Back to Journals » Infection and Drug Resistance » Volume 16
Fecal Carriage of Carbapenem Resistant Enterobacterales and Associated Factors Among Admitted Patients in Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Authors Mekonnen Y , Solomon S , Gebreyohanns A, Teklu DS , Ayenew Z , Mihret A, Bonger ZT
Received 7 June 2023
Accepted for publication 15 September 2023
Published 26 September 2023 Volume 2023:16 Pages 6345—6355
DOI https://doi.org/10.2147/IDR.S418066
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yonas Mekonnen,1,2 Semaria Solomon,1 Alganesh Gebreyohanns,1 Dejenie Shiferaw Teklu,2 Zeleke Ayenew,2 Amete Mihret,2 Zelalem Tazu Bonger3
1Department of Medical Microbiology, Immunology and Parasitology, Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Clinical Bacteriology and Mycology National Reference Laboratory, Ethiopian Public Health Institute, Addis Ababa, Ethiopia; 3Ohio State Global One Health, LLC, Addis Ababa, Ethiopia
Correspondence: Yonas Mekonnen, Clinical Bacteriology and Mycology National Reference Laboratory, Ethiopian Public Health Institute, PO. Box. 1242, Addis Ababa, Ethiopia, Tel +251 946346352, Email [email protected]
Purpose: The Enterobacterales family colonizes the human gut as normal flora in all age groups, with bacterial infections being the most common cause. Resistance is currently observed in all normal flora. The aim of this study was to determine the frequency of fecal carriage of carbapenem-resistant Enterobacterales (CRE), carbapenemase-producing Enterobacterales (CPE), and associated factors in the faeces of admitted patients.
Methods: A cross-sectional study was conducted in Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. A total of 384 rectal swabs were collected from various wards in admitted patients who have consented to participate. The specimens were inoculated on a MacConkey agar plate, and then they were incubated at 37 °C for 18 to 24 hours. Using the BD PhoenixTM M50 compact system identification and antimicrobial susceptibility testing were performed. Using the modified carbapenem inactivation method, it was determined whether the carbapenem-resistant bacterial isolate produced carbapenemase or not.
Results: Overall prevalence of carbapenem-resistant Enterobacterales carriage and carbapenemase producing Enterobacterales in admitted patients was 17.2% (95%, Confidence Interval: 13.3– 21.1%) and 7% (95%, Confidence Interval: 4.7– 9.9%), respectively. The predominate carbapenem-resistant Enterobacterales in fecal carriage was K. pneumoniae, 15.4% (23/149), E. cloacae 15.4% (6/39), followed by E. coli 12.4% (37/307) of carbapenem-resistant Enterobacterales (CRE) isolate. Carbapenem-resistant Enterobacterales carriage isolates showed large level of resistance to ciprofloxacin, and sulfamethoxazole-trimethoprim. Prior intake of antibiotics (Odds Ratio 2.42, 95% CI: 11.186– 4.95) was significantly associated with higher carbapenem-resistant Enterobacterales carriage.
Conclusion: We observed a high prevalence of carbapenem-resistant Enterobacterales carriage and carbapenemase-producing Enterobacterales among admitted patients. There were only amikacin and colistin that could be effective for carbapenem-resistant Enterobacterales isolates. Hence, the control of carbapenem-resistant Enterobacterales carriage should be given priority by carbapenem-resistant Enterobacterales screening for fecal of admitted patients, and adhering to good infection prevention practice in hospital settings.
Keywords: carbapenem, resistance, Enterobacterales, fecal, carriage, carbapenemase
Background
The family of Enterobacterales heavily colonizes the human gut as normal flora in all age groups of the individual, and bacterial infection is the most common cause.1 Multidrug resistance, now days, is observed in all normal commensal flora.2 The implemented strategies designed work to monitor antibiotic resistance mainly focus on examining pathogenic organisms.3 Carbapenem resistance Enterobacterales (CRE) is a bacteria that develops resistance to one or more antimicrobials belonging to carbapenem classes like imipenem, ertapenem, and meropenem using the current CLSI breakpoints.4 It was determined to be one of the multidrug-resistant Gram-negative bacteria (MDR-GNB), which have limited treatment options and high fatality rates when compared to susceptible strains.5 Know a day’s treatment by carbapenems is very common due to the introduction of MDR.6 β-lactams antibiotics like penicillin, cephalosporins, carbapenems, and aztreonam are routinely utilized to treat bacterial infection.7
Enterobacterales use two main mechanisms to develop resistance to carbapenems. Non-carbapenemase-producing carbapenem-resistant Enterobacterales (via alterations in membrane permeability, development of drug efflux pumps, or alterations in antimicrobial target site binding) and carbapenemase-producing carbapenem-resistant Enterobacterales (eg, KPC, VIM, and OXA).8
Carbapenem-resistant recently, it has been noted that Enterobacterales is widespread and that it is primarily responsible for the synthesis of carbapenemases. These enzymes can confer a high degree of resistance to most β-lactam antibiotics, such as cephalosporins and carbapenems.9
It is critical to identify patients who are asymptomatic carriers, since they could act as a source of transmission.10 Since the gastrointestinal system is the primary CRE reservoir, screening for CRE carriage, stool samples can be used.11 In a hospital setting without active surveillance tests, gastrointestinal carriage might not be detected.12 To the best of our knowledge, there is no study that specifically focuses on CRE-fc patients admitted to hospital settings in Ethiopia, and information on the prevalence of CRE-fc in the country is still lacking. However, there are very few reported data on CPE.13,14 Therefore, this study is designed to determine the prevalence of carbapenem-resistant Enterobacterales, determine the prevalence of carbapenemase-producing Enterobacterales, and associated factors among admitted patients.
Materials and Methods
Study Design, Period, and Setting
A cross-sectional study design was conducted from December to January 2022 at Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. In addition to teaching undergraduate and specialty programs, conducting research projects, and providing medical specialty services to referred patients, the institution employs more than 2800 staff members (clinical, academic, administrative, and support). Despite having more than 700 beds available for patients, the hospital sees 1200 emergency and outpatient patients every day on average. A Lottery method was conducted to select each ward and according to the number of beds, a proportional sample size from each ward was taken: Medical Wards (226 patients), Surgical Wards (135 patients), and Intensive Care Units (23 patients). After receiving verbal informed consent from all patients, a successive sampling technique was utilized to collect stool and rectal samples from patients who had been hospitalized. Structured, previously tested questionnaires were used to collect data on socio-demographics and related aspects. Through the assessment of medical records, information about past antibiotic usage (over the previous 12 months) was gathered. The Clinical Bacteriology and Mycology National Reference Laboratory of the Ethiopian Public Health Institute (EPHI) carried out the laboratory analysis. Since 2016, the laboratory has held accreditation from the national accreditation office of Ethiopia.
Variables
Prevalence of carbapenem-resistant Enterobacterales carriage, prevalence of carbapenemase-producing Enterobacterales carriage, and antibiotic susceptibility pattern of carbapenem-resistant Enterobacterales carriage were the dependent variables, while age, sex, prior intake of antibiotics, previous hospital admission, long hospital stays, hematologic malignancy, and indwelling devices were the study’s independent factors.
Inclusion and Exclusion Criteria
All admitted patients for greater than or equal to 48 hours were included in this study. However, patients who were seen in the outpatient department, those who were observed in the emergency room for less than 48 hours, and patients who were who are less than 18 years old, and patients undergone same-day treatment or surgery during the survey date were excluded from this study.
Bacterial Identification
The identification of bacteria was performed using the BD PhoenixTM M50 automated system, which utilizes a series of conventional, chromogenic, and fluorogenic biochemical tests for the identification of the organism at the species-level. The ID panels are modifications of the classical methods. These include tests for fermentation, oxidation, degradation, and hydrolysis of various substrates. The system utilizes chromogenic and fluorogenic substrates as well as single carbon source substrates in the identification of organisms. A maximum of 50 identification and antimicrobial susceptibility test can be performed in the BD phoenix M50 instrument at a time using BD phoenix combination panels. A sealed and self-inoculating molded polystyrene tray with 136 micro-wells containing dried reagents serves as the BD phoenix disposable. The combination panel includes an identification side with dried substrates for bacterial or yeast identification and AST side with varying concentration of antimicrobial agents. To cover different types of reactivity within the range of taxa, it uses growth-based and enzymatic substrates. Therefore, bacterial identification is based on microbial utilization and degradation of specific substrates detected by various color indicator systems. When the testing bacteria utilize the carbohydrate substrate, the pH drops because of acid formation which is indicated by the color indicator (phenol red), in addition upon enzymatic hydrolysis of either p-nitroanilide or p-nitrophenyl compounds the chromogenic substrate forms a yellow color. Additional tests are also used that can detect the ability of the organism to degrade, hydrolyze, reduce, or utilize a substrate. Lastly, results from each substrate were displayed as +, -, V, or X for each reaction, then the organism identification was reported with the probability percentage, compared from the Phoenix updated database version V6.81A.15
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was performed simultaneously with the BD PhoenixTMM50 automated system using NMIC/ID-431 combination panels based on the manufacturer’s instructions. The system uses a broth-based micro-dilution using a redox indicator solution for the detection of testing bacterial growth in the existence of an antimicrobial agent. The AST broth is cation-adjusted (Ca+++ and Mg+++) to optimize susceptibility. Each AST panel configuration contains several antimicrobial agents with a wide range of two-fold doubling dilution concentrations. Finally, the MIC value of each antibiotic is released and interpreted as susceptible, intermediate, or resistant based on the CLSI.4,15
NMIC/ID-431 panels are formalized in the BD PhoenixTM M50 automated system to determine the susceptibility of the clinically relevant aerobic gram-negative rod to the antimicrobial agents; in addition, it indicates resistance markers like carbapenemase. This panel is composed of all CLSI recommended antimicrobial agents for Enterobacterales such as amikacin, cefepime, ceftazidime, ceftolozane-tazobactam, ciprofloxacin, colistin, gentamicin, imipenem, levofloxacin, meropenem, and piperacillin-tazobactam.
Test for Carbapenemase Production
After AST tests, candidate (non-susceptible) isolates having ≥4 µg/mL MIC for imipenem and/or meropenem were selected for further carbapenemase production testing (Modified Carbapenem Inactivation Method: mCIM).4 A loop full of test CRE isolate was suspended, in two tubes containing 2 mL of tryptic soy broth. Meropenem (MEM: 10 μg, Abtek Biologicals Ltd, Liverpool, United Kingdom) disks were submerged in each tube, and the tubes were incubated at ambient temperatures for 4 hours ± 15 minutes. Then, the disks were removed from the tubes and placed on Mueller–Hinton agar plates upon which a carbapenem-susceptible reporter E. coli ATCC 25922 was freshly applied. Finally, the sample was incubated with Mueller–Hinton agar plates at 35 °C ±2 °C in ambient air for 18–24 hours. After incubation, a measure of inhibition zone with diameter of 6–15 mm or pinpoint colonies was determined as positive for carbapenemase enzyme production; and a zone of inhibition ≥19 mm was considered to be negative for carbapenemase enzyme production. The procedure was monitored using Quality Control (QC) strains; K. pneumoniae ATCC BAA-1706 was as a negative control and K. pneumoniae ATCC BAA-1705 was as the positive control.4
Quality Assurance
The questionnaire underwent pre-testing (5%) to ensure its quality in order to safeguard the integrity of the data. On-site and daily checks for completeness, accuracy, and clarity were made on the collected data. All culture media were made in accordance with the manufacturer’s instructions, and overnight incubation at 35–37°C was used to confirm the sterility. The following ATCC control was used to evaluate the performance of culture media: P. mirabilis 12453, E. coli 29212, E. faecalis 29212, S. aureus 25923, and S. flexneri, 12022.
According to the manufacturer’s specifications, the phoenix system was validated using standard strains of E. coli 25922, E. coli 35218, and K. pneumonia, 700603. The above QC strains were also used to check the new lot ID and AST panel, and the findings were compared to the listed predicted results for each QC organism on the package inserts to confirm acceptable performance of the system.
Data Analysis
Paper-based data was translated to electronic form using the well-designed Open Data Kit (ODK); data cleaning was done in Excel, and the data analysis was done using a Statistical Package for Social Science (SPSS) version 26. A simple frequency table was used to describe the study population in relation to social-demographic, clinical conditions, and other relevant variables. Logistic regression analysis was used to explore associated factors with the prevalence of CRE carriage, and multiple logistic regression analysis was also used for p-value <0.025. A P-value of <0.05 was considered for statistical significance.
Results
Socio-Demographic Characteristics
A total of 384 inpatients were enrolled in this study. Of this, 95 (24.7%) and 84 (21.9%) of patients were in the age group 28–30 and 18–27, respectively. Age had a mean of 41 years and a standard deviation of 15.8 years, respectively. The majority of the patients were female (59.6%). Most patients (70.6%) had a family size of five or less. The study participants' educational status showed that 101 (26.3%) patients are illiterate. The majority of the patients were came from outside of Addis Ababa (55.2%) (Table 1).
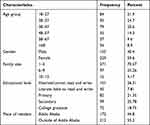 |
Table 1 Socio-Demographic Characteristics of Patients |
Clinical Conditions of Study Participants
The majority of patients (72.4%) had either exposure to previous antibiotic usage or had taken the antibiotic during the study period. About 53% of the study participants have a history of previous hospital visits, and 68% have long hospital stay history, which means that they have stayed in the hospital for a minimum of 3–7 days (Table 2).
 |
Table 2 Clinical Conditions of Study Participants |
Fecal Carriage of Carbapenem-Resistant Enterobacterales
The overall prevalence of CRE-fc was 17.2% (66/384; 95% CI: 13.3–21.1%) among hospitalized patients. Among several species, CRE-fc was distributed differently. K. pneumoniae had the highest intra-species frequency of CRE-fc at 15.4% (23/149), followed by E. cloacae at 15.4% (6/39) and E. coli at 12.4% (37/307). The CRE-fc proportion was higher among admitted patients in the age groups >68 years 26.5% (9/34). However, there was no difference in the number of CRE-fc between males 19.4% (30/155) and females 15.7% (36/229). Patients who have taken antibiotics have a higher rate of CRE-fc 20.6% (56/278) (Table 3).
 |
Table 3 Fecal Carriage of Carbapenem-Resistance Enterobacterales Carriage Among Admitted Patients |
Fecal Carriage of Carbapenemase-Producing Enterobacterales
Of 66 carbapenem-resistant Enterobacterales, CPE was confirmed in 42.4% (28/66) of isolates were CPE. The overall prevalence of CPE was 7.3% (28/384; 95% CI: 4.7–9.9%), which constitutes E. cloacae 66.7% (4/6), K. pneumoniae 52.2% (12/23) and E. coli, 32.4% (12/37). The detection of CPE varied among various types of species of Enterobacterales, and the largest intra-species frequency of carbapenemase production was observed among E. cloacae 66.7% (4/6) followed by K. pneumoniae 52.2% (12/23) and E. coli 32.4% (37). However, none of the other bacteria is producing carbapenemase (Table 4).
 |
Table 4 Fecal Carriage of Carbapenemase-Producing Enterobacterales Among Admitted Patients |
Factors Associated with Carbapenem-Resistant Enterobacterales Carriage
Using a pair-wise analysis and multivariable analysis, prior intake of antibiotics was associated with fecal carriage of carbapenem-resistant Enterobacteriaceae (CRE-fc). Patients with a prior intake of antibiotics were 2.4 times more likely to be CRE-fc than patients with no history of antibiotic intake (AOR = 2.406 (95% CI: 1.169–4.952)). However, there was no statistical-significant association found with the other variable (Table 5).
 |
Table 5 The Associated Factor for Fecal Carriage Carbapenem-Resistant Enterobacterales Among Admitted Patients |
Antimicrobial Susceptibility Profile
The highest resistance level of CRE-fc isolate was recorded for ciprofloxacin (95.5%) and sulfamethoxazole-trimethoprim (95.5%), followed by gentamycin (43.9%). However, lower resistance levels were observed against amikacin (3%).
Escherichia coli showed the highest resistance to ciprofloxacin (97.3%) and sulfamethoxazole-trimethoprim (97.3%) the same result was seen in K. pneumoniae which observed against ciprofloxacin (95.7%) followed by sulfamethoxazole-trimethoprim (91.3%). However, low resistance levels were detected in colistin (16.7%) and amikacin, which do not recordresistance level (Table 6).
 |
Table 6 Antimicrobial Resistance Pattern of Fecal Carriage Carbapenem-Resistant Enterobacterales |
Discussion
The gastrointestinal system is populated by a variety of typical flora, and it can translocate into a sterile region and serve as a reservoir for bacteria resistant to antibiotics.16 CRE has successfully spread worldwide over in recent decades, and the nature of the presence of carbapenemase enzymes on plasmids may promote the spread of certain bacterial species and contribute to the endemic nature of CRE in medical facilities.17 Additionally, inadequate sanitation and hygiene in the community may have facilitated the spread of CRE.18
In different studies around the world, CRE carriage rate in fecal specimen varies from country to country.19–21 As far as we are aware, there is no substantial information presented on the fecal carriage of CRE among admitted patients in Ethiopia, especially in hospital setting from hospital perspective. In the current study, the frequency of CRE-fc was 17.2% (66/384; 95% CI: 13.3–21.1%) which is higher than the report by previous researchers in Cape Town, South Africa (0.5%),22 Shanghai (8.6%),23 and New York City (5.4%).12 Irrational use of antibiotics, poor hygienic practices, and hospital settings may contribute to high CRE-fc reports. On the other hand hospitals could report low CRE carriage if they implemented a good infection prevention and control strategy. However, due to limited resources, infection control, screening, and contact isolation of patients carrying CRE are typically difficult in impoverished countries. The finding of this study was similar to studies in Khartoum (17.3%),24 India (18.1–21%),25,26, and Mexican Tertiary Care Hospital (16.6%).27
The prevalence of CRE in the current study is lower than the study by Solgi et al (37.9%),28 Kotb et al (47.9%).29 The high occurrence of the above studies may be due to the laboratory method they used, reporting multiple CRE isolates in the same patients and uncontrolled antibiotics may contribute. This report is also lower than the report in Port Harcourt Teaching Hospital, Nigeria (45.6%).30 In Nigeria, most drugs are available over the country without prescription by qualified medical personnel.31 Further self-medication is common in this country.32
The higher proportion of CRE isolates in this study was found among K. pneumoniae 15.4% (23/149) followed by E. cloacae 15.4% (6/39) and E. coli 12.4% (37/307), is in agreement with studies done in Zhejiang Province, China hospital,33 and Iran.28
Carbapenemase enzymes reportedly were identified in Enterobacterales for the last ten years, and it is showing an increment.33 Due to this, CPE is an emerging threat to healthcare, because of its resistance to many common antibiotics.34,35 In the present study, the prevalence of CPE was 7.3% (28/384; 95% CI: 4.7–9.9%), which is greater than the prevalence reported by other researchers in China (2.6%) and36 France (2.4%).20 The prolonged hospital stays in this study compared those contraries, which predispose the patients to higher antibiotic exposure, colonization by carbapenemase-producing bacteria, and the infectious environment of the hospital, which may be responsible for the high report rate.
In this study, CPE was predominately found among E. cloacae 66.7% (4/6) followed by K. pneumoniae 52.2% (12/23) and E. coli 32.4%, which is in close agreement with studies done in Zhejiang (E. aerogenes 51.8%, E. coli 32.1%); however, this result is not comparable with other studies which were shown in China (K. pneumonia 65.4%, E. coli 23.08%, and C. freundii 3.85%). This variation may be due to the difference in the environmental conditions, health practice, patient conditions, laboratory method, and level of personal hygiene.
Different studies reported different results related to the association of independent variables with CRE.25,37,38 In the present study, prior intake of antibiotics (P = 0.017) is associated with CRE carriage, which is comparable to a study conducted in New York City37 and Brazil.39 However, the study conducted in Chinese36 did not find a significant statistical association with CRE carriage. These variations may be due to the sample size difference, and regional disparity. This study’s findings showed that there was no relationship between age and CRE carriage, which is similar to a study in New York City21 and Mexico City.27 Our research revealed no association between gender and CRE carriers. The present study showed that previous chronic illness has no significant association with CRE carriage, which is in line with a study done in Spain40 and Turkey.41 Nevertheless, it is unlikely very few reports that indicate having a chronic illness is an associated factor with CRE carrier.27,42
This variation is due to the type of drug used for treating different diseases being different and the study population. Additional possible expiation for this variation may be due to the species of Enterobacterales and the resistance mechanism.43,44
High resistance was found in the current study to ciprofloxacin (95.5%), sulfamethoxazole-trimethoprim (95.5%), and gentamycin (43.9%). The results of this study were in line with the findings of studies conducted in Rawalpindi, Pakistan,9 and Xiangya, China.19 A unique resistant mechanism or a combination of more than one mechanism may be to blame for the high resistance of CRE carriers to antibiotics. To brief, few CRE develop resistance by non-carbapenemase carbapenem resistance mechanism, which is mediated by specific point mutations (development of drug efflux pumps via alterations in membrane permeability or alterations in antimicrobial target site binding) and due to the production of the enzymes (carbapenemase) or mediated both mechanisms.45,46
The resistance level of E. coli to ciprofloxacin (85.7%) and gentamycin (42.9%) in our study was concordant with a study done in Xiangya, China.19 However, it was greater than a study conducted in Pakistan on (sulfamethoxazole-trimethoprim 67.0%, ciprofloxacin 57.0%, tigecycline 0.0%, Colistin 0.0%, and meropenem 44.0%) but other antibiotics show a greater resistance when compared to our report on gentamycin (43.9%), and amikacin (3.0%).47 These findings may be explained by variances in the selection of antibiotics from various classes or by variations in the rational application of antibiotics in clinical settings.
In K. pneumoniae, the highest level of resistance was observed against ciprofloxacin (95.7%), sulfamethoxazole-trimethoprim (91.3%), and tigecycline (21.7%) but low resistance to gentamycin (16.9%), amikacin (4.3%), and colistin. The outcomes of this study were consistent with the findings of Xiangya.19 But ciprofloxacin (14.3%) shows a low resistance level when compared to our findings. The reason for this discrepancy could be due to the unnecessary prescription of this drug, different study settings, and variances in the characteristics of the various carbapenemase types and patient conditions.
In the present study, E. cloacae shows high resistance for sulfamethoxazole-trimethoprim (100%), gentamycin (100.0%), and ciprofloxacin (83.3%). Relatively lower resistance was shown in tigecycline (33.0%). This is concordant with a study done in Pakistan: sulfamethoxazole-trimethoprim (95.0%), gentamycin (76.0%), ciprofloxacin (90.0%) but in this study no resistance level of tigecycline was reported.47 The misuse, and overuse, of antibiotics and lack of infection control practices may contribute to the increasing CRE resistance to antibiotics.48 Relatively tigecycline and colistin were also found to be sensitive in this study and as it is reported by other studies.49,50 Due to the availability of this medication at neighborhood pharmacies, doctors may not be able to prescribe it, which may account for the low resistance to tigecycline and colistin. Tigecycline and colistin are currently not available in public hospitals in Ethiopia, which poses a great challenge for further patient management.
Conclusion
High prevalence was reported in this study of CRE (17.2%) and CPE (7.3%), carriage among admitted patients. There was also a high level of resistance to ciprofloxacin and sulfamethoxazole-trimethoprim. However, amikacin and colistin were effective against the majority of CRE isolates. This report also demonstrated that patients who have taken antibiotics before had a significant association with CRE-fc. This indicates that prior intake of antibiotics plays a major role in a high level of drug resistance and CRE carriage. However, this is a single study and they may need a variety of studies at the national level, especially in the association factor.
Abbreviations
AMR, Antimicrobial Resistance; AST Antimicrobial Susceptibility Testing; ATCC, American Type Culture Collection; CIM, Carbapenem Inactivation Method; CLSI, Clinical and Laboratory Standards Institute;CRE,Carbapenem-resistantEnterobacterales;CRF-fc,Carbapenem-resistant Enterobacterales Fecal Carriage; CRKP, Carbapenem-Resistant Klebsiella pneumoniae; DDST, Double Disk Synergy Test; ESBL, Extended Spectrum Beta-lactamase; ETT, Endotracheal Tube; IC, Index Cases; IMP, Imipenemase metallo-β-lactamase; KPC, K. pneumoniae carbapenemase; MAC, MacConkey Agar; mCIM, modified Carbapenem Inactivation Method; MDR, Multi-Drug Resistant; MDR-GNB, Multi-Drug Resistant Gram-Negative Bacteria; MHA, Mueller Hinton Agar; NDM, New Delhi metallo-β-lactamases; OXA-48, Oxacillinases-48; VIM, Verona integron-encoded metallo-β-lactamase; XDR, Extensively Drug-Resistant.
Data Sharing Statement
There are no more files in this manuscript, and it contains all of the necessary data. The primary data that we used to make this finding is available to the first author and it will be shared upon request.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Review Board of Saint Paul’s Hospital Millennium Medical College; the letter was obtained from the IRB of SPHMMC with reference no. (PM 23/275). Permission letters were obtained from the study site (EPHI bacteriology and mycology laboratory where the identification was performed). Individual informed consent or verbal informed consent was obtained when each participant was clarified about the study’s benefits. Individual informed consent or verbal informed consent was approved by IRB of SPHMMC. All results were kept strictly confidential. All verbal consent was witnessed and documented. The subject was given the full right to refuse or withdraw at any time from participating in the research. The study adhered strictly to the criteria mentioned in the Helsinki Declaration.
Acknowledgments
- Saint Paul’s Hospital Millennium Medical College.
- Ethiopian Public Health Institute.
- My heartfelt gratitude would also go to my colleagues Dr Zewdu Terefework, and Mr. Dawit Assefa.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas as; took part in drafting, revising, or critically reviewing the article. Gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This project was sponsored by Saint Paul’s Hospital Millennium Medical College and Ethiopian Public Health Institute.
Disclosure
There is no any conflict of interest for this work.
References
1. Grundmann H, Livermore D, Giske C, et al. Carbapenem-non-susceptible Enterobacterales in Europe: conclusions from a meeting of national experts. Eurosurveillance. 2010;15(46):19711. doi:10.2807/ese.15.46.19711-en
2. Andremont A. Commensal flora may play key role in spreading antibiotic resistance (vol 69, pg 605, 2003). Asm News. 2004;70(2):47.
3. Mittal G, Gaind R, Kumar D, et al. Risk factors for fecal carriage of carbapenemase producing Enterobacterales among intensive care unit patients from a tertiary care center in India. BMC Microbiol. 2016;16(1):1. doi:10.1186/s12866-016-0763-y
4. CLSI. Performance standards for antimicrobial susceptibility testing.
5. Zaidah AR, Mohammad NI, Suraiya S, et al. High burden of Carbapenem-resistant Enterobacterales (CRE) fecal carriage at a teaching hospital: cost-effectiveness of screening in low-resource setting. Antimicrob Resist Infect Control. 2017;6:1–6. doi:10.1186/s13756-017-0200-5
6. Lombardi G, Tanzarella ES, Cutuli SL, et al. Treatment of severe infections caused by ESBL or carbapenemases-producing Enterobacteriaceae. Med Intensiva. 2022;47:34–44. doi:10.1016/j.medine.2022.09.002
7. Guilhaumou R, Benaboud S, Bennis Y, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients guidelines from the French Society of Pharmacology and Therapeutics and the French Society of Anaesthesia and Intensive Care Medicine. Crit Care. 2019;23(1):1–20. doi:10.1186/s13054-019-2378-9
8. Bradley N, Lee Y. Practical implications of new antibiotic agents for the treatment of carbapenem-resistant Enterobacteriaceae. Microbiol Insights. 2019;12:1178636119840367. doi:10.1177/1178636119840367
9. Day KM, Ali S, Mirza IA, et al. Prevalence and molecular characterization of Enterobacterales producing NDM-1 carbapenemase at a military hospital in Pakistan and evaluation of two chromogenic media. J Antimicrob Chemother. 2013;75(2):187–191.
10. Tischendorf J, de Avila RA, Safdar N. Risk of infection following colonization with carbapenem-resistant Enterobactericeae: a systematic review. Am J Infect Control. 2016;44(5):539–543. doi:10.1016/j.ajic.2015.12.005
11. Rai S, Das D, Niranjan DK, Singh NP, Kaur IR. Carriage prevalence of carbapenem-resistant Enterobacteriaceae in stool samples: a surveillance study. Med J Aust. 2014;7(2):64. doi:10.4066/AMJ.2014.1926
12. Swaminathan M, Sharma S, Blash SP, et al. Prevalence and risk factors for acquisition of carbapenem-resistant Enterobacterales in the setting of endemicity. Am J Infect Control. 2013;34(8):809–817.
13. Worku M, Getie M, Moges F, Getaneh A. Extended-spectrum beta-lactamase and carbapenemase producing enterobacterales among patients with gastrointestinal complaints in North West Ethiopia. Interdiscip Perspect Infect Dis. 2019;2019:1.
14. Desta K, Woldeamanuel Y, Azazh A, et al. High gastrointestinal colonization rate with extended-spectrum β-lactamase-producing Enterobacteriaceae in hospitalized patients: emergence of carbapenemase-producing K. pneumoniae in Ethiopia. PLoS One. 2016;11(8):e0161685. doi:10.1371/journal.pone.0161685
15. BD Phoenix™ M50. BD Phoenix M50 automated microbiology system users manual 07 ed; 2020.
16. Calfee D, Jenkins SG. Use of active surveillance cultures to detect asymptomatic colonization with carbapenem-resistant Klebsiella pneumoniae in intensive care unit patients. Infect Control Hosp Epidemiol. 2008;29(10):966–968. doi:10.1086/590661
17. Control CfD, Prevention. Guidance for Control of Carbapenem-Resistant Enterobacterales (CRE). Atlanta: National Center for Emerging and Zoonotic Infectious Diseases, Division of Health Care Quality Promotion, CDC; 2012.
18. Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi:10.1016/S1473-3099(13)70318-9
19. Liu Q, Liu L, Li Y, Chen X, Yan Q, Liu WE. Fecal carriage and epidemiology of carbapenem-resistant Enterobacteriaceae among hospitalized patients in a University Hospital. Infect Drug Resist. 2019;Volume 12:3935–3942. doi:10.2147/IDR.S233795
20. Pantel A, Marchandin H, Prère MF, et al. Faecal carriage of carbapenemase-producing Gram-negative bacilli in hospital settings in southern France. Eur J Clin Microbiol. 2015;34:899–904. doi:10.1007/s10096-014-2298-1
21. Banach DB, Francois J, Blash S, et al. Active surveillance for carbapenem-resistant Enterobacterales using stool specimens submitted for testing for Clostridium difficile. Infect Prev Pract. 2014;35(1):82–84.
22. Ogunbosi BO, Moodley C, Naicker P, Nuttall J, Bamford C, Eley B. Colonisation with extended spectrum beta-lactamase-producing and carbapenem-resistant Enterobacterales in children admitted to a paediatric referral hospital in South Africa. PLoS One. 2020;15(11):e0241776. doi:10.1371/journal.pone.0241776
23. Xu Q, Pan F, Sun Y, et al. Fecal carriage and molecular epidemiology of carbapenem-resistant Enterobacteriaceae from inpatient children in a pediatric hospital of Shanghai. Infect Drug Resist. 2020;Volume 13:4405–4415. doi:10.2147/IDR.S275549
24. Dahab RA, Ibrahim AM, Altayb HN. Phenotypic and genotypic detection of carbapenemase enzymes producing gram-negative bacilli isolated from patients in Khartoum State. F1000Research. 2017;6:1656. doi:10.12688/f1000research.12432.1
25. Mohan B, Prasad A, Kaur H, Hallur V, Gautam N, Taneja N. Fecal carriage of carbapenem-resistant Enterobacteriaceae and risk factor analysis in hospitalised patients: a single centre study from India. Indian J Med Microbiol. 2017;35(4):555–562. doi:10.4103/ijmm.IJMM_17_144
26. Jaiswal SR, Gupta S, Kumar RS, et al. Gut colonization with carbapenem-resistant Enterobacteriaceae adversely impacts the outcome in patients with hematological malignancies: results of a prospective surveillance study. Mediterr J Hematol Infect Dis. 2018;10(1). doi:10.4084/MJHID.2018.025
27. Torres-Gonzalez P, Cervera-Hernandez ME, Niembro-Ortega MD, et al. Factors associated to prevalence and incidence of carbapenem-resistant Enterobacteriaceae fecal carriage: a cohort study in a Mexican tertiary care hospital. PLoS One. 2015;10(10):e0139883. doi:10.1371/journal.pone.0139883
28. Solgi H, Badmasti F, Aminzadeh Z, et al. Molecular characterization of intestinal carriage of carbapenem-resistant Enterobacteriaceae among inpatients at two Iranian university hospitals: first report of co-production of bla NDM-7 and bla OXA-48. Eur J Clin Microbiol & Infect Dis. 2017;36:2127–2135. doi:10.1007/s10096-017-3035-3
29. Kotb S, Lyman M, Ismail G, et al. Epidemiology of carbapenem-resistant Enterobacterales in Egyptian intensive care units using National Healthcare–associated infections surveillance data, 2011–2017. Antimicrob Resist Infect Control. 2020;9(1):1–9. doi:10.1186/s13756-019-0639-7
30. Akani N, Douglas S, Kamani N. Characterization of carbapenem resistant Enterobacterales from patients stool in tertiary hospitals, Port Harcourt, Rivers State, Nigeria; 2022.
31. Esimone CO, Nworu CS, Udeogaranya OP. Utilization of antimicrobial agents with and without prescription by out-patients in selected pharmacies in South-eastern Nigeria. Pharm World Sci. 2007;29:655–660. doi:10.1007/s11096-007-9124-0
32. Fakeye TO, Adisa R, Olatunji E. Self-medication among hospitalized patients in selected secondary health facilities in South Western Nigeria. Pharm Pract. 2010;8(4):233. doi:10.4321/S1886-36552010000400005
33. Shu LB, Lu Q, Sun RH, et al. Prevalence and phenotypic characterization of carbapenem-resistant Klebsiella pneumoniae strains recovered from sputum and fecal samples of ICU patients in Zhejiang Province, China. Infect Drug Resist. 2018;Volume 12:11–18. doi:10.2147/IDR.S175823
34. Cantón R, Akóva M, Carmeli Y, et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect. 2012;18(5):413–431. doi:10.1111/j.1469-0691.2012.03821.x
35. Hawkey PM. The growing burden of antimicrobial resistance. J Antimicrob Chemoth. 2008;62(suppl_1):1–9. doi:10.1093/jac/dkn241
36. Zhao ZC, Xu XH, Liu MB, Wu J, Lin J, Li B. Fecal carriage of carbapenem-resistant Enterobacteriaceae in a Chinese university hospital. Am J Infect Control. 2014;42(5):e61–4. doi:10.1016/j.ajic.2014.01.024
37. Bhargava A, Hayakawa K, Silverman E, et al. Risk factors for colonization due to carbapenem-resistant Enterobacteriaceae among patients: exposed to long-term acute care and acute care facilities. Infect Control Hosp Epidemiol. 2014;35(4):398–405. doi:10.1086/675614
38. Saxena S, Kumar S, Kumar V, Ravinder KA. Risk factors associated with colonization of intestine by carbapenem resistant Enterobacteriaceae in a pediatric ICU. Clin Microbiol Infect. 2020;10(02):75–81.
39. Salomão M, Guimarães T, Duailibi D, et al. Carbapenem-resistant Enterobacterales in patients admitted to the emergency department: prevalence, risk factors, and acquisition rate. J Hosp Infect. 2017;97(3):241–246. doi:10.1016/j.jhin.2017.08.012
40. Madueño A, García JG, Ramos MJ, et al. Risk factors associated with carbapenemase-producing Klebsiella pneumoniae fecal carriage: a case–control study in a Spanish tertiary care hospital. Am J Infect. 2017;45(1):77–79.
41. Kizilates F, Yakupogullari Y, Berk H, Oztoprak N, Otlu B. Risk factors for fecal carriage of extended-spectrum beta-lactamase-producing and carbapenem-resistant Escherichia coli and Klebsiella pneumoniae strains among patients at hospital admission. Am J Infect. 2021;49(3):333–339.
42. Schechner V, Kotlovsky T, Kazma M, et al. Asymptomatic rectal carriage of blaKPC producing carbapenem-resistant Enterobacteriaceae: who is prone to become clinically infected? Clin Microbiol Infect. 2013;19(5):451–456. doi:10.1111/j.1469-0691.2012.03888.x
43. Akova M, Daikos GL, Tzouvelekis L, Carmeli Y. Interventional strategies and current clinical experience with carbapenemase-producing Gram-negative bacteria. Clin Microbiol Infect. 2012;18(5):439–448. doi:10.1111/j.1469-0691.2012.03823.x
44. Saidel-Odes L, Borer A. Limiting and controlling carbapenem-resistant Klebsiella pneumoniae. Infect Drug Resist. 2013;7:9–14. doi:10.2147/IDR.S44358
45. Alizadeh N, Ahangarzadeh Rezaee M, Samadi Kafil H, et al. Evaluation of resistance mechanisms in carbapenem-resistant Enterobacteriaceae. Infect Drug Resist. 2020;Volume 13:1377–1385. doi:10.2147/IDR.S244357
46. Senchyna F, Gaur RL, Sandlund J, et al. Diversity of resistance mechanisms in carbapenem-resistant Enterobacterales at a health care system in Northern California, from 2013 to 2016. Diagnostic microbiology and infectious disease. Diagn Microbiol Infect Dis. 2019;93(3):250–257. doi:10.1016/j.diagmicrobio.2018.10.004
47. Perry JD, Naqvi SH, Mirza IA, et al. Prevalence of faecal carriage of Enterobacteriaceae with NDM-1 carbapenemase at military hospitals in Pakistan, and evaluation of two chromogenic media. J Antimicrob Chemother. 2011;66(10):2288–2294. doi:10.1093/jac/dkr299
48. Adler A, Katz DE, Marchaim D. The continuing plague of extended-spectrum β-lactamase–producing Enterobacteriaceae infections. Infect Dis Clin. 2016;30(2):347–375. doi:10.1016/j.idc.2016.02.003
49. Sader HS, Castanheira M, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Tigecycline activity tested against carbapenem-resistant Enterobacteriaceae from 18 European nations: results from the SENTRY surveillance program (2010–2013). Diagn Microbiol Infect Dis. 2015;83(2):183–186. doi:10.1016/j.diagmicrobio.2015.06.011
50. Poirel L, Nordmann P. Lack of polymyxin resistance among carbapenemase-producing Enterobacteriaceae in a university hospital in China. Infect Dis. 2017;49(7):556–557. doi:10.1080/23744235.2017.1292543
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
