Back to Journals » Journal of Inflammation Research » Volume 16
Fibrinogen is Associated with Clinical Adverse Events in Patients with Psoriasis and Coronary Artery Disease
Authors Zhao L, Zeng Y, Sun L, Zhang Z, Yang K, Li Z, Wang M, Zhou X, Yang W
Received 28 June 2023
Accepted for publication 19 August 2023
Published 12 September 2023 Volume 2023:16 Pages 4019—4030
DOI https://doi.org/10.2147/JIR.S427992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Lin Zhao,* Yan Zeng,* Lin Sun, ZengLei Zhang, KunQi Yang, ZuoZhi Li, Man Wang, XianLiang Zhou, WeiXian Yang
Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Disease, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yan Zeng; WeiXian Yang, Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Disease, Chinese Academy of Medical Sciences and Peking Union Medical College, No. 167, Beilishi Road, Beijing, 100037, People’s Republic of China, Email [email protected]; [email protected]
Purpose: The presence of elevated fibrinogen levels is associated with cardiovascular disease. However, whether fibrinogen level is associated with adverse clinical events in patients with psoriasis and coronary artery disease (CAD) is unknown. This study aimed to investigate the relationship between fibrinogen levels and cardiovascular adverse events in these patients.
Patients and Methods: This retrospective cohort study collected consecutive patients with psoriasis and CAD between January 2017 and May 2022 in our hospital. The clinical records were collected, and comparisons were made between groups. The Cox regression analysis and Kaplan–Meier survival analysis were used to evaluate the association between variables.
Results: Of the 267 participants, one hundred and forty-seven patients (55.1%) had elevated fibrinogen levels. Compared with patients in low fibrinogen group, white blood cell and platelet counts and high-sensitivity C-reactive protein levels were higher, whereas the left ventricular ejection fraction was lower in patients in high fibrinogen group. After a median follow-up of 35.5 months, the incidence of major adverse cardiovascular events (MACEs) was higher in patients in high fibrinogen group compared with patients in low fibrinogen group (31.4% vs 16.4%, p = 0.013). The Kaplan–Meier survival curves showed the same trend (log rank p = 0.020). Subgroup analysis revealed a positive association between elevated fibrinogen levels and MACEs in patients aged < 60 years (log-rank p = 0.013), those with diabetes (log-rank p = 0.027), and those who were not admitted for acute cardiovascular syndrome (log-rank p = 0.015).
Conclusion: Elevated fibrinogen levels were associated with adverse clinical events in patients with psoriasis and CAD, especially among patients aged < 60 years, those with diabetes, and those not admitted for acute cardiovascular syndrome.
Keywords: fibrinogen, coronary artery disease, major adverse cardiovascular events, psoriasis
Introduction
Fibrinogen plays an important role in blood viscosity.1 There has been a growing concern regarding the relationship between fibrinogen levels and coronary artery disease (CAD). Studies have reported that fibrinogen levels are associated with CAD and adverse cardiovascular events.2–6 Several mechanisms may contribute to pathophysiology of fibrinogen causing cardiovascular disease, including increased blood viscosity, contribution to inflammation and atherogenesis, thrombogenesis promotion, increased platelet aggregation, altered fibrin clot structure, and enhanced red blood cell attachment to thrombi.7–9 However, in patients who have suffered from CAD, the association between elevated fibrinogen levels and the prognosis remains controversial.6,10–12
Diseases such as psoriasis are associated with CAD progression. Psoriasis is a chronic inflammatory skin disease that affects multiple body systems, and evidence from clinical studies has indicated that patients with psoriasis have an increased risk of cardiovascular diseases.13,14 Compared with control groups, people with psoriasis have an approximately 6-year shorter life expectancy, and most psoriasis-related deaths are associated with cardiovascular or cerebrovascular morbidities.15 Whether increased fibrinogen levels cause differences in the adverse clinical outcomes of patients with psoriasis who already suffered from CAD remains unclear. Patients with psoriasis and CAD may benefit from a better understanding of the relationship between fibrinogen levels and prognosis. Therefore, the aim of this study was to investigate the associations between fibrinogen levels and clinical outcomes in patients with psoriasis and CAD.
Materials and Methods
Study Population
All consecutive patients with psoriasis who were diagnosed with CAD based on the results of coronary angiography at Fuwai Hospital between January 2017 and May 2022 were included. Patients younger than 18 years of age, patients with a history of malignancies, patients with a history of other rheumatic and connective tissue diseases, patients with severe liver disease or active infection were excluded from the study. The clinical records of the patients were collected. The treatments included medication therapy alone, percutaneous coronary intervention, and coronary artery bypass grafting, which were performed in accordance with the current guidelines and patient preferences.16,17 Outpatient records and telephone calls were used to obtain the follow-up results. All patients were followed up for a minimum of 6 months after discharge. The study was approved by the Institutional Ethics Committee of Fuwai Hospital and was conducted in accordance with the Declaration of Helsinki.
Biochemical Analysis and Coronary Angiography
Laboratory indicators were obtained from the patients at the time of admission, and all patients fasted for a minimum of 12 h before venous blood was collected. We conducted biochemical measurements at Fuwai Hospital’s Clinical Chemistry Department. Blood samples were collected in vacuum tubes containing sodium citrate prior to angiography. Fibrinogen levels were measured using a BCS analyzer (Multifibren U; Siemens Healthcare, Erlangen, Germany), according to a modification of the Clauss method. An automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan) was used to measure serum triglyceride, total cholesterol, and high- and low-density lipoprotein cholesterol levels. Immuturbidimetry (Beckman Assay 360, Bera, California, USA) was used to determine high-sensitivity C-reactive protein levels.
Coronary angiography was accomplished mainly via the radial artery. If the radial artery was unavailable, the brachial artery or femoral artery was considered. TIG catheters were a preferred use for transradial diagnostic coronary angiography. Judkins diagnostic catheters were used when the TIG catheters were not able to finish the coronary angiography. The relevant devices and certain percutaneous coronary intervention techniques including type, diameter, and length of stents; implantation technique; and use of adjunctive drugs or intravascular imaging devices were left to the operator’s discretion. The culprit vessel was determined primarily by coronary angiography. Coronary angiography images were assessed by two experienced cardiologists who were unaware of all other clinical data of the patients.
Definitions
Diabetes was diagnosed when patients met one of the following criteria:18,19 (1) the presence of typical symptoms of diabetes combined with random blood glucose levels ≥11.1 mmol/L; or (2) asymptomatic with a fasting plasma glucose level of equal to or above than 7.0 mmol/L, or a 2-h plasma glucose level of equal to or above than 11.1 mmol/L during 75 g oral glucose tolerance tests, or a glycosylated hemoglobin level of equal to or above than 6.5% confirmed by repeated tests; or (3) a previous diagnosis of diabetes and current treatment with hypoglycemic medication or diet. Hypertension was defined when patients met one of the following criteria:20 (1) a systolic blood pressure of ≥140 mmHg or a diastolic blood pressure ≥90 mmHg in the office following repeated examinations; or (2) a home systolic blood pressure of ≥135 mmHg or a home diastolic blood pressure ≥85 mmHg; or (3) a previous hypertension diagnosis with established antihypertensive medication or diet. The term “major adverse cardiac events (MACEs)” is used to describe a group of clinical events, including death from any cause, non-fatal myocardial infarction, revascularization unplanned, non-fatal stroke, and re-hospitalization due to heart failure or severe arrhythmias. ST-elevation myocardial infarction (STEMI) and unstable angina/non-STEMI were both considered as non-fatal myocardial infarction. Only emergencies requiring hospital admission were recorded in cases of unstable angina. The term “unplanned revascularization” refers to repeat percutaneous coronary interventions or surgical bypasses of any segment of the target vessel for ischemic symptoms.21 The stroke was diagnosed based on clinical records. Steroids and methotrexate are non-biological systemic treatments for psoriasis, whereas biologics include tumor necrosis factor alpha, interleukin 12/23, and interleukin 17. Based on the Chronic Kidney Disease Epidemiology Collaboration equation, the estimated glomerular filtration rate (eGFR) was calculated.22 The chronic kidney disease (CKD) was defined as an eGFR less than 60 mL/min/1.73 m2 for at least 3 months.23
Statistical Analysis
The continuous values were showed as the mean ± standard or median (25th, 75th percentiles). Comparing continuous variables between groups was done using Student’s t-test or rank-sum tests. The categorical values are showed as numbers (percentages). To detect differences between categorical values, Pearson’s chi-square or Fisher’s exact tests were used. We determined the cut-off value of fibrinogen levels in this study according to the methods in previous studies.24–26 The receiver operating characteristic results showed that the cutoff value of fibrinogen levels for predicting MACEs was 3.4 g/L. Thus, the patients in this study were divided into two groups according to this value, namely, the low- (< 3.4 g/L) and high-fibrinogen groups (≥ 3.4 g/L). The groups were compared using Kaplan–Meier survival curves and Log rank tests. Subgroup analyses of MACEs were performed based on the following factors: age (≤ 60 and > 60 years), gender, diabetes, hypertension, acute coronary syndromes (ACS), and left ventricular ejection fraction. The association between fibrinogen levels and MACEs was evaluated using Cox regression analysis. It was considered statistically significant when a two-tailed p-value of < 0.05 was obtained. All statistical analyses were conducted using SPSS 25.0 (IBM Corp., Armonk, NY, USA). GraphPad Prism 8.0 (GraphPad, San Diego, CA, USA) was used to generate Kaplan–Meier curves and forest plots. Since no previous studies have reported the effects of fibrinogen levels on the prognosis of patients with psoriasis and CAD, we included all patients who met the inclusion criteria in our hospital between January 2017 and May 2022. This study included 311 patients, of which 44 had missed fibrinogen data. Consequently, 267 patients were included in the study for analysis, of which 120 were in the low-fibrinogen group and 147 were in the high-fibrinogen group. A flowchart of the included patients is shown in Figure 1. The incidence of MACEs was 16.4% in the low fibrinogen group and 31.4% in the high fibrinogen group. We set α to 0.05 and calculated a power of 83.6% by using PASS (Power Analysis and Sample Size, version 15.0).
 |
Figure 1 Flow chart showing the selection of patients. |
Results
Characteristics of Patients in the Whole Group
Table 1 presents the baseline clinical characteristics of the patients. The study predominantly included men (87.6%). Among the patients, 56.9% had hypertension, 46.4% had diabetes, and 62.2% had ACS. Overall, 91.7% of the discharged patients were instructed to take aspirin, 81.5% to take P2Y12 inhibitors, 84.5% to take β-blockers, and 97.0% to take statins. According to the Psoriasis Area Severity Index score (median, 6.4), the cohort had mild-to-moderate skin diseases. The median psoriasis duration was 20 years. Regarding the treatment of psoriasis, 13.2% of the patients used phototherapy, 10.7% used biologic treatment and 39.7% used non-biological systemic treatment.
 |
Table 1 Clinical Characteristics Between the Two Groups |
Characteristics of the Patients in the Two Groups
Of the 267 participants, 147 (55.1%) were in the high-fibrinogen group and 120 (44.9%) were in the low-fibrinogen group. No significant differences existed in age (p = 0.859), gender (p = 0.494), or body mass index (p = 0.862). The proportions of patients with hypertension (p = 0.187), diabetes (p = 0.243), CKD (p = 0.345), and ACS (p = 0.878) did not differ between the two groups (Table 1). Moreover, no significant differences existed between the two groups based on the Psoriasis Area Severity Index scores (p = 0.110), disease duration (p = 0.322), or psoriasis-specific medication use. Patients in the high fibrinogen group had higher white blood cell counts (p < 0.001), platelet counts (p < 0.001), and high-sensitivity C-reactive protein levels (p < 0.001) than those in the low-fibrinogen group. The left ventricular ejection fraction was lower in the high-fibrinogen group than in the low-fibrinogen group [60 (55, 64) vs 63 (60, 65), p < 0.001] (Table 2).
 |
Table 2 Biochemical and Coronary Characteristics Between the Two Groups |
Clinical Outcomes
Overall, 256 patients were followed up for a median of 35.5 months, including 116 and 140 in the low- and high-fibrinogen groups, respectively. Finally, 63 patients (24.6%) experienced MACEs, including 19 (16.4%) and 44 (31.4%) in the low and high fibrinogen groups, respectively; there was a significant difference between the two groups (p = 0.013) (Table 2). According to the Cox regression analysis results, the high-fibrinogen group was associated with an increased risk of MACEs [hazard ratio (HR) 1.853, 95% confidence interval (95% CI) 1.089–3.152, p = 0.023]. Similarly, the Kaplan–Meier estimates showed the same trend (log-rank p = 0.020) (Figure 2).
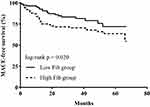 |
Figure 2 Kaplan–Meier survival curves estimated MACEs for patients between the two groups in the whole cohort. Abbreviations: MACEs, major adverse cardiovascular events; Fib, fibrinogen. |
The significant differences were found in the subgroup analysis (Figure 3). The positive association between the high-fibrinogen group and MACEs was found among patients aged < 60 years (HR 2.410, 95% CI 1.173–4.951, p = 0.017), those with diabetes (HR 2.284, 95% CI 1.072–4.867, p = 0.032), and those who were not admitted for ACS (HR 2.943, 95% CI: 1.174–7.379, p = 0.021) (Figure 3). The significant interaction was only observed between fibrinogen levels and diabetes (p = 0.002). According to the results of Kaplan–Meier survival curves, there were significant differences in MACEs between the two groups among patients aged <60 years (log-rank p = 0.013) (Figure 4B), those with diabetes (log-rank p = 0.027) (Figure 4E) and those who were not admitted for ACS (log-rank p = 0.015) (Figure 4J).
Discussion
In this study, the effect of serum fibrinogen levels on MACEs was examined in a large Chinese cardiovascular center using real-world patient data. Our findings showed that high fibrinogen levels were associated with MACEs in Chinese patients with psoriasis and CAD. Subgroup analysis showed that elevated fibrinogen levels were associated with MACEs among patients aged <60 years, those with diabetes, and those without ACS. These results are helpful for the risk stratification of patients with psoriasis and CAD.
Studies have evaluated the effects of fibrinogen levels on the prognosis of patients with CAD. Mahmud et al6 showed that among patients who received percutaneous coronary intervention, fibrinogen ≥2.8 g/L was associated with a 2.65-fold increase in the risk of major cardiovascular events within one year. Song et al27 suggested that in patients with non-ST-elevation ACS after percutaneous coronary intervention, fibrinogen level was an independent predictor of death or non-fatal reinfarction. Peng et al26 reported that among 3020 consecutive patients with coronary angiography-diagnosed CAD, elevated fibrinogen levels were significantly associated with mortality risk. The present study included patients with psoriasis and CAD and showed that elevated fibrinogen levels were associated with MACEs. Although these studies are different, the conclusions reached are very similar, indicating that fibrinogen is related to the poor prognosis of patients with CAD. However, in AtheroGene study,28 there was a positive relationship between fibrinogen levels and future cardiovascular risk, but fibrinogen levels did not provide further information on top of that obtained from models including traditional risk factors in patients with documented CAD and stable angina. Ndrepepa G also reported that the adjusted risk for all-cause and cardiac mortality was 7% and 5% for each 0.50 g/L increase in fibrinogen level in patients with angiography-proven CAD,10 but it did not provide additional prognostic information on top of that provided by traditional cardiovascular risk factors. Sjöland et al showed that in patients after coronary artery bypass grafting, there was no independent association between fibrinogen levels and long-term mortality.12 Chen et al11 included 170 patients hospitalized for suspected CAD, after an average follow-up of 10 years, they found that fibrinogen level did not have a significant predictive value for cardiac events. Different inclusion criteria, clinical endpoints and racial differences in the aforementioned studies may explain these inconsistent conclusions. The prognostic effect of fibrinogen levels in patients with CAD with specific characteristics requires further research.
Although the mechanisms through which fibrinogen increases the risk of cardiovascular events are not fully understood, the association between elevated fibrinogen levels and cardiovascular events observed in recent studies may be explained by multiple ways. One possible explanation is that systemic inflammation triggers fibrinogen production and release.29 Inflammation plays an important role in atheromatous plaque development.30 Additionally, by binding to ligand receptors, fibrinogen alters endothelial integrity and vascular wall permeability, attracts leukocytes to the vessel wall, and induces platelet accumulation and activation.31 Fibrinogen promotes smooth muscle cell proliferation and induces monocyte chemotaxis.32 Furthermore, hyperfibrinogenemia may lead to denser fibrin clots and impaired fibrinolysis, which may enhance atherosclerosis.8
The effects of fibrinogen on prognosis in patients with diabetes and CAD remains controversial. According to a prospective study from China, elevated fibrinogen levels were strongly associated with MACEs risk in patients with ACS complicated by diabetes; conversely, in patients without diabetes, fibrinogen level was not associated with MACEs.33 Another large-scale observational study showed that elevated fibrinogen levels increased MACEs risk in patients with stable CAD especially in the presence of diabetes and prediabetes.34 Yuan et al35 included patients with CAD who underwent percutaneous coronary intervention, after a median follow-up of 5.1 years, they found that patients with diabetes with medium or high fibrinogen levels had 2.57- and 3.04-fold higher risk of mortality, respectively, indicating that fibrinogen may be helpful for further risk stratification in patients with CAD and diabetes after percutaneous coronary intervention. The study from Yang et al36 included patients with angiographically proven CAD and diabetes, it showed that elevated baseline fibrinogen levels were associated with cardiovascular events in these patients. Although our study included patients with psoriasis and CAD, which differs from the above studies, we also found that elevated fibrinogen levels were associated with MACEs especially in patients with diabetes. These findings suggest that fibrinogen levels can be used for risk stratification of patients with diabetes and CAD. However, the ADVANCE study37 showed that fibrinogen was not an independent predictor of mortality after further adjustment. There are several possible explanations for this discrepancy. First, the inclusion criteria varied. Particularly, the ADVANCE study37 included patients with type 2 diabetes and a history of cardiovascular disease or one or more additional cardiovascular risk factors, whereas other studies included patients with diabetes and stable CAD36 or solely patients with ACS,33 and the present study included patients with psoriasis and CAD. Second, although the ADVANCE study included patients from many countries, Chinese and Indian patients were excluded.37 Fibrinogen levels vary according to ethnicity,38–40 hence, differences in ethnicities may have affected the results. Finally, the definitions of the clinical endpoints differed. The ADVANCE study37 used major macrovascular events, microvascular complications, and mortality as clinical endpoints, whereas Yang et al defined their clinical endpoints as cardiac death, stroke, non-fatal myocardial infarction, post-discharge revascularization owing to clinical deterioration or unstable angina.36 Moreover, Yuan35 defined the clinical endpoints as all-cause and cardiac mortalities.
Meanwhile, the role of diabetes in the prognosis of patients with other diseases needs attention. Studies have showed that elevated fibrinogen levels were associated with adverse clinical events in patients with CAD and diabetes. Besides, Güzel et al’s study41 found that diabetes was associated with mortality in patients with chronic total occlusion in the univariate cox analysis. What’s more, diabetes may affect coronary collateral development. In Guzel et al’s study,42 there were more patients in the poor collateral group had a history of diabetes (p < 0.001). In Aktan et al’s study,43 51 of 148 patients had diabetes, and diabetes prevalence was not determined to be statistically significant even though it was higher in the poor collateral group, which might be due to low diabetic case number. The prognostic impact of diabetes in patients with other diseases is an interesting topic that deserves further study.
There are also different conclusions regarding the effects of fibrinogen levels on the prognosis of patients with ACS. Bint et al44 showed that the fibrinogen levels in patients with ACS were higher than those in controls and a high fibrinogen level was associated with the risk of ACS. Shi et al45 reported that patients with ACS who developed clinical events had significantly higher fibrinogen levels than those who did not, and during short- and long-term follow-up, plasma fibrinogen levels could serve as an independent predictor of major adverse cardiac events. However, Choussat et al46 did not find that fibrinogen levels were predictive factors of coronary events during 1-year follow-up in patients with unstable angina or non-Q-wave myocardial infarction. In this study, we did not find a relationship between fibrinogen levels and prognosis in patients with ACS. However, fibrinogen levels were observed to be associated with a poor prognosis in patients without ACS. Notably, there are several differences between these studies. Binti et al44 included patients with ACS based on characteristic electrocardiograms and troponin I value, whereas Choussat et al46 included patients with unstable angina pectoris or non-Q-wave acute myocardial infarction. Our study included patients with psoriasis and CAD based on the results of coronary angiography. Shi et al45 defined endpoints as death or re-occlusion of an infarct-related artery at 30 days and 2 years, whereas Choussat et al46 defined endpoints as death, myocardial infarction, recurrent angina, or revascularization at the 1-year follow-up. There is still a need for further research in these patients in order to determine the prognostic value of fibrinogen levels.
According to the results of the subgroups in our study, we also found that there was an association between MACEs and high fibrinogen levels in patients aged <60 years. Hsieh et al47 evaluated the effects of fibrinogen levels on the risk of cardiovascular disease and all-cause death, they found that there is a greater risk of all cause death among patients aged <65 years who were with higher fibrinogen levels (test for trend p = 0.004). However, the patients in the study by Hsieh et al47 did not have CAD at baseline. Jiang et al48 assessed the relationship between fibrinogen levels and the prognosis of patients who underwent percutaneous coronary intervention, according to the results of subgroup analysis, fibrinogen was related to all-cause mortality among patients aged > 65 years, which is inconsistent with our results. The different clinical characteristics of patients included in above studies may partly explain the differences in these conclusions. Our findings indicate that young patients with psoriasis, CAD, and high fibrinogen levels are more likely to have subsequent malignant events. Further research is needed to confirm these novel findings.
In this study, the left ventricular ejection fraction was lower in the high-fibrinogen group than that in the low-fibrinogen group, which is similar to the previous study.34 This result may partly explain the poor prognosis in patients with high fibrinogen levels, as our previous study confirmed that patients with low left ventricular ejection fraction had an increased risk of MACEs49 in patients with psoriasis and CAD. According to above discussion about fibrinogen and inflammatory status, it is easy to understand that the levels of some inflammatory factors, such as white blood cells, platelet and hypersensitive C-reactive protein, were higher in the high-fibrinogen group than those in the low-fibrinogen group, which is also consistent with the previous studies.33,34,45 Considering the role of fibrinogen as an inflammatory biomarker, further studies are needed in order to determine whether lowering fibrinogen levels can improve long-term prognoses.
Recently, many studies have gradually discovered the effects of some clinical factors on prognosis of patients. Our findings showed that high fibrinogen levels were associated with clinical adverse events in Chinese patients with psoriasis and CAD. Guzel et al42 demonstrated that a high atherogenic plasma index is an independent factor associated with weak collateral formation. They are all simple, non-invasive, and economic, obtains a fast result and has an important value, should be carefully evaluated in determining individuals at risk for cardiovascular diseases.
Our study has some limitations. First, this was a single-center observational cohort study, which is less convincing than clinical trials. Second, because this study was based on a Chinese population, the results may differ from those from other races. Third, the study only included patients with psoriasis and CAD, suggesting that the results may not be generalizable to all patients with CAD. Forth, we only performed baseline measurements of fibrinogen levels, we could not assess their changes in these patients and whether these changes modified the observed clinical outcomes. Future prospective multicenter studies with high quality are expected to provide more evidence.
Conclusion
Elevated fibrinogen levels are related to MACEs in Chinese patients with psoriasis and CAD, especially in those aged <60 years, those with diabetes, and those without ACS. These findings provide valuable insight into the risk stratification of patients with psoriasis and CAD.
Abbreviations
ACS, acute coronary syndromes; CAD, coronary artery disease; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; MACEs, major adverse cardiovascular events; STEMI, ST-elevation myocardial infarction; HR, hazard ratio; 95% CI; 95% confidence interval.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding authors upon request.
Ethics Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Fuwai hospital (Approval No. 2021-1544). Written informed consent was obtained from all participants and data was anonymized before analysis.
Acknowledgments
We are very grateful to Dr. Jiayi Yi and Dr. Hanping Ma for their suggestions on the revision of the manuscript.
Funding
This work was supported by the Suzhou Industrial Park Xinxin Cardiovascular Health Foundation “Progress · Progress Fund 2020” funded project (2020-CCA-ACCESS-120), the National Natural Science Foundation of China (82192902), the Drug Research Fund for Cardiac Rehabilitation and Metabolic Therapy (T2016-ZX027), the CAMS Innovation Fund for Medical Sciences (CIFMS, 2022-I2M-C&T-A-010) and the National Key Research and Development Program of China (2016YFC1300100). The funding sources had no involvement in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the article for publication.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Herrick S, Blanc-Brude O, Gray A, Laurent G. Fibrinogen. Int J Biochem Cell Biol. 1999;31(7):741–746. doi:10.1016/S1357-2725(99)00032-1
2. Danesh J, Lewington S, Thompson SG, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005;294(14):1799–1809. doi:10.1001/jama.294.14.1799
3. Kaptoge S, Di Angelantonio E, Pennells L, et al. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310–1320.
4. Mora S, Rifai N, Buring JE, Ridker PM. Additive value of immunoassay-measured fibrinogen and high-sensitivity C-reactive protein levels for predicting incident cardiovascular events. Circulation. 2006;114(5):381–387. doi:10.1161/CIRCULATIONAHA.106.634089
5. Ang L, Thani KB, Ilapakurti M, Lee MS, Palakodeti V, Mahmud E. Elevated plasma fibrinogen rather than residual platelet reactivity after clopidogrel pre-treatment is associated with an increased ischemic risk during elective percutaneous coronary intervention. J Am Coll Cardiol. 2013;61(1):23–34. doi:10.1016/j.jacc.2012.09.037
6. Mahmud E, Behnamfar O, Lin F, Reeves R, Patel M, Ang L. Elevated serum fibrinogen is associated with 12-month major adverse cardiovascular events following percutaneous coronary intervention. J Am Coll Cardiol. 2016;67(21):2556–2557. doi:10.1016/j.jacc.2016.03.540
7. Kim PY, Stewart RJ, Lipson SM, Nesheim ME. The relative kinetics of clotting and lysis provide a biochemical rationale for the correlation between elevated fibrinogen and cardiovascular disease. J Thromb Haemost. 2007;5(6):1250–1256. doi:10.1111/j.1538-7836.2007.02426.x
8. Undas A. Fibrin clot properties and their modulation in thrombotic disorders. Thromb Haemost. 2014;112(1):32–42. doi:10.1160/TH14-01-0032
9. Luyendyk JP, Schoenecker JG, Flick MJ. The multifaceted role of fibrinogen in tissue injury and inflammation. Blood. 2019;133(6):511–520. doi:10.1182/blood-2018-07-818211
10. Ndrepepa G, Braun S, King L, et al. Relation of fibrinogen level with cardiovascular events in patients with coronary artery disease. Am J Cardiol. 2013;111(6):804–810. doi:10.1016/j.amjcard.2012.11.060
11. Chen WS, Chen SJ, Lee CC, Cherng WJ, Liu MH, Wang CH. Plasma P-selectin predicts long-term cardiovascular events in hospitalized patients with suspected coronary artery disease and preserved left ventricular function: a 10-year follow-up study. Biomed J. 2013;36(3):137–143. doi:10.4103/2319-4170.113231
12. Sjöland H, Tengborn L, Stensdotter L, Herlitz J. Lack of very strong association between pre-treatment fibrinogen and PAI-1 with long-term mortality after coronary bypass surgery. Cardiology. 2007;108(2):82–89. doi:10.1159/000095935
13. Miller IM, Ellervik C, Yazdanyar S, Jemec GB. Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors. J Am Acad Dermatol. 2013;69(6):1014–1024. doi:10.1016/j.jaad.2013.06.053
14. Mehta NN, Azfar RS, Shin DB, Neimann AL, Troxel AB, Gelfand JM. Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the General Practice Research Database. Eur Heart J. 2010;31(8):1000–1006. doi:10.1093/eurheartj/ehp567
15. Abuabara K, Azfar RS, Shin DB, Neimann AL, Troxel AB, Gelfand JM. Cause-specific mortality in patients with severe psoriasis: a population-based cohort study in the U.K. Br J Dermatol. 2010;163(3):586–592. doi:10.1111/j.1365-2133.2010.09941.x
16. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44–e122. doi:10.1016/j.jacc.2011.08.007
17. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(24):e123–e210. doi:10.1016/j.jacc.2011.08.009
18. Weng J, Ji L, Jia W, et al. Standards of care for type 2 diabetes in China. Diabetes Metab Res Rev. 2016;32(5):442–458. doi:10.1002/dmrr.2827
19. Elenkova A, Matrozova J, Vasilev V, Robeva R, Zacharieva S. Prevalence and progression of carbohydrate disorders in patients with pheochromocytoma/paraganglioma: retrospective single-center study. Ann Endocrinol. 2020;81(1):3–10. doi:10.1016/j.ando.2020.01.001
20. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi:10.1161/HYPERTENSIONAHA.120.15026
21. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–2351. doi:10.1161/CIRCULATIONAHA.106.685313
22. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
23. Xu N, Tang XF, Yao Y, et al. Association of Plasma Lipoprotein(a) with long-term adverse events in patients with chronic kidney disease who underwent percutaneous coronary intervention. Am J Cardiol. 2018;122(12):2043–2048. doi:10.1016/j.amjcard.2018.04.058
24. Meng Z, Zhao Y, He Y. Fibrinogen level predicts outcomes in critically ill patients with acute exacerbation of chronic heart failure. Dis Markers. 2021;2021:6639393. doi:10.1155/2021/6639393
25. Fricault P, Piot J, Estève C, et al. Preoperative fibrinogen level and postcardiac surgery morbidity and mortality rates. Ann Card Anaesth. 2022;25(4):485–489. doi:10.4103/aca.aca_103_21
26. Peng Y, Wang H, Li YM, et al. Relation between admission plasma fibrinogen levels and mortality in Chinese patients with coronary artery disease. Sci Rep. 2016;6:30506. doi:10.1038/srep30506
27. Song J, Yu T, Sun Z, Li Z, He D, Sun Z. Comparison of prognostic significance between serum fibrinogen and Global Registry of Acute Coronary Events score for prognosis of patients with non-ST-elevation acute coronary syndromes undergoing percutaneous coronary intervention. Coron Artery Dis. 2020;31(2):124–129. doi:10.1097/MCA.0000000000000789
28. Sinning JM, Bickel C, Messow CM, et al. Impact of C-reactive protein and fibrinogen on cardiovascular prognosis in patients with stable angina pectoris: the AtheroGene study. Eur Heart J. 2006;27(24):2962–2968. doi:10.1093/eurheartj/ehl362
29. Gabay C, Kushner I, Epstein FH. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448–454. doi:10.1056/NEJM199902113400607
30. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–1695. doi:10.1056/NEJMra043430
31. Pretorius E. Platelets as potent signaling entities in type 2 diabetes mellitus. Trends Endocrinol Metabol. 2019;30(8):532–545. doi:10.1016/j.tem.2019.05.003
32. Naito M, Stirk CM, Smith EB, Thompson WD. Smooth muscle cell outgrowth stimulated by fibrin degradation products. The potential role of fibrin fragment E in restenosis and atherogenesis. Thromb Res. 2000;98(2):165–174. doi:10.1016/S0049-3848(99)00202-9
33. Zhang L, Xu C, Liu J, et al. Baseline plasma fibrinogen is associated with haemoglobin A1c and 2-year major adverse cardiovascular events following percutaneous coronary intervention in patients with acute coronary syndrome: a single-centre, prospective cohort study. Cardiovasc Diabetol. 2019;18(1):52. doi:10.1186/s12933-019-0858-5
34. Liu SL, Wu NQ, Shi HW, et al. Fibrinogen is associated with glucose metabolism and cardiovascular outcomes in patients with coronary artery disease. Cardiovasc Diabetol. 2020;19(1):36. doi:10.1186/s12933-020-01012-9
35. Yuan D, Jiang P, Zhu P, et al. Prognostic value of fibrinogen in patients with coronary artery disease and prediabetes or diabetes following percutaneous coronary intervention: 5-year findings from a large cohort study. Cardiovasc Diabetol. 2021;20(1):143. doi:10.1186/s12933-021-01335-1
36. Yang SH, Du Y, Zhang Y, et al. Serum fibrinogen and cardiovascular events in Chinese patients with type 2 diabetes and stable coronary artery disease: a prospective observational study. BMJ Open. 2017;7(6):e015041. doi:10.1136/bmjopen-2016-015041
37. Lowe G, Woodward M, Hillis G, et al. Circulating inflammatory markers and the risk of vascular complications and mortality in people with type 2 diabetes and cardiovascular disease or risk factors: the ADVANCE study. Diabetes. 2014;63(3):1115–1123. doi:10.2337/db12-1625
38. Cook DG, Cappuccio FP, Atkinson RW, et al. Ethnic differences in fibrinogen levels: the role of environmental factors and the beta-fibrinogen gene. Am J Epidemiol. 2001;153(8):799–806. doi:10.1093/aje/153.8.799
39. Albert MA, Pare G, Morris A, et al. Candidate genetic variants in the fibrinogen, methylenetetrahydrofolate reductase, and intercellular adhesion molecule-1 genes and plasma levels of fibrinogen, homocysteine, and intercellular adhesion molecule-1 among various race/ethnic groups: data from the Women’s Genome Health Study. Am Heart J. 2009;157(4):777–783.e771. doi:10.1016/j.ahj.2008.12.012
40. Albert MA, Glynn RJ, Buring JE, Ridker PM. Relation between soluble intercellular adhesion molecule-1, homocysteine, and fibrinogen levels and race/ethnicity in women without cardiovascular disease. Am J Cardiol. 2007;99(9):1246–1251. doi:10.1016/j.amjcard.2006.12.041
41. Güzel T, Aktan A, Demir M, Özbek M, Aslan B. Relationship between contrast-induced nephropathy and long-term mortality after percutaneous coronary intervention in patients with chronic coronary total occlusion. Rev Assoc Med Bras. 2022;68(8):1078–1083. doi:10.1590/1806-9282.20220283
42. Guzel T, Bilik MZ, Arslan B, Kilic R, Aktan A. The effect of atherogenic plasma index on collateral development in patients with chronic coronary total occlusion. Exper Biomed Res. 2021;4(4):291–301. doi:10.30714/j-ebr.2021471924
43. Aktan A, Güzel T, Özbek M, et al. The relationship between coronary collateral circulation and visceral fat. J Cardiovasc Med. 2021;9(1):1–12.
44. Binti NN, Ferdausi N, Anik MEK, Islam LN, Cesaro A. Association of albumin, fibrinogen, and modified proteins with acute coronary syndrome. PLoS One. 2022;17(7):e0271882. doi:10.1371/journal.pone.0271882
45. Shi Y, Wu Y, Bian C, Zhang W, Yang J, Xu G. Predictive value of plasma fibrinogen levels in patients admitted for acute coronary syndrome. Tex Heart Inst J. 2010;37(2):178–183.
46. Choussat R, Montalescot G, Collet J, et al. Effect of prior exposure to Chlamydia pneumoniae, Helicobacter pylori, or cytomegalovirus on the degree of inflammation and one-year prognosis of patients with unstable angina pectoris or non-Q-wave acute myocardial infarction. Am J Cardiol. 2000;86(4):379–384. doi:10.1016/S0002-9149(00)00950-4
47. Hsieh CT, Chien KL, Hsu HC, et al. Associations between fibrinogen levels and the risk of cardiovascular disease and all-cause death: a cohort study from the Chin-Shan community in Taiwan. BMJ Open. 2022;12(4):e054638. doi:10.1136/bmjopen-2021-054638
48. Jiang P, Gao Z, Zhao W, et al. Relationship between fibrinogen levels and cardiovascular events in patients receiving percutaneous coronary intervention: a large single-center study. Chin Med J. 2019;132(8):914–921. doi:10.1097/CM9.0000000000000181
49. Zhao L, Sun L, Yang K, et al. Effects of metabolic syndrome on cardiovascular outcomes of psoriatic patients with coronary artery disease: a single center retrospective cohort study. Diabetes Metab Syndr Obes. 2023;16:1003–1012. doi:10.2147/DMSO.S402618
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


