Back to Journals » International Journal of General Medicine » Volume 16
Factors of Hospital Mortality in Men and Women with ST-Elevation Myocardial Infarction – An Observational, Retrospective, Single Centre Study
Authors Marinsek M , Šuran D , Sinkovic A
Received 8 September 2023
Accepted for publication 23 November 2023
Published 18 December 2023 Volume 2023:16 Pages 5955—5968
DOI https://doi.org/10.2147/IJGM.S439414
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Martin Marinsek,1,* David Šuran,2,* Andreja Sinkovic1,3,*
1Department of Medical Intensive Care, University Clinical Centre Maribor, Maribor, 2000, Slovenia; 2Department of Cardiology, University Clinical Centre Maribor, Maribor, 2000, Slovenia; 3Medical Faculty of University Maribor, Maribor, 2000, Slovenia
*These authors contributed equally to this work
Correspondence: Andreja Sinkovic, Department of medical intensive care, University clinical centre Maribor, Ljubljanska 5, Maribor, 2000, Slovenia, Tel +38641337822, Email [email protected]
Purpose: There are well-known gender differences in mortality of patients with ST-elevation myocardial infarction (STEMI). Our purpose was to assess factors of hospital mortality separately for men and women with STEMI, which are less well known.
Patients and Methods: In 2018– 2019, 485 men and 214 women with STEMI underwent treatment with primary percutaneous coronary intervention (PCI). We retrospectively compared baseline characteristics, treatments and hospital complications between men and women, as well as between nonsurviving and surviving men and women with STEMI.
Results: Primary PCI was performed in 94% of men and 91.1% of women with STEMI, respectively. The in-hospital mortality was significantly higher in women than in men (14% vs 8%, p=0.019). Hospital mortality in both genders was associated significantly to older age, heart failure, prior resuscitation, acute kidney injury, to less likely performed and less successful primary PCI and additionally in men to hospital infection and in women to bleeding. In men and women ≥ 65 years, mortality was similar (13.3% vs 17.8%, p = 0.293).
Conclusion: Factors of hospital mortality were similar in men and women with STEMI, except bleeding was more likely observed in nonsurviving women and infection in nonsurviving men.
Keywords: ST-elevation myocardial infarction, female sex, male sex, sex differences, hospital mortality, 30-day survival, 6-month survival
Introduction
The use of primary percutaneous coronary intervention (PCI) as the leading reperfusion strategy has significantly decreased the hospital mortality of ST-segment-elevation myocardial infarction (STEMI) patients to less than 10%, particularly in developed countries.1–3
During recent decades, several risk scores with many individual risk factors have been created to predict the outcome in STEMI patients. The most powerful scores, such as Global Registry of Acute Coronary Events (GRACE) and Thrombolysis in Myocardial Infarction (TIMI) scores, were recommended for years. However, the latest European Society of Cardiology (ESC) guidelines downgrade their prognostic importance.4,5 TIMI risk score was clinically useful in the triage and management of fibrinolysis-eligible patients with STEMI decades ago and included a spectrum of admission variables, such as comorbidities, older age, hypotension, tachycardia, Killip classes II–IV, body weight below 70 kg, anterior STEMI, and more than a 4-hour treatment delay.6 However, later studies demonstrated, in addition to timely use of primary PCI, other important predictors of prognosis such as prior resuscitation, TIMI III flow after primary PCI, in-hospital cardiogenic shock, bleeding, and acute kidney injury.7–9 In particular, TIMI flow < III after primary PCI, multivessel coronary artery disease in patients with cardiogenic shock, cardiogenic shock alone, renal failure and the need for mechanical ventilation, significantly predicted hospital mortality in STEMI patients.10,11
Men usually represent the majority of STEMI patients; up to 30% of the STEMI population comprises women.12–14 In STEMI patients, female gender is associated with an increased risk of mortality compared to men despite improvements in presentation and treatments within the last decade.12–15 Nevertheless, assessing the prognosis in STEMI population, either in men or women, is important, at least via the identification of the most significant factors of mortality for each gender.
However, specific factors of hospital mortality for men and women with STEMI are less well known. Therefore, our objective was to evaluate separately factors associated with hospital mortality in men and women with STEMI.
Materials and Methods
Patients
We retrospectively obtained and analysed the electronic records of all the patients, discharged in 2018 and 2019 from the Department of cardiology and/or the Department of medical intensive care with the main diagnosis according to International classification of diseases (ICD)-10 codes I21.0–I21.4 and I21.9 and the supervising physician carefully reviewed these data. We extracted patient data from the electronic hospital computer programme and finally included all the consecutive 699 patients, fulfilling the criteria of STEMI. The inclusion criteria were oppressive chest pain at rest and ST-segment elevation in 12-lead ECG, obtained and interpreted as soon as possible. ST-segment, measured at the J point, was elevated in at least two contiguous leads: ≥0.25 mV in men younger than 40 years, ≥0.2 mV in men older than 40 years, or ≥0.15 mV in women in leads V2-V3 and/or ≥0.1mV in other leads or new or presumably new left bundle branch block with the presence of concordant ST elevation (ie in leads with positive QRS deflections).5
We excluded patients with non-ST-elevation myocardial infarction (NSTEMI).
Methods
This was a retrospective monocenter observational study of STEMI patients admitted to the hospital between 2018 and 2019. The study was conducted at the University Clinical Centre Maribor, a tertiary clinical institution in the northeastern part of Slovenia, which is the 24/7 regional referral center for primary PCI in STEMI patients in an area with a population of 850.000. Approximately 800 coronary interventions are performed each year, of which up to 400 per year are performed in STEMI patients.
The Institutional Medical Ethics Committee (University Clinical Centre Maribor Medical Ethics Committee (KME)) approved this retrospective observational study (approval UKC-MB KME-16/20). The informed consent of the included patients was waived due to the retrospective nature of the study. The study was conducted in accordance with the 1964 Declaration of Helsinki and its subsequent amendments. We protected the personal data of the patients according to the Law on Personal Data Protection.
The treatment of STEMI patients between 2018 and 2019 was administered in accordance with ESC guidelines.5 Primary PCI was the main reperfusion strategy.
We registered the demographic, clinical and mortality data of STEMI patients. We gathered data on gender, age, body mass index (BMI), BMI ≥ 25 kg/m2, prior myocardial infarction, diabetes, arterial hypertension (AH), resuscitation before admission, and the time interval to primary PCI. We included measurements of cardiac troponin I and serum creatinine upon admission, as well as peak serum creatinine levels during in-hospital stay. We included the use of primary PCI, data on thrombus aspiration, the use of stents (all were drug eluting stents (DES)) and TIMI flows < III after primary PCI, and data on radial and femoral access. The proportions of TIMI flow < III, radial access, GP IIb/IIIa inhibitors, use of stents and thrombus aspirations and times to primary PCI were presented as the proportion of patients who were treated with PCI and not as the proportions of the total population. After primary PCI, we monitored patients in the coronary care unit or medical Intensive Care Unit (ICU) for approximately 24 hours or longer in case of complications until they reached a stable condition and could be transferred to the cardiology ward or local hospitals.5
During hospital stay, we registered acute complications such as acute in-hospital heart failure, arrhythmias, acute bleeding, acute kidney injury, in-stent thrombosis, hospital-acquired bacterial infection, and mortality. Acute heart failure (HF) was classified as either pulmonary congestion (Killip class II), pulmonary edema (Killip class III), or cardiogenic shock, or any hypotension necessitating a vasopressor infusion (Killip class IV).5,16 Any category of acute heart failure was marked as Killip classes II–IV. We registered arrhythmias as any ventricular and/or atrial. We registered acute kidney injury as an increase in serum creatinine of at least 50% from the baseline within the first 72 hours.17,18 We registered any bleeding as defined by the Bleeding Academic Research Consortium (BARC).19 Hospital infection was defined as the presence of microorganisms in the otherwise sterile milieu of the body (blood, cerebrospinal liquor, lung tissue, urinary tract, etc.) with or without clinical symptoms (fever, increased C-reactive protein (CRP), leukocytosis, or leukocytopenia) or as antibiotic administration due to the strong clinical suspicion of infection.20
We registered all standard pharmacological treatments (the use of acetylsalicylic acid (ASA) with clopidogrel, ticagrelor, or prasugrel; heparins; noradrenalin; dobutamine; levosimendan; loop diuretic; glycoprotein receptor antagonist IIb/IIIa); and treatments in complications (insertion of intra-aortic balloon pump (IABP) and mechanical ventilation). Left ventricular systolic function was assessed using transthoracic echocardiography during in-hospital stay.5
We compared baseline, treatment, hospital complication and hospital mortality data between men and women with STEMI, as well as baseline, treatment and in-hospital data between surviving and nonsurviving men and women with STEMI admitted to hospital from 2018 to 2019, with an emphasis on:
• Comparison of 30-day and six-month survival of men and women with STEMI;
• The evaluation of hospital mortality in men and women with STEMI older and younger than 65 years of age.
Statistical Analysis
Statistical analysis was performed using the SPSS Statistical package version 19 (IBM Corp., Armonk, N.Y., USA) for Windows. Continuous variables were reported as means and standard deviations (mean ± SD) and categorical data were presented as numbers and percentages. We used a two-sided Student’s t-test to compare the differences between the groups for means ± standard deviations and Fisher’s exact test to compare percentages. A p value <0.05 was considered statistically significant. Cumulative 30-day and 6-month survival was estimated using the Kaplan–Meier method and the difference between the groups (men vs women) was tested with a Log rank test.
Results
Baseline Characteristics
Table 1 shows the baseline characteristics of all included STEMI patients and comparisons between men and women. Men accounted for 69.4% of STEMI patients and women for 30.6%. The prevalences of age ≥65 years, AH and heart failure upon admissions were significantly higher in women than in men, BMI ≥ 25kg/m2 was significantly less likely observed in women. However, women with STEMI were less likely to be treated using primary PCI within the first three, six and twelve hours of chest pain than men, but the difference was nonsignificant.
 |
Table 1 Baseline Characteristics of All STEMI Patients |
Comparisons between surviving and nonsurviving men and women with STEMI are presented in Table 2. Older age, prior resuscitation and heart failure upon admission were significantly more prevalent in nonsurviving men and women than in survivors of both genders. In addition, admissions with TnI levels ≥5 µg/l were significantly more prevalent in nonsurviving than surviving men. In nonsurvivors of both genders, the use of primary PCI within the first three, six hours and twelve hours of chest pain in comparison to survivors was similar.
 |
Table 2 Baseline Characteristics of Surviving and Nonsurviving Men and Women with STEMI |
Treatments
Hospital treatments in all STEMI patients are presented in Table 3. Primary PCI, the leading reperfusion strategy, was used in 93.1% of all STEMI patients: 94% in men and 91.1% in women, respectively. Between men and women we did not observe any significant difference in the use of thrombus aspiration and the use of stents. In women with STEMI, there was a significant reduction in the use of radial access and the use of prasugrel, statins and Angiotensin-Converting Enzyme (ACE) inhibitors, as well as a significantly higher use of clopidogrel, noradrenalin, dobutamine, levosimendan and loop diuretics in comparison to men with STEMI.
 |
Table 3 Treatment of All STEMI Patients |
Treatment data of surviving and nonsurviving men and women with STEMI are presented in Table 4. We observed significantly lower use of primary PCI in nonsurviving men and women in comparison to survivors of both genders. We also observed significantly increased proportion of TIMI flow <III after primary PCI and less likely the use of ASA, ACE inhibitors, statins, beta receptor blockers, as well as significantly increased use of noradrenalin, dobutamin, and mechanical ventilation in nonsurviving men and women compared to survivors of both genders. In addition, there was a significantly higher use of loop diuretics and antibiotics but significantly lower use of radial access in nonsurviving men in comparison to survivors. We observed significantly less likely the use of stents during primary PCI in nonsurviving vs surviving women. There was nonsignificantly less likely used thrombus aspiration in nonsurviving women vs surviving ones.
 |
Table 4 Treatment of Surviving and Nonsurviving Men and Women with STEMI |
Target Coronary Arteries
Data regarding target coronary arteries in all STEMI patients are presented in Table 5. We did not observe any significant difference in the target coronary arteries between men and women with STEMI.
 |
Table 5 Target Coronary Arteries in All STEMI Patients |
Data regarding target coronary arteries in surviving and nonsurviving men and women are shown in Table 6. We observed that multivessel coronary artery disease was significantly more likely in nonsurviving men than in survivors, but in nonsurviving women, the left main coronary artery was significantly more likely the target coronary artery than in surviving women.
 |
Table 6 Target Coronary Arteries in Surviving and Nonsurviving Men and Women with STEMI |
Hospital Complications
Hospital complications in all STEMI patients are presented in Table 7. Hospital mortality in all STEMI patients was 9.9%: 8% in men and 14% in women, respectively (p = 0.019). In women with STEMI, we observed significantly increased prevalence of hospital heart failure, including pulmonary edema and cardiogenic shock, as well as acute kidney injury. Correspondingly, the use of noradrenalin, dobutamine, levosimendan, and diuretics was increased in women, as shown in Table 7.
 |
Table 7 Hospital Complications in All STEMI Patients |
Hospital complications in surviving and nonsurviving men and women with STEMI are presented in Table 8. In nonsurvivors of both genders, we observed significantly higher rate of hospital heart failure (Killip classes II–IV), in particularly pulmonary edema and cardiogenic shock, and acute kidney injury. Infection was significantly more prevalent in nonsurviving men and bleeding in women, respectively, in comparison to survivors. Correspondingly, the use of noradrenalin, Dobutamine, and mechanical ventilation was increased in nonsurvivors of both gender as shown in Table 4.
 |
Table 8 Hospital Complications in Surviving and Nonsurviving Men and Women with STEMI |
Hospital Mortality Data According to Age
Hospital mortality data of all STEMI patients, men and women with STEMI are presented in Figure 1. Hospital mortality was 8% in men and 14% in women, respectively (p = 0.019). Hospital mortality of STEMI patients ≥65 years was 15.1%: 13.3% in men and 17.8% in women, respectively (p = 0.293). Hospital mortality of STEMI patients <65 years was 4.4%: 4% in men and 5.9% in women, respectively (p = 0.293).
 |
Figure 1 Hospital mortality of men and women with STEMI according to age. |
Survival Difference Between Men and Women with STEMI
We present survival within 30 days of men and women with STEMI in Figure 2. Survival of men was 92.1% and of women 86.4% (log-rank p = 0.015).
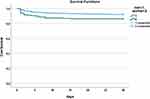 |
Figure 2 Survival difference between men and women with STEMI within 30 days. |
We present survival within 6 months of men and women in Figure 3. Survival of men was 89.8% and of women 82.2% (log-rank p = 0.004).
 |
Figure 3 Survival difference between men and women with STEMI within 6 months. |
Discussion
In our retrospective analysis, we observed that 30.6% of STEMI patients were women and 69.4% were men. In both genders, hospital mortality was significantly associated with several clinical variables, including age over 65 years, prior resuscitation, heart failure, acute kidney injury, primary PCI less likely to be performed, followed TIMI flow < III, less likely used ASA, statins, beta receptor blockers and ACE inhibitors. In nonsurvivors of both genders noradrenalin, dobutamin, mechanical ventilation were more likely to be utilized due to heart failure such as pulmonary edema and cardiogenic shock. Additionally, mortality in men was significantly associated with increased admission troponin I levels, more likely used loop diuretics, hospital infection and multivessel coronary artery disease and in women to bleeding and left main coronary artery disease. When we compared hospital mortality between older (age ≥ 65 years) and between younger (age < 65 years) men and women, the differences were nonsignificant. In addition, men with STEMI within 30 days and within 6 months survived significantly better than women.
In majority of studies, women with STEMI were significantly older than their male counterparts.13–15,21 In our study, women with STEMI were, on average, 8 years older than men. Nonsurviving men were significantly older than survivors - 7.5 years on average. However, nonsurviving men were, on average, 7 years younger than nonsurviving women. Age ≥65 years was significantly associated with hospital mortality in men and women with STEMI. Older age is also associated with increased prevalence of comorbidities such as diabetes, AH, chronic heart failure, prior myocardial infarcts.13,21 Older age is in general a powerful predictor of mortality in STEMI patients. Therefore, in our patients after adjustment for age, mortality in men and women with STEMI was similar.
Comorbidities, in particular AH and diabetes, are important risk factors for coronary artery disease and frequent findings in women with STEMI.13,21,22 We observed significant increase in the prevalence of AH in approximately 65% of women. However, AH was not associated with hospital mortality in our STEMI patients.
In some studies, hospital mortality in STEMI patients is associated with older age irrespective of gender.8,15 In studies, higher risk of mortality in older STEMI patients is associated with several factors such as delayed primary PCI, comorbidities, high-risk features during in-hospital stay (heart failure, prior resuscitation, bleeding, infection).23 Emerging data show that sex-specific pathophysiological differences, and not only sex disparities in quality and timing of care, may contribute to the higher mortality of females with STEMI, mainly at younger ages.24,25
The timely use of primary PCI with novel antithrombotic therapy has significantly decreased hospital mortality in STEMI patients over the last decade to <10%.26 In our STEMI patients, the use of primary PCI was over 90% in both genders, and the hospital mortality of all STEMI patients was 9.8%: 8% in men and 14% in women, respectively.
The reopening of the occluded epicardial coronary artery via the timely use of primary PCI is accepted as the most effective treatment for STEMI patients, reducing myocardial infarct size, preserving left ventricular function, and lowering mortality.26 In our STEMI patients, we observed a similar use of primary PCI in both genders within the first 3, 6 and 12 hours of chest pain. The use of primary PCI within the first few hours of chest pain in nonsurvivors of both genders was reduced but these differences were not significant.
TIMI III flow after primary PCI reflects the success of PCI treatment. The absence of final TIMI III flow causes worse short-term clinical outcomes as demonstrated by trials.10,27 TIMI flow < III was nonsignificantly more prevalent in women compared to men and significantly more prevalent in nonsurvivors of both genders in comparison to survivors. TIMI flow < III after primary PCI was associated with mortality in both genders. In previous studies, TIMI flow < III after primary PCI was independently predicted via factors such as high thrombus burden, older age, lower systolic blood pressure, and pre-procedural TIMI flow I. In addition, cumulative Major Adverse Cardiac Events (MACE) and mortality increased with TIMI flow < III.10,27 When comparing TIMI III flows in the subgroups of our STEMI patients, we observed TIMI flow < III after primary PCI in approximately 40% in nonsurviving women in comparison to approximately 20% in nonsurviving men. Therefore, the successful reperfusion of jeopardized myocardium was much more effective in men than in women according to TIMI III flows. Prior studies demonstrated that longer delays until primary PCI were responsible for less successful reperfusion in women with STEMI.13 However, in our STEMI population, the delay until primary PCI in both genders was similar.
According to previous studies, high thrombotic burden is not only among the independent predictors of TIMI flow < III, but there is also evidence that STEMI patients of both sexes with high thrombotic burden have an increased risk of cardiovascular events.27 In particular, women with high thrombotic burden are at an excessive risk of mortality and in-stent thrombosis.28 Thrombus aspiration at the time of primary PCI may reflect higher thrombotic burden in STEMI patients and the procedure was more frequently used in our women with STEMI.
Previous studies demonstrated that in STEMI patients with cardiogenic shock and/or prior resuscitation in the prehospital settings, mortality remains over 10% in spite of early symptomatic treatment and early primary PCI.26,29,30 In nonsurvivors of both genders, we observed an increased prevalence of prior resuscitation, mainly in out-of-hospital settings, as well as in hospital cardiogenic shock, requiring vasopressors, inotropes and mechanical ventilation despite the similar time delay until primary PCI as in survivors. The MUST study observed the inherent tendency of a poorer prognosis among women with STEMI, who developed sudden cardiac arrest in spite of similar management, causes, and settings of occurrence as in men.30 We observed significantly more likely prior resuscitation (in approximately 40%) in nonsurviving men and women with STEMI. This complication in STEMI patients, in particular in the out-of-hospital settings, contributed to cardiogenic shock and subsequent hospital mortality.
In-hospital acute cardiogenic shock or pulmonary edema are mostly observed in extensive acute STEMI and/or with mechanical complications. Early successful revascularization may reverse pump failure and hemodynamic compromise. The risk of hospital heart failure is increased, particularly in women with STEMI.31
The prevalence of infection in STEMI patients was approximately 20% and was significantly associated to mortality of men. High prevalence of infection in dying men was mostly associated with severe pulmonary congestion with respiratory failure in pulmonary edema an/or prior resuscitation with the use of invasive procedures such as intubation and mechanical ventilation and/or infection at the vessel puncture site, which are important predisposing factors for hospital infection and even sepsis. In dying men with STEMI, mechanical ventilation was used in even 63.7%.
The combined use of antiplatelets and anticoagulants effectively prevented in-stent thrombosis and reinfarction in our STEMI patients, particularly in women.5 However, bleeding was more frequently experienced by women, particularly in nonsurvivors. Majority of studies demonstrate that bleeding is associated with a significant increase in mortality in STEMI patients with combined antithrombotic drugs, particularly in women with low BMI, older age, and hepatic or renal dysfunction.32,33 Bleeding in women is also associated with smaller vessel size, higher risk of overdosing drugs and possible different pharmacological response to antithrombotics in comparison to men, as well as possible predisposing genetic factors for bleeding.19,21 Another important observation is that bleeding risk often overlaps with ischemic risk. Severe bleeding can induce hemodynamic compromise, hypoxemia due to anaemia, necessitating temporary interruption of antithrombotics, which can exacerbate reinfarction.21,34–36
To prevent bleeding in STEMI patients, in particular in women, attention should be focused to appropriate dosing and selection of antithrombotic drugs with the lowest bleeding rates. Unfractionated heparin use, DAPT for the shortest possible duration, prevention of gastrointestinal bleeding by pantoprazole, radial access for primary PCI used together with vascular closure devices should be implemented in special recommendations for treatment of women with STEMI.19,21,37,38
Acute kidney injury is another significant in-hospital complication. The use of nephrotoxic substances and reduction in glomerular perfusion due to cardiac pump failure in STEMI are among the most important factors of acute kidney injury, some of which can be prevented by IV infusion of crystalloids.5 Acute kidney injury was significantly more prevalent in women than men with STEMI, as demonstrated by other studies.39 However, in our STEMI patients, acute kidney injury was significantly prevalent in nonsurvivors of both genders.
In addition, 30-day and 6-month survival of men was significantly better than that of women.
Our results suggest that, in STEMI patients of both genders, it is important to perform primary PCI as early as possible in order to prevent hemodynamic deterioration, resulting in pulmonary edema or cardiogenic shock. At the same time, we must pay attention to the risk of hospital acquired bacterial infection especially in men. In women, the risk of bleeding should be prevented by judicious and tailored use of antithrombotic drugs.
Strength of the Study
Our data originate from the real life, where all the consecutive STEMI patients were included. STEMI patients were treated according to the current guidelines of STEMI, with primary PCI as the leading reperfusion strategy and modern dual antiplatelet therapy as soon as possible after the first medical contact, with relatively high use of radial access during catheterisation and adjuvant pharmacological treatment during primary PCI with heparins and GPIIb/IIIa antagonists as bail-out therapy. The study provides important information about the differences and similarities between genders, in particular survivor and nonsurvivors of both genders, regarding baseline characteristics, the use of primary PCI, complications and pharmacological treatment.
Limitations of the Study
Limitations are several. One is a large difference in the proportion of men and women included, in particular between survivors and nonsurvivors of both genders, commonly encountered in a STEMI population. Relatively small sample size of nonsurvivors of both genders limits statistical analysis, in particular regression analysis.
Retrospective nature of the study may lead to selection and recall biases. Observational characteristic of the study cannot completely exclude residual confounding.
As this was a monocenter study from one PCI center the results are not representative for a larger population.
Finally, there are some missing data in particular on EF and laboratory tests due to early fatalities in STEMI patients or due to early transfer to the local hospitals.
Conclusion
Hospital mortality of women with STEMI exceeded that of men. However, after age adjustment, hospital mortalities in both genders were similar. Factors of hospital mortality in men and women with STEMI were mainly similar as well as the modern management of STEMI patients with primary PCI and antithrombotic drugs. In future, early invasive treatment by primary PCI should focus on elderly patients with STEMI, in particular with comorbidities and irrespective of gender, to improve early and late survival of STEMI patients.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Takagi K, Tanaka A, Yoshioka N, et al. In-hospital mortality among consecutive patients with ST-Elevation myocardial infarction in modern primary percutaneous intervention era ~ Insights from 15-year data of single-center hospital-based registry. PLoS One. 2021;16(6):e0252503. doi:10.1371/journal.pone.0252503
2. Zeymer U, Ludman P, Danchin N, et al.; On behalf of the ACVC EAPCI EORP ACS STEMI investigators group of the ESC. Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe: the ACVC-EAPCI EORP STEMI Registry of the European Society of Cardiology. Eur Heart J. 2021;42(44):4536–4549. doi:10.1093/eurheartj/ehab342
3. Timmis A, Townsend N, Gale CP, et al. European Society of Cardiology: cardiovascular Disease Statistics 2019 On behalf of the Atlas Writing Group The ESC Atlas of Cardiology is a compendium of cardiovascular statistics compiled by the European Heart Agency, a department of the European Society of Cardiology Developed in collaboration with the national societies of the European Society of Cardiology member countries. Eur Heart J. 2020;41(1):12–85. doi:10.1093/eurheartj/ehz859
4. Bauer D, Toušek P. Risk stratification of patients with acute coronary syndrome. J Clin Med. 2021;10(19):4574. doi:10.3390/jcm10194574
5. Ibanez B, Agewall J, Antunes MJ, et al. 2017 ESC Guidelines for the management of acute al infarction in patients presenting with ST-segment elevation The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
6. Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation an intravenous nPA for treatment of infarcting myocardium early II Trial Substudy. Circulation. 2000;102(17):2031–2037. doi:10.1161/01.CIR.102.17.2031
7. Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039–1044. doi:10.1503/cmaj.092119
8. Zorbozan O, Cevik AA, Acar N, et al. Predictors of mortality in ST-elevation MI patients. A prospective study. Medicine. 2018;97(9):e0065. doi:10.1097/MD.0000000000010065
9. Mehta RH, F-S O, Peterson ED, et al; American College of Cardiology-National Cardiovascular Database Registry Investigators. Clinical significance of post-procedural timi flow in patients with cardiogenic shock undergoing primary percutaneous coronary intervention. JACC. 2009;2(1):56–64. doi:10.1016/j.jcin.2008.10.006
10. Kammler J, Kypta A, Hofmann R, et al. TIMI 3 flow after primary angioplasty is an important predictor for outcome in patients with acute myocardial infarction. Clin Res Cardiol. 2009;98(3):165–170. doi:10.1007/s00392-008-0735-9
11. Bărcan A, Chițu M, Benedek E, et al. Predictors of mortality in patients with ST-segment elevation acute myocardial infarction and resuscitated out-of-hospital cardiac arrest. J Crit Care Med. 2016;2(1):22–29. doi:10.1515/jccm-2016-0001
12. Xi Z, Qiu H, Guo T, et al. Contemporary sex differences in mortality among patients with STsegment elevation myocardial infarction: a systematic review and meta-analysis. BMJ Open. 2022;12:e053379.
13. Bugiardini R, Ricci B, Cenko E, et al. Delayed Care and Mortality Among Women and Men With Myocardial Infarction. J Am Heart Assoc. 2017;6:e005968.
14. Khan E, Brieger D, Amerena J, et al. Differences in management and outcomes for men and women with ST-elevation myocardial infarction. Med J Aust. 2018;209(3):118–123. doi:10.5694/mja17.01109
15. Kanič V, Vollrath M, Tapajner A, Sinkovic A. Sex-related 30-day and long-term mortality in acute myocardial infarction patients treated with percutaneous coronary intervention. J Women’s Health. 2017;26(4):374–379. doi:10.1089/jwh.2016.5957
16. Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967;20(4):457–464. doi:10.1016/0002-9149(67)90023-9
17. Levey AS. Defining AKD: the spectrum of AKI, AKD, and CKD. Nephron. 2022;146(3):302–305. doi:10.1159/000516647
18. Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders H-J. Acute kidney injury. Nat Rev Dis Primers. 2021;7(1):52. doi:10.1038/s41572-021-00284-z
19. Steg PG, Huber K, Andreotti F, et al. Bleeding in acute coronary syndromes and percutaneous coronary interventions: position paper by the Working Group on Thrombosis of the European Society of Cardiology. Eur Heart J. 2011;32(15):1854–1864. doi:10.1093/eurheartj/ehr204
20. Calandra T, Cohen J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005;33(7):538–548. doi:10.1097/01.CCM.0000168253.91200.83
21. van der Meer MG, Nathoe HM, van der Graaf Y, Doevendans PA, Appelman Y. Worse outcome in women with STEMI: a systematic review of prognostic studies. Eur J Clin Invest. 2015;45(2):226–235. doi:10.1111/eci.12399
22. Gök G, Çoner A, Çınar T, et al. Evaluation of demographic and clinical characteristics of female patients presenting with MINOCA and differences between male patients: a subgroup analysis of MINOCA-TR registry. Turk Kardiyol Dern Ars. 2022;50(1):4–13. doi:10.5543/tkda.2022.86219
23. Kumar S, McDaniel M, Samady H, Forouzandeh F. Contemporary Revascularization Dilemmas in Older Adults. J Am Heart Assoc. 2020;9(3):e014477. doi:10.1161/JAHA.119.014477
24. Cenko E, Yoon J, Kedev S, et al. Sex differences in outcomes after STEMI effect modification by treatment strategy and age. JAMA Intern Med. 2018;178(5):632–639. doi:10.1001/jamainternmed.2018.0514
25. Sabbag A, Matetzky S, Porter A, et al. Sex differences in the management and 5-Year outcome of young patients (<55 Years) with acute coronary syndromes. Am J Med. 2017;130(11):1324.e15–22. doi:10.1016/j.amjmed.2017.05.028
26. Scholz KH, Maier SKG, Maier LS, et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39(13):1065–1074. doi:10.1093/eurheartj/ehy004
27. Elakabawi K, Huang X, Shah SA, et al. Predictors of suboptimal coronary blood flow after primary angioplasty and its implications on short-term outcomes in patients with acute anterior STEMI. BMC Cardiovasc Disorders. 2020;20(1):391. doi:10.1186/s12872-020-01673-0
28. Manzi MV, Buccheri S, Jolly SS, et al. Sex-related differences in thrombus burden in STEMI patients undergoing primary percutaneous coronary intervention. JACC. 2022;15(20):2066–2076. doi:10.1016/j.jcin.2022.08.013
29. Bertic M, Fordyce CB, Moghaddam N, et al. Association of left anterior descending artery involvement on clinical outcomes among patients with STEMI presenting with and without out-of-hospital cardiac arrest. Open Heart. 2020;7:e001065.
30. Karam N, Bataille S, Marijon E, et al. For the e-MUST study investigators, incidence, mortality, and outcome-predictors of sudden cardiac arrest complicating myocardial infarction prior to hospital admission. Circ Cardiovasc Interv. 2019;12:e007081.
31. Jenča D, Melenovský V, Stehlik J, et al. Heart failure after myocardial infarction: incidence and predictors. EHJ Heart Fail. 2021;8(1):222–237. doi:10.1002/ehf2.13144
32. Wei J, Henry TD. Gender equity in STEMI: not so simple! Catheter Cardiovasc Interv. 2015;85(3):369–370. doi:10.1002/ccd.25800
33. Yu J, Mehran R, Grinfeld L, et al. Sex-based differences in bleeding and long term adverse events after percutaneous coronary intervention for acute myocardial infarction: three year results from the HORIZONS-AMI trial. Catheter Cardiovasc Interv. 2015;85(3):359–368. doi:10.1002/ccd.25630
34. Lindholm D, Sarno G, Erlinge D, et al. Combined association of key risk factors on ischaemic outcomes and bleeding in patients with myocardial infarction. Heart. 2019;105(15):1175–1181. doi:10.1136/heartjnl-2018-314590
35. Matsuura Y, Moribayashi K, Kaikita K. Optimal antithrombotic therapy in patients undergoing percutaneous coronary intervention: a focused review on high bleeding risk. J Atheroscler Thromb. 2022;29(10):1409–1420. doi:10.5551/jat.RV17066
36. Valgimigli M, Gragnano F. The benefit and harm of treating STEMI: between ischemia, bleeding, and reperfusion injury. Eur Heart J. 2020;9:259–261.
37. Gargiulo G, Giacoppo D, Jolly SS, et al. Effects on mortality and major bleeding of radial versus femoral artery access for coronary angiography or percutaneous coronary intervention: meta-analysis of individual patient data from 7 multicenter randomized clinical trials. Circulation. 2022;146(18):1329–1343. doi:10.1161/CIRCULATIONAHA.122.061527
38. Tersalvi G, Biasco L, Cio GM, Pedrazzini G. Acute coronary syndrome, antiplatelet therapy, and bleeding: a clinical perspective. J Clin Med. 2020;9(7):2064. doi:10.3390/jcm9072064
39. Frydman S, Freund O, Banai A, Zornitzki L, Banai S, Shacham Y. Relation of gender to the occurrence of AKI in STEMI patients. J Clin Med. 2022;11(21):6565. doi:10.3390/jcm11216565
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
