Back to Journals » Advances in Medical Education and Practice » Volume 9
Fourth-year medical students do not perform a focused physical examination during a case-based simulation scenario
Authors Bilello LA , Dubosh NM, Lewis JJ, Hall MM, Fisher J, Ullman EA
Received 23 December 2017
Accepted for publication 2 March 2018
Published 17 August 2018 Volume 2018:9 Pages 583—588
DOI https://doi.org/10.2147/AMEP.S160701
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Leslie A Bilello,1 Nicole M Dubosh,1 Jason J Lewis,1 Matthew M Hall,1 Jonathan Fisher,2 Edward A Ullman1
1Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA; 2Department of Emergency Medicine, Maricopa Medical Center, Phoenix, AZ, USA
Background: The art of physical examination is one of the most valuable diagnostic tools bestowed upon new generations of medical students. Despite traditional educational techniques and significant attention on a national level, both trainees and educators have noticed a decrease in physical examination proficiency. Simulation has been identified as a potential way to improve physical examination techniques within undergraduate medical education. We sought to determine the utility of a cardiac case-based simulation scenario to assess physical examination performance of fourth-year medical students during an emergency medicine (EM) clerkship.
Materials and methods: Fourth-year medical students enrolled in a 4-week EM clerkship were prospectively evaluated during a case-based scenario using a simulation mannequin (Laerdal SimMan®). The case involved a patient presenting with chest pain that evolved into cardiac arrest. All simulations were video recorded and two emergency physicians reviewed each video. The reviewers recorded whether or not each student completed the essential components of a focused physical examination.
Results: Twenty-seven students participated in the simulation. The percentage of students completing each of the four components of the physical examination was as follows: cardiac auscultation 33.3% (95% CI 18.5–52.3), lung auscultation 29.6% (95% CI 15.7–48.7), pulse and extremity examination 55.6% (95% CI 37.3–72.4), and abdominal examination 3.70% (95% CI 0–19.8). None of the students completed all four of these components.
Conclusion: Our study showed that fourth-year medical students did not uniformly perform components of a focused physical examination during a high-acuity chest pain simulation scenario. Although our study showed limited physical examination performance, simulation allows evaluators to observe and provide constructive feedback and may lead to an improvement in these skills. These findings call for improved technology to increase authenticity of simulators and continued faculty development for more creative, meaningful integration of physical examination skills into high-acuity simulation cases.
Keywords: emergency medicine, medical student education, undergraduate medical education, physical examination skills
A Letter to the Editor has been received and published for this article.
Introduction
Physical examination skills represent one of the most important diagnostic tools imparted to new generations of medical students and trainees. It is essential to patient care, diagnostic, and treatment plans and may also impact perceived patient satisfaction.1 As a measure of its importance, two of the 24 emergency medicine (EM) competency-based milestones for fourth-year medical students specifically evaluate the ability to perform and communicate history and physical examination findings.2
Medical students have traditionally learned the physical examination through didactic sessions, bedside teaching rounds, and standardized patients.3,4 Despite conventional educational techniques and significant attention on a national level, both trainees and educators have noticed a decrease in physical examination proficiency.5–9 Simulation provides an opportunity to expose students to physical examination skills and provides an arena for deliberate practice. In addition to mimicking the human body, high-fidelity mannequins have functions that allow auscultation of heart and lung sounds and palpation of pulses.10 Simulation has been identified as one way to potentially improve physical examination techniques in the medical student population.9,11 In this study, we sought to determine the utility of a cardiac case-based simulation to evaluate physical examination performance of fourth-year medical students during an EM clerkship, specifically cardiac and lung auscultation, abdominal examination, and pulse and extremity assessment.
Materials and methods
Study design
This was a prospective observational study of fourth-year medical students enrolled in an EM clerkship at an academic, urban medical center. The study was evaluated by the Institutional Review Board at Beth Israel Deaconess Medical Center and, in accordance with the Code of Federal Regulations 45 CFR 46.101(b), determined to be exempt from further review as the subjects are not identifiable outside of the study.
Study setting and population
The study population consisted of fourth-year medical students participating in an elective, 4-week EM clerkship at an academic hospital that is affiliated with a major medical school and is home to a 3-year EM residency training program (Table 1). All US medical students enrolled in the clerkship within a 4-month period were included.
  | Table 1 Demographics for medical student participants Abbreviation: EM, emergency medicine. |
As part of the clerkship requirement, all students participated in a high-fidelity case-based simulation scenario during the third week. The simulation session occurred at our medical center’s simulation laboratory using a high-fidelity mannequin (Laerdal SimMan®). Prior to the case, students were instructed to evaluate the patient as they would evaluate a real ED patient including obtaining a history and physical exam. They were informed that any equipment, testing, specialty consultation, and ancillary support that they would normally have in the ED were available to them. Students were divided into the following groups: one group of four, three groups of three, seven groups of two, and one single student who performed the simulation by himself. Each student had to perform his or her own physical examination in order to be given credit during our video assessment.
The simulation case, as described in Supplement 1, involved an adult male patient complaining of chest pain. The case was scripted prior to this exercise and the same emergency physician provided the voice for the mannequin in all cases. The simulation began as a low-acuity scenario with a stable patient. After ample time to obtain history of present illness, review of systems, and physical examination, the students were given an electrocardiogram (ECG) demonstrating acute elevation between the S and T myocardial infarction (STEMI). Within 1–2 minutes of this ECG discovery, the patient became unresponsive and had a cardiac arrest. Critical actions expected of the students included history taking and development of a differential diagnosis, focused physical examination, interpretation of STEMI on ECG, immediate medical management including antiplatelet therapy and heparin, emergent cardiology consultation, resuscitation utilizing the advanced cardiac life support algorithm, and effective communication with the team, patient, and consultant. These critical actions were not provided to the students prior to simulation so as not to bias their performance.
Study protocol
All simulation encounters were video recorded for teaching and evaluation purposes as part of the existing clerkship curriculum. There were five reviewers involved with the study and each underwent a 30-minute group training session on simulation evaluation. Specifically, the reviewers included two senior emergency physicians, two junior emergency physicians, and a second-year resident. All physicians had prior experience with simulation. In an effort to prevent confounding factors such as previous clinical experience with the student or prior knowledge of the simulation case, the videos were randomly divided among the reviewers and two physicians evaluated each video. Prior to the onset of the study, the clerkship directors determined the following four physical examination components to be necessary for a chest pain case: auscultation of the heart, auscultation of the lungs, palpation of the abdomen, and pulse and extremity examination. Any pulse examination, including carotid, radial, femoral, and distal extremities, was considered a positive action. The video allowed visualization of palpation and auscultation to confirm completion of the four examination components. The reviewers used a checklist to assess whether or not the student performed each of these four components during the case.
Statistical analysis
Proportions and CI for the completion of each physical examination component were calculated using GraphPad.
Results
Twenty-seven fourth-year students participated in the case-based simulation. The percentage of students completing each of the four components of the focused physical examination varied. The greatest proportion of students performed a pulse and extremity examination (55.6%; 95% CI 37.3–72.4). Approximately one-third of students completed cardiac auscultation (33.3%; 95% CI 18.5–52.3) and lung auscultation (29.6%; 95% CI 15.7–48.7). A small subset of students performed an abdominal examination (3.70%; 95% CI 0–19.8). No student completed all four of the physical examination components (Table 2). The video provided clear identification of whether or not the physical examination component was performed and there was 100% agreement among evaluators.
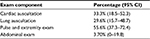  | Table 2 Performance of focused physical exam components during cardiac simulation |
Discussion
Our study demonstrated that components of a focused physical examination were not uniformly performed in a chest pain simulation scenario, which raises the issue of whether a simulation-based patient encounter can adequately assess physical examination skills.
The reasons for our findings are likely multifactorial. Students may have perceived the simulator as insufficiently realistic to suspend belief enough to treat the mannequin as a proxy for a human patient. The case scenario may have led the students to believe that the primary focus was on therapeutic actions rather than on in-depth diagnostic ones. Finally, students may have had little understanding of the capabilities of simulators because of limited experience.
Our work expands on previous studies investigating the role of physical examination skills within simulation settings. One study by Warrington et al showed that simulation is not perceived as a realistic portrayal of the physical examination. Their study found that utilization of a specialized simulation stethoscope led to improved cardiopulmonary physical examination performance, specifically an increase in correct diagnoses and trainee satisfaction.12 Another study by McCoy et al confirms that students with previous simulation experience perform better in a simulated clinical scenario. Their investigation demonstrated that simulation-trained students performed 22% more critical actions and scored 26% higher on their simulation physical examinations compared to the didactic-trained control group.13 Finally, Kern et al trained medical students using the addition of a cardiac simulator to the traditional standardized patient curriculum and saw a statistically significant increase in the number of students performing components of the cardiac examination.14 This study supports the finding that previous experience will likely improve one’s simulation performance.
Our investigation involving a high-acuity case adds to the current body of simulation education literature and serves as a contrast to studies involving isolated task trainers, procedural-based simulation, and low-acuity scenarios.14,15 In two previous studies, cardiac simulators were added to existing curricula in order to demonstrate the utility of physical examination practice and assessment, yet there was no clinical framework accompanying the cardiac training.14,15 As educators, we aim to find ways to evaluate learners in an environment that is similar to the clinical setting, such as our high-acuity cardiac arrest scenario for an EM clerkship.
Our limitations include the fact that our sample size of 27 students is relatively small. Second, our students performed the simulation case in groups, which may have contributed to the finding that not all students examined the patient. However, the group dynamic might have offered an opportunity for students to compensate for others’ lack of physical examination performance. Finally, our study involved students from different institutions and previous simulation training may vary among the participants.
Conclusion
Our study showed that fourth-year medical students did not uniformly perform components of a focused physical examination during a high-acuity chest pain simulation scenario. Although our study showed limited physical examination performance, simulation allows evaluators to observe the student–simulation patient interaction in order to give constructive feedback. Critiques on the physical examination will hopefully lead to an improvement in these skills and achievement of future milestones.16 These findings call for improved technology to increase authenticity of simulators and continued faculty development for more creative, meaningful integration of physical examination skills into high-acuity simulation cases. These findings may indicate a professional trend toward reliance on technology and lab diagnostic tools as a possible distraction to the power of a thorough physical examination.
Author contributions
All the authors have made substantial contributions to the design, data acquisition, analysis, and creation of this paper. All the authors have approved this paper and agreed with its submission to the Advances in Medical Education and Practice. All the authors are accountable for the integrity of this original research and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Feletti GI, Carney SL. Evaluating patients’ satisfaction with medical students’ interviewing skills. Med Educ. 1984;18(1):15–20. | ||
Santen SA, Peterson WJ, Khandelwal S, House JB, Manthey DE, Sozener CB. Medical student milestones in emergency medicine. Acad Emerg Med. 2014;21(8):905–911. | ||
Roberts L, Lu WH, Go RA, Daroowalla F. Effect of bedside physical diagnosis training on third-year medical students’ physical examination skills. Teach Learn Med. 2014;26(1):81–85. | ||
Herbstreit F, Merse S, Schnell R, et al. Impact of standardized patients on the training of medical students to manage emergencies. Medicine (Baltimore). 2017;96(5):e5933. | ||
Burdick WP, Schoffstall J. Observation of emergency medicine residents at the bedside: how often does it happen? Acad Emerg Med. 1995;2(10):909–913. | ||
Haring CM, Cools BM, van der meer JW, Postma CT. Student performance of the general physical examination in internal medicine: an observational study. BMC Med Educ. 2014;14:73. | ||
Howley LD, Wilson WG. Direct observation of students during clerkship rotations: a multiyear descriptive study. Acad Med. 2004;79(3):276–280. | ||
Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548–551. | ||
Okuda Y, Bryson EO, DeMaria S Jr, et al. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76(4):330–343. | ||
McKinney J, Cook DA, Wood D, Hatala R. Simulation-based training for cardiac auscultation skills: systematic review and meta-analysis. J Gen Intern Med. 2013;28(2):283–291. | ||
Issenberg SB, McGaghie WC, Hart IR, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–866. | ||
Warrington SJ, Beeson MS, Fire FL. Are simulation stethoscopes a useful adjunct for emergency residents’ training on high-fidelity mannequins? West J Emerg Med. 2013;14(3):275–277. | ||
McCoy CE, Menchine M, Anderson C, Kollen R, Langdorf MI, Lotfipour S. Prospective randomized crossover study of simulation vs. didactics for teaching medical students the assessment and management of critically ill patients. J Emerg Med. 2011;40(4):448–455. | ||
Kern DH, Mainous AG 3rd, Carey M, Beddingfield A. Simulation-based teaching to improve cardiovascular examination skills performance among third-year medical students. Teach Learn Med. 2011;23(1):15–20. | ||
Butter J, McGaghie WC, Cohen ER, Kaye M, Wayne DB. Simulation-based mastery learning improves cardiac auscultation skills in medical students. J Gen Intern Med. 2010;25(8):780–785. | ||
Leung CG, Thompson L, McCallister JW, Way DP, Kman NE. Promoting achievement of level 1 milestones for medical students going into emergency medicine. West J Emerg Med. 2017;18(1):20–25. |
Supplementary materials
Supplement 1: Chest pain simulation case
Vignette
The patient is a 52 year-old man with past medical history (PMH) of hypertension (HTN) presenting with chest pain. He has had exertional angina over 2–3 weeks and then constant pain today. He arrived in stable condition with continued pain. Electrocardiogram (ECG) demonstrates ST elevation myocardial infarction (STEMI). The patient experiences cardiac arrest with an initial rhythm of ventricular fibrillation (VF) and he achieves return of spontaneous circulation after 1–2 shocks from the defibrillator. He has a reassuring neurologic examination after the arrest and is transported to the cardiac catheterization laboratory.
Patient presentation
HPI: A 52-year-old man with chest pain. Over the last few weeks, he has been getting a burning sensation and pressure in his chest. The pain is exacerbated when he walks quickly or goes up the stairs, but improves with rest. Pain is located in the left chest and travels to bilateral shoulders. The pain is not worse with deep inspiration or change in position, but it is associated with nausea and diaphoresis. He is unsure if it feels similar to his gastroesophageal reflux disease (GERD). He went to work this morning, but his pain did not improve while sitting at his desk and so he presents for evaluation.
PMH: GERD, HTN
Medications: Tums, hydrochlorothiazide
Social: The patient lives with wife and two teenage kids. He quit smoking 2 years ago and drinks alcohol socially. He works as insurance salesman.
Vitals:
Temperature 37.0 Celsius
Heart rate 90
Blood pressure 136/82
Respiratory rate 16
Oxygen saturation 97% without supplement oxygen
Pain scale 8 out of 10
Examination: The patient is in no acute distress and speaking in full sentences on arrival. Students are told that he appears mildly diaphoretic. He has clear, equal lung sounds without evidence of wheezing or rales. His cardiac examination demonstrates normal heart sounds with a regular rate and rhythm without evidence of murmur or rub. There is no abdominal pain elicited with palpation. There is no swelling in the patient’s extremities. He has intact pulses in all four extremities upon arrival.
Clinical course
The patient is in bed with a telemetry monitor attached. He is awake and alert and able to give a good history. The team should gather history, perform a physical examination, and order preliminary tests including ECG, complete blood count, chemistries, troponin, and chest X-ray. The team should give aspirin, start intravenous lines, and ensure patient is on the telemetry monitor. The students may place supplemental oxygen, as well as give nitroglycerin and morphine for pain relief. After asking for the ECG, they will receive an ECG demonstrating an acute STEMI. The students should interpret the ECG together and recognize this finding. They are expected to apply defibrillator pads correctly and call the cardiologist in order to activate the cardiac catheterization laboratory.
The patient will ask what is going on and request an update. If team does not say “heart attack” when describing his condition, the patient will inquire further about the results of his ECG. As the team is calling cardiology, patient’s telemetry monitor will demonstrate VF and he will become unresponsive. Team should start effective cardiopulmonary resuscitation efforts, including defibrillation. They may also give epinephrine. After 1–2 defibrillation shocks, the patient will regain pulses and follow commands. The students should start heparin and the patient will be transferred to the catheterization laboratory.
Critical actions
- Gather focused and accurate history and physical examination to develop a differential diagnosis
- Interpret ECG as an acute STEMI
- Provide immediate medical management including antiplatelet agents and heparin
- Consult cardiology emergently
- Recognize ventricular fibrillation cardiac arrest and provide resuscitation including compressions and defibrillation
- Communicate effectively with other students, the patient, nursing team, and consultants
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
