Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Frequency and Characteristics of Depression and Its Association with Diminished Quality of Life in a Cohort of Individuals with Post-Acute Sequelae of COVID-19
Authors Shahar S, Lynch S , Dornbush R, Klepacz L, Smiley A , Ferrando SJ
Received 21 July 2023
Accepted for publication 20 September 2023
Published 3 October 2023 Volume 2023:19 Pages 2069—2079
DOI https://doi.org/10.2147/NDT.S427957
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Sivan Shahar,1,2 Sean Lynch,1,3 Rhea Dornbush,1,4 Lidia Klepacz,1,4 Abbas Smiley,5 Stephen J Ferrando1,4
1Department of Psychiatry and Behavioral Sciences, New York Medical College, Valhalla, NY, USA; 2Department of Psychiatry, Icahn School of Medicine at Mount Sinai, Mount Sinai Hospital, New York City, NY, USA; 3Department of Psychiatry, Icahn School of Medicine at Mount Sinai, Mount Sinai Beth Israel, New York City, NY, USA; 4Department of Psychiatry, Westchester Medical Center Health System, Valhalla, NY, USA; 5Department of Surgery, Westchester Medical Center Health System, Valhalla, NY, USA
Correspondence: Stephen J Ferrando, Department of Psychiatry, Westchester Medical Center Health System, New York Medical College, 100 Woods Road, Valhalla, NY, 10595, USA, Tel +1 914-493-1905, Fax +1 914-493-1015, Email [email protected]
Background: Approximately one-third of COVID-19 survivors will experience persistent symptoms, which may include neurological and psychiatric disturbances. Previous research has suggested that up to 45% of people develop clinically significant depressive symptoms post-COVID. This study sought to determine frequency, symptom profile, and clinical correlates of depression post-COVID.
Methods: Seventy-five participants who had recovered from COVID-19 underwent neurocognitive, psychiatric, medical, and cognitive testing/screening. The primary measures of interest in this report included the Patient Health Questionnaire (PHQ-9), a 9-item depression-screening tool, and the Endicott Quality of Life Enjoyment and Satisfaction Questionnaire.
Results: One-third of study participants screened as positive on the PHQ-9 for clinically significant depression, with the most commonly reported symptom being fatigue, followed by sleep disturbance and poor concentration. Also reported were decreased satisfaction in employment, sexual life, and mood. Depressed patients described greater illness severity during COVID-19 infection and subjective cognitive impairment, which was not found on neurocognitive testing. The only significant predictor of depression was COVID-19 illness severity.
Limitations: A significant portion of participants was a clinical population with specific post-COVID complaints and was predominately comprised of white females. Formal psychiatric evaluation was not performed.
Conclusion: Many individuals may experience depression after COVID-19 infection, with symptoms appearing to be predominately somatic in nature and correspond with COVID-19 illness severity.
Keywords: COVID-19, depression, quality of life, neuropsychological testing
Introduction
As of September 2023, more than 100 million Americans have been infected with the SARS-CoV-2 virus, the virus which causes COVID-19, and over 1 million have died.1 One-third of those who survive will experience persistent, and often debilitating symptoms even months after recovering from acute COVID-19 infection. This phenomenon has been dubbed “Post-Acute Sequelae of COVID-19” (PASC), or “Long-COVID”. Accumulating data indicate that a significant proportion of people who have been previously infected with COVID-19 are now suffering from mental health consequences.2 These symptoms appear to be more prevalent in individuals recovering from COVID-19 as compared to those recovering from other respiratory diseases, such as influenza.3
While there has been progress made in delineating some of the psychiatric outcomes of PASC, specifically depression, the existing studies are limited in scope.4 Firstly, many rely on online population-based surveys or medical record reviews, with limited information regarding prior psychiatric history, current treatments, or measures of other psychiatric domains.5 In addition, most individuals were not screened with validated clinical tools, such as the Patient Health Questionnaire-9 (PHQ-9), to measure the prevalence and severity of depression. The PHQ-9 provides a snapshot of symptom profiles in patients with PASC as it relates to DSM-V depression criteria.6 Finally, few included an assessment of quality of life to ascertain the relationship of these depressive symptoms to psychosocial functioning.
The pathophysiological mechanism of depression post-COVID-19 is also speculative. It is likely to be multifactorial, including prior psychiatric vulnerability, pandemic-related economic and psychosocial distress, and biological, related to the inflammatory-immune response to SARS-CoV2 and medical comorbidities, among others. It is thought that increases in pro-inflammatory cytokines, such as TNF-α, IL-1β, and IL-6, as well as other immune mediators activated by COVID-19, increase the permeability of the blood-brain-barrier, resulting in downstream changes in neurocircuitry, neurotransmission, and the hypothalamic–pituitary–adrenal (HPA) axis, ultimately leading to vulnerability to depression.4
The current study sought to address limitations in the general body of literature regarding the frequency, onset, characteristics and risk factors for depression after COVID-19 by analyzing data from a cohort that underwent an in-person neuropsychological assessment 6–8 months after acute infection. Investigators sought to determine the frequency of clinically significant depression in individuals with PASC; the symptom profiles of depression in PASC; the sociodemographic, medical, and neurocognitive factors associated with depression in PASC; the association between clinically significant depression and specific aspects of quality of life in PASC; and the inflammatory markers that correlate with depressive symptoms in PASC.
Methods
This study was conducted at Westchester Medical Center Health System (WMC Health)/New York Medical College (NYMC) in Valhalla, New York. The study complies with the Declaration of Helsinki and was approved by both the Institutional Review Board of NYMC (Protocol #14400) and the WMCHealth Clinical Research Institute. The results presented here were obtained from 75 recruited via flyers, social media, email and word-of-mouth. A subset of study participants was referred from the WMCHealthPost-COVID-19 Recovery Program. Participants were screened for eligibility to participate by the investigators (SL, SS) based on inclusion criteria: 1) Age at least 20 years old; 2) documented positive COVID-19 nasopharyngeal test or positive antibody test prior to vaccination; 3) recovery from acute COVID-19 infection as per CDC recommendations (10–20 days after symptom onset and 24 hours without fever); 4) completed a minimum 8th grade education; 5) fluent in English; and 6) capable of signing informed consent. Persons with a prior diagnosis of a major neurocognitive disorder, traumatic brain injury with loss of consciousness, uncorrected visual/hearing deficits, intellectual disability, or unstable psychiatric symptoms were excluded.
Eligible participants met with the study assessors (SL, SS) who were trained to perform and score the assessment battery. During this visit, all risks and benefits were explained to prospective participants, and signed informed consent was obtained. Participants were compensated $40.00 for their time.
Study Measurements and Instruments
The primary measure of interest in this study was the PHQ-9, a 9-item self-administered clinical screening tool used in the diagnosis of depression and the measurement of depression severity.6 The PHQ-9 score ranges from 0 to 27, with each question being scored from 0 (not at all) to 3 (nearly every day). PHQ-9 scores are often divided into the following sub-categories based on severity: 0–4 (none-minimal), 5–9 (mild), 10–14 (mild-moderate), 15–19 (moderate-severe) and 20 and above (severe).6 As a screening tool in medical and psychiatric practice, a cutoff score of ≥10 on the PHQ-9 is utilized to trigger further evaluation and treatment, with formal psychiatric evaluation being the gold-standard method of diagnosing psychiatric illness.7 For major depression diagnosis, a criterion-based strategy can be used: Major Depression is present if 5 or more (out of the 9) depressive symptoms are present for “more than half of the days” over the previous 2 weeks, with 1 of the symptoms being depressed mood or anhedonia. This would be a more conservative and diagnostically accurate method to diagnose depression compared to cutoff scoring and is thus employed in this study in order to screen for clinically significant depression. Regardless of duration, if participants respond to the question related to having “thoughts that you would be better off dead or of hurting yourself in some way”, it is included towards a diagnosis of depression.6 Additionally, the final item on the PHQ-9 scale asks the participant “How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?”, which is used to measure functional impairment and assist in formal diagnosis. To examine the severity of individual symptoms, a score of 2 (more than half the days) or 3 (nearly every day) was scored as experiencing that symptom.
The Endicott Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) was used to characterize quality of life in this population.8 The Q-LES-Q queries multiple domains of life enjoyment and satisfaction (eg, mood, occupational and social functioning). The scale has a maximum of 70, with raw scores converted into a total percentage, with higher percentage scores indicating greater quality of life.8 Prior studies have examined the relationship between psychiatric illnesses and subjective quality of life and found significant and substantial impairment across multiple domains in trial participants suffering from affective disorders.9 Specifically, subjects with major depressive disorder tend to score the lowest on the sexual drive, mood, economic status, and household activities scales.9
Sociodemographic measures obtained from the participants included age, gender, ethnicity, relationship status, years of education and current employment. Medical measures included a self-reported medical history and a detailed history of COVID-19 illness. Participants were assessed on their daily functioning, using the Lawton-Brody Instrumental Activities of Daily Living Scale (IADL) which measures practical aspects of everyday functioning on a scale of 0–8.10 Study participants were also evaluated for fatigue using the Chalder Fatigue Scale (CFS-11), an 11-item questionnaire measuring the severity of mental and physical fatigue and is scored from 0 to 33. A cutoff score of >21 is considered clinically significant fatigue.11 Psychiatric information included prior psychiatric treatment, substance use history, and self-reported questionnaires including the Post Traumatic Stress Disorder Checklist for DSM-5 (PCL-5) which has a maximum score of 80, and for which a score of ≥33 indicates PTSD; and the Generalized Anxiety Disorder-7 (GAD-7) which is scored from 0 to 21, with a score ≥10 indicating a possible anxiety disorder.12,13
The neurocognitive battery used in this study included the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) Form A, which is an assessment designed to identify and characterize abnormal cognitive decline, and yields both a Total Score as well as sub-scores for five cognitive domains.14 Also included was the MoCA, a 30-point screening test scored from 0 to 30, with a score below 26 possibly indicative of cognitive impairment.15 Participants additionally completed the Patient Assessment of Own Function (PAOF), which queries subjective cognitive complaints yielding an average score of 0–5 for multiple domains, including memory, language and communication and cognitive/intellectual functioning, and for which a higher score indicates greater subjective impairment.16
Serological samples were obtained from a subset of participants and assayed for CRP, IL-6, and TNF-α, as these proinflammatory markers have previously been associated with neurocognitive and psychiatric disorders, both in general and in relation to COVID-19.4,17 Assays were performed by the Mayo Clinic Laboratories, and standardized reference ranges were used, whereas the following are considered elevated: CRP > 8.0 mg/L, IL-6 > 1.8 pg/mL, and TNF-α > 2.8 pg/mL.
Analyses were conducted on the entire sample of 75 participants and on two subgroups – a “Depressed” and a “Non-Depressed” Group. The “Depressed” subgroup consisted of participants who were screened as positive using the criterion-based strategy on the PHQ-9, as described above. All data were analyzed using SPSS software, including all descriptive statistics (frequency, mean, and standard deviation), chi-square for group comparisons of categorical variables and independent and one-sample t-tests for group comparisons of continuous variables.18 A logistic regression model was used to identify predictors of clinically significant depression, and a linear model was used to identify factors predicting higher PHQ-9 scores overall.
Results
The overall sample was predominately female (over two-thirds), predominately white (approximately two-thirds), with over three-quarters being currently employed and about two-thirds being in a relationship. The average age of the overall sample was 43.5 years, with an average educational attainment equivalent to a bachelor’s degree. The average amount of time since acute COVID-19 infection was 220 days, though with significant variance. A small minority (12%) had a history of hospitalization due to COVID-19 infection (Table 1). Over 40% of the total sample had some history of psychiatric illness, with about one-third of the sample having a prior history of depression.
 |
Table 1 Sociodemographic and Clinical Factors Between Groups |
Using criterion-based PHQ-9 scoring, 25 (33.3%) screened as positive for clinically significant depression. Utilizing cutoff scoring, 41 (54.7%) would have screened positive for clinically significant depression. Twenty-four percent of the participants scored as none-minimal depression severity, 21.3% as mild, 30.7% as mild-moderate, 18.7% as moderate-severe, and 5.3% as severe.
To characterize the symptoms of depression experienced by this population, the questions on the PHQ-9 were examined individually (Figure 1). The most commonly reported symptom was decreased energy/fatigue, followed by sleep disturbance, and poor concentration. No participants reported suicidal ideation.
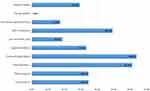 |
Figure 1 Individual PHQ-9 Symptom Frequencies. |
There were no significant sociodemographic differences (Table 1) between the Depressed and Non-Depressed groups. In terms of medical measures, a greater proportion of the Depressed Group was comprised of patients from the WMC Health Post-COVID Care Clinic, or the “Clinical Group”. The Depressed Group had on average a higher COVID symptom severity score both during the acute infection and at the time of the appointment, in addition to higher scores on the Chalder Fatigue Scale, both in total score and in physical fatigue and mental fatigue subscores) (Table 1).
More participants in the Depressed Group had a prior psychiatric history, especially in terms of prior diagnosis of depression (52% vs 20%) or anxiety (56% vs 14%), and were also more likely to be prescribed psychotropic medications (48% vs 24%) (Table 1). Forty-eight percent of patients who screened positive for depression would be considered “new-onset”. The Depressed Group had on average a PHQ-9 score that was over twice that of the Non-Depressed Group and also had higher GAD-7, higher PCL-5, and lower Q-LES-Q scores.
Individual responses to the Q-LES-Q were also examined and compared between the Depressed and Non-Depressed Group (Figure 2). Depressed participants reported lowest satisfaction in the domains of work, sexual life, and mood. There were significant differences between the two groups in all domains on this scale, with the exception of living situation, vision, and economic status.
There was no significant difference noted between the groups in terms of neurocognitive testing measures (RBANS Total Score and MoCA Total Score). However, significant differences were found among the subdomains of the PAOF, including memory, language and communication, and cognitive/intellectual functioning (Table 1).
A logistic regression model using backwards elimination was developed to identify predictors of screening positive for depression (based on criterion scoring) (Table 2). Variables that were statistically significant, or approaching significance, were entered into the model. Four of the five variables were not found to be significant and were removed by backwards elimination. The model for the remaining predictor was significant (−2Log Likelihood=77.25, χ2=18.23, df=3, p<0.001). The only positive predictor identified in the model was the COVID Symptom Total Score during the time of peak COVID-19 illness (OR=1.11, p=0.04) (Table 2).
 |
Table 2 Logistic Regression Model Predicting Depression |
To quantify the effect of variables of interest on depressive symptomatology, a linear regression model was developed to identify predictors of total PHQ-9 score (Table 3). Two of the five variables were found not to be significant and were removed from the model by backwards elimination. The model for the remaining predictors was significant (R2=0.72, F (4, 70)=19.21, p<0.001) (Table 3). The positive predictors identified included Appointment 1 COVID Symptom Total Score (β=0.47, p<0.01), Peak COVID Symptom Total Score (β=0.23, p=0.02), and Prior Psychiatric History (β=2.91, p=0.01).
 |
Table 3 Linear Regression Model Predicting PHQ-9 Score |
No significant differences were found between the groups in terms of elevated inflammatory markers or COVID-19 immunoglobulins (Table 1). Pearson correlations were performed including PHQ-9 score and titers of CRP, IL-6, and TNF-α, however none were statistically significant (p-values of 0.07, 0.49, and 0.20 respectively).
Discussion
This study aimed to describe the frequency, symptom profile, and severity of depression in patients suffering from PASC. Using a conservative criterion-based scoring of the PHQ, we found that one-third of our sample screened as positive for clinically significant depression, with about one-half of these being new-onset depression. Based on a less conservative measure, employed in many studies, greater than half of the sample would be considered to have clinically significant depressive symptoms. Utilizing either strategy, our prevalence rates are in the range of two recent meta-analyses, one of which found a rate ranging from 11% to 28% 12 weeks after COVID-19 infection, consistent with our findings using criterion scoring and another reporting a range of 47–52% based specifically on self-report measures (such as the PHQ-9), consistent with our findings using a cutoff of ≥10.4,19
The Depressed Group had significantly higher scores on the PHQ-9, on average over double that of the Non-Depressed Group. This finding carried over into the GAD-7 and PCL-5, suggesting a likely global increase in psychiatric impairment across various symptom domains, which is consistent with previous reports.3,20 This relationship between depression and anxiety symptoms post-COVID was also found in prior reports from this study sample, which suggested that patients experiencing clinically significant anxiety symptoms had significantly higher PHQ-9 scores and lower Q-LES-Q scores than those who were not.21 This is unsurprising given the high rate of co-occurrence of depression and anxiety.
In terms of depression severity, most participants had PHQ-9 scores in the mild-moderate range (a score of 10–14) and only 3 had scores indicating severe depression, which is consistent with prior research.4 Results indicated that depression in this population was primarily a somatic experience, with participants reporting higher rates of decreased energy (64.0%) and sleep disturbance (61.3%), and much lower rates of cognitive or affective symptoms (such as anhedonia or guilt). This is congruent with the findings of a recent meta-analysis, which found a correlation between self-rated depression and fatigue.4 This also corresponded with fatigue measures, as both physical and mental fatigue were more prevalent among the Depressed Group as measured by the CFS-11.
Our findings support the use of criterion-based scoring of the PHQ-9 versus utilizing the cutoff score of ≥10, as the latter may be overly inclusive of patients with predominantly somatic symptoms. Fatigue and poor sleep have been reported in many post-COVID studies, with one meta-analysis finding that approximately one out of every three people experienced fatigue 12 or more weeks after COVID-19 infection.22 The symptomatology of depression experienced by this participant population may be like that of other medically ill populations, particularly those where neuropathological processes exist that may produce depressive and other neuropsychiatric symptoms. For instance, the distribution of depressive symptoms in this cohort closely resembles that found in patients with Multiple Sclerosis who were also screened for depression with the PHQ-9.23 PASC, like Multiple Sclerosis, has been associated with a number of neurological manifestations, including neurocognitive impairment, fatigue, sleep disturbances, subjective cognitive complaints, and depressed mood.
No statistically significant sociodemographic differences were found between the Depressed Group and Non-Depressed Group. This finding differs from prior studies, which have suggested that post-COVID-19 depression is more common in women than in men, in people with less social support, and either low or high levels of education.4 As our sample overall was predominately women with a relatively small range in years of education, it may be that these differences were not able to be detected.
We found that the Depressed Group had a greater proportion of participants that were referred from the WMCHealth Post-COVID Care Clinic, almost double, which indicates that this group was largely comprised of individuals actively seeking care for post-COVID complaints. This is consistent with previous findings from this research group, which found that patients seeking post-COVID care were more likely to have poorer performance on neurocognitive testing, as well as higher rates of psychiatric distress and more functional difficulties.24 However, when included in the regression models (Table 2 and Table 3), this was not found to be a significant predictor of screening positive on the PHQ-9, nor having a higher PHQ-9 score, so it may be that this relationship is better explained by other variables.
When looking at neurocognitive test performance, we did not find any significant difference between the Depressed and Non-Depressed groups. This is in contrast to prior literature, which suggests that cognitive impairment can be a contributor to increased depression and a diminished quality of life.25
Despite this lack of differences between groups in measured cognitive impairment, there were significant differences in terms of subjective cognitive complaints. The Depressed Group reported significantly more cognitive complaints among the domains of memory, language and communication, and cognitive/intellectual functioning. This may suggest that other post-COVID symptoms, such as depressive symptoms and/or fatigue, may cause patients to feel more impaired than shown on objective neuropsychological testing. This is congruent with a recent machine-learning analysis, which found that cognitive complaints post-COVID were entirely due to depressive symptom severity and older age.4
When comparing the results of the Q-LES-Q between groups, we found that individuals who screened positive on the PHQ-9 also scored lower in terms of satisfaction and enjoyment on each individual quality of life domain when compared to those who were not depressed, with the exception of living situation, vision, and economic status. The most predominantly affected areas were sexual drive/interest, mood, and work. Impairments in sexual drive, mood, and household activities were expected based on prior studies using the Q-LES-Q in depressed patients in general, as well as other studies post-COVID-19, however we did not find impairment in economic status, which has previously been reported.4,9 Our findings on the Q-LES-Q support our findings with the individual PHQ-9 domains, such as fatigue and sleep disturbance, which further indicates disturbances in physical functioning in this cohort.
The severity of COVID-19 infection in this sample appeared to play a major role in later depressive symptoms. Descriptive statistics showed higher average COVID severity scores during the acute infection and at the time of assessment, indicating that more severe illness may be associated with greater long-term depressive symptoms. This was further supported in the regression analyses, with logistic regression finding that only the acute illness severity score predicted later depression, and the linear regression finding that both peak and current symptoms predicted higher PHQ-9 scores. The only other predictor identified was prior psychiatric history. This may indicate that patients with history of psychiatric illness, combined with more severe COVID-19 illness, may be more susceptible to depressive symptoms after COVID-19. Findings similar to these were reported in a multi-cohort observational study of 250,000 individuals across six countries, where researchers found that COVID illness severity was positively correlated with psychiatric comorbidities up to 16 months after the acute infection, with support from recent meta-analyses.4,20 Research related to this is not homogenous, however, with other studies finding that the severity of acute COVID-19 is not associated with the frequency of depressive symptoms.19
No significant differences were found in this sample in terms of inflammatory markers. This was not entirely surprising, as a recent meta-analysis of 16 studies found that while in some samples post-COVID depressive symptoms were associated with such markers, this was not the case in all studies.4 The current results are likely related to small sample size and the conservative approach to utilizing reference ranges. Not all participants in this study consented to serological testing, as venipuncture was an optional component of the study. Additionally, the sample size of participants that screened as positive for clinically severe depression was even smaller, which may have prevented the discovery of significant correlation with inflammatory markers.
Some study limitations must be considered. The sample size was relatively small and may be somewhat biased in that a significant proportion of participants were a clinical population with specific post-COVID complaints, and therefore not strictly representative of the general post-COVID population. However, the inclusion of such a group of patients seeking care for PASC allowed us to compare rates of depression in such a clinical group as compared to those not seeking care and to assess for clinical correlates. This sample was also comprised of predominately white females, which may limit generalizability. This sample cannot be used to estimate the total prevalence of depression in patients with PASC. Additionally, a formal psychiatric evaluation was not performed, which remains the gold standard for diagnosis of depressive disorders. The PHQ-9, while routinely used, is designed as a screening tool, and may detect symptoms from other psychiatric and medical illnesses. The results reported above are cross-sectional and therefore cannot indicate definitively whether or not COVID-19 infection caused psychiatric symptoms. However, strengths include the use of a variety of psychiatric self-report measures in addition to neurocognitive testing and medical/COVID-19 history.
Conclusions
Overall, the results from this study indicate that a significant proportion of individuals experiencing PASC may suffer from symptoms of depression, with many likely meeting DSM-V criteria for a depressive disorder. Symptoms appear to be prominently somatic in nature and correspond with perceived COVID-19 illness severity, prior psychiatric history, post-COVID care-seeking and significant impairment in quality of life. The PHQ-9 and Q-LES-Q scale are easy to use, freely available assessments that may assist in identifying individuals suffering from PASC-related depression and referring them to psychiatric care. Understanding the type of depression experienced by people suffering from PASC is crucial in order to determine treatment, which should target the most appropriate symptom profile. Longer-term studies are indicated to evaluate psychiatric symptoms longitudinally.
Data Sharing Statement
Data from this study are not available at this time as assessment of this cohort is still in progress. Upon completion of the study, data will be available by individual request from the corresponding author, Dr. Ferrando.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding for the current study is from the Edith Har Esh, M.D. Professorship Endowment Fund – New York Medical College. Funds were utilized to cover the costs of participant reimbursement, laboratory assays and neuropsychological test materials.
Disclosure
The authors declare that they have no known competing financial interests or personal/professional relationships that could have appeared to influence the work reported in this paper.
References
1. World Health Organization. Coronavirus Disease; 2023. Available from: https://covid19.who.int/region/amro/country/us.
2. Krishnan K, Lin Y, Prewitt K-RM, Potter DA. Multidisciplinary approach to brain fog and related persisting symptoms post covid-19. J Health Serv Psychol. 2022;48(1):31–38. doi:10.1007/s42843-022-00056-7
3. Lamontagne SJ, Winters MF, Pizzagalli DA, Olmstead MC. Post-acute sequelae of COVID-19: evidence of mood & cognitive impairment. Brain Behav Immun. 2021;17:100347. doi:10.1016/j.bbih.2021.100347
4. Mazza MG, Palladini M, Poletti S, Benedetti F. Post-COVID-19 depressive symptoms: epidemiology, pathophysiology, and pharmacological treatment. CNS Drugs. 2022;36(7):681–702. doi:10.1007/s40263-022-00931-3
5. Perlis RH, Santillana M, Ognyanova K, et al. Comparison of post-COVID depression and major depressive disorder. MedRxiv. 2021. doi:10.1101/2021.03.26.21254425
6. Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
7. Manea L, Gilbody S, McMillan D. Optimal Cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Can Med Assoc J. 2011;184(3):E191–6. doi:10.1503/cmaj.110829
8. Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire. PsycTESTS Dataset. 1993. doi:10.1037/t49981-000
9. Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–1178. doi:10.1176/appi.ajp.162.6.1171
10. Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52–62. doi:10.1097/01.naj.0000314810.46029.74
11. Jackson C. The Chalder Fatigue Scale (CFQ 11). Occup Med. 2015;65(1):86. doi:10.1093/occmed/kqu168
12. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. doi:10.1002/jts.22059
13. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166(10):1092. doi:10.1001/archinte.166.10.1092
14. Randolph C, Tierney MC, Mohr E, Chase TN. The repeatable battery for the assessment of neuropsychological status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310–319. doi:10.1076/jcen.20.3.310.823
15. Nasreddine ZS, Phillips NA, Bã©dirian V, et al. The Montreal Cognitive Assessment, MOCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi:10.1111/j.1532-5415.2005.53221.x
16. Chelune GJ, Heaton RK, Lehman RA. Neuropsychological and personality correlates of patients’ complaints of disability. Adv Clin Neuropsychol. 1986;95–126. doi:10.1007/978-1-4613-2211-5_4
17. Bauer ME, Teixeira AL. Inflammation in psychiatric disorders: what comes First? Ann N Y Acad Sci. 2018;1437(1):57–67. doi:10.1111/nyas.13712
18. IBM Corp. IBM SPSS statistics for windows. Armonk, NY: IBM Corp.; 2020. Available from: https://hadoop.apache.org.
19. Renaud-Charest O, Lui LMW, Eskander S, et al. Onset and frequency of depression in POST-COVID-19 syndrome: a systematic review. J Psychiatr Res. 2021;144:129–137. doi:10.1016/j.jpsychires.2021.09.054
20. Magnúsdóttir I, Lovik A, Unnarsdóttir AB, et al. Acute covid-19 severity and mental health morbidity trajectories in patient populations of Six nations: an observational study. Lancet Public Health. 2022;7(5):e406–e416. doi:10.1016/s2468-2667(22)00042-1
21. Ferrando SJ, Lynch S, Ferrando N, Dornbush R, Shahar S, Klepacz L. Anxiety and posttraumatic stress in post-acute sequelae of COVID-19: prevalence, characteristics, comorbidity, and clinical correlates. Front Psychiatry. 2023;14. doi:10.3389/fpsyt.2023.1160852
22. Ceban F, Ling S, Lui LMW, et al. Fatigue and cognitive impairment in POST-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. doi:10.1016/j.bbi.2021.12.020
23. Ferrando SJ, Samton J, Mor N, Nicora S, Findler M, Apatoff B. Patient health questionnaire-9 to screen for depression in outpatients with multiple sclerosis. Int J MS Care. 2007;9(3):99–103. doi:10.7224/1537-2073-9.3.99
24. Ferrando SJ, Dornbush R, Lynch S, et al. Neuropsychological, medical, and psychiatric findings after recovery from acute COVID-19: a cross-sectional study. J Acad Consult Liaison Psychiatry. 2022;63(5):474–484. doi:10.1016/j.jaclp.2022.01.003
25. Miklitz C, Westerteicher C, Lippold S, Ochs L, Schneider A, Fliessbach K. The impact of COVID-19-related distress on levels of depression, anxiety and quality of life in Psychogeriatric patients. Eur Arch Psychiatry Clin Neurosci. 2021;272(1):53–66. doi:10.1007/s00406-021-01340-1
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

