and screws requires fine technical skills and good knowledge of the material”, highlighting a potential learning curve to the procedure. If similar results were reproduced independently by other authors in larger samples, then using bioabsorbable materials may become a treatment option in future.
The Role of Closed Reduction
Closed reduction and percutaneous k-wire fixation have often been proposed for minimally displaced fractures. In the three studies included in this review,23–26 the technique was attempted for all fracture types, even those that would be hard to reduce under direct vision following open exposure. The authors reported excellent results in 100%, 96%, and 94% of patients with this technique, albeit in small cohorts. Combining the data shows excellent results in 73 of 76 (96%) of patients. Song et al note in their paper the “learning curve” required – one of their surgeons did not even attempt closed reduction due to “lack of experience”.
It appears that significant technical skill is a prerequisite for this technique. Given the rarity of the injury, it is unlikely that surgeons outside of specialist centres will gain sufficient confidence and exposure to this technique for it to become commonplace. If other studies are performed by other investigators that reproduces the excellent results of Song et al, then closed reduction may become a standard of care in the future.
Study Limitations
Other factors may have influenced the findings of this systematic review. Unpublished studies, editorials, guidelines, and protocols were excluded. This was in an attempt to identify high-quality studies only, although this may have led to selection bias. Selecting English-only studies (due to translation difficulties) may also have limited the scope of the review. Our computer search process, despite being the most efficient technique, may have excluded some articles.
Conclusion
Two comparative studies appear to show that screw fixation is associated with better long-term functional outcomes without an increased risk of complications. However, these studies lack power. Pooling all the available data also appears to show a slight benefit of screw fixation, but the evidence is not strong enough to guide a complete change in practice.
Adequate comparison between k-wiring and screw fixation could probably only be achieved by a prospective, randomised study comparing the two. This would help eliminate selection bias and other confounding factors such a surgeon choice.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Emery KH, Zingula SN, Anton CG, Salisbury SR, Tamai J. Pediatric elbow fractures: a new angle on an old topic. Pediatr Radiol. 2016;46(1):61–66. doi:10.1007/s00247-015-3439-0
2. Tejwani N, Phillips D, Goldstein RY. Management of lateral humeral condylar fracture in children. J Am Acad Orthop Surg. 2011;19(6):350–358. doi:10.5435/00124635-201106000-00005
3. Landin LA. Fracture patterns in children: analysis of 8682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand. 1983;54(sup202):3–109. doi:10.3109/17453678309155630
4. Kim SS, Kim HJ, Kim HH, Seok SY, Jung SY. The changes in patient pattern for pediatric supracondylar and lateral condylar humeral fractures. J Korean Orthop Assoc. 2015;50(2):132–136. doi:10.4055/jkoa.2015.50.2.132
5. Lovell WW, Winter RB, Morrissy RT, Weinstein SL. Lovell and Winter’s Pediatric Orthopaedics. Lippincott Williams & Wilkins; 2006.
6. Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. Bone Joint J. 1975;57(4):430–436.
7. Bhandari M, Tornetta P, Swiontkowksi MF. Displaced lateral condyle fractures of the distal humerus. J Orthop Trauma. 2003;17(4):306–308. doi:10.1097/00005131-200304000-00012
8. Sullivan JA. Fractures of the lateral condyle of the humerus. J Am Acad Orthop Surg. 2006;14(1):58–62. doi:10.5435/00124635-200601000-00010
9. Flynn JC, Richards JJ, Saltzman RI. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J Bone Joint Surg Am. 1975;57(8):1087–1092. doi:10.2106/00004623-197557080-00009
10. Flynn JC. Nonunion of slightly displaced fractures of the lateral humeral condyle in children: an update. J Pediatr Orthop. 1989;9(6):691–696.
11. Milch H. Fractures of the external humeral condyle. J Am Med Assoc. 1956;160(8):641–646. doi:10.1001/jama.1956.02960430031006
12. Launay F, Leet AI, Jacopin S, Jouve J-L, Bollini G, Sponseller PD. Lateral humeral condyle fractures in children: a comparison of two approaches to treatment. J Pediatr Orthop. 2004;24(4):385–391. doi:10.1097/01241398-200407000-00008
13. Loke W, Shukur M, Yeap J. Screw osteosynthesis of displaced lateral humeral condyle fractures in children: a mid-term review. Med J Malaysia. 2006;61:40–44.
14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi:10.7326/0003-4819-151-4-200908180-00135
15. Morrey BF. The Elbow and Its Disorders. Elsevier Health Sciences; 2009.
16. Hardacre JA, Nahigian SH, Froimson AI, Brown JE. Fractures of the lateral condyle of the humerus in children. JBJS. 1971;53(6):1083–1095. doi:10.2106/00004623-197153060-00003
17. CASP U. Critical Appraisal Skills Programme (CASP). Qual Res Checklist. 2017;31:13.
18. Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW. Accuracy and reliability of the Mayo elbow performance score. J Hand Surg. 2014;39(6):1146–1150. doi:10.1016/j.jhsa.2014.01.041
19. Andrey V, Tercier S, Vauclair F, Bregou-Bourgeois A, Lutz N, Zambelli PY. Lateral condyle fracture of the humerus in children treated with bioabsorbable materials. Sci World J. 2013;2013:869418. doi:10.1155/2013/869418
20. Frongia G, Janosi C, Mehrabi A, Schenk JP, Gunther P. Long-term outcome in displaced lateral humeral condyle fractures following internal screw fixation in children. Acta Orthop Belg. 2016;82(4):889–895.
21. Gilbert SR, MacLennan PA, Schlitz RS, Estes AR. Screw versus pin fixation with open reduction of pediatric lateral condyle fractures. J Pediatr Orthop B. 2016;25(2):148–152. doi:10.1097/BPB.0000000000000238
22. Marcheix PS, Vacquerie V, Longis B, Peyrou P, Fourcade L, Moulies D. Distal humerus lateral condyle fracture in children: when is the conservative treatment a valid option? Orthop Traumatol. 2011;97(3):304–307.
23. Mintzer CM, Waters PM, Brown DJ, Kasser JR. Percutaneous pinning in the treatment of displaced lateral condyle fractures. J Pediatr Orthop. 1994;14(4):462–465. doi:10.1097/01241398-199407000-00008
24. Sharma JC, Arora A, Mathur NC, Gupta SP, Biyani A, Mathur R. Lateral condylar fractures of the humerus in children: fixation with partially threaded 4.0-mm AO cancellous screws. J Trauma. 1995;39(6):1129–1133. doi:10.1097/00005373-199512000-00021
25. Song KS, Kang CH, Min BW, Bae KC, Cho CH, Lee JH. Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children. J Bone Joint Surg Am. 2008;90(12):2673–2681. doi:10.2106/JBJS.G.01227
26. Song KS, Shin YW, Oh CW, Bae KC, Cho CH. Closed reduction and internal fixation of completely displaced and rotated lateral condyle fractures of the humerus in children. J Orthop Trauma. 2010;24(7):434–438. doi:10.1097/BOT.0b013e3181de014f
27. Stein BE, Ramji AF, Hassanzadeh H, Wohlgemut JM, Ain MC, Sponseller PD. Cannulated lag screw fixation of displaced lateral humeral condyle fractures is associated with lower rates of open reduction and infection than pin fixation. J Pediatr Orthop. 2017;37(1):7–13. doi:10.1097/BPO.0000000000000579
28. Wirmer J, Kruppa C, Fitze G. Operative treatment of lateral humeral condyle fractures in children. Eur J Pediatr Surg. 2012;22(4):289–294. doi:10.1055/s-0032-1308709
29. Dhillon KS, Sengupta S, Singh BJ. Delayed management of fracture of the lateral humeral condyle in children. Acta Orthop Scand. 1988;59(4):419–424. doi:10.3109/17453678809149395
30. Foster DE, Sullivan JA, Gross RH. Lateral humeral condylar fractures in children. J Pediatr Orthop. 1985;5(1):16–22. doi:10.1097/01241398-198501000-00004
31. Hope P, Williamson D, Coates C, Cole W. Biodegradable pin fixation of elbow fractures in children. A randomised trial. J Bone Joint Surg Br. 1991;73(6):965–968. doi:10.1302/0301-620X.73B6.1659570
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
