Back to Journals » Drug Design, Development and Therapy » Volume 10
Fimasartan for independent reduction of blood pressure variability in mild-to-moderate hypertension
Authors Shin M, Kang D, Kim C, Cho EJ, Sung K, Kang S, Kim DS, Joo S, Lee S, Hwang K, Park JB
Received 29 February 2016
Accepted for publication 4 April 2016
Published 5 May 2016 Volume 2016:10 Pages 1573—1580
DOI https://doi.org/10.2147/DDDT.S107433
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Wei Duan
Mi-Seung Shin,1 Dae Ryong Kang,2 Changsoo Kim,3 Eun Joo Cho,4 Ki-Chul Sung,5 Seok-Min Kang,6 Dong-Soo Kim,7 Seung Jae Joo,8 Seung Hwan Lee,9 Kyung-Kuk Hwang,10 Jeong Bae Park11
1Division of Cardiology, Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, 2Office of Biostatistics, Ajou University School of Medicine, Suwon, 3Department of Preventive Medicine, Yonsei University College of Medicine, 4Division of Cardiology, Department of Internal Medicine, St Paul’s Hospital, Catholic University of Korea, 5Division of Cardiology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 6Cardiology Division, Severance Cardiovascular Hospital and Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, 7Division of Cardiology, Paik Hospital, Inje University College of Medicine, Busan, 8Division of Cardiology, Jeju National University Hospital, Jeju, 9Division of Cardiology, Wonju Severance Christian Hospital, Wonju Medical College, Yonsei University, Wonju, 10Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, 11Division of Medicine/Cardiology, Department of Internal Medicine, Cheil General Hospital, Dankook University College of Medicine, Seoul, South Korea
Background: The angiotensin receptor antagonist fimasartan lowered blood pressure (BP) in a previous large population study. The purpose of this study was to evaluate whether fimasartan treatment for 3 months affects clinical and home BP variability in addition to reducing BP.
Methods: The study enrolled 1,396 patients (mean age 56.2±10.0 years; males 53.6%) with mild-to-moderate hypertension who had a complete set of home BP measurements (morning and evening) and metabolic risk evaluation. During the 3 months of study, fimasartan alone was used to control BP at a daily dose of 30–120 mg. Clinical and home BP measurements were performed before and after the 3-month treatment. BP variability included beat-to-beat variability (clinical) and day-to-day variability (home).
Results: Fimasartan reduced BP after 3 months of treatment. The average reduction of clinical systolic BP (c-SBP) was 15.08±18.36 mmHg (P<0.0001), and the average reduction of morning home SBP (m-SBP) was 11.49±19.33 mmHg (P<0.0001). Beat-to-beat variability as standard deviation (SD) of c-SBP was reduced from 4.56±3.22 to 4.24±3.11 mmHg (P=0.0026). Day-to-day variability as SD of m-SBP was reduced from 7.92±6.74 to 6.95±4.97 mmHg (P<0.0001). Multiple regression analysis revealed an independent association between the change in the SD of c-SBP and the change in c-SBP (P=0.0268) and, similarly, between the change in the SD of m-SBP and the change in m-SBP (P=0.0258), after adjusting for age, sex, body mass index, and change in mean BP.
Conclusion: This study indicated that 3 months of fimasartan treatment reduced day-to-day BP variability independent of BP reduction in patients with hypertension.
Keywords: angiotensin receptor blockers, hypertension, blood pressure variability
Introduction
Blood pressure (BP) measured in the clinic does not provide comprehensive information about an individual’s BP profile and may be of limited prognostic value, thus requiring out-of-office BP monitoring.1,2 Home BP can be measured repeatedly in the comfort of the patient’s own home in a relaxing environment, which provides information about day-to-day BP variability (BPV) and enables a more accurate understanding of a subject’s BP profile. Home BP has been widely accepted as a useful tool for clinical management of patients with hypertension and cardiovascular disease.
BP is characterized by marked temporal fluctuations showing beat-to-beat variability, 24-hour variability, day-to-day variability, and visit-to-visit variability. Clinically, BPV is a well-known risk factor for cardiovascular events and is associated with target organ damage and all-cause mortality that is independent of office BP levels.3–8 Beat-to-beat variability or 24-hour variability reflects increases in central sympathetic drive, decreases in arterial or cardiopulmonary reflex, and increases in arterial stiffness.9,10 Humoral, rheological, and emotional factors and behavioral influences also can be involved in BPV. By contrast, day-to-day variability or visit-to-visit variability is proposed to be due to increased arterial stiffness, improper dosing or titration of antihypertensive medication, poor medication compliance, and seasonal variations in BP.11,12
Day-to-day BPV is independent of beat-to-beat BPV and may have significantly different effects on hypertension prognosis. Recent studies show that increased day-to-day home BPV is associated with cardiovascular risk, severity of target organ damage in patients with hypertension13 or diabetes mellitus,14 and cardiovascular mortality in a community-dwelling population.15 In the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure-Lowering Arm trial, visit-to-visit systolic BPV during treatment was a strong predictor of stroke and coronary events independent of mean levels of clinical or ambulatory systolic BP (SBP) in patients with hypertension.16 Therefore, reducing both BPV and mean BP has been recognized as a potential target for improved management of hypertension to prevent cardiovascular events, particularly stroke.6,16
Several small-scale and heterogeneous human studies on the effects of antihypertensive drugs report conflicting results. Calcium channel blockers such as amlodipine, but not beta-blockers, confer favorable effects to decrease home BPV.17 Other studies reported increased home BPV after treatment with beta-blockers.18,19 Inconsistent results also were observed even within the same class of antihypertensive medication, such as angiotensin II receptor blockers (ARBs).20–22
Fimasartan is an ARB that effectively and safely reduced high BP in the Safe-KanArb study.23 However, its effect on reducing BPV has not yet been determined. The objective of the present study was to determine whether fimasartan reduced BPV in the clinic and at home after 3 months of treatment in hypertensive patients with low-to-moderate cardiovascular risk.
Methods
This investigation is part of the K-MetS Study, which is a prospective, multicenter, single-arm, observational study. The study design, socioeconomic and demographic characteristics of the study, and project details have been described in our previous article.24 This study was approved by the Institutional Review Board Committee at the Cheil General Hospital, on behalf of 582 primary care clinics. Another ten university hospitals in South Korea approved this study through their own Institutional Review Board committees. Informed consent was obtained from all study subjects.
Study population
A total of 10,601 hypertensive patients from 582 primary clinics and eleven university hospitals were enrolled between October 17, 2011 and October 31, 2012. Patients were required to meet the following inclusion criteria: 1) diagnosed with hypertension, at least 20 years old, and intend to use fimasartan; 2) agree to participate in the study and sign the informed consent form; and 3) maintain a fasting state at each visit. Patients who were treated with fimasartan at baseline were excluded.24 Finally, 1,396 patients were enrolled who were treated with fimasartan at a daily dose of 30–120 mg for 3 months, completed the 3-month follow-up visits, and scheduled BP measurements. Patients were enrolled in three different groups: naïve, switch, and add-on. In naïve group, patients had no previous antihypertensive medication and received fimasartan. In switch group, patients were switched from other antihypertensive drug in the baseline to fimasartan and in an add-on group, patients who received antihypertensive drug also received fimasartan as an add-on therapy.
BP measurement
The Omron HEM-7220 and the Omron HEM-7200 (both Omron, Tokyo, Japan) were used to measure BP in the clinic and at home, respectively.25 These are upper-arm cuff devices based on the cuff automated-oscillometric principle. Clinical BP measurements were performed under standardized conditions (in the same arm by the same physician or nurse). The study participants were educated about self-measurement of BP at home. They were instructed to measure their BP in the morning and evening. An average of two or more BP readings at 2-minute intervals from the same arm was recorded in the morning and evening for 7 consecutive days. Morning BP was measured within 1 hour of waking, after urination, in the sitting position, after resting for 5 minutes, and before taking medications or eating. In the evening, BP was measured before going to bed, after resting for 5 minutes, and in the sitting position. An average of 6 days of recordings from the 2nd to the 7th day was used for the analysis. Baseline assessment included a health questionnaire and BP measurements and was conducted before and after the 3-month treatment with fimasartan.24 Clinical BPV, which measures beat-to-beat variability, was defined as the standard deviation (SD) of clinical systolic BP (c-SBP) measured three times at 2-minute intervals. Home BPV, which represents day-to-day BPV, was defined as the SD of morning home systolic BP (m-SBP).
Data analysis
The baseline characteristics of the study subjects were compared between sexes using the χ2 test for dichotomous variables or the independent t-test for continuous variables. Differences between measured variables (eg, BP) were examined using the paired t-test between baseline and after 3 months of follow-up. We analyzed males and females separately because sex may affect BPV.26 To evaluate the potential factors associated with clinical or home SBP variability, both simple and multiple linear regression analyses were conducted. Multiple linear regression models included potential factors such as clinical or home average SBP and diastolic BP (DBP), sex, age, history of cardiovascular disease, and smoking. This was done because most of these factors have a positive relationship with BPV, in part due to the stiffening influence on large- and medium-sized arteries, with an increase in the pressure excursions within the arterial compartment. All analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
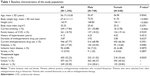
Baseline demographic and clinical characteristics of the participants are presented in Table 1. A total of 1,396 participants were enrolled; the mean age was 56.17±10.0 years; 17.55% had diabetes, 6.88% had ischemic heart disease, and 0.93% had stroke.
Changes in BP during the study
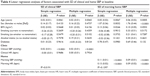
At baseline, the mean c-SBP and clinical DBP levels were 142.39±17.00 and 88.03±11.35 mmHg, respectively. These values were significantly reduced to 127.32±13.14 and 79.37±9.40 mmHg (P<0.0001 for both), respectively, after 3 months of fimasartan treatment (Table 2). m-SBP and morning home DBP levels were 138.80±19.81 and 83.26±13.16 mmHg, respectively; these were significantly reduced after 3 months of fimasartan treatment to 127.32±16.72 and 76.62±11.32 mmHg (P<0.0001 for both), respectively. The same pattern was observed for evening home SBP (e-SBP) and evening home DBP after 3 months of fimasartan treatment; e-SBP was 137.57±20.53 mmHg and declined to 126.33±17.06 mmHg, and evening home DBP was 81.35±13.29 mmHg and declined to 75.07±11.44 mmHg (P<0.0001 for both).
Changes in BPV during the study
At baseline, the SDs of c-SBP and clinical DBP were 4.56±3.22 and 3.19±2.45 mmHg, respectively (Table 3). After 3 months of fimasartan treatment, the SDs of c-SBP and DBP were significantly reduced to 4.24±3.11 mmHg (P=0.0026) and 2.94±2.20 mmHg (P=0.0024), respectively. The SDs of m-SBP and morning home DBP also showed significant reduction from 7.92±6.74 and 5.30±3.98 mmHg to 6.95±4.97 and 4.83±3.23 mmHg (P<0.0001 and P=0.0002), respectively. The same trend was observed for the SDs of evening home SBP and DBP; SD of e-SBP declined from 8.39±6.94 to 7.16±5.38 mmHg (P<0.0001), and SD of evening home DBP declined from 5.80±4.13 to 5.16±3.32 mmHg (P<0.0001). Figure 1 shows that the correlation between the SD of c-SBP and the SD of m-SBP was weak at baseline and then became stronger after 3 months of fimasartan treatment. The same pattern was observed for the SD of c-SBP and e-SBP. Figure 2 summarizes the observed BP changes in c-SBP and home SBP after 3 months of follow-up.
Regression analyses of BPV at baseline and after fimasartan treatment can identify factors associated with the change in BPV (SD) in the clinic and at home
At baseline, simple and multiple regression analyses indicated that the SD of c-SBP was independently associated with c-SBP (P<0.0001 for both), and the SD of m-SBP was independently associated with m-SBP (P<0.0001 for both). Both simple and multiple regression analyses showed that the SD of m-SBP was independently associated with age, female sex, and m-SBP (P=0.0067 and P=0.0005, P=0.0032 and P<0.0001, P<0.0001 and P<0.0001, respectively), but only the simple regression analysis showed an association between the SD of m-SBP and body mass index (P=0.0246 and P=0.0553, respectively) (Table 4).
Simple and multiple regression analyses (adjusted for age, sex, body mass index, and change in mean arterial pressure) were performed to elucidate any factors associated with reduced BPV in the clinic and at home after 3 months of fimasartan treatment. The change in the SD of c-SBP was independently associated with the change in c-SBP (P<0.0001 and P=0.0268, respectively), and the change in the SD of m-SBP was independently associated with the change in m-SBP (P<0.0001 and P=0.0258, respectively) (Table 5).
Discussion
The major finding of this study was that after 3 months of fimasartan treatment, clinical and home BPVs were significantly reduced independent of strong BP reduction. These results were derived primarily from the general practitioners and participants with relatively low-to-moderate hypertension risk, and thus represent unbiased BP data in a real clinical setting.
In our study, clinical BPV is calculated as the SD of three consecutive readings on the same patient in the clinic, and thus represents beat-to-beat BPV. By contrast, home BPV represents day-to-day variability of BP measured by the patients themselves at home for 7 consecutive days. BPV is thought to result from various intrinsic and extrinsic factors, although it is poorly understood. Beat-to-beat variability is known to be more strongly influenced by increased central sympathetic drive, decreased arterial and cardiopulmonary reflex, and humoral, rheological, behavioral, and emotional factors.27 Day-to-day variability has been reported to depend more strongly on arterial stiffness, improper dosing or titration of medication, poor medication compliance, and irregularity of self-measurements performed at home.4,27
Clinical BP has been shown to be strongly correlated with home BP, but the correlation between clinical BPV and home BPV has not been elucidated. Home BP measurement is reported to reflect the patient’s true BP because measurements are recorded multiple times throughout the day in a comfortable environment. This means that the “white coat effect” can be ruled out. Therefore, home BP measurement is a better predictor of cardiovascular morbidity and mortality. BPV was assessed by home BP measurement in our study. The results are supported by demonstrating a relationship of day-to-day BPV with cardiovascular outcomes, which is independent of mean BP.15,16 The Finn-Home Study confirmed this by showing that morning day-to-day BPV is a predictor of cardiovascular events after adjusting for age and mean home BP.28 Other studies also demonstrated this association15,28 and the association with increased risk of cardiac, vascular, and renal organ damage.13 The reduction of BPV is recognized as a potential target for improved management of hypertension to prevent cardiovascular events.
There have been conflicting results regarding the capacity of antihypertensive drugs to reduce BPV. In general, calcium channel blockers have been reported to reduce BPV, which was determined by the SD of 24-hour ambulatory BP,29,30 and were superior to enalapril in the prevention of coronary events in patients with angiographically proven coronary artery disease and controlled BP.31 Some ARBs were shown to reduce BPV, whereas others did not show any effects. In the X-CELLENT study, 3 months of candesartan treatment did not show any effect on BPV evaluated by 24-hour BP monitoring.30 Valsartan did not significantly change BPV in patients with hypertension after 12 months of treatment, despite reducing BP.29 In a recent study with home monitoring of BP, valsartan increased individual SD of morning SBP, but telmisartan did not affect BP after its use as an add-on agent in patients on amlodipine monotherapy.32 In an animal study, the superiority of telmisartan over valsartan in sustained BP control and reduction of BPV was attributed to further suppression of sympathetic activity and improvement of the baroreceptor reflex.33 Based on this evidence, the ARB-mediated reduction of BPV might not be due to its classic effects, but instead may be due to the effects of its own drug characteristics.
In our study, 3 months of fimasartan treatment significantly reduced BP and BPV in the clinic and at home. Although the methods of measuring BPV differ, the reductions in SD after fimasartan treatment were similar to the results of the X-CELLENT study with amlopidine.30 A reduction in beat-to-beat variability probably indicates a positive influence on its physiological mechanism, which may be attributable to a fimasartan-mediated reduction in central sympathetic drive. Factors that result in day-to-day variability, including increased arterial stiffness, improper dosing or titration of antihypertensive medication, and poor medication compliance, cannot be readily changed with 3 months of fimasartan treatment. However, we clearly observed a reduction in BP after fimasartan treatment, indicating better BP control, which in turn might have led to better BPV control. Further research is needed to identify the pharmacological mechanisms behind these effects.
To the best of our knowledge, the present study provides the first prospective evidence that fimasartan stabilizes day-to-day home systolic BPV. This conclusion was derived from data on measurement of BP in real clinical practice and self-measurement at home, not at a highly selected tertiary center. Although this study did not identify the exact mechanism of fimasartan-mediated BPV reduction, the efficacy of fimasartan to reduce BPV was observed in home BPV independent of clinical BPV. The effect of fimasartan on reducing home systolic BPV may be related to its positive effects on hypertension prognosis shown by recent population-based data, which suggest that higher BPV is associated with increased all-cause mortality. Therefore, we can presume that hypertensive patients with elevated day-to-day BPV may benefit from treatment with fimasartan.
Study limitations
This study has some limitations that require consideration. First, there is limited information concerning the underlying mechanism of BPV reduction. However, reduced mean SBP may imply amelioration of autonomic nervous system regulation. Second, the quality of the measurement procedure could have affected the BPV data, although the participants were instructed to measure BP under relatively controlled conditions. The details of home BP data were blinded until final analysis; therefore, information bias was probably not a significant contributing factor to the measurement and evaluation of home BPV. Third, potential confounding factors of BPV, including those related to diet, psychological factors, and drug compliance, were not investigated in the present study.
Perspectives
Potential confounding factors of BPV, such as diet, psychological factors, and drug compliance, should be investigated in future studies. Further studies on the change in clinical BP, morning BP, and BPV between diabetic and nondiabetic patients may be necessary as the findings may provide some insight into the mechanism of fimasartan on day-to-day BPV (eg, arterial stiffness related to diabetes). Studies on the effects of ARBs in different populations (eg, uncontrolled or resistant hypertension) will be necessary. Whether the change in BPV is dependent on the fimasartan dosage remains to be analyzed. Fimasartan may have additional beneficial effects on cardiovascular protection by reducing BPV in addition to significantly reducing the mean levels of home BP. Whether reduction in BPV translates into long-term clinical benefits, such as reduction of all-cause and cardiovascular mortality and target organ damage, needs to be investigated in future research. The observed superiority of fimasartan over other antihypertensive drugs in reducing BPV and preventing cardiovascular events warrants further investigation within clinical settings.
Conclusion
The angiotensin receptor antagonist fimasartan is known to have a strong antihypertensive effect. However, the effects on targets other than BP are unknown. This study evaluated whether fimasartan treatment affected clinical and home BP variability in addition to reducing BP. Three months of fimasartan treatment reduced day-to-day BP variability independent of BP reduction in patients with mild-to-moderate hypertension. The results suggest that fimasartan attenuates BP fluctuations and provides better control of hypertension. Fimasartan treatment also significantly reduced day-to-day BP variability at home independent of BP reduction, which may provide an additional benefit for prevention of cardiovascular events.
Acknowledgments
This study was funded by Boryung Pharmaceutical Company, South Korea. We thank Ji Hye Jang for data analysis and Eura Muyang Kim for writing support.
Disclosure
The authors report no conflicts of interest in this work.
References
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. | ||
Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25(6):1105–1187. | ||
Kawai T, Ohishi M, Kamide K, et al. The impact of visit-to-visit variability in blood pressure on renal function. Hypertens Res. 2011;35(2):239–243. | ||
Lee HT, Lim Y-H, Kim BK, et al. The relationship between ambulatory arterial stiffness index and blood pressure variability in hypertensive patients. Korean Circ J. 2011;41(5):235–240. | ||
Masugata H, Senda S, Murao K, et al. Visit-to-visit variability in blood pressure over a 1-year period is a marker of left ventricular diastolic dysfunction in treated hypertensive patients. Hypertens Res. 2011;34(7):846–850. | ||
Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population findings from NHANES III, 1988 to 1994. Hypertension. 2011;57(2):160–166. | ||
Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375(9718):895–905. | ||
Suchy-Dicey AM, Wallace ER, Elkind MS, et al. Blood pressure variability and the risk of all-cause mortality, incident myocardial infarction, and incident stroke in the cardiovascular health study. Am J Hypertens. 2013;26(10):1210–1217. | ||
Conway J, Boon N, Davies C, Jones JV, Sleight P. Neural and humoral mechanisms involved in blood pressure variability. J Hypertens. 1984;2(2):203–208. | ||
Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A. Arterial baroreflexes and blood pressure and heart rate variabilities in humans. Hypertension. 1986;8(2):147–153. | ||
Okada H, Fukui M, Tanaka M, et al. Visit-to-visit variability in systolic blood pressure is correlated with diabetic nephropathy and atherosclerosis in patients with type 2 diabetes. Atherosclerosis. 2012;220(1):155–159. | ||
Sega R, Cesana G, Bombelli M, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. J Hypertens. 1998;16(11):1585–1592. | ||
Matsui Y, Ishikawa J, Eguchi K, Shibasaki S, Shimada K, Kario K. Maximum value of home blood pressure a novel indicator of target organ damage in hypertension. Hypertension. 2011;57(6):1087–1093. | ||
Ushigome E, Fukui M, Hamaguchi M, et al. The coefficient variation of home blood pressure is a novel factor associated with macroalbuminuria in type 2 diabetes mellitus. Hypertens Res. 2011;34(12):1271–1275. | ||
Kikuya M, Ohkubo T, Metoki H, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis the Ohasama study. Hypertension. 2008;52(6):1045–1050. | ||
Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010;375(9718):938–948. | ||
Rothwell P, Howard S, Dolan E, et al; ASCOT-BPLA and MRC Trial Investigators. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9(5):469–480. | ||
Fukui M, Ushigome E, Tanaka M, et al. Home blood pressure variability on one occasion is a novel factor associated with arterial stiffness in patients with type 2 diabetes. Hypertens Res. 2012;36(3):219–225. | ||
Schutte R, Thijs L, Liu Y-P, et al. Within-subject blood pressure level – not variability – predicts fatal and nonfatal outcomes in a general population. Hypertension. 2012;60(5):1138–1147. | ||
Masuda S, Tamura K, Wakui H, et al. Effects of angiotensin II type 1 receptor blocker on ambulatory blood pressure variability in hypertensive patients with overt diabetic nephropathy. Hypertens Res. 2009;32(11):950–955. | ||
Parati G, Dolan E, Ley L, Schumacher H. Impact of antihypertensive combination and monotreatments on blood pressure variability: assessment by old and new indices. Data from a large ambulatory blood pressure monitoring database. J Hypertens. 2014;32(6):1326–1333. | ||
Shigenaga A-I, Tamura K, Dejima T, et al. Effects of angiotensin II type 1 receptor blocker on blood pressure variability and cardiovascular remodeling in hypertensive patients on chronic peritoneal dialysis. Nephron Clin Pract. 2009;112(1):c31–c40. | ||
Park JB, Sung K-C, Kang SM, Cho EJ. Safety and efficacy of fimasartan in patients with arterial hypertension (Safe-KanArb Study). Am J Cardiovasc Drugs. 2013;13(1):47–56. | ||
Kim C, Kim MY, Kang DR, Kim JY, Park JB; K-MetS study investigators. The efficacy of fimasartan for cardiovascular events and metabolic syndrome (K-MetS Study): Rationale, design and participant characteristics. Pulse (Basel). 2014;1(3–4):177–185. | ||
Asmar R, Khabouth J, Topouchian J, El Feghali R, Mattar J. Validation of three automatic devices for self-measurement of blood pressure according to the International Protocol: The Omron M3 Intellisense (HEM-7051-E), the Omron M2 Compact (HEM 7102-E), and the Omron R3-I Plus (HEM 6022-E). Blood Pres Monit. 2010;15(1):49–54. | ||
Cicconetti P, Cacciafesta M, Migliori M, et al. Influence of sex and age on blood pressure variability. Arch Gerontol Geriatr. 2000;30(3):225–236. | ||
Parati G, Ochoa JE, Bilo G. Blood pressure variability, cardiovascular risk, and risk for renal disease progression. Curr Hypertens Rep. 2012;14(5):421–431. | ||
Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home-measured blood pressure and heart rate the Finn-Home Study. Hypertension. 2012;59(2):212–218. | ||
Ichihara A, Kaneshiro Y, Takemitsu T, Sakoda M. Effects of amlodipine and valsartan on vascular damage and ambulatory blood pressure in untreated hypertensive patients. J Hum Hypertens. 2006;20(10):787–794. | ||
Zhang Y, Agnoletti D, Safar ME, Blacher J. Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) Study. Hypertension. 2011;58(2):155–160. | ||
Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA. 2004;292(18):2217–2225. | ||
Yoshida H, Akasaka H, Saitoh S, Shimamoto K, Miura T. Comparative effects of telmisartan and valsartan as add-on agents for hypertensive patients with morning blood pressure insufficiently controlled by amlodipine monotherapy. Hypertens Res. 2013;37(3):225–231. | ||
Pringle E, Phillips C, Thijs L, et al. Systolic blood pressure variability as a risk factor for stroke and cardiovascular mortality in the elderly hypertensive population. J Hypertens. 2003;21(12):2251–2257. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.