Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Fluoxetine May Enhance VEGF, BDNF and Cognition in Patients with Vascular Cognitive Impairment No Dementia: An Open-Label Randomized Clinical Study
Authors Zhang L, Liu X, Li T, Xu B, Fu B
Received 17 August 2021
Accepted for publication 8 December 2021
Published 29 December 2021 Volume 2021:17 Pages 3819—3825
DOI https://doi.org/10.2147/NDT.S334647
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Lei Zhang, Xuan Liu, Tong Li, Bing Xu, Binfang Fu
Department of Neurology, Xiangyang Central Hospital, Affiliated Hospital of Hubei University of Arts and Science, Xiangyang, Hubei, 441021, People’s Republic of China
Correspondence: Xuan Liu
Department of Neurology, Xiangyang Central Hospital, Affiliated Hospital of Hubei University of Arts and Science, Xiangyang, Hubei, 441021, People’s Republic of China
Tel +86 710 3524339
Fax +86 710 3524330
Email [email protected]
Purpose: Selective serotonin reuptake inhibitors (SSRIs) enhance angiogenesis and neurogenesis. Brain-derived neurotrophic factor (BDNF) and vascular endothelial growth factor (VEGF) play an important role in neurogenesis and angiogenesis. However, the effect of SSRIs on cognition and serum BDNF and VEGF in patients with vascular cognitive impairment no dementia (VCIND) is largely unknown.
Patients and Methods: It was an open label study. Fifty VCIND patients were randomly allocated to receive fluoxetine (20 mg/d; n = 25) or no fluoxetine (control group; n = 25) for 12 weeks. VCIND patients received fluoxetine 20 mg/d and secondary prevention of stroke for 12 weeks in the fluoxetine group, whereas the control group received only secondary prevention of stroke for 12 weeks. The primary outcome and secondary outcome were of assessment of Alzheimer’s Disease Assessment Scale cognitive subscale (ADAS-cog) score, Ten Point Clock drawing test score (TPC), Verbal Fluency Test (VFT), Trail Making Test form a (TMTa), Trail Making Test form b (TMTb) and Digit Span Test score at baseline and week 12 in the both groups. And serum concentration of BDNF and VEGF was also tested at baseline and week 12 in both groups.
Results: After 12 weeks, TPC scores increased more significantly in the fluoxetine group than in the control group, while TMTa score and TMTb score were decreased more significantly in the fluoxetine group than in the control group. We also found that the serum concentration of BDNF and VEGF in the fluoxetine group increased more significantly than in the control group. However, we found no significant differences in mean change from baseline between fluoxetine and control group in ADAS-Cog score, Digit Span Test score and VFT score.
Conclusion: Fluoxetine may enhance cognition in certain cognitive domains and serum concentration of BDNF and VEGF in patients with VCIND.
Keywords: cognition, enhancement, neuroprotection, selective serotonin reuptake inhibitors
A Letter to the Editor has been published for this article.
Introduction
Vascular cognitive impairment no dementia (VCIND) is a mild stage of vascular cognitive impairment (VCI), which is a spectrum of cognitive impairments caused by or associated with vascular factors.1
So far, the exact pathophysiology and neurobiology of VCI has not been fully understood. Some regulatory mechanisms and cellular signal transduction, including oxidative stress, neuroinflammation, endothelial dysfunction, hypoperfusion, destruction of blood-brain barrier, cortical hyperexcitability and neurotransmitter imbalance, are considered to play a role in VCI.2 Many research and treatment methods have been tried to be applied to VCI, including drug therapy and non-drug therapy. Acetylcholinesterase (AChE) inhibitor such as donepezil hydrochloride, galantamine, kabalatin, etc., and an N-methyl-D-aspartic acid (NMDA) glutamate receptor antagonist (memantine) can be used in the treatment of vascular dementia. However, the role of Acetyl-L-Carnitine in AD and other cognitive disorders is still controversial due to the lack of evidence-based medical evidence.3 By non-pharmaceutical means, a systematic TMS evaluation of VCI patients can promote the diagnostic process, enhance the therapeutic arsenal, and predict the prognosis.4
VCIND is an important stage of VCI and does not follow a unidirectional progression towards dementia.5 That means if patients with VCIND were handled well, and they might not develop vascular dementia definitely. Whereas, there are no drugs licensed for the treatment of VCIND, and treatment is limited to controlling known vascular risk factors.
Selective serotonin reuptake inhibitors (SSRIs) are widely used antidepressant. However, preclinical study found that antidepressants including SSRIs had direct effects on brain functions associated with plasticity, neurogenesis, and neuronal differentiation.6 Furthermore, studies have also shown that chronic antidepressant administration increases neurogenesis and the expression of cyclic adenosine monophosphate (cAMP) response element binding protein, an important upstream signaling molecule of brain-derived neurotrophic factor (BDNF) in the adult rat hippocampus,7,8 In addition, the results show that SSRIs increase vascular endothelial growth factor (VEGF) expression in the hippocampus and that fluoxetine induction of VEGF occurs in both neurons and endothelial cells.8 Furthermore, a previous study showed BDNF-induced VEGF release in a neuroblastoma cell line, and BDNF-TRKB signaling stimulated VEGF release in primary cortical neurons.9 Clinical study found that remission of depression was correlated with improved outcomes with rehabilitation after stroke.10 However, recent studies showed that administration of antidepressant also might be useful in fostering recovery in nondepressed patients with stroke.11 Clinical studies showed that SSRIs enhanced motor function and cognition in nondepressed patients with stroke.11,12 A small retrospective clinical study of selective serotonin reuptake inhibitor showed benefits on executive function in patients with VCI.13 Our previous clinical study also showed that fluoxetine could enhance cognition and increase serum concentration of BDNF in patients with vascular dementia (VaD).14 In light of the observed beneficial effects of antidepressants and previous research, we hypothesized that SSRIs would enhance cognitive function and increase serum concentration of BDNF and VEGF in patients with VCIND.
Patients and Methods
Study Design and Patients
This prospective study was conducted at Xiangyang Central Hospital from June 2012 to June 2019. The study was performed according to the Declaration of Helsinki and subsequent revisions and was approved by institutional review boards of Xiangyang Central Hospital. Written informed consent was obtained from each participant (or legal representative).
Sample Size
The study was designed to detect a clinically meaningful difference in cognition between the two groups. A sample size of 50 (minimum of 25 treatment and 25 control) was needed to detect such a difference with a statistical power of 80% at a 5% significance level according to the results of previous trials.15
Inclusion Criteria
The inclusion criteria were: (1) age 45–80 years; (2) history of stroke and/or neuroimaging (computed tomography or magnetic resonance imaging) showing evidence of cerebrovascular disease; (3) cognitive impairment did not meet the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for dementia;16 (4) cognitive impairment was judged to have a vascular cause and the Hachinski Ischemic Score was greater than 7.17 (5) The VCIND covers one or multiple cognitive impairment domains, of which the instrumental activities of daily living could be normal or slightly affected. In the meanwhile, it does not disturb the main daily-life independency.
Exclusion Criteria
Participants were excluded if they had depression according to DSM-IV diagnostic criteria, including mild, moderate, and major depressive disorder patients.16 The patients will also be excluded if they had (1) respiratory failure, heart failure, other organ failure, pregnancy, or a tumor that could put the patient at special risk; (2) history of neurodegenerative diseases including Alzheimer’s disease, Parkinson’s disease, multiple system atrophy and Huntington’s disease that could interfere with the efficacy evaluations; (3) severe aphasia that could make the participants unable to perform neuropsychological tests; (4) history of alcohol and/or other drug abuse, or use of anticholinesterase, or other drugs that could potentially improve cognition within 1 year prior to enrollment. Participants were administered an interview for DSM-IV diagnostic criteria for depression16 at the 12-week follow-up and were also excluded if they met these criteria.
Randomization and Blind
All participants underwent a standardized baseline assessment including a physical and neurological examination. Allocation of participants to the control group or fluoxetine group was made by reference to a statistical series based on a random number table drawn up for each participant at each center by Doctor Tong Li. It was an open-label study and the investigators were aware of the allocation of participants. However, the data collectors were blinded to group allocation. Data analysis was conducted by the first author on a de-identified database.
Treatment
VCIND patients received fluoxetine 20 mg/d and secondary prevention of stroke for 12 weeks in the fluoxetine group, whereas the control group received only secondary prevention of stroke for 12 weeks. Secondary prevention of stroke is about controlling known vascular risk factors.
Follow-Up and Efficacy and Safety Outcomes
VCIND patients were followed up at weeks 4 and 8 by telephone and at week 12 by a visit to the clinic. Information about any adverse reactions was collected at each follow-up. The primary outcome was cognitive assessment using the Alzheimer’s Disease Assessment Scale cognitive subscale (ADAS-Cog) and Ten Point Clock drawing test (TPC) score at baseline and week 12 in both groups by an experienced neuropsychologist.18,19 The secondary outcome was measurement of Mini-Mental State Examination (MMSE),20 Verbal Fluency Test (VFT), Trail Making Test form a (TMTa), Trail Making Test form b (TMTb) and Digit span test score at baseline and week 12 in both groups.21–23 The cognitive subscale of the ADAS-Cog has 12 items. The total score of ADAS-Cog ranges from 0 to 70, and higher scores indicating more severe cognitive impairment. The test has previously been validated into four domains: attention, language, memory, praxis. The executive function was assessed using the TPC. The Trail Making Test form a and b (TMTa and TMTb) assesses visual searching speed, attention, and mental flexibility. For both parts, the time range required to accomplish the test is measured separately. The Digit Span Test requires subjects to repeat an orally presented series of numbers of increasing length, first forward and then backward. The Verbal Fluency Test evaluates the ability to form and fluently utter words compatible with given criteria. The participant is required to list in 60 seconds as many words as possible that belong to a given semantic category (fruit, vegetable and animal). The score was the sum of three 1 min trials with different letters. The serum concentration of BDNF and VEGF was measured at baseline and week 12 in both groups.
Statistical Analysis
The data are presented as the mean ± standard deviation. The two-sample t-test (or the Mann–Whitney U-test for data with a non-normal distribution) was used to compare baseline characteristics between the two groups. Pearson χ2 test was used to compare the gender distribution in the two groups. The primary and secondary outcomes were compared across the two time points (baseline and week 12) with the two-tailed paired t-test for paired samples in each of the two groups. Significance of the results was set at p < 0.05. All statistical analyses were carried out using Statistical Package for the Social Sciences version 12 software (SPSS Inc., Chicago, IL, USA).
Results
Recruitment
One hundred and fifty-seven patients with VCIND were screened and a total of 50 patients were recruited and randomized into two groups: fluoxetine and control group. Forty-seven patients completed the 12-week follow-up. Of the 50 patients with VCIND, informations on study outcomes was available for 47 patients (94%) as one patient withdrew and another patient was unconnected in the fluoxetine group before a follow-up of cognitive evaluation carried out at week 12. One patient in the control group was unconnected at week 8.
Table 1 shows the demographic and clinical characteristics of VCIND patients in the fluoxetine and control groups. The two treatment groups were well balanced in terms of gender (p = 0.571), age (p = 0.800), years of education (p = 0.796), body mass index (p = 0.640), TIA (p = 0.544), stroke (p = 0.765), cardiovascular disease (p = 0.777), smoking (p = 0.083), hypertension (p = 0.564), diabetes mellitus (p = 0.254), hypercholesterolaemia (p = 0.571), MMSE score (p = 0.947), ADAS-Cog score (p = 0.759), TPC score (p = 0.326), VFT score (p = 0.827), TMTa score (p = 0.125), TMTb score (p = 0.171), Digit span test score (p = 0.330), BDNF (p = 0.885) and VEGF (p = 0.074).
 |
Table 1 Demographic and Clinical Characteristics of VCIND Patients Randomized to the Fluoxetine and Control Groups |
Efficacy
Baseline and week 12 ADAS-Cog score, TPC score, VFT score, TMTa score, TMTb score, Digit span test score, serum concentration of BDNF and VEGF are shown in Table 2. There were significant differences in mean change from baseline between fluoxetine and control in MMSE score (p = 0.013) TPC score (p = 0.017), TMTa score (p = 0.03) and TMTb (p < 0.0001) score serum concentration of BDNF (p < 0.0001) and VEGF (p = 0.024). However, we found no significant differences in mean change from baseline between fluoxetine and control in the primary endpoints of ADAS-Cog score (p = 0.08), Digit Span Test score (p = 0.442) and VFT score (p = 0.595) (Table 2).
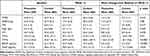 |
Table 2 Mean Change from Baseline and Week 12 ADAS-Cog Score, TPC Score, and Digit Span Test Score and VFT Score of VCIND Patients Stratified by Treatment Group |
Discussion
In the present study, we investigated the effects of fluoxetine on cognitive function and concentration of serum BDNF and VEGF in patients with VCIND. Patients receiving fluoxetine demonstrated improvement mainly in MMSE score, TPC score, TMTa score and TMTb score, neuropsychological tests assessing executive function and increased concentration of serum BDNF and VEGF, compared with patients receiving only secondary prevention of stroke. Patients in the control group also demonstrated some improvement in executive function though it did not reach statistical significance.
A small clinical study was conducted in patients with Alzheimer’s disease and reported that fluoxetine enhanced memory and cognition in patients with mild cognitive impairment,24 and sertraline improved executive function in patients with VCI.13 Moreover, citalopram improved dexterity in chronic stroke patients,25 and escitalopram was associated with improved cognitive recovery following stroke compared with placebo and problem solving therapy.12 What is more, in our previous study we found fluoxetine enhanced cognition and increased serum BDNF concentration in patients with VaD.14 Our study is consistent with these previous studies. We found improvement in cognitive function following treatment with fluoxetine in patients with VCIND. Thus, SSRIs may be an alternative treatment for improving cognitive impairment in patients with VCIND.
In preclinical studies, multiple beneficial effects of SSRIs have been demonstrated in both normal and diseased brains. First, fluoxetine may have a neuroprotective effect.7 Second, growing evidence suggests that SSRIs have neurotrophic effect.3 The effects of chronic and acute treatment with SSRIs on tropomyosin-related kinase (TrkB) autophosphorylation and TrkB protein levels have been tested in animal studies and escitalopram increased BDNF and TrkB mRNA levels in the hippocampus and prefrontal cortex of juvenile rats after 4 days of treatment.26 TrkB is a high-affinity receptor for BDNF, and its autophosphorylation results in activation and serves as an indirect signal of neuronal release.26
In another study, experimentally lowering brain BDNF or lowering expression of TrkB in neural progenitor cells in the hippocampus diminished the antidepressant efficacy in animal models.27 Furthermore, evidence also shows that blockage of hippocampal neurogenesis diminishes the antidepressant-like effects of fluoxetine, suggesting involvement of BDNF in antidepressant actions.28 In our previous study we also found increased serum BDNF concentration in patients with VaD treated with fluoxetine.14 A preclinical study also showed that vascular endothelial growth factor (VEGF) was identified as a key mediator of both the cytogenetic and behavioral actions of antidepressants.29 Chronic fluoxetine administration significantly increased endothelial cell proliferation in the subgranular zone (SGZ) and VEGF receptor signaling was identified induction of endothelial cell proliferation as an action of antidepressants.29 In our study, we also found increased concentration of serum BDNF and VEGF in patients with VCIND treated with fluoxetine. Thus, we speculate that the improvement in global cognitive function observed in our study may be partly related to remodeling of the hippocampal circuitry and increased dentate gyrus neurogenesis and angiogenesis. However, a small clinical study did not find any improvement in the memory of patients with Alzheimer’s disease who were treated with fluoxetine.30 Overall, the utility of SSRIs for cognitive recovery in patients with VCIND should be investigated further in future studies.
Our study has significant implications. Impairments of cognition are a major contributor to disability and decreased quality of life following stroke.31 Vascular cognitive impairment has been associated with increased caregiver burden and health-care costs.32 The results from this follow-up study suggest that fluoxetine is useful in VCIND, which means the patients with VCIND have the chance to enhance their cognition and have the potential to significantly reduce the burden of this disease. SSRIs would be a simple and widely applicable treatment for patients with VCIND.
To our knowledge, this is the first study describing the impact of fluoxetine on cognition and concentration of serum BDNF and VEGF in patients with VCIND. However, we must note that our findings are limited by the open-label drug administration protocol and small sample size. Larger double-blind, placebo-controlled studies with a longer period of follow-up are needed to confirm these findings in the future.
Conclusions
In our study, we found that fluoxetine was associated with improved cognitive recovery in certain cognitive domains and increased concentration of serum BDNF and VEGF in patients with VCIND compared with matched controls who did not receive fluoxetine. The utility of fluoxetine in patients with VCIND requires further investigation.
Data Sharing and Data Accessibility
All the authors shared individual deidentified participant data. All the original specific data and the other study documents we intended to share. The trial was registered in the (https://www.chictr.org.cn/index.aspx) website. Data would be always accessible through the website when they were needed, and the Identifier is ChiCTR-TRC-12002247.
Ethical Approval and Informed Consent
The study was performed according to the Declaration of Helsinki and subsequent revisions and was approved by institutional review boards of Xiangyang Central Hospital. Written informed consent was obtained from each participant (or legal representative).
Acknowledgments
The authors thank Dr Zhang Lei for technical support.
Disclosure
The authors declare no conflicts of interest.
References
1. Rockwood K, Ebly E, Hachinski V, Hogan D. Presence and treatment of vascular risk factors in patients with vascular cognitive impairment. Arch Neurol. 1997;54(1):33–39. doi:10.1001/archneur.1997.00550130019010
2. Vinciguerra L, Lanza G, Puglisi V, et al. Update on the neurobiology of vascular cognitive impairment: from lab to clinic. Int J Mol Sci. 2020;21(8):2977. doi:10.3390/ijms21082977
3. Pennisi M, Lanza G, Cantone M, et al. Acetyl-L-carnitine in dementia and other cognitive disorders: a critical update. Nutrients. 2020;12(5):1389. doi:10.3390/nu12051389
4. Cantone M, Lanza G, Fisicaro F, et al. Evaluation and treatment of vascular cognitive impairment by transcranial magnetic stimulation. Neural Plast. 2020;2020:8820881. doi:10.1155/2020/8820881
5. Ingles JL, Wentzel C, Fisk JD, Rockwood K. Neuropsychological predictors of incident dementia in patients with vascular cognitive impairment, without dementia. Stroke. 2002;33(8):1999–2002. doi:10.1161/01.STR.0000024433.36590.1B
6. Planchez B, Surget A, Belzung C. Adult hippocampal neurogenesis and antidepressants effects. Curr Opin Pharmacol. 2019;27(50):17–24.
7. Khodanovich M, Kisel A, Kudabaeva M, Yarnykh V. Effects of fluoxetine on hippocampal neurogenesis and neuroprotection in the model of global cerebral ischemia in rats. Int J Mol Sci. 2018;19(1):162. doi:10.3390/ijms19010162
8. Greene J, Banasr M, Lee B, et al. Vascular endothelial growth factor signaling is required for the behavioral actions of antidepressant treatment: pharmacological and cellular characterization. Neuropsychopharmacology. 2009;34(11):2459–2468. doi:10.1038/npp.2009.68
9. Deyama S, Bang E, Kato T, Duman RS. Neurotrophic and antidepressant actions of brain-derived neurotrophic factor require vascular endothelial growth factor. Biol Psychiatry. 2019;86(2):143–152. doi:10.1016/j.biopsych.2018.12.014
10. Wang S, Wang C-X, Zhang N. The association between post-stroke depression, aphasia, and physical independence in stroke patients at 3-month follow-up. Front Psychiatry. 2018;9:374. doi:10.3389/fpsyt.2018.00374
11. Chollet F, Tardy J, Albucher JF. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME) a randomised placebo-controlled trial. Lancet Neurol. 2011;10(2):123–130. doi:10.1016/S1474-4422(10)70314-8
12. Jorge RE, Acion L, Moser D, Adams HP, Robinson RG. Escitalopram and enhancement of cognitive following stroke. Arch Gen Psychiatry. 2010;67(2):187–196. doi:10.1001/archgenpsychiatry.2009.185
13. Royall DR, Cordes JA, Román G. Sertraline improves executive function in patients with vascular cognitive impairment. J Neuropsychiatry Clin Neurosci. 2009;21(4):445–454. doi:10.1176/jnp.2009.21.4.445
14. Liu X, Zhang J, Sun D, Fan Y, Zhou H, Fu B. Effects of fluoxetine on brain-derived neurotrophic factor serum concentration and cognition in patients with vascular dementia. Clin Interv Aging. 2014;9:411–418. doi:10.2147/CIA.S58830
15. Serdar CC, Cihan M, Yucel D, et al. Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem Med. 2021;31(1):10502. doi:10.11613/BM.2021.010502
16. Association AP. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. American Psychiatric Publishing, Inc; 2000.
17. Moroney JT, Bagiella E, Desmond DW, et al. Meta-analysis of the Hachinski Ischemic Score in pathologically verified dementias. Neurology. 1997;49(4):1096–1105. doi:10.1212/WNL.49.4.1096
18. Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry. 1984;141(11):1356–1364.
19. Manos PJ, Wu R. The ten point clock test: a quick screen and grading method for cognitive impairment in medical and surgical patients. Int J Psychiatry Med. 1994;24(3):229–244. doi:10.2190/5A0F-936P-VG8N-0F5R
20. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
21. Mok EHL, Lam LCW, Chiu HFK. Category verbal fluency test performance in Chinese elderly with Alzheimer’s disease. Dement Geriatr Cogn Disord. 2004;18(2):120–124. doi:10.1159/000079190
22. Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8(3):271–276. doi:10.2466/pms.1958.8.3.271
23. Wechsler D. Wechsler Adult Intelligence Scale–(WAIS–IV).
24. Mowla A, Mosavinasab M, Pani A. Does fluoxetine have any effect on the cognition of patients with mild cognitive impairment? A double-blind, placebo-controlled, clinical trial. J Clin Psychopharmacol. 2007;27(1):67–70. doi:10.1097/JCP.0b013e31802e0002
25. Zittel S, Weiller C, Liepert J. Citalopram improves dexterity in chronic stroke patients. Neurorehabil Neural Repair. 2008;22(3):311–314. doi:10.1177/1545968307312173
26. Kozisek ME, Middlemas D, Bylund DB. The differential regulation of BDNF and TrkB levels in juvenile rats after four days of escitalopram and desipramine treatment. Neuropharmacology. 2008;54(2):251–257. doi:10.1016/j.neuropharm.2007.08.001
27. Groves N, O’Keeffe I, Lee W, et al. Blockade of TrkB but not p75NTR activates a subpopulation of quiescent neural precursor cells and enhances neurogenesis in the adult mouse hippocampus. Dev Neurobiol. 2019;79(9–10):868–879. doi:10.1002/dneu.22729
28. Surget A, Saxe M, Leman S, et al. Drug-dependent requirement of hippocampal neurogenesis in a model of depression and of antidepressant reversal. Biol Psychiatry. 2008;64(4):293–301. doi:10.1016/j.biopsych.2008.02.022
29. Nowacka MM, Obuchowicz E. Vascular endothelial growth factor (VEGF) and its role in the central nervous system: a new element in the neurotrophic hypothesis of antidepressant drug action. neuropeptides. 2012;46(1):1–10.
30. Geldmacher DS, Waldman AJ, Doty L, Heilman KM. Fluoxetine in dementia of the Alzheimer’s type: prominent adverse effects and failure to improve cognition. J Clin Psychiatry. 1994;55(4):161.
31. Hachinski V. The 2005 Thomas Willis Lecture: stroke and vascular cognitive impairment: a transdisciplinary, translational and transactional approach. Stroke. 2007;38(4):1396. doi:10.1161/01.STR.0000260101.08944.e9
32. Moorhouse P, Rockwood K. Vascular cognitive impairment: current concepts and clinical developments. Lancet Neurol. 2008;7(3):246–255. doi:10.1016/S1474-4422(08)70040-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
