Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Factors Related with Hospital Attendance and Mortality in Patients with COPD: A Case–Control Study in a Real-Life Setting
Authors López-Pardo ME , Candal-Pedreira C, Valdés-Cuadrado L , Represas-Represas C, Ruano-Ravina A , Pérez-Ríos M
Received 7 January 2022
Accepted for publication 28 March 2022
Published 14 April 2022 Volume 2022:17 Pages 809—819
DOI https://doi.org/10.2147/COPD.S355236
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
María Estrella López-Pardo,1 Cristina Candal-Pedreira,2 Luis Valdés-Cuadrado,3 Cristina Represas-Represas,4 Alberto Ruano-Ravina,2,5,6 Mónica Pérez-Ríos2,5,6
1Department of Planning and Health Reform, Galician Health Service, Santiago de Compostela, Spain; 2Department of Preventive Medicine and Public Health, School of Medicine, University of Santiago de Compostela, Santiago de Compostela, Spain; 3Department of Pulmonology, University Clinical Teaching Hospital of Santiago de Compostela, Santiago de Compostela, Spain; 4Respiratory Medicine, Alvaro Cunqueiro University Teaching Hospital, Vigo, Spain; 5Consortium for Biomedical Research in Epidemiology and Public Health (CIBER en Epidemiología y Salud Pública/CIBERESP), Madrid, Spain; 6Health Research Institute of Santiago de Compostela (Instituto de Investigación Sanitaria de Santiago de Compostela - IDIS), Santiago de Compostela, Spain
Correspondence: Alberto Ruano-Ravina, Departamento de Medicina Preventiva y Salud Pública, Facultad de Medicina, University of Santiago de Compostela, C/ San Francisco s/n, Santiago de Compostela, 15782, Spain, Tel +34-981-581237, Fax +34-981-572282, Email [email protected]
Introduction: The rising trend in hospital admissions among patients with chronic obstructive pulmonary disease (COPD) is worrying, not only because of the increasing costs, but also because of the worsening quality of life. We aimed to identify the predictive factors of hospital admission, re-admission and mortality of COPD patients through using information exclusively registered in electronic clinical records.
Methods: We conducted a population-based case–control study. All data were sourced from the different information systems comprising the Galician Health Service electronic record database. We included in the study patients diagnosed with COPD (code R95 in the medical record), ≥ 35 years old and with at least one spirometry performed ≤ 3 years prior inclusion. We fitted three logistic regression models, each one to ascertain the factors that influence the probability of admission, re-admission, and mortality, and calculated odds ratios (OR) with their 95% confidence intervals (95% CI).
Results: COPD patients were admitted due to respiratory causes a mean of 1.51 times across the period December 2016–December 2017, with 55% requiring re-admission in the next 90 days. The factor most closely associated with the re-admission profile was home oxygen therapy (OR 3.06 95% CI 2.42– 3.87), followed by male gender (OR 2.01 95% CI 1.48– 2.72), a CHA2D-VASc scale score > 2 (OR 1.28 95% CI 1.16– 1.42), and severity by clinical risk group stratification (OR 1.14 95% CI 1.04– 1.26). Male sex (OR 1.47 CI 95% 1.04– 2.09), having been readmitted ≥ 2 times (OR 1.34 CI 95% 1.11– 1.61) and being ≥ 70 years old (OR 1.05 CI 95% 1.03– 1.08) increase the probability of dying from COPD during the study period.
Conclusion: These results confirm the complexity of management of COPD exacerbations, and indicate the need to establish strategies that would ensure continuity of care after hospital admission, with the aim of preventing re-admissions and death.
Keywords: case–control study, COPD, hospital discharge, mortality
Introduction
Chronic obstructive pulmonary disease (COPD) has a relevant and growing impact on health and healthcare policies worldwide. It is currently ranked as the most prevalent chronic respiratory disease, in men and women alike, and is expected to increase in the coming years, due to population ageing among other causes.1,2 The main risk factor of COPD is smoking, followed by indoor and outdoor exposures to air pollutants and previous infections, among others.3 A recent study concluded that heavy smokers exposed to high radon concentrations had a higher risk of developing COPD.4
Apart from its high prevalence among the world’s population, COPD is a frequent cause of hospitalization in adults. This is mainly due to the fact that, over the course of the disease, patients with COPD tend to present with a worsening of respiratory symptoms, which sometimes requires hospital admission for their clinical stabilization. These exacerbations are linked, in turn, to a progressive deterioration of the patients’ pulmonary function and quality of life.5 The occurrence of exacerbations translates as frequent hospital attendance and, by extension, increased use of healthcare services.
In hospital emergency services, care of COPD patients accounts for 2% of all patients attended, with 40% of such patients needing hospital admission.6 It is estimated that COPD patients present with a mean of 1 to 4 exacerbations annually, and that one out of six episodes will culminate in hospital admission.7 Although there is wide geographical variability in COPD hospitalization rates, these have great influence, with an upward trend in recent years which has led to numbers doubling in certain regions.8
In addition to frequent hospital attendance, another matter of concern is that, according to a study conducted by Pozo-Rodríguez et al,9 37% of COPD patients who had received hospital discharge required re-admission in the next 90 days. Another study10 has reported that 10% to 20% of hospitalized patients were readmitted within the next 30 days, and that this small group of patients represents more than half of all COPD-related hospital care. Patients with a hospital readmission profile are mainly those who either are in or progressing toward a moderate-to-severe stage of the disease, and with each additional exacerbation, their risk of dying rises.11,12 As some studies have shown, early re-admission entails a higher risk of mortality and worse clinical results, and more than one third of the patients discharged following a COPD exacerbation are readmitted within the first three months post-discharge, with 7% dying.13–15
Frequent hospital attendance, including hospitalizations and re-admissions, have a considerable impact on the progress, prognosis, and mortality of COPD patients, as well as limiting their quality of life to a considerable degree.16 Furthermore, a greater demand for hospital care increases the cost related with COPD, which is already high per se.
In light of this, it is essential to develop health strategies and policies targeted at those groups of patients in which healthcare processes are less effective, with the aim of reducing both their frequent hospital attendance and mortality. To this end, we must be capable of identifying and characterizing these groups of patients, systematically and simply.
The aim of this study was thus to ascertain the profile of COPD patients who require hospitalization and/or hospital re-admission due to respiratory exacerbations, through the study of individual comorbidity and healthcare factors, by analyzing the universe of COPD patients in a health area with universal coverage and electronic health records (EHRs) since 2008. In addition, it sought to identify the predictive factors of mortality of COPD patients.
Methods
Study Design
We conducted a population-based case-control study, in which the study base comprised national health cardholders from the Santiago de Compostela health area (Galicia, Spain). This health area covers a population of 450,000 residing in 46 towns with a total land surface area of 4500 km2. The health network is made up of 75 health centers, 18 continuous care points (CCPs), a tertiary university teaching hospital complex, and a district hospital. A total of 18% of the population is aged over 70 years, and health coverage is practically universal (97%).
For study purposes, we designed a case-control study. The study population consisted of patients with a diagnosis of COPD prior to 2011. The period for analysis of events (used to define “case” or “control”) covered the 12 months from December 2016 through December 2017. We included all patients allocated to general practitioners in the health area and had an active clinical episode of COPD as of 21/12/2016, identified in their EHRs with International Classification of Primary Care (ICPC-2) code R95. By way of inclusion criteria, patients were required to have a minimum of one follow-up spirometry test in the preceding three years (both at hospital and in primary care), be over 35 years and have an active prescription of any of the medications associated with obstructive diseases included in the R03 therapeutic group of the Anatomical Therapeutic Chemical Classification (ATC).
We formed two groups of cases and one group of controls based on attendance at the Hospital Emergency Service (HES), general practitioners and CCPs. To establish these groups, the 75th percentile (P75) and the 90th percentile (P90) of care during the period were defined as cutpoints. The following groups were thus formed: a control group of “non-frequent attenders” (NF) with 0–10 demands, corresponding to <P75; a first group of cases “with moderately frequent attendance” (MF), with 11 to 19 demands, corresponding to the P75-90; and lastly, a second group of cases with “extremely frequent attendance” (EF), with 20 or more demands, corresponding to >P90. This study was approved by the Santiago-Lugo Research Ethics Committee under registry code 2016/196.
All data were sourced from electronic records without any type of intervention or possible modification of the clinical disease course in any case, since all data were collected retrospectively. Because of that, informed consent was not required in this study. The collection, processing, conservation, communication, and transfer of the data was done in accordance with the provisions of the General Data Protection Regulation (EU Regulation 2016–679 of the European Parliament and of the Council of 27 April 2016) and the Spanish regulations on personal data protection (Organic Law 3/2018 of 5 December on the Protection of Personal Data and guarantee of digital rights) and Law 14/2007 on biomedical research.
Data Sources and Data Collection
The data were obtained via EHRs and different health information systems, including: national health cards; Primary Care Information System (Sistema de Información de Atención Primaria); Minimum Basic Data Set (Conjunto Mínimo Básico de Datos); Hospital Outpatient Visit and Diagnostic Test Information System (Sistema de Información Hospitalaria de Consultas Externas y Pruebas Diagnósticas); clinical risk group (CRG) stratification; Out-of-Hospital Pharmacy; Vaccine Registry; and Home Oxygen Therapy Database. Information was also obtained from Complex Data-Analysis Systems (Sistemas Inteligentes de Análisis Complejos).
The following variables were collected from all participants: a) socio-demographic characteristics, including sex, age, town of residence, and health center of reference; b) active smoking habit; c) active episodes of comorbidity, anxiety, depression, dementia; d) CRGs: the CRG assigned to each patient with COPD was obtained in accordance with the clinical information available. Each individual was placed in a single group that was then regrouped into different health states (0 to 9) with levels of severity (1 to 6), by an automatic grouper in accordance with healthcare contact with primary care, hospitalization and pharmaceutical prescription registered in the EHR; e) CHA2DS2-VASc scale score which indicates the risk of suffering a stroke over the next twelve months. This scale is made up of the following variables: congestive heart failure or left ventricular systolic dysfunction, arterial hypertension, age, type-2 diabetes, previous vascular disease, and sex; f) influenza vaccination, ie, vaccinated/unvaccinated and date of vaccination; g) follow-up spirometry test and place of performance: date and place of performance of tests; h) healthcare requests: we obtained the number of requests for care received by the HES; i) hospitalization: all-cause admissions, respiratory-cause admissions and emergency re-admissions were recorded; g) home hospitalization stays; h) pharmacological treatment: medication related with obstructive diseases prescribed during the period analyzed; j) treatment with home oxygen therapy. In addition, we also recorded distance to the referral hospital, presence of a CCP in patients’ town of residence, and deaths.
Statistical Analysis
We first performed a descriptive statistical analysis of the variables of interest. Multinomial logistic regression models were then fitted to identify predictor variables of respiratory-cause admissions and hospital re-admissions. Whereas the fact of having undergone more than one respiratory-related hospitalization was used as the dependent variable in the first model, re-admissions were used as the dependent variable in the second model.
The predictor variables included in both models were depression (yes/no), anxiety (yes/no), dementia (yes/no), CRG (0–9), CHA2DS2-VASc scale score (0–8), follow-up spirometry test in primary care (yes/no), home oxygen therapy (yes/no), respiratory-cause admissions (continuous), distance to referral hospital (continuous), and presence of CCP in town of residence (yes/no). Lastly, sex (male/female), age (continuous) and smoking habit (yes/no) were used as variables of adjustment.
In the last model, deaths were used as the dependent variable. To identify the predictors of mortality a logistic regression was performed, including the following as predictor variables: age (continuous); sex (male/female); CRG (0–4, 5–9); CHA2DS2-VASc scale score (0–1, 2–8); home oxygen therapy (yes/no); respiratory-cause admissions (continuous); re-admissions (continuous); attendance (non-attendance, moderately frequent, extremely frequent). In all models, odd ratios (OR) were calculated along with their 95% confidence intervals (95% CIs).
To assess the model’s performance, its discrimination was analyzed using the area under the ROC curve, and its calibration using the Hosmer-Lemeshow test. We ascertained the optimal cutpoint corresponding to the probability of attendance and determined the point on the ROC curve closest to 1. All statistical analyses were performed using the IBM SPSS Statistics 19.0 computer software package.
Results
Of the 304,819 persons over age 35 years allocated to the health area, a total of 8,861 subjects were identified in their EHR as COPD patients over the course of 2016. A total of 4,587 patients were excluded, in the majority of cases because they had not undergone spirometry test in the previous three years, despite undergoing treatment with some medication in the R03 group (76.8%). Lastly, a total of 4,274 patients who fulfilled the inclusion criteria were included. While no significant differences were observed in terms of sex between those who were and those who were not included, age was higher in the excluded group (71 vs 78 years).
Table 1 describes the main characteristics of the participants: 71.8% were men; the median age was 71 years; 22.4% were smokers; depression was the most frequent comorbidity (8.9%), followed by anxiety (3.6%); 62.7% had been immunized with the influenza vaccine in the preceding year; and 61.1% presented with a medium risk of suffering from stroke over the next 12 months (CHA2DS2-VASc scale score of 2 to 4).
 |
Table 1 Main Characteristics of the Study Population |
Of the 4,274 subjects included, 2,637 (61.7%) were allocated to the NF group, 1,140 (26.7%) to the MF attendance group, and 497 (11.6%) to the EF attendance group. Table 2 shows attendance at hospital emergency facilities, as well as admissions for each of the study groups.
 |
Table 2 Hospital Attendance and Admissions in Cases and Controls |
The factors associated with a higher probability of hospital admission due to respiratory causes are shown in Table 3. Cases with respiratory-related admissions had a higher probability of being smokers (OR 1.47; 95% CI 1.15–1.87) and receiving oxygen therapy (OR 4.36; 95% CI 3.60–5.29). Presence of comorbidity and availability of healthcare resources (presence of a CCP in town of residence and distance of less than 16 km to hospital) did not prove to be significant factors.
 |
Table 3 Result of Logistic Regression (Respiratory Admissions and Re-Admissions) |
When it came to factors associated with hospital re-admissions, the results showed that male gender, age over 70 years, multimorbidity, CHA2D-VASc scale score higher than 3, use of home oxygen therapy, and absence of spirometric follow-up in primary care were all associated with a higher probability of re-admission. The factor most closely associated with the re-admission profile was home oxygen therapy (OR 3.06; 95% CI 2.42–3.87), followed by male gender (OR 2.01; 95% CI 1.48–2.72) (Table 3).
The factors related with higher mortality among COPD patients are shown in Table 4. Male gender, aged 70 years and over, respiratory admissions and re-admissions were factors associated with mortality. In addition, greater out-of-hospital attendance (CCPs and primary care) was also associated with higher mortality in these types of patients. The factor most strongly associated with mortality was having been readmitted twice or more (OR 1.34; 95% CI 1.11–1.61).
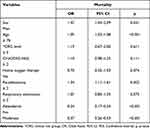 |
Table 4 Results of Logistic Regression. Factors Related with Mortality |
As can be seen in Figures 1–3, all predictive models displayed an acceptable degree of discrimination (0.7 ≤ AUC < 0.8).
 |
Figure 1 ROC curve. Admissions due to respiratory exacerbation. |
 |
Figure 2 ROC curve. All-cause readmissions. |
 |
Figure 3 ROC curve. Mortality. |
Discussion
The results of this study highlight the fact that certain individual and healthcare factors can predict hospitalization of COPD patients due to respiratory causes, as well as re-admissions and mortality. The different risk factors identified in the groups of patients hospitalized and subsequently readmitted due to respiratory exacerbations point to the existence of different profiles that require the application of specific healthcare strategies to this group of patients.
While COPD patients were admitted to hospital due to exacerbations a mean of 1.51 times, this figure rose to 2.56 times when admissions for any medical reason were taken into account. These figures highlight the important influence that comorbidities have on these patients’ hospital attendance. In this respect, the information provided by CHA2D-VASc score in this study is novel, in that it shows itself to be a powerful predictive factor of hospitalization. The ARTIC study17 found that comorbidities associated with a greater number of severe exacerbations in patients with COPD included heart failure, ischemic heart disease, and stroke. Moreover, previous diagnosis of mental health problems is similar to that reported in other previous studies, such as that by Lajas et al, which found that 8.6% of patients admitted due to an exacerbation presented with prior diagnosis of depression and 3.3% presented with prior diagnosis of anxiety.18 Social and health aspects may likely play a role in patients’ depression and anxiety. According to other studies,19 patients who live alone or have little family support experience more re-admissions due to COPD exacerbations. These aspects were not measured in this study since they are not included in patients’ EHRs, something that amounts to a limitation.
The results suggest that patients hospitalized due to respiratory causes have a higher probability of being men, aged 70 years and over, and a smoker. These findings are in line with those of other descriptive studies with population and hospital enrolment.20–22 This severe exacerbation profile, coupled with ageing, multimorbidity and severity, might account for the growing trend in acute hospitalization and increased risk of mortality in recent years.
A total of 55% of patients who at some time underwent hospitalization during the study period needed to be readmitted to hospital after the first medical discharge. This percentage is higher than that reported in previous studies,13,15,23 and may be due to the fact that, rather than focusing on a given department or hospital, our study instead focused on the overall health area setting. Attention should be drawn to the small percentage of re-admitted patients who received follow-up spirometry tests in primary care and influenza vaccination, which might indicate that patients who undergo repeated hospitalizations leave the ambit of primary care, thereby reducing the possibilities of implementing the socially and medically complex prevention and management measures that these patients need.
The results of this study show greater therapeutic intensity, particularly with respect to home oxygen therapy, among patients who required hospitalization due to respiratory causes. Likewise, home oxygen therapy was identified as the most powerful predictor of hospital re-admission in COPD patients, results that coincide with those of Lajas et al.15 Patients who need home oxygen therapy tend to present with a more advanced and, by extension, more severe disease profile, and in order to reduce re-admissions, it is thus essential that this group of patients receive healthcare and follow-up after hospital discharge.
It should be noted that, as also reported by another study,11 re-admissions and respiratory exacerbations were associated with a higher mortality rate. In our study, 14.3% of hospitalized and 15.8% of re-admitted patients died. These figures are higher than those estimated by Cerezo et al’s study.15 In addition, a novel finding was the association observed between frequent out-of-hospital attendance (primary care and CCPs) and mortality, with the figure rising to 16% in patients with extremely frequent attendance. These findings highlight the need for frequent COPD-related attendance, exacerbations and re-admissions to become an important intervention point in healthcare planning and clinical practice.
Given the profound clinical implications that hospitalizations and re-admissions have for the patient, owing to their high mortality and negative impact on quality of life, it is essential to develop evidence-based approaches, targeted at preventing and managing severe exacerbations. In this context, primary care plays a key role, though once the patient has been repeatedly hospitalized, it appears to become less important. The need of establishing circuits must be reinforced, to ensure that, once the patients are discharged, they receive self-care training and support as well as a structured follow-up, since interventions designed to empower patients and their families serve to prevent the appearance of exacerbations.24 Furthermore, the re-admission rate among COPD patients is very high, so that it is considered fundamental that, on being discharged from hospital, patients be followed up by means of visits to the pulmonology department, telephone calls, pulmonary rehabilitation, and a nursing and medical care continuity plan, underpinned and supported, where necessary, by information and communication technologies.25 Another aspect connected with the lack of follow-up is that almost half of the patients were not included for failing to have a spirometry test performed in the preceding 3 years, which is in direct contradiction with recommendations made in disease management guidelines.26 This is an even greater problem, bearing in mind that all health centers are equipped with spirometers.
This study has limitations, the main one being the exclusion of a substantial percentage of subjects for not having had a spirometry test performed in the preceding 3 years, despite being classified as COPD and receiving treatment for the disease. We chose to include only those subjects that had a confirmed diagnosis -something that can only be done when spirometry results are available- in order to avoid including subjects that might not have COPD. The approach to studying attendance from a statistical standpoint, by setting a cutpoint and taking, by way of reference, a given percentile above which attendance is deemed to be excessive, could also be seen as a limitation. While this methodology might classify clinically appropriate situations as frequent attendance, the cutpoints used are nonetheless similar to those applied in other studies on frequent attendance due to COPD.27,28 Another limitation of this study is the non-inclusion of other complications in addition to mental health problems, as we had no information available. It was also not possible to include information on whether patients had undergone respiratory rehabilitation.
This study’s main strength lies in the inclusion of the whole population of patients allocated to a given health area, since it ensures representativeness of the local population, and in addition serves to reduce patient selection bias. A further important strength of this study is that a uniform data-collection system was applied, which reduces information bias since there is no intervention by the researcher. Thanks to the data-collection method, data loss was zero, since the databases are regularly updated. Moreover, the follow-up period established was long enough to allow for the occurrence of events of interest. Another important advantage linked to the inclusion of all patients is that, in contrast with other studies, the hospital department concerned has no influence whatsoever on the inclusion or management of patients (as occurs in pulmonology vs internal medicine). Lastly, another highly relevant advantage is that our study shows that the joint use of health information systems by experts affords an enormous potential for the generation of useful scientific evidence for clinical decision-making.
The results of this study indicate the potential of EHRs in the approach to chronic diseases such as COPD, which makes it possible to advance in the design of population-based studies that provide a broad, comprehensive picture and enable results to be obtained more efficiently. To conclude, the time of hospital discharge should be considered a critical intervention point, bearing in mind the high re-admission and mortality rate. Furthermore, we feel that the role of primary care is crucial in terms of reducing hospital attendance through health education, professional counseling and healthcare continuity in these types of chronic patients, with special attention being paid to those patients who present with profiles of anxiety, depression or cardiovascular problems.
Abbreviations
ATC, Anatomical Therapeutic Chemical Classification; CCP, continuous care point; COPD, chronic obstructive pulmonary disease; CRG, clinical risk group; EHR, electronic health record; EF, extremely frequent attenders; MF, with moderately frequent attendance; NF, non-frequent attenders; ICPC, International Classification of Primary Care.
Ethics Approval
This study protocol was reviewed and approved by the Santiago-Lugo Research Ethics Committee under registry code 2016/196.
Data Sharing Statement
Data available on request from the authors (Alberto Ruano-Ravina, [email protected]).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors have no conflicts of interest for this work to declare.
References
1. Soriano JB, Kendrick PJ, Paulson KR, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 2020;8(6):585–596. doi:10.1016/S2213-2600(20)30105-3
2. Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1223–1249. doi:10.1016/S0140-6736(20)30752-2
3. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. doi:10.1016/S0140-6736(07)61380-4
4. Ruano-Ravina A, Cameselle-Lago C, Torres-Durán M, et al. Indoor radon exposure and COPD, synergic association? a multicentric, hospital-based case–control study in a radon-prone area. Arch Bronconeumol. 2021;57(10):630–636. doi:10.1016/J.ARBRES.2020.11.015
5. Miravitlles M. Drug treatment of acute infective exacerbations of COPD. Arch Bronconeumol. 2007;43(SUPPL.4):18–26. doi:10.1016/s0300-2896(07)74006-1
6. Soler JJ, Sánchez L, Latorre M, Alamar J, Román P, Perpiñá M. Impacto asistencial hospitalario de la EPOC. Peso específico del paciente con EPOC de alto consumo sanitario [The impact of COPD hospital resources: the specific burden of COPD patients with high rates of hospitalization]. Arch Bronconeumol. 2001;37(9):375–381. Spanish. doi:10.1016/S0300-2896(01)78818-7
7. Ancochea J. Estrategia en EPOC del SNS [Spanish National Health System COPD strategy]; 2010. Available from: http://www.msssi.gob.es/organizacion/sns/planCalidadSNS/pdf/ActualizacionEstrategiaCancer.pdf.
8. Librero J, Ibañez-Beroiz B, Peiró S, et al. Trends and area variations in potentially preventable admissions for COPD in Spain (2002-2013): a significant decline and convergence between areas. BMC Health Serv Res. 2016;16(1). doi:10.1186/s12913-016-1624-y
9. Pozo-Rodríguez F, López-Campos JL, Álvarez-martínez CJ, et al. Clinical audit of COPD patients requiring hospital admissions in Spain: AUDIPOC study. PLoS One. 2012;7(7):e42156. doi:10.1371/JOURNAL.PONE.0042156
10. Shah T, Churpek MM, Perraillon MC, Konetzka RT. Understanding why patients with COPD get readmitted: a large national study to delineate the medicare population for the readmissions penalty expansion. Chest. 2015;147(5):1219–1226. doi:10.1378/chest.14-2181
11. Guerrero M, Crisafulli E, Liapikou A, et al. Readmission for acute exacerbation within 30 days of discharge is associated with a subsequent progressive increase in mortality risk in COPD patients: a long-term observational study. PLoS One. 2016;11(3):e0150737. doi:10.1371/JOURNAL.PONE.0150737
12. Celli BR, Decramer M, Wedzicha JA, et al. An official American Thoracic Society/European Respiratory Society statement: research questions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;191(7):e4–e27. doi:10.1164/rccm.201501-0044ST
13. Escarrabill J, Torrente E, Esquinas C, et al. Auditoría clínica de los pacientes que ingresan en el hospital por agudización de EPOC. Estudio MAG-1 [Clinical audit of patients hospitalized due to COPD exacerbation. MAG-1 study]. Arch Bronconeumol. 2015;51(10):483–489. Spanish. doi:10.1016/J.ARBRES.2014.06.023
14. Harries TH, Thornton H, Crichton S, Schofield P, Gilkes A, White PT. Hospital readmissions for COPD: a retrospective longitudinal study. NPJ Prim Care Respir Med. 2017;27(1):31. doi:10.1038/S41533-017-0028-8
15. Cerezo Lajas A, Rodríguez Jimeno E, Gallo González V, Oliva Ramos A, Puente Maestu L, Miguel Díez de J. Mortalidad y factores asociados al reingreso en los pacientes dados de alta por una exacerbación aguda de EPOC [Mortality and associated factors with readmission in patients discharged by acute exacerbation of COPD]. Rev patol respir. 2018;21:79–85. Spanish.
16. Bafadhel M, Criner G, Dransfield MT, et al. Exacerbations of chronic obstructive pulmonary disease: time to rename. Lancet Respir Med. 2020;8(2):133–135. doi:10.1016/S2213-2600(19
17. Ställberg B, Janson C, Larsson K, et al. Real-world retrospective cohort study Arctic shows burden of comorbidities in Swedish COPD versus non-COPD patients. NPJ Prim Care Respir Med. 2018;28(1). doi:10.1038/s41533-018-0101-y
18. Lajas AC, Madrigal IB, Puente Maestu L, De J, Díez M. Ansiedad y depresión en pacientes ingresados por una exacerbación de EPOC [Anxiety and depression in patients admitted for COPD exacerbation]. Rev Patol Respir. 2020;23(4):134–140. Spanish.
19. Fernández-García S, Represas-Represas C, Ruano-Raviña A, Mosteiro-Añón M, Mouronte-Roibas C, Fernández-Villar A. Social profile of patients admitted for COPD exacerbations. A gender analysis. Arch Bronconeumol. 2020;56(2):84–89. doi:10.1016/J.ARBRES.2019.03.009
20. Almagro P, Cabrera FJ, Diez-Manglano J, et al. Comorbidome and short-term prognosis in hospitalised COPD patients: the ESMI study. Eur Respir J. 2015;46(3):850–853. doi:10.1183/09031936.00008015
21. Mascaró Cavaller O, Serra Batlles J, Roura Poch PLDG.Estudio EPOC. Clasificación fenotípica y comorbilidades de una población hospitalaria [COPD study: phenotypic classification and comorbidities in a hospital population]. Med Respir. 2017;10(2):49–57. Spanish.
22. Lajas AC, Puente Maestu L, De J, Díez M. Revista de patología respiratoria [Relevance of co-morbidities in COPD]. Rev Patol Respir.2019;22(3):81-83. Spanish
23. Vos T, Lim SS, Abbafati Cet al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20
24. Ferrone M, Masciantonio MG, Malus N, et al. The impact of integrated disease management in high-risk COPD patients in primary care. NPJ Prim Care Respir Med. 2019;29(1):1–9. doi:10.1038/s41533-019-0119-9
25. Braman SS. Hospital readmissions for COPD: we can meet the challenge. J Chronic Obstr Pulm Dis Found. 2015;2(1):4. doi:10.15326/JCOPDF.2.1.2015.0130
26. Guía Española de la Enfermedad Pulmonar Obstructiva Crónica (GesEPOC) - GuíaSalud [Spanish COPD guidelines (GesEPOC): Pharmacological treatment of stable COPD]. Available from: https://portal.guiasalud.es/gpc/epoc/.
27. Fuertes Goñi MC, Carracedo E, Lorda A, Arillo Crespo A, Gómez AR, Martinez Vera MJ. Intervención con pacientes hiperfrecuentadores persistentes en atención primaria [Intervention with persistent hyperfrequent visiting patients in primary care]. Med Gen. 2017;6(1):3. Spanish.
28. González-Peredo R, Prieto-Salceda MD, Campos-Caubet L, Fernández-Díaz F, García-Lago-Sierra Á, Incera-Alvear IM. Perfil del usuario de un servicio de urgencias hospitalarias [Characteristics of hospital emergency department users]. Hiperfrecuentación. Med Gener Fam Semergen. 2018;44(8):537–548. Spanish. doi:10.1016/j.semerg.2018.05.009
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
