Back to Journals » Clinical Ophthalmology » Volume 16
First Real-World, Multicenter, Post-Marketing, Retrospective Study of Dexamethasone Intraocular Suspension for Inflammation After Cataract Surgery
Authors Bacharach J, McCabe C, Jackson M , Rao S, Singh IP, Heersink S, Radcliffe N , Weinstock R, Paggiarino D, Patel K
Received 20 January 2022
Accepted for publication 23 May 2022
Published 3 June 2022 Volume 2022:16 Pages 1783—1794
DOI https://doi.org/10.2147/OPTH.S357267
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Scott Fraser
Jason Bacharach,1 Cathleen McCabe,2 Mitchell Jackson,3 Sanjay Rao,4 I Paul Singh,5 Sebastian Heersink,6 Nathan Radcliffe,7 Robert Weinstock,8 Dario Paggiarino,9 Keyur Patel9
1North Bay Eye Associates Petaluma, Petaluma, CA, USA; 2The Eye Associates, Bradenton, FL, USA; 3Jacksoneye Ophthalmology, Lake Villa, IL, USA; 4DeKalb Eye Consultants - Hauser-Ross Eye Institute, Sycamore, IL, USA; 5The Eye Centers of Racine & Kenosha, Racine, WI, USA; 6Eye Center South, Dothan, AL, USA; 7New York Eye Surgery Center, Bronx, NY, USA; 8The Eye Institute of West Florida, Largo, FL, USA; 9EyePoint Pharmaceuticals, Watertown, MA, USA
Correspondence: Jason Bacharach, North Bay Eye Associates, 104 Lynch Creek Way, Suite 15, Petaluma, CA, 94954, USA, Email [email protected]
Purpose: To evaluate dexamethasone intraocular suspension 9% (intraocular DXM) in real-world clinical use to manage inflammation associated with cataract surgery.
Setting: Patients who underwent cataract surgery and received intraocular DXM at 22 outpatient eye surgery centers in the US.
Design: Retrospective, observational chart review.
Methods: Records of all patients who received intraocular DXM from March to December 2019 at participating centers were reviewed.
Main Outcome Measures: Outcomes included anterior chamber cell (ACC) grades, anterior chamber flare (ACF) grades, and visual acuity, as well as intraocular pressure (IOP) and adverse events (AEs) at postoperative days (PODs) 1, 8, 14, 30. Descriptive statistics were generated.
Results: The study population included 527 patients (641 eyes), with glaucoma history in 66 patients (80 eyes). Among eyes with recorded ACC grades, the percentage with grade 0 increased from 40% at POD 1 to 89.7% at POD 30, with similar results in eyes with glaucoma history. Among eyes with recorded ACF grades, the percentage with grade 0 increased from 78.4% at POD 1 to 97.1% at POD 30. At POD 30, 96.6% eyes with recorded results achieved target acuity. Mean IOP was 18.6 mmHg at POD 1 but declined to ≤ 15.2 mmHg thereafter. Investigators reported 22 AEs in 20 patients, all reported mild or moderate, the most common: IOP increase (7 events).
Conclusion: Patients undergoing cataract surgery and treated with intraocular DXM showed favorable inflammatory and visual outcomes, without unanticipated safety problems, consistent with results of previous controlled clinical trials.
Keywords: cataract surgery, corticosteroids, dexamethasone, inflammation, intraocular suspension, ocular drug delivery systems
Introduction
In cataract surgery, tissue damage can induce ocular inflammation, resulting in intraocular vasodilation and increased vascular permeability.1,2 Consequent disruption and breakdown of the blood-ocular barrier increases anterior chamber cells (ACCs) and anterior chamber flare (ACF).1,3 Postoperative inflammation may lead to pain or discomfort, prolonged recovery, and visual symptoms.2,4
Treatment with topical anti-inflammatory drugs, including corticosteroids and non-steroidal anti-inflammatory drugs (NSAIDs), is widely employed in managing postoperative ocular inflammation.6 In general, the discretion of individual surgeons has guided anti-inflammatory treatment approaches.
Patient-administered postoperative topical treatment can pose adherence problems.4,7,8 Penetration of topical corticosteroids into the anterior chamber is limited, requiring administration up to 4 times a day, for 2 weeks or more. Patients, especially those who are elderly, may have difficulty administering medication properly.7
Dexamethasone intraocular suspension 9% (DEXYCU; EyePoint Pharmaceuticals, Watertown, MA) (intraocular DXM) is an alternative to topical agents for treatment of inflammation associated with cataract surgery.5 This medication is the first Food and Drug Administration (FDA)-approved intraocular treatment for postoperative ocular inflammation.4,5,9
Dexamethasone molecules are incorporated in a depot suspension formulation, enabling a rapid initial release of drug, followed by a gradual taper. A single injection at the conclusion of surgery is typically sufficient to control inflammation during the postoperative period.5 Intraocular DXM is administered behind the iris or into the capsular bag as a sterile, unpreserved suspension in a 0.005 mL volume at the end of surgery. Increasingly, administration into the capsular bag, at the edge of the intraocular lens optic, is found to produce reliable and consistent placement with favorable anti-inflammatory and safety outcomes.9
Intraocular DXM has been evaluated in two Phase 3 trials in patients undergoing cataract surgery;10,11 a randomized, double-masked placebo-control trial in patients undergoing phacoemulsification;10 and a randomized, open-label, active control trial comparing it with topical prednisolone acetate 1.0% ophthalmic suspension (QID for 3 weeks).11 A pooled analysis of the phase 3 trials found that intraocular DXM was not an independent risk factor for postoperative intraocular pressure (IOP) increase, compared to conventional topical corticosteroid.13 Intraocular DXM was comparable to the topical medication in overall safety, the primary study outcome, and in ACC clearing, an exploratory effectiveness endpoint.11,12
However, these trials by design excluded several clinical scenarios and could not address some management issues likely to be encountered in real-world practice.10,11 Although cataract and glaucoma often coexist, most patients with glaucoma or ocular hypertension are excluded from clinical trials assessing novel postoperative anti-inflammatory treatments. Also, in pivotal trials of postoperative ocular anti-inflammatory treatments, concomitant use of other medications used to manage postoperative inflammation is typically limited to rescue treatment.
“Real-world” observational studies of heterogeneous patient populations in clinical settings can complement controlled clinical trials in evaluating effectiveness and safety of treatments.14 We report a large-scale observational study of patients who received intraocular DXM for treatment of inflammation following cataract surgery. This population included patients with glaucoma and other ocular comorbidities and was diverse with respect to surgical procedures and concomitant medications used.
Materials and Methods
Design
This retrospective observational study (ClinicalTrials.gov Identifier NCT04290676) reviewed medical records from patients at multiple clinical centers in the US who received intraocular DXM for treatment of postoperative inflammation after cataract surgery. The study was reviewed and approved by an independent institutional review board (IntegReview IRB) and conducted in accordance with International Council for Harmonisation/Good Clinical Practice requirements as well as applicable federal and state regulations. As the study used only de-identified patient data and involved no patient contact, waivers of informed consent and HIPAA authorization were obtained.
Patient Population
Patients who underwent cataract surgery between March 2019 and December 2019 and received intraocular DXM for treatment of postoperative inflammation were eligible. Use of intraocular DXM was subsequent to the drug’s FDA approval (in February 2018) and in a manner consistent with the product labeling. While use of intraocular DXM at participating clinical centers was at the discretion of surgeons, all patients who received intraocular DXM at the centers were included in the study population.
Data Collection
Information was recorded from patient charts per usual practices at participating clinical centers, with no changes to centers’ ordinary clinical practice or documentation required for study participation. Data from charts were entered by the study coordinator or other designated, trained personnel at study sites into a password-protected electronic data capture system (Fusion, Axiom Real-Time Metrics). Data extracted included:
- Patient demographics and medical history, including history of glaucoma and diabetes
- Details of surgery, including affected eye, procedure type (eg, femtosecond laser-assisted surgery), concomitant micro-invasive glaucoma surgery (MIGS) procedure, and use of phenylephrine/ketorolac intraocular solution 1%/0.3% (Omidria)
- Administration of intraocular DXM
- Use of adjunctive topical NSAIDs and steroids
- Clinical outcomes at postoperative days (PODs) 1, 8, 14, 30
- Indices of patient and surgeon satisfaction
No patient-identifying data were extracted. The study was sponsored by EyePoint Pharmaceuticals and was contracted to an external entity to develop and maintain the platform for clinical data collection and training of study site staff.
Clinical Outcomes
Inflammatory activity was evaluated at postoperative visits using ACC and ACF grades per Standardization of Uveitis Nomenclature (SUN) grading schemes.15 Corrected distance visual acuity (CDVA) and uncorrected distance visual acuity (UCVA) were recorded, as well as achievement of target visual acuity as determined by the surgeon. Effectiveness of intraocular DXM versus topical steroid was ranked by surgeons (superior, comparable, inferior) for each visit.
Tolerability and Safety
Records of IOP were obtained, as available, for each postoperative visit. Postoperative surgical complications were ascertained by questionnaire. AEs were reported by investigators. Clinician investigators also answered a survey item asking whether intraocular DXM was “well tolerated” in the treated eye (yes or no).
Surgeon and Patient Satisfaction
Surgeons reported their satisfaction with intraocular DXM on a per-patient basis. Surgeons also rated patient satisfaction based on their impressions of individual patients’ satisfaction.
Statistical Analysis
Results for inflammatory activity as measured by ACC and ACF grade were recorded by eye and dichotomized (grade 0, grade >0). Similarly, results for visual acuity—CDVA and UCVA—were dichotomized (20/25 or better, worse than 20/25). These clinical outcomes were analyzed for the entire study population and by type of surgery (phacoemulsification and intraocular lens insertion alone, plus MIGS and/or femto) and concomitant medication (topical steroids, topical NSAID, phenylephrine/ketorolac).
Results for inflammatory activity (ACC, ACF) and visual acuity (CDVA, UCVA, attainment of target visual acuity) were analyzed for each of the PODs (1, 8, 14, and 30), as were the use of concomitant medications, mean IOP, and overall tolerability (questionnaire item: “Was DEXYCU well tolerated?”).
In this retrospective, clinical practice-based study, neither evaluation at every POD analyzed nor data for all outcomes assessed was required for inclusion. For each assessed outcome and POD, there were substantial numbers of eyes for which data was not recorded. For each outcome analyzed by POD, results are reported: for all eyes, including those with assessment data not recorded, and for only eyes with recorded assessment data.
In the subpopulation defined by history of glaucoma, inflammatory activity (ACC) was analyzed by POD, along with mean IOP and use of IOP-lowering medications.
In this observational study, only descriptive statistics were generated. No hypothesis testing was performed, and no inferential statistics were derived.
Results
Patients
Data from 527 patients (641 eyes) were included in the study (Table 1). Mean (SD) age was 71.5 (8.35) years, and 308 (58.4%) patients were female. History of glaucoma was recorded in 66 patients (80 eyes).
 |
Table 1 Demographic Characteristics |
Surgical Procedures and Concomitant Medication
Most commonly, 565 eyes received femtosecond laser-assisted cataract surgery (88.1%), and 58 eyes (9%) underwent phacoemulsification alone (see Supplemental Table 1). In 14 eyes (2.1%), procedures were considered complex, as defined by use of Malyugin ring (6, 0.9%), trypan blue staining (6, 0.9%), or iris hooks (2, 0.3%). Complications occurred in 16 (2.8%) eyes, and included intra-operative floppy iris (5, 0.8%), bleed (1, 0.2%), and other or missing (11, 1.8%).
Concomitant medications initiated at any time during treatment (ie, perioperatively, on the day of surgery, and at any postoperative assessment) are listed in Supplemental Table 1. The most common concomitant medications were topical NSAIDs and steroids. Intraocular DXM without concomitant NSAIDs or steroids was used in 150 eyes. With few exceptions, treatments were initiated perioperatively or on the day of surgery. At POD 1, a topical NSAID was initiated in 92 eyes (14.4% of eyes) and a topical steroid in 23 (3.6%); at PODs 8, 14, and 30, these treatments were initiated in fewer than 1% of eyes.
ACC Clearing
All Patients
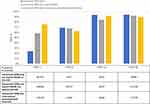
Proportions of eyes with a record of ACC clearing (ACC grade 0) at PODs 1, 8, 14, and 30 are shown in panel A of Figure 1. Among eyes whose ACC grades were recorded, the percentage with ACC grade 0 increased from 40% (214 of 535 recorded eyes) at POD 1 to 89.7% (297 of 331 recorded eyes) at POD 30, although the number of eyes with recorded ACC grade differed among PODs.
Patients with Glaucoma History
In patients with glaucoma history, the percentage of eyes with recorded ACC grades that exhibited clearing increased from 51.6% (31 of 60 recorded eyes) at POD 1 to 90.2% at (37 of 41 recorded eyes) at POD 30, as shown in panel B of Figure 1. Again, the numbers of eyes with no grading recorded varied among PODs.
ACC Grade by Concomitant Medication
Results for ACC grading at each study visit for eyes treated with intraocular DXM alone and those also receiving concomitant topical NSAID are shown in Figure 2. Among eyes treated with intraocular DXM alone whose ACC grade was recorded at the visit, the proportion with grade 0 increased from 23.8% at POD 1 to 94.1% at POD 30. Of eyes with a recorded ACC grade at the visit, 58.6% of those that received an adjunctive NSAID (but no topical steroid) had ACC grade 0 at POD 1, increasing to 92.5% at POD 30.
ACF Clearing
All Patients
Among eyes whose ACF grade was recorded, the percentage of eyes with grade 0 increased from 78.4% at POD 1 to 97.1% at POD 30, although the numbers of eyes with recorded ACF grades differed between PODs.
By Concomitant Medication Use
Among eyes treated with intraocular DXM alone with recorded ACF grade at the visits, 78.7% had ACF clearing at POD 1, and ≥98% had clearing at subsequent PODs. Similarly, of eyes treated with intraocular DXM plus an NSAID (but no topical steroid) whose ACF grade was recorded, 78.9% had ACF clearing at POD 1 and 98.4% had clearing at POD 30.
Visual Acuity
The results for CDVA, UCVA, and achievement of target visual acuity at POD 30 are summarized in Table 2. At POD 30, 96.6% eyes with recorded results achieved target acuity.
 |
Table 2 Visual Acuity at Postoperative Day 30 |
Rank Effectiveness versus Topical Steroid
At POD 1, of 276 eyes with rank effectiveness data, intraocular DXM was ranked superior or comparable to the expected resolution of inflammation with topical steroids by the surgeon in 271 (98%). Results were identical or similar at days 8, 14, 30.
Intraocular Pressure
All Patients
Mean IOP by POD for all eyes is shown in Figure 3. Mean IOP declined after POD 1. In subgroups defined by concomitant medication, mean IOP at POD 1 ranged from 17.5 mmHg to 19.1 mmHg, with IOP tending to decrease at subsequent days. Results were similar for procedure-type subgroups, with mean IOP at POD 1 ranging from 17.1 mmHg to 18.6 mmHg.
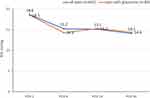 |
Figure 3 Mean intraocular pressure (IOP) by POD for all eyes undergoing surgery (n=641) and eyes with glaucoma (n = 80). |
Patients with Glaucoma History
Mean IOP by POD for eyes with glaucoma is shown in Figure 3. Mean IOP declined after POD 1. Use of IOP lowering medications for patients with glaucoma in this study was recorded; 5 (6.3%) eyes were treated with 1 IOP-lowering medication and 4 (5.0%) were treated with 2. In no patient with glaucoma was IOP-lowering medication initiated after POD 1.
Adverse Events
Investigator-Reported AEs
Investigators reported a total of 22 AEs in 20 patients (Table 3). The most commonly reported were IOP increase (7 events), corneal edema (6), and iritis (4). Events were rated mild (11) or moderate (10) in severity; a single event, termed “retained cortex in anterior chamber,” was not rated. Of these AEs, 8 were judged by the reporting investigator to be definitely related (3), probably related (2), or possibly related (3) to intraocular DXM; the 14 other AEs were judged to be unrelated.
 |
Table 3 Treatment-Emergent Adverse Events Spontaneously Reported by Investigators |
Questionnaire Item on Tolerability
To the questionnaire item completed by surgeons on whether intraocular DXM was well tolerated at POD 1, a “no” response was recorded for only 1 (0.2%) eye. For 513 eyes (80%), the response was “yes,” and for 110 (17.2%), no response was recorded.
Satisfaction Surveys
Survey data on surgeon satisfaction and surgeon-reported patient satisfaction were available for 506 patients. Of these, 92% of surgeons were “very satisfied” or “satisfied” with intraocular DXM, and 84% were “very satisfied” or “satisfied” with its ease of use. For 81% of patients, the surgeons reported that the patient was “very satisfied” or “satisfied.”
Discussion
Phase 3 trials of intraocular DXM for the management of postoperative inflammation excluded certain patient types and clinical scenarios routinely encountered in real-world practice. This retrospective observational study was aimed to complement these trials with results from a heterogeneous real-world patient population treated by multiple surgeons. Although a variety of surgical interventions and concomitant medications were used in this study, including topical corticosteroids and NSAIDs, some patients (23.4% of eyes) received intraocular DXM alone for postoperative inflammation, and results overall were consistent with those from phase 3 clinical trials.
In the controlled clinical trials, concomitant anti-inflammatory medication was permitted only in rescue treatment. Use of rescue medication was uncommon in patients receiving intraocular DXM (eg, 10% by day 8 for the marketed dose in the placebo-controlled trial). In our analyses by concomitant medication, rates of ACC and ACF clearing were favorable for eyes treated with intraocular DXM alone as well as for eyes receiving other anti-inflammatory medications (Figure 2). Initiation of concomitant medication perioperatively or on day of surgery was common, perhaps reflecting clinicians’ limited experience with intraocular DXM or their routine use of NSAIDs for pain and inflammation management.
In our study population, mean IOP at POD 1 was 18.6 mmHg and declined at later visits. Elevated IOP was spontaneously reported as an AE in 7 (1.3%) patients. These results accord with those in the placebo-controlled trial, in which increases of 10 mmHg or more from baseline were observed in 29% of patients treated with the currently recommended dose, but mean IOP did not exceed 21 mmHg at any assessment up to 30 days. In the active-control trial, a higher incidence of IOP increase was observed with intraocular DXM than with topical prednisolone (11.1% vs 3.6%). However, a post hoc analysis of pooled trial data found that risk did not significantly differ for intraocular DXM versus topical prednisolone. Between the two studies, 25 (8.9%) eyes treated with intraocular DXM received a topical IOP-lowering medication.13
An important feature of this study was inclusion of patients with history of glaucoma. In this subgroup, the rate of ACC clearing at day 8 was consistent with that in intraocular DXM clinical trials (34 of 50 [68%] of eyes graded at POD 8), and mean IOP at PODs did not exceed the 18.5 mmHg observed at POD 1. A mean of 1.4 IOP-lowering medications were used, and none were initiated after POD 1, suggesting an absence of clinically important IOP increases. Patients with glaucoma may particularly benefit from the use of intraocular DXM to help limit their eyedrop burden during the postoperative period.
Surgeons participating in this study completed satisfaction surveys, and a majority were “very satisfied” or “satisfied” with the ease of use of intraocular DXM. Notably, patients in this study were treated during the 9 months immediately after intraocular DXM became commercially available; thus, most surgeons in these settings were relatively unfamiliar with the product and its administration. As clinical experience with intraocular DXM has grown, surgeons have experimented with techniques to make administration more consistent and reliable.9 Many surgeons have shifted from placement into the ciliary sulcus, immediately behind the iris, toward placement into the lenticular capsule. This technique enables better surgeon visualization of the drug depot and ensures that it remains in place, out of direct contact with the iris, ciliary body, trabecular meshwork, and corneal endothelium.9
Surgeons were also asked to rate patient satisfaction with intraocular DXM; results (81% “very satisfied” or “satisfied”) were consistent with patient survey data from the phase 3 active-control trial of intraocular DXM. Among patients who received intraocular DXM at the labeled dose level and responded to the survey, more than two-thirds (68.7%) strongly agreed that not having to use eyedrops after cataract surgery was very convenient, and a similar proportion (67.8%) strongly agreed that they would opt for not using eyedrops after cataract surgery in the future.11
A more recent, small-scale study in patients (N = 27) undergoing bilateral cataract surgery assigned one eye of each patient to receive intraocular DXM and an intracameral antibiotic, while the fellow eye received topical steroid and antibiotic formulations. All but one of these patients (96%) preferred intraocular medications over eyedrops.12
Limitations of this current study include those inherent to a retrospective observational study design. Selection of patients for treatment with intraocular DXM was made by individual clinician investigators; however, all patients who received the medication at the centers during the studied time interval were included. The study relied on chart information recorded per the practices of individual clinical centers, without prospectively defined requirements on assessments or timing of evaluations. For indices of postoperative inflammation and other variables, throughout the 30-day postoperative period, substantial numbers of evaluations were not recorded or were missing. It is not known to what extent outcomes might differ, if at all, between patients with unrecorded observations and those with data. The study also did not obtain detailed baseline data on variables such as visual acuity or IOP. Despite analyses of subgroups, this study was not designed to test hypotheses or allow statistical comparisons.
Conclusion
This is the first large postmarketing study of DEXYCU, and it yielded data on multiple effectiveness and safety outcomes from on a diverse population of patients undergoing cataract surgery and receiving intraocular DXM in real-world settings. It thereby complements results from previously reported clinical trials in establishing intraocular DXM as an effective and well-tolerated single-dose option for the management of postoperative ocular inflammation.
Data Sharing Statement
Because study participants did not agree for their data to be made public, supporting data are not available for this study. Select deidentified data may be made available upon reasonable request to the corresponding author, Jason Bacharach.
Acknowledgments
The authors acknowledge the participation of the following investigators and centers:
Robert Sorenson, MD, Inland Eye Specialists, Hemet, California; John Hovanesian, Harvard Eye Associates, Laguna Hills, California; Dan B. Tran, MD, Coastal Vision Medical Group, Orange, California; Francis Price, MD, Price Vision Group, Indianapolis, Indiana; Jeffrey L. Wexler, MD, Physicians Eyecare Center, Baltimore, Maryland; Doug O. Dehning, MD, Discover Vision Centers, Independence, Missouri; Steven M. Silverstein, MD, Silverstein Eye Centers Kansas City, Missouri; Navin Tekwani, MD, Tekwani Vision Center, Saint Louis, Missouri; Cynthia Matossian, MD, Surgery Center of Central New Jersey, Pennington, New Jersey; Michael Savetsky, MD, SightMD, PLLC Hauppauge, New York; Eric Donnenfeld, MD Island Eye Surgicenter, Westbury, New York; Mark Pyfer, MD, Wills Surgery Center, Jenkintown, Pennsylvania; Subba Gollamudi, MD, VRF Eye Specialty Group, Memphis, Tennessee; Victor H. Gonzalez, MD, Valley Retina Institute, PA, McAllen, Texas.
Weinstock RJ. Dexamethasone intraocular suspension 9% after cataract surgery: data from a retrospective study. Presented at the American Academy of Ophthalmology Annual Meeting. November 13–15, 2020; virtual.
Radcliffe N. Use of dexamethasone intraocular suspension 9% in patients with glaucoma: results from a retrospective study. Presented at the Association for Research in Vision and Ophthalmology Annual Meeting. May 1–7, 2021; virtual.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by EyePoint Pharmaceuticals, Watertown, Massachusetts, USA.
Disclosure
Jason Bacharach is a consultant and speaker for EyePoint. Cathleen McCabe reports grants, personal fees from Alcon, during the conduct of the study; grants and/or personal fees from Alcon, Bausch and Lomb, Novartis, Omeros, Ocular Therapeutix, EyePoint, Allergan, Imprimis, Dompe, Johnson and Johnson Vision, and Science Based Health, outside the submitted work. Mitchell Jackson is a consultant and speaker for EyePoint, Omeros, and Ocular Therapeutix. Sebastian Heersink received research support from EyePoint for conducting this study. He also reports grants and/or personal fees from Alcon, Allergan, Eyepoint, Glaukos, Genentech, Johnson and Johnson, Iridex, Ivantis, Kala, Lenstec, grants from and ownership for Lunovus, grants from Nicox, Rayner, Sight Sciences, and Zeiss, during the conduct of the study. Sanjay Rao received research support from EyePoint for conducting this study. Nathaniel Radcliffe is a consultant for CATS, LLC, Allergan, Alcon, Novartis, Eyenovia, Lumenis, Equinox, Iridex, Aerie, Bausch and Lomb, BVI, EyePoint, Ivantis, Glaukos, Alimera, New World Medical, Ocular Therapeutics, Kala, SpyGlass, Sight Science, Thea, Reichert, Shire, Carl Zeiss Meditec, and Omeros; and a speaker for Allergan, Lumenis, Iridex, Aerie, Bausch and Lomb, New World Medical, and Sight Science; and has stock or stock options in Equinox, Sight Sciences, SpyGlass, Ivantis, ELT Sight, CATS, LLC, and Vialase. I Paul Singh is a speaker for EyePoint, B+L, Kala, Ocular Therapeutix, Glaukos, Alcon, Sight Sciences, New World Medical, Elios, Nicox, and iStar Medical; consulting for Imprimus, outside the submitted work. Robert Weinstock is a consultant for EyePoint, Alcon, Bausch and Lomb, Johnson and Johnson, and Lensar. Dario Paggiarino and Keyur Patel are employees of EyePoint Pharmaceuticals, Watertown, Massachusetts, USA. The authors report no other conflicts of interest in this work.
References
1. El-Harazi SM, Feldman RM. Control of intra-ocular inflammation associated with cataract surgery. Curr Opin Ophthalmol. 2001;12(1):4–8. doi:10.1097/00055735-200102000-00002
2. Porela-Tiihonen S, Kokki H, Kaarniranta K, Kokki M. Recovery after cataract surgery. Acta Ophthalmol. 2016;94(Suppl 2):1–34. doi:10.1111/aos.13055
3. Shah SM, Spalton DJ. Changes in anterior chamber flare and cells following cataract surgery. Br J Ophthalmol. 1994;78(2):91–94. doi:10.1136/bjo.78.2.91
4. Shah TJ, Conway MD, Peyman GA. Intracameral dexamethasone injection in the treatment of cataract surgery induced inflammation: design, development, and place in therapy. Clin Ophthalmol. 2018;12:2223–2235. doi:10.2147/OPTH.S165722
5. Grzybowski A, Brockmann T, Kanclerz P, Pleyer U. Dexamethasone intraocular suspension: a long-acting therapeutic for treating inflammation associated with cataract surgery. J Ocul Pharmacol Ther. 2019;35(10):525–534. doi:10.1089/jop.2019.0072
6. AAO PPP Cataract/Anterior Segment Panel, Hoskins Center for Quality Eye Care. Cataract in the adult eye PPP; 2016. Available from: https://www.aao.org/preferred-practice-pattern/cataract-in-adult-eye-ppp-2016.
7. Schwartz GF, Hollander DA, Williams JM. Evaluation of eye drop administration technique in patients with glaucoma or ocular hypertension. Curr Med Res Opin. 2013;29(11):1515e1522. doi:10.1185/03007995.2013.833898
8. An JA, Kasner O, Samek DA, Lévesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–1861. doi:10.1016/j.jcrs.2014.02.037
9. Osher RH, Weinstock RJ. Dexamethasone intraocular suspension 9% in the capsular bag [published online ahead of print, 2020 Nov 27]. J Cataract Refract Surg. 2020. doi:10.1097/j.jcrs.0000000000000458
10. Donnenfeld E, Holland E. Dexamethasone intracameral drug-delivery suspension for inflammation associated with cataract surgery: a randomized, placebo-controlled, Phase III trial. Ophthalmology. 2018;125(6):799–806. doi:10.1016/j.ophtha.2017.12.029
11. Donnenfeld ED, Solomon KD, Matossian C. Safety of IBI-10090 for inflammation associated with cataract surgery: phase 3 multicenter study. J Cataract Refract Surg. 2018;44(10):1236–1246. doi:10.1016/j.jcrs.2018.07.015
12. Hovanesian JA, Donnenfeld ED. Patient-reported tolerance and satisfaction with intraocular administration of dexamethasone and moxifloxacin vs a topical regimen.
13. Matossian C, Hovanesian J, Bacharach J, Paggiarino D, Patel K. Impact of dexamethasone intraocular suspension 9% on intraocular pressure following routine cataract surgery: post hoc analysis. J Cataract Refract Surg. 2020. doi:10.1097/j.jcrs.0000000000000363
14. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35(11):1763–1774. doi:10.1007/s12325-018-0805-y
15. Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.