Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Functional Alterations in Patients with Bipolar Disorder and Their Unaffected First-Degree Relatives: Insight from Genetic, Epidemiological, and Neuroimaging Data
Authors Zhang H, Chen J , Fang Y
Received 26 June 2023
Accepted for publication 30 November 2023
Published 14 December 2023 Volume 2023:19 Pages 2797—2806
DOI https://doi.org/10.2147/NDT.S427617
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Haonan Zhang,1 Jun Chen,1,2 Yiru Fang1– 4
1Clinical Research Center, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Shanghai Key Laboratory of Psychotic Disorders, Shanghai, People’s Republic of China; 3Department of Psychiatry & Affective Disorders Center, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 4CAS Center for Excellence in Brain Science and Intelligence Technology, Shanghai, People’s Republic of China
Correspondence: Jun Chen, Clinical Research Center, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, No. 600 Wanping South Road, Xuhui District, Shanghai, 200030, People’s Republic of China, Email [email protected] Yiru Fang, Department of Psychiatry & Affective Disorders Center, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, No. 197 Ruijin 2nd Road, Huangpu District, Shanghai, 200025, People’s Republic of China, Email [email protected]
Abstract: Bipolar disorder (BD) profoundly affects cognitive and psychosocial functioning, leading to a significant illness burden on patients and their families. Genetic factors are predominant in the onset of bipolar disorder and functional impairments. This disorder exhibits a strong family aggregation, with heritability estimates reaching up to 80%. Individuals with BD often experience impaired functioning, especially in significant areas such as physical performance, sleep, cognition, interpersonal interactions, socioeconomic status, family and marital relationships, work and school performance, well-being, and life expectancy. However, patients with different subtypes exhibit significant heterogeneity in social functioning, cognition, and creativity levels. There are notable differences in psychosocial and cognitive function in their unaffected first-degree relatives (UFR) who do not suffer but may carry susceptibility genes compared to healthy control (HC) without a family history. The observations indicate common genetic structures between BD patients and their UFR, which results in varying degrees of functional abnormalities. Therefore, this article mainly provides evidence on cognition, creativity, and psychosocial functioning in patients with BD and their UFR to provide a more comprehensive understanding of this critical topic in the field of BD. By integrating various findings, including clinical data and neuroimaging studies, our article aims to provide insights and valuable information for a deeper exploration of the pathogenesis of BD and the development of more targeted therapeutic strategies in the future.
Keywords: bipolar disorder, cognition, psychosocial function, creativity, unaffected first-degree relatives, genetics
Introduction
BD is a group of chronic mental illnesses marked by recurrent episodes of mania and depression, which alternate as the primary clinical symptoms. It exhibits a high prevalence, frequent relapses, and elevated rates of suicide, which has become one of the major mental health issues globally threatening human physical and mental well-being.1 Statistically speaking, there are approximately 39.5 million patients with BD worldwide.2 The lifetime prevalence (12-month prevalence) in the population is about 2.4% (0.6–1.5%), with BD-I type prevalence at approximately 0.6% (0.4%) and BD-II type at around 0.4% (0.3%).3,4 The systematic analysis from the Global Burden of Disease Study 2019 revealed that the age-standardized prevalence rate indicates an average of 489.8 BD patients per 100,000 people and it is one of the top 30 causes of years lived with disability (YLDs) globally and the fifth leading cause of disability-adjusted life years (DALYs) in mental and substance use disorders.2
Function and Disability in Bipolar Disorder
Currently, Various updated guides emphasize the importance of functional recovery, and many patients consider the restoration of normal psychosocial functioning as an essential indicator of remission. The human function is a general concept of which various organizations or scholars provide different definitions. The International Classification of Functioning, Disability, and Health (ICF) summarizes it in the following 3 points: Body structure and function, activity participation, and personal environmental factors,5 of which are judged by assessing whether the person’s eligibility to perform a specific task. It primarily refers to the ability to work, learn, live independently, participate in recreational activities, and maintain interpersonal relationships. Disability usually means an individual is experiencing one or more difficulties or challenges in functioning across various aspects of life.6
However, Studies on what contributes to functional alteration in patients with BD have reached mixed conclusions. Patients with BD often suffer damage in function, particularly evident in the following essential aspects: physical fitness, sleeping, cognition, interpersonal interactions, socio-economic status, family and marital relationships, work and academic performance, well-being, and life expectancy.4 Up to 50% of patients have residual depressive symptoms in the interictal phase, and even euthymic patients and those with subsyndromes also have cognitive deficits. In these populations, the activity of the Dorsolateral Prefrontal Cortex (DLPFC), which plays an important role in advanced cognitive functions, and the Ventrolateral Prefrontal Cortex (VLPFC), which is closely related to activities such as language and emotion regulation, were found to be reduced during the Stroop task.7 Residual symptoms compromise functional recovery and serve as a major contributor to relapse.8 Besides, the diencephalic function of patients with long courses will likely be affected to varying degrees, leading to an increased risk of dementia.9 Furthermore, there is a high rate of misdiagnosis at the first clinic visit for BD. The average duration of misdiagnosis correction is 6.46 years, even up to 10 years.10 Age at onset is negatively correlated with a delay in treatment.11 At least 1/5 of major depressive disorder (MDD) patients in China may not be appropriately diagnosed with BD,12 the same indicator shown to be from 3.3% to 21.6% globally.13 Admittedly, the earlier diagnosis and intervention are given, the fewer functional problems arise.
It is worth noting that cognition is heterogeneous in patients with BD, more prominent in BD-I. A subset of patients showed cognitive performance similar to that of unaffected individuals, and even exceeded the functioning of unaffected individuals in some domains.14 Patients with a first episode of BD-I could be divided into three cognitive subgroups using latent class analysis of processing speed, verbal memory, nonverbal memory, executive function, attention, and working memory scores. Further use of neuroimaging scans to compare IQ, intracranial volume, whole brain volume, and regional volume before and after the onset of subgroups and HC revealed apparent differences between subgroups in whole gray matter and white matter volume.15 Such cognitive difference might be associated with altered pathophysiological structures resulting from an abnormal neurodevelopmental process before the first episode.
Genetic Factors and Familial Aggregation
BD is a polygenic inherited psychiatric disorder with up to 80% heritability. The age of onset, frequency of attacks, and type of symptom demonstrate a highly heritable and familial pattern.16 Unfortunately, family members of patients have a 9-fold risk of developing BD and an approximately 2.5-fold risk of other affective disorders than HC.17 The offspring of parents diagnosed with BD have a notably higher risk of major psychiatric disorders.18,19 72% of BD offspring matched DSM-IV criteria for Axis I diagnosed disease, 54% had mood disorders, 13% were diagnosed with BD, and 3% were diagnosed BD-I.20 They have an increased risk of attention deficit hyperactivity disorder21 and abnormal levels of immune-related factors such as BDNF, IGF-BP2, IL-7.22
In the field of molecular genetics, a genome-wide association study (GWAS) involving over 50,000 patients and healthy controls has identified 30 genetic loci associated with BD. These include genes like voltage-gated calcium channel (CACNA1C), neurotransmitter receptor (GRIN2A), synaptic component (ANK3), and several other candidate genes.23 Subsequently, A GWAS study of 6472 Han Chinese patients discovered novel risk loci, including VRK1 and RHEBL2, suggesting genetic heterogeneity between different racial groups.24
In conclusion, Genetics play a considerable role in the development of BD and high incidence in offspring, demonstrating irrefutable evidence of familial aggregation. Childhood trauma and family functioning also contribute to it.25,26 However, it’s still unclear how susceptibility genes lead to neural pathways or processes to generate clinical symptoms. And that is why clinical research tends to favor investigating patients, UFR, and HC to showcase the wonders of genetics in the occurrence and progress of BD.
Summary
As previously mentioned, genetic effects are seen in functioning differences among patients, UFR, and HC. While those UFR themselves have not experienced episodes of mania or depression, they may be affected to some extent in areas such as cognition and social functioning due to the potential presence of susceptibility genes. Therefore, it is imperative to consolidate research evidence spanning various domains of functional performance in individuals with BD and their UFR and discuss the mechanics behind it.
Cognition
Cognition and Related Neuroimaging Performance in BD Patients and UFR
It is widely recognized that patients have varying degrees of neurocognitive impairment. This conclusion is well illustrated both using the traditional Screen for Cognitive Impairment in Psychiatry (SCIP) tool and the newly developed Internet-Based Cognitive Assessment Tool (ICAT) recommended by the International Society for Bipolar Disorders (ISBD).27 Cognition is closely associated with daily psychosocial functioning, employment and quality of life, more directly, a meta-analysis even indicated that cognitive functioning had a greater impact on patients’ working capacity than subclinical depressive and manic symptoms.28 Verbal memory and executive function have been found to be moderately positively correlated with career development.29,30 As mentioned earlier, cognitive functions are heterogeneous among patients.16 Some researchers collected data about cognition and structural magnetic resonance imaging (sMRI) of 80 patients with the first episode of BD-I and calculated brain-predicted age difference (brainPAD) via machine learning.31 They found markedly lower global cognitive scores and prominent verbal memory deficits in the low-brainPAD group. That suggested that early cognitive dysfunction in BD-I was associated with a marked delay in age-related brain changes, and verbal memory was probably a core defect in BD-I. Meanwhile, cognitive differences were probably associated with various subtypes of BD. Patients with psychotic history and diagnosed with BD-I were more closely related to global cognitive impairment, including noticeably worse verbal memory, processing speed, executive function, social cognition, and working memory. Unfortunately, this difference has not been widely confirmed in oceans of studies, probably due to a mixture of varying symptom severity among the patients.32 What’s more, factors such as years of education, the number of hospitalizations, age, antipsychotic drugs, and childhood trauma have been also proven to affect cognition.14 A resting-state magnetic resonance imaging study observing the striatum in patients and HC explored mechanisms for different levels of cognition. BD-I patients may have lenient brain effects, which allows for increased “compensatory” functional connectivity and higher choline concentrations required in the striatum to preserve cognitive function.33
Research on the neurocognition of BD patients and their UFR demonstrate that the verbal intelligence quotient (IQ) of UFR drops apparently.34 And the verbal memory35 and facial expression recognition of those with global cognitive disorders are impaired, however, other non-emotional cognition is not impaired.36 Furthermore, UFR, compared to HC, exhibit an increased corrected intracranial volume,37 a larger regional cortical surface area mainly concentrating on speech-related auditory areas in the temporal lobe,38 bigger volume of the inferior frontal gyrus and decreased cerebellar volume;39 Compared to patients, there is no significant enlargement of the intracranial volume of relatives, which suggests genetics effects may result in different intracranial volumes.37 The association between familial predisposition to increased intracranial volume and IQ in BD’s relatives is unclear.
Admittedly, the amygdala and hippocampus are both involved in memory and learning. The right amygdala in BD-unstricken offspring exhibited significantly greater volume compared to BD-stricken offspring and HC. The amygdala may serve as a potential marker of susceptibility to BD.40 Patients have a smaller hippocampal volume with greater variability in volume compared to UFR.41 From the perspective of disease progression, late-stage patients has a reduction in hippocampal volume, and there was no significant difference in the early and middle stages compared to the HC. Middle-and-late patients have poorer immediate recall than early-stage patients and HC.42 The left para-hippocampal volume of BD relatives was larger than corresponding patients,43 and unaffected offspring also enlarging apparently in left para-hippocampus/hippocampal gray matter volume compared to age-matching HC.44
The Hypothesis of Neurodevelopmental Defects
There is wide-ranging controversy about the potential mechanisms contributing to the cognitive heterogeneity in BD. Studies of cognitive deficits in schizophrenia (SCZ) align with the neurodevelopmental etiological model and suggest cognitive deficits in patients with SCZ may emerge as early as childhood development, earlier than the onset of symptoms.45 Therefore, the researchers hypothesize whether the cognitive development of BD also applies to the above modal.
Some viewpoints argue that the more prominent neurodevelopmental problems in childhood, the higher the likelihood of developing BD with psychotic symptoms and the closer the alignment with the neurobiological characteristics of SCZ.46 Indeed, the offspring with psychopathology arising in early adulthood have been found to have worse cognitive outcomes in adulthood than the ones with psychopathology in late adulthood and healthy offspring. A cohort study of male conscripts recruited healthy male conscripts (average age of 19.9 years) and discovered impaired visual-spatial reasoning before the onset of BD, SCZ, and other psychiatric disorders and that the dose-response relationship is very clear.47 And most remarkably, the earlier the age of onset, the greater the impact on cognitive outcomes,48 which seems to validate this hypothesis.
Surprisingly, if comparing BD patients alone in the above study, researchers found the lower scores in arithmetic reasoning before onset did not necessarily indicate an increased risk of BD. This finding appears to contradict the previous understanding. Furthermore, other large-sample observational studies have discovered no deficits in patients’ cognition of early development. The result refutes the above theory. A cohort study with longitudinal follow-up recruited a total of 10,717 adolescent boys and young adult males in Sweden, where all subjects underwent cognitive tests at the age of 13 and were followed to observe the development of psychosis in adulthood. Although patient groups of SCZ and other non-affective psychosis all showed a certain degree of decline in cognitive function during early development, the results of BD demonstrated patients outperformed HC on all tasks at every time point before onset. Language decline at age 13 could be a valid diagnostic predictor.49 It is worth noting that another large sample cohort in Sweden (n=1,017,691) observed a U-shaped association between BD and social maturity (low extraversion and high neuroticism have been identified as characteristics of BD, with social maturity reflecting extraversion and responsibility).50 In response, Parellada proposed a linear risk trend for cognitive impairment in the SCZ but U-shaped risk trends in BD, more reasonably explaining the phenomenon of cognitive heterogeneity after compiling the articles about cognitive function and early developmental milestone data in SCZ and BD before onset. People at risk who are significantly higher or lower than the average cognitive function of their peers are more likely to develop BD eventually.51
Creativity
Creativity is the mental process of adopting new methods or approaches to solve problems and create entirely new value objects. As a complex and multidimensional brain function, creativity has cognitive and emotional components, which belongs to the most common process of human thinking and cognitive activity, with a certain degree of heritability. Since Aristotle proposed the viewpoint that “No Great Genius Has Ever Existed Without a Strain of Madness”, creative geniuses have often been associated with BD. Initially, evidence for this association was presented mainly in biographies and case studies of extremely creative individuals and in group studies of artists and composers.52 Subsequently, academic research on creativity and mental illness demonstrates a correlation between BD and creativity, professional achievement in specific fields such as humanities, arts, scientific research, and organizational leadership.
Writers and poets are more likely to suffer from mental illness than the HC, particularly mood disorders, and show a predisposition towards BD.53 The long-term emotional changes of famous writers such as Yu Dafu, Goethe, and Hemingway are closely related to their literary creativity.54,55 So a hypothesis was raised- “highly creative groups are at higher risk of developing BD” - and there is solid evidence to support it. BD is more prevalent in high-achieving language arts students.56,57 First- and second-degree relatives of university academics (defined as a highly creative population) were also discovered to have a higher risk of BD than the HC in a large-sample registry study.58
Surprisingly, Patients with BD and their UFR have increased creativity compared to the HC, which was confirmed in 29,644 individuals with major mental disorders. Both patients and their UFR wereS far more likely to be in creative occupations than the HC, and as the blood relationship with the patient diminishes, they are gradually less likely to engage in creative occupations.59 Remarkably, the proportion of creative occupations did not increase in the MDD group. Another large (N = 4,454,763) case-control study of BD, SCZ, and MDD and siblings showed an association with artistic creativity only in families with BD, but not in SCZ and MDD.60 What’s more, BD high-risk offspring also have higher Barron-Welsh Art Scale (BWAS) scores than the HC.61 BD and creative HC scored significantly higher on the BWAS-Total than MDD.62 A small-sample pilot study of MDD also concluded that patients with the risk of mania scored higher on BWAS than those without bipolar risk.63 Furthermore, patients in hypomania or stable asymptomatic phase scored higher than depressed states.64
In addition, some progress has been made in the genetics of BD and creativity. Some research investigated the relationship between music activity participation and mental health through polygenic scores and found that the higher the genetic risk of BD, the more participation.65 The GWAS study of creativity also supports a shared genetic basis between psychiatric disorders and creativity.66 Of course, despite the achievements of many BD patients, the majority of patients suffer from cognitive impairment and severe disability, leading to decreased psychosocial function and increased economic costs. This phenomenon is probably related to the spectrum of BD’s inverted-U model.52
Work and Educational Performance
Educational achievement and occupational difficulties among patients and UFR have received attention in recent years. Meta-analysis has shown that people with BD have impaired work ability, higher unemployment rates, divorce and widowhood, low participation in social activities, and weak family relationships.5 BD-I patients have worse psychosocial function than HC67 and apparent deficits in social perception and emotional perception related to social cognitive impairment.68
Patients with SCZ and MDD and their UFR and BD patients show poor academic performance at different stages of education, with SCZ patients showing the earliest decline. It’s consistent with the neurodevelopmental hypothesis in SCZ. And it’s worth noting that UFR with BD were not worse off in academic achievement at all educational stages than the HC overall, supporting the conclusion of cognitive heterogeneity.69 Consistently, data on the performance of 16-year-old students and their prevalence in adulthood in Sweden demonstrate that high-achieving students have a nearly fourfold increased risk of BD in adulthood and that the worst-achieving students also moderately increased their risk.56
50% of patients report problems with employment and work, including difficulty keeping a job, reduced productivity, greater absenteeism, and unsatisfactory earnings.30,70 They have three times the unemployment rate than HC and lose twice as much productivity as those with MDD.71 The relationship between subthreshold symptoms and cognition on work performance and disability deserves further investigation. Even euthymic patients have a long period of impaired function and unsatisfactory quality of life.72 However, the influential pathways between residual symptoms, cognition, and work performance are not entirely clear. In addition, UFR show the same relatively poor socio-economic status as the patient.73 But it remains to be explored whether the UFR’s working competence itself has declined - after all, their economic status is greatly influenced by the caring burden.
Social Functioning
People with BD appear to have more pronounced deficits in social functioning, including poorer interpersonal relationships, diminished interests and recreation, and less general satisfaction. It seems that BD patients are more isolated and communicate less with their neighbors than HC.6 Furthermore, intimate partners of patients are slightly more introverted, with narrower social circles and compromised psychosocial functioning compared to HC.74
A Danish Demographic Registry study assessed familial load (FL) in a large sample of first-degree relatives of BD patients and found that impaired social functioning may not be attributable to familial aggregation. Neither the patients nor their UFR experienced higher levels of functional deficits in the context of a higher burden of psychopathology. Further exploration into the causes of impaired social functioning may be worthwhile.73,75,76
BD and their UFR are often affected by varying degrees of social stress due to social interaction and financial factors. It exacerbates the emotional symptoms and further results in a heavy burden.77 The rate of disability service utilization among patients with MDD and BD is 2.03 times higher than that of HC, with the same rate among BD patients approximately 2.37 times higher than that of MDD patients. Cognitive deficits are an important cause of social function decline and occupational disorders.78 Therefore, improving the cognitive and social function of patients with BD is also a carefully considered aspect by clinicians.
Family Functioning
For the patient and UFR, the damaged family function reflects more in the burden of caregiving and emotional stress. Health insurance claims data show that patients have a heavy financial burden due to illness. In 2015, the total cost of medical care for BD-I in the United States was estimated at $202.1 billion ($81,559 per capita), and the total excess cost (the difference in medical costs between those diagnosed with BD-I and those without) was estimated at $119.8 billion, equivalent to $48,333 per capita.79 Another study showed that the All-cause total health care for patients diagnosed with BD-I alone and no other mental disorders was $26,396, compared to $51,085 for people diagnosed with SCZ and BD-I.80 Annual Medicare payments for BD-I are much higher than for many other mental illnesses. The out-of-pocket cost per capita was estimated at $568 in 2003, twice as high as other mental illnesses.81 The latest longitudinal cohort study suggested that BD patients’ average annual direct medical costs have risen by €6910. However, the costs could be dropped by more than 50% based on two-year follow-up observations for the subgroup with skilled nursing treatment.82 Notably, in addition to the cost of treatment, impaired academic performance, unemployment, loss of productivity, and reduced interpersonal interactions due to symptoms and cognitive impairment also impose incalculable financial costs on patients.83
Moreover, the burden faced by BD families cannot be ignored. More than 90% of families have reported it.84 On the one hand, it is reflected in families with children and adolescents. The marital survival for parents of pediatric patients is associated with family stress, and the speculation is that it may cause conflicts about children’s management. Families with young people with BD are worse at problem-solving and communication.85 Such families show more quarrels, parent relationship tension, negative emotional expression, lower intimacy, cohesion, intellectual-cultural orientation, and active entertainment behaviors.86,87 The functional impairment of the family mentioned above is affected by the age of the offspring and is mainly mediated by the psychosocial functioning of the parents.88 But it has to be said it’s acknowledged that better family function and parenting skills for children with BD can help improve treatment and function.89 On the other hand, BD also significantly impacts the spouse of an adult with BD, including caregiving burdens, marriage, self-sacrifice, and personal development.90,91
Inverted-U Hypothesis
The broad spectrum of BD includes typical manic and depressive symptoms as well as cyclothymic and hypomanic. Based on the classification of affective states, they can be divided into hyperactive, depressive, irritable, and cyclothymic moods.92 Studies have shown that UFR is more likely to be diagnosed with cyclothymic temperament (CT) than the general population. After examining emotional temperament and cognitive function in symptomatic offspring (SO) and without asymptomatic offspring (AO), it’s found that the SO group has higher emotional temperament scores than the AO group and that those in the SO and AO groups who are CT have a higher cognitive function such as processing speed, verbal learning, and attention, than in the other emotional states. BD’s cognitive functions and emotional temperament may share a common neurogenetic basis.93 BD represents an overall continuous and dimensional phenotypic change in temperament, personality, and cognition of the population, and the studies about cognitive, creative and emotional temperament support the U-shaped distribution pattern. Greenwood argued that the U-shaped pathology hypothesis is a result of the cumulative effect of small effector genes.52 Positive traits such as creativity and cognition may be enhanced with increased genetic risk. However, once the genetic risk for bipolar disorder reaches a critical threshold, these positive traits are attenuated as the genetic load continues to increase. This relationship shows a distribution similar to an inverted “U” curve, which can be seen in more detail in Figure 1.
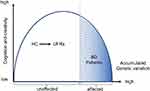 |
Figure 1 Inverted-U model of positive features such as cognition and creativity in BD patients. |
Conclusions
Over the past decade, increasing attention has been focused on the functional performance of patients with BD as well as UFR. This is due to the high prevalence, misdiagnosis, delayed diagnosis, and progressive neurologic impairment experienced by patients, which has a critical impact on their work, school, and social interactions. One of the main goals of clinical treatment and scientific research is to achieve remission of clinical symptoms while focusing on restoring cognitive and psychosocial functioning. Of particular importance are those functions that are closely related to the patient’s professional accomplishments, such as cognition, creativity, and IQ. Although some studies support the hypothesis of an inverted U-shaped relationship between positive traits such as cognition and creativity and genetic risk in patients with bipolar disorder, more large-scale cohort studies and meta-analyses are needed to validate this idea. Indeed, the heterogeneity of positive traits such as cognitive functioning and creativity in BD patients and UFR is triggered by a common set of genetic risk genes that lead to structural and functional changes in specific brain regions. In addition, the burden on the whole family increases due to high unemployment and poorer interpersonal relationships in patients, while UFR show a decline in economic status and well-being. However, to date, no large-scale longitudinal studies have been conducted to monitor the performance of BD patients and their UFR across the three dimensions of quality of life, symptoms, functioning, and cognition. The urgent task at hand is to determine the relationship between psychosocial functioning, cognition, and clinical variables, and to find clinical predictors and interventions that influence the prognosis of functioning in order to improve the level of functioning of patients, to help those severely afflicted by dysfunction to return to work, and to alleviate the burden on them, as well as on their families.
Acknowledgments
The authors of this article would like to thank the funding support from the National Natural Science Foundation of China (81761128032, 81930033, 81771465), the Clinical Research Plan of SHDC (SHDC12020126), Key Area Research and Development Program of Guangdong Province (2018B030334001), Clinical Research Center of Shanghai Mental Health Center Key Project (CRC2021ZD01, CRC2021DX01), Shanghai Key Clinical Specialties Construction Project (Psychiatry and Mental Health), Shanghai Clinical Research Center for Mental Health (19MC1911100).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2016;387(10027):1561–1572. doi:10.1016/s0140-6736(15)00241-x
2. Gbdmd C. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–150. doi:10.1016/S2215-0366(21)00395-3
3. Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi:10.1016/S2215-0366(18)30511-X
4. Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. doi:10.1111/bdi.12609
5. Chen M, Fitzgerald HM, Madera JJ, Tohen M. Functional outcome assessment in bipolar disorder: a systematic literature review. Bipolar Disord. 2019;21(3):194–214. doi:10.1111/bdi.12775
6. Sanchez-Moreno J, Martinez-Aran A, Tabares-Seisdedos R, Torrent C, Vieta E, Ayuso-Mateos JL. Functioning and disability in bipolar disorder: an extensive review. Psychother Psychosom. 2009;78(5):285–297. doi:10.1159/000228249
7. Cerullo MA, Adler CM, Delbello MP, Strakowski SM. The functional neuroanatomy of bipolar disorder. Int Rev Psychiatry. 2009;21(4):314–322. doi:10.1080/09540260902962107
8. Radua J, Grunze H, Amann BL. Meta-analysis of the risk of subsequent mood episodes in bipolar disorder. Psychother Psychosom. 2017;86(2):90–98. doi:10.1159/000449417
9. Kessing LV, Andersen PK. Evidence for clinical progression of unipolar and bipolar disorders. Acta Psychiatr Scand. 2017;135(1):51–64. doi:10.1111/acps.12667
10. Sherwood SN, Carlson GA, Freeman AJ. Decreasing rate of inpatient pediatric bipolar disorder diagnosis in the US between 2004 and 2010. Bipolar Disord. 2022;24(2):149–160. doi:10.1111/bdi.13145
11. Post RM, Altshuler LL, Kupka R, et al. Double jeopardy in the United States: early onset bipolar disorder and treatment delay. Psychiatry Res. 2020;292:113274. doi:10.1016/j.psychres.2020.113274
12. Hu C, Xiang YT, Ungvari GS, et al. Undiagnosed bipolar disorder in patients treated for major depression in China. J Affect Disord. 2012;140(2):181–186. doi:10.1016/j.jad.2012.02.014
13. Smith DJ, Griffiths E, Kelly M, Hood K, Craddock N, Simpson SA. Unrecognised bipolar disorder in primary care patients with depression. Br J Psychiatry. 2011;199(1):49–56. doi:10.1192/bjp.bp.110.083840
14. Rabelo-da-ponte FD, Lima FM, Martinez-Aran A, et al. Data-driven cognitive phenotypes in subjects with bipolar disorder and their clinical markers of severity. Psychol Med. 2022;52(9):1728–1735. doi:10.1017/s0033291720003499
15. Chakrabarty T, Torres IJ, Su WW, Sawatzky R, Keramatian K, Yatham LN. Cognitive subgroups in first episode bipolar I disorder: relation to clinical and brain volumetric variables. Acta Psychiatr Scand. 2021;143(2):151–161. doi:10.1111/acps.13245
16. Gordovez FJA, McMahon FJ. The genetics of bipolar disorder. Mol Psychiatry. 2020;25(3):544–559. doi:10.1038/s41380-019-0634-7
17. Lau P, Hawes DJ, Hunt C, Frankland A, Roberts G, Mitchell PB. Prevalence of psychopathology in bipolar high-risk offspring and siblings: a meta-analysis. Eur Child Adolesc Psychiatry. 2018;27(7):823–837. doi:10.1007/s00787-017-1050-7
18. Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr Bull. 2014;40(1):28–38. doi:10.1093/schbul/sbt114
19. Stapp EK, Mendelson T, Merikangas KR, Wilcox HC. Parental bipolar disorder, family environment, and offspring psychiatric disorders: a systematic review. J Affect Disord. 2020;268:69–81. doi:10.1016/j.jad.2020.03.005
20. Mesman E, Nolen WA, Reichart CG, Wals M, Hillegers MH. The Dutch bipolar offspring study: 12-year follow-up. Am J Psychiatry. 2013;170(5):542–549. doi:10.1176/appi.ajp.2012.12030401
21. Birmaher B, Merranko J, Hafeman D, et al. A longitudinal study of psychiatric disorders in offspring of parents with bipolar disorder from preschool to adolescence. J Am Acad Child Adolesc Psychiatry. 2021;60(11):1419–1429. doi:10.1016/j.jaac.2021.02.023
22. Snijders G, Mesman E, de Wit H, et al. Immune dysregulation in offspring of a bipolar parent. Altered serum levels of immune growth factors at adolescent age. Brain Behav Immun. 2017;64:116–123. doi:10.1016/j.bbi.2017.04.004
23. Stahl EA, Breen G, Forstner AJ, et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat Genet. 2019;51(5):793–803. doi:10.1038/s41588-019-0397-8
24. Li HJ, Zhang C, Hui L, et al. Novel risk loci associated with genetic risk for bipolar disorder among Han Chinese individuals: a Genome-Wide Association Study and meta-analysis. JAMA Psychiatry. 2021;78(3):320–330. doi:10.1001/jamapsychiatry.2020.3738
25. Koenders MA, Mesman E, Giltay EJ, Elzinga BM, Hillegers MHJ. Traumatic experiences, family functioning, and mood disorder development in bipolar offspring. Br J Clin Psychol. 2020;59(3):277–289. doi:10.1111/bjc.12246
26. Smoller JW, Finn CT. Family, twin, and adoption studies of bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;123C(1):48–58. doi:10.1002/ajmg.c.20013
27. Miskowiak KW, Jespersen AE, Obenhausen K, et al. Internet-based cognitive assessment tool: sensitivity and validity of a new online cognition screening tool for patients with bipolar disorder. J Affect Disord. 2021;289:125–134. doi:10.1016/j.jad.2021.04.039
28. Miskowiak K, Gjerullf-Hansen C, Jensen M, Nielsen S, Ott C. Udredning og behandling af kognitive vanskeligheder ved affektive lidelser [Assessment and treatment of cognitive impairments in patients with affective disorders]. Ugeskr Laeger. 2019;181(45): V04190234. Danish
29. Keramatian K, Torres IJ, Yatham LN. Neurocognitive functioning in bipolar disorder: what we know and what we don’t. Dialogues Clin Neurosci. 2021;23(1):29–38. doi:10.1080/19585969.2022.2042164
30. Dominiak M, Jazdzyk P, Antosik-Wojcinska AZ, et al. The impact of bipolar spectrum disorders on professional functioning: a systematic review. Front Psychiatry. 2022;13:951008. doi:10.3389/fpsyt.2022.951008
31. Chakrabarty T, Frangou S, Torres IJ, Ge R, Yatham LN. Brain age and cognitive functioning in first-episode bipolar disorder. Psychol Med. 2022;1–9. doi:10.1017/S0033291722002136
32. Bora E. Neurocognitive features in clinical subgroups of bipolar disorder: a meta-analysis. J Affect Disord. 2018;229:125–134. doi:10.1016/j.jad.2017.12.057
33. Okanda Nyatega C, Qiang L, Jajere Adamu M, Bello Kawuwa H. Altered striatal functional connectivity and structural dysconnectivity in individuals with bipolar disorder: a resting state magnetic resonance imaging study. Front Psychiatry. 2022;13:1054380. doi:10.3389/fpsyt.2022.1054380
34. McCormack C, Green MJ, Rowland JE, et al. Neuropsychological and social cognitive function in young people at genetic risk of bipolar disorder. Psychol Med. 2016;46(4):745–758. doi:10.1017/S0033291715002147
35. Russo M, Van Rheenen TE, Shanahan M, et al. Neurocognitive subtypes in patients with bipolar disorder and their unaffected siblings. Psychol Med. 2017;47(16):2892–2905. doi:10.1017/s003329171700143x
36. Kjærstad HL, Eikeseth FF, Vinberg M, Kessing LV, Miskowiak K. Neurocognitive heterogeneity in patients with bipolar disorder and their unaffected relatives: associations with emotional cognition. Psychol Med. 2021;51(4):668–679. doi:10.1017/s0033291719003738
37. de Zwarte SMC, Brouwer RM, Agartz I, et al. The association between familial risk and brain abnormalities is disease specific: an ENIGMA-relatives study of schizophrenia and bipolar disorder. Biol Psychiatry. 2019;86(7):545–556. doi:10.1016/j.biopsych.2019.03.985
38. de Zwarte SMC, Brouwer RM, Agartz I, et al. Intelligence, educational attainment, and brain structure in those at familial high-risk for schizophrenia or bipolar disorder. Hum Brain Mapp. 2022;43(1):414–430. doi:10.1002/hbm.25206
39. Saricicek A, Yalin N, Hidiroglu C, et al. Neuroanatomical correlates of genetic risk for bipolar disorder: a voxel-based morphometry study in bipolar type I patients and healthy first degree relatives. J Affect Disord. 2015;186:110–118. doi:10.1016/j.jad.2015.06.055
40. Bauer IE, Sanches M, Suchting R, et al. Amygdala enlargement in unaffected offspring of bipolar parents. J Psychiatr Res. 2014;59:200–205. doi:10.1016/j.jpsychires.2014.08.023
41. Angelescu I, Brugger SP, Borgan F, Kaar SJ, Howes OD. The magnitude and variability of brain structural alterations in bipolar disorder: a double meta-analysis of 5534 patients and 6651 healthy controls. J Affect Disord. 2021;291:171–176. doi:10.1016/j.jad.2021.04.090
42. Cao B, Passos IC, Mwangi B, et al. Hippocampal volume and verbal memory performance in late-stage bipolar disorder. J Psychiatr Res. 2016;73:102–107. doi:10.1016/j.jpsychires.2015.12.012
43. Roberts G, Lenroot R, Frankland A, et al. Abnormalities in left inferior frontal gyral thickness and parahippocampal gyral volume in young people at high genetic risk for bipolar disorder. Psychol Med. 2016;46(10):2083–2096. doi:10.1017/S0033291716000507
44. Ladouceur CD, Almeida JRC, Birmaher B, et al. Subcortical gray matter volume abnormalities in healthy bipolar offspring: potential neuroanatomical risk marker for bipolar disorder? J Am Acad Child Adolesc Psychiatry. 2008;47(5):532–539. doi:10.1097/CHI.0b013e318167656e
45. Reichenberg A, Caspi A, Harrington H, et al. Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. Am J Psychiatry. 2010;167(2):160–169. doi:10.1176/appi.ajp.2009.09040574
46. Valli I, Fabbri C, Young AH. Uncovering neurodevelopmental features in bipolar affective disorder. Br J Psychiatry. 2019;215(1):383–385. doi:10.1192/bjp.2019.117
47. Tiihonen J, Haukka J, Henriksson M, et al. Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts. Am J Psychiatry. 2005;162(10):1904–1910. doi:10.1176/appi.ajp.162.10.1904
48. Tempelaar WM, Mesman E, Breetvelt EJ, Hillegers MHJ. The Dutch Bipolar Offspring Study: cognitive development and psychopathology. J Abnorm Child Psychol. 2019;47(9):1559–1567. doi:10.1007/s10802-019-00532-7
49. MacCabe JH, Wicks S, Lofving S, et al. Decline in cognitive performance between ages 13 and 18 years and the risk for psychosis in adulthood: a Swedish longitudinal cohort study in males. JAMA Psychiatry. 2013;70(3):261–270. doi:10.1001/2013.jamapsychiatry.43
50. Hayes JF, Osborn DPJ, Lewis G, Dalman C, Lundin A. Association of late adolescent personality with risk for subsequent serious mental illness among men in a Swedish Nationwide Cohort Study. JAMA Psychiatry. 2017;74(7):703–711. doi:10.1001/jamapsychiatry.2017.0583
51. Parellada M, Gomez-Vallejo S, Burdeus M, Arango C. Developmental differences between schizophrenia and bipolar disorder. Schizophr Bull. 2017;43(6):1176–1189. doi:10.1093/schbul/sbx126
52. Greenwood TA. Creativity and bipolar disorder: a shared genetic vulnerability. Annu Rev Clin Psychol. 2020;16:239–264. doi:10.1146/annurev-clinpsy-050718-095449
53. Andreasen NC. Creativity and mental illness: prevalence rates in writers and their first-degree relatives. Am J Psychiatry. 1987;144(10):1288–1292. doi:10.1176/ajp.144.10.1288
54. Chen Z, Xiao S. How does affective disorder relate to creativity? The pathography of the Chinese Writer Yu Dafu. Psychopathology. 2020;53(1):1–7. doi:10.1159/000503394
55. Mason OJ, Mort H, Woo J. Research Letter: investigating psychotic traits in poets. Psychol Med. 2015;45(3):667–669. doi:10.1017/s0033291714002670
56. MacCabe JH, Lambe MP, Cnattingius S, et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br J Psychiatry. 2010;196(2):109–115. doi:10.1192/bjp.bp.108.060368
57. Pedersen SD, Østergaard SD, Petersen L. The association between school exam grades and subsequent development of bipolar disorder. Acta Neuropsychiatr. 2018;30(4):209–217. doi:10.1017/neu.2018.3
58. Parnas J, Sandsten KE, Vestergaard CH, Nordgaard J. Schizophrenia and bipolar illness in the relatives of university scientists: an epidemiological report on the creativity-psychopathology relationship. Front Psychiatry. 2019;10:175. doi:10.3389/fpsyt.2019.00175
59. Kyaga S, Lichtenstein P, Boman M, Hultman C, Långström N, Landén M. Creativity and mental disorder: family study of 300 000 people with severe mental disorder. Br J Psychiatry. 2011;199(5):373–379. doi:10.1192/bjp.bp.110.085316
60. MacCabe JH, Sariaslan A, Almqvist C, Lichtenstein P, Larsson H, Kyaga S. Artistic creativity and risk for schizophrenia, bipolar disorder and unipolar depression: a Swedish population-based case-control study and sib-pair analysis. Br J Psychiatry. 2018;212(6):370–376. doi:10.1192/bjp.2018.23
61. Simeonova DI, Chang KD, Strong C, Ketter TA. Creativity in familial bipolar disorder. J Psychiatr Res. 2005;39(6):623–631. doi:10.1016/j.jpsychires.2005.01.005
62. Santosa CM, Strong CM, Nowakowska C, Wang PW, Rennicke CM, Ketter TA. Enhanced creativity in bipolar disorder patients: a controlled study. J Affect Disord. 2007;100(1–3):31–39. doi:10.1016/j.jad.2006.10.013
63. Burkhardt E, Pfennig A, Breitling G, et al. Creativity in persons at-risk for bipolar disorder-A pilot study. Early Interv Psychiatry. 2019;13(5):1165–1172. doi:10.1111/eip.12748
64. Miller N, Perich T, Meade T. Depression, mania and self-reported creativity in bipolar disorder. Psychiatry Res. 2019;276:129–133. doi:10.1016/j.psychres.2019.05.006
65. Wesseldijk LW, Lu Y, Karlsson R, Ullén F, Mosing MA. A comprehensive investigation into the genetic relationship between music engagement and mental health. Transl Psychiatry. 2023;13(1):15. doi:10.1038/s41398-023-02308-6
66. Li H, Zhang C, Cai X, et al. Genome-wide association study of creativity reveals genetic overlap with psychiatric disorders, risk tolerance, and risky behaviors. Schizophr Bull. 2020;46(5):1317–1326. doi:10.1093/schbul/sbaa025
67. Dou W, Yu X, Fang H, et al. Family and psychosocial functioning in bipolar disorder: the mediating effects of social support, resilience and suicidal Ideation. Front Psychol. 2021;12:807546. doi:10.3389/fpsyg.2021.807546
68. Easwaran K, Palaniappan P. Social cue recognition and attributional bias in remitted bipolar disorder: impact on social functioning. Psychiatry Res. 2021;306:114300. doi:10.1016/j.psychres.2021.114300
69. Tempelaar WM, Termorshuizen F, MacCabe JH, Boks MP, Kahn RS. Educational achievement in psychiatric patients and their siblings: a register-based study in 30 000 individuals in The Netherlands. Psychol Med. 2017;47(4):776–784. doi:10.1017/S0033291716002877
70. Depp CA, Mausbach BT, Bowie C, et al. Determinants of occupational and residential functioning in bipolar disorder. J Affect Disord. 2012;136(3):812–818. doi:10.1016/j.jad.2011.09.035
71. Laxman KE, Lovibond KS, Hassan MK. Impact of bipolar disorder in employed populations. Am J Manag Care. 2008;14(11):757–764.
72. Zhang X, Cheng X, Chen J, et al. Association of subthreshold manic symptoms and cognitive impairments in euthymic patients with bipolar disorder I. Psychiatry Res. 2019;278:303–308. doi:10.1016/j.psychres.2019.06.032
73. Sletved KSO, Coello K, Stanislaus S, et al. Socio-economic status and functioning in patients newly diagnosed with bipolar disorder and their unaffected siblings - Results from a cross-sectional clinical study. J Affect Disord. 2022;310:404–411. doi:10.1016/j.jad.2022.05.023
74. Serravalle L, Iacono V, Hodgins S, Ellenbogen MA. A comprehensive assessment of personality traits and psychosocial functioning in parents with bipolar disorder and their intimate partners. Int J Bipolar Disord. 2020;8(1):8. doi:10.1186/s40345-019-0172-x
75. Sletved KSO, Ziersen SC, Andersen PK, Vinberg M, Kessing LV. Socio-economic functioning in patients with bipolar disorder and their unaffected siblings - results from a nation-wide population-based longitudinal study. Psychol Med. 2021:1–8. doi:10.1017/S0033291721002026
76. Sletved KSO, Maiggaard K, Thorup AAE, Kessing LV, Vinberg M. Familial load of psychiatric disorders and overall functioning in patients newly diagnosed with bipolar disorder and their unaffected first-degree relatives. Int J Bipolar Disord. 2022;10(1):28. doi:10.1186/s40345-022-00277-1
77. Fares-Otero NE, Martinez-Aran A. Social stress in bipolar disorder. Eur Neuropsychopharmacol. 2022;60:22–24. doi:10.1016/j.euroneuro.2022.04.002
78. Frey BN, Vigod S, de Azevedo Cardoso T, et al. The early burden of disability in individuals with mood and other common mental disorders in Ontario, Canada. JAMA Netw Open. 2020;3(10):e2020213. doi:10.1001/jamanetworkopen.2020.20213
79. Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;226:45–51. doi:10.1016/j.jad.2017.09.011
80. Broder MS, Greene M, Chang E, et al. Health care resource use, costs, and diagnosis patterns in patients with schizophrenia and bipolar disorder: real-world evidence from US Claims Databases. Clin Ther. 2018;40(10):1670–1682. doi:10.1016/j.clinthera.2018.08.004
81. Peele PB, Xu Y, Kupfer DJ. Insurance expenditures on bipolar disorder: clinical and parity implications. Am J Psychiatry. 2003;160(7):1286–1290. doi:10.1176/appi.ajp.160.7.1286
82. Laidi C, Godin O, Etain B, et al. Direct medical cost of bipolar disorder: insights from the FACE-BD longitudinal cohort. J Affect Disord. 2022;306:223–231. doi:10.1016/j.jad.2022.02.071
83. Miller S, Dell’Osso B, Ketter TA. The prevalence and burden of bipolar depression. J Affect Disord. 2014;169(Suppl 1):S3–S11. doi:10.1016/S0165-0327(14)70003-5
84. Maji KR, Sood M, Sagar R, Khandelwal SK. A follow-up study of family burden in patients with bipolar affective disorder. Int J Soc Psychiatry. 2012;58(2):217–223. doi:10.1177/0020764010390442
85. MacPherson HA, Ruggieri AL, Christensen RE, et al. Developmental evaluation of family functioning deficits in youths and young adults with childhood-onset bipolar disorder. J Affect Disord. 2018;235:574–582. doi:10.1016/j.jad.2018.04.078
86. Perez Algorta G, MacPherson HA, Youngstrom EA, et al. Parenting stress among caregivers of children with bipolar spectrum disorders. J Clin Child Adolesc Psychol. 2018;47(sup1):S306–S320. doi:10.1080/15374416.2017.1280805
87. Reinares M, Bonnin CM, Hidalgo-Mazzei D, et al. Family functioning in bipolar disorder: characteristics, congruity between patients and relatives, and clinical correlates. Psychiatry Res. 2016;245:66–73. doi:10.1016/j.psychres.2016.08.010
88. Shalev A, Merranko J, Goldstein T, et al. A Longitudinal Study of family functioning in offspring of parents diagnosed with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(10):961–970. doi:10.1016/j.jaac.2018.10.011
89. MacPherson HA, Weinstein SM, Henry DB, West AE. Mediators in the randomized trial of Child- and Family-Focused Cognitive-Behavioral Therapy for pediatric bipolar disorder. Behav Res Ther. 2016;85:60–71. doi:10.1016/j.brat.2016.08.014
90. Naqvi TF, Dasti R, Khan N. Emotional journey of wives of spouses diagnosed with bipolar I disorder: moving from vicissitude towards reconciliation. Int J Qual Stud Health Wellbeing. 2021;16(1):1946926. doi:10.1080/17482631.2021.1946926
91. Azorin JM, Lefrere A, Belzeaux R. The impact of bipolar disorder on couple functioning: implications for care and treatment. A systematic review. Medicina. 2021;57(8). doi:10.3390/medicina57080771
92. Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23(1):68–73.
93. Liu T, Xu G, Lu W, et al. Affective temperament traits measured by TEMPS-A and their associations with cognitive functions among offspring of parents with bipolar disorder with and without subthreshold symptoms. J Affect Disord. 2021;283:377–383. doi:10.1016/j.jad.2021.01.061
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
