Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Factors Influencing Long-Term Behavioral Intervention Outcomes in Preschool Children with Attention-Deficit Hyperactivity Disorder in Southeast China
Authors Huang X, Qian Q, Huang Y, Wang Y, Ou P
Received 21 June 2023
Accepted for publication 10 August 2023
Published 4 September 2023 Volume 2023:19 Pages 1911—1923
DOI https://doi.org/10.2147/NDT.S424299
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Xin-xin Huang,1 Qin-fang Qian,2 Yan Huang,2 Yan-xia Wang,2 Ping Ou1
1The Ministry of Health, Fujian Maternity and Child Health Hospital College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian Province, People’s Republic of China; 2The Child Health Division, Fujian Maternity and Child Health Hospital College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian Province, People’s Republic of China
Correspondence: Ping Ou, Tel +86-13905916211, Email [email protected]
Introduction: Previous studies have demonstrated the long-term effectiveness of behavioral interventions for attention-deficit hyperactivity disorder (ADHD) in preschool children. We continue to design a case‒control study to further investigate the factors influencing the long-term effect of behavioral intervention.
Methods: From May 2020 to August 2021, children who were newly diagnosed with ADHD and not receiving any treatment received a one-year behavioral intervention. A total of 86 children completed the behavioral intervention and assessment.
Results: 50 children (58.140%) were in the effective group, and 36 children (41.860%) were in the ineffective group. Attention retention time (OR=0.559, 0.322– 0.969), Swanson, Nolan, and Pelham total score (OR=1.186, 1.024– 1.374) at baseline, performance score for parents (OR=0.631, 0.463– 0.859), and teacher coordination (OR=0.032, 0.002– 0.413) were the influencing factors of behavioral intervention effects. The area under the receiver operating curve was 0.979 (p< 0.001). The comprehensive nomogram model showed that the discrimination and mean absolute error were 0.979 and 0.023, respectively.
Discussion: During behavioral intervention, the implementation skills of parents should be evaluated in a timely manner. The behavioral intervention effect can be predicted based on a child’s attention retention time at baseline, teacher involvement, behavioral scale score, and performance score for parents, which can guide clinicians in adjusting personalized treatment plans and provide a basis for clinical decision-making. The treatment of ADHD in preschool children requires a systematic framework that integrates family, school, and society.
Keywords: attention-deficit hyperactivity disorder, behavioral intervention, influencing factors, preschool child
Attention-deficit hyperactivity disorder (ADHD) is a childhood-onset neurodevelopmental disorder that is characterized by a persistent pattern of inattention, hyperactivity, and impulsivity1 and is often accompanied by comorbid conditions such as autism spectrum disorder (ASD), oppositional defiant disorder (ODD) or conduct disorder (CD).2 Cross-sectional studies with large samples have found reduced brain indicators among children with ADHD, with major differences in surface area measures.3 Multiple studies have shown that ADHD can result in impaired behavioral functioning across home and school settings and is associated with negative academic outcomes,4,5 leading to dropout in severe cases.6 There are three subtypes of ADHD: inattention type (ADHD-I), hyperactive-impulsive type (ADHD-H), and combined type (ADHD-C). Recent studies suggest that ADHD diagnosed in childhood predicts the development of adverse childhood experience (ACE) and that the inattentive subtype may have the greatest impact on this risk.7 Children diagnosed with ADHD in preschool have more functional impairment than those not diagnosed with ADHD at preschool age.8
The purpose of ADHD treatment is to improve core symptoms and reduce behavioral problems. The current evidence-based treatment for ADHD involves the use of psychostimulant medications and behavioral interventions9–11 and their combination. Psychostimulant medications are first-line medications for ADHD. Recent mechanistic studies have suggested that psychostimulants increase static FC and decrease dynamic FC (DFC), and DFC is associated with therapeutic effects.12 However, drug treatments can lead to potential adverse side effects.13 Because behavioral interventions may improve outcomes, reduce treatment costs, and minimize side effects,14 they are the first treatment choice for preschool children.15–17 The American Academy of Pediatrics (AAP) recommends behavioral parent training (BPT) as the first line of treatment for preschool-aged children with ADHD.13 China’s latest guidelines for ADHD diagnosis and treatment also emphasize the use of behavioral interventions in children under the age of 12 years.18
Parent training is designed to train parents to use behavioral or cognitive behavioral techniques to manage their children’s behavior. Parent-based behavior interventions have been shown to reduce disruptive behavior in children, and therapeutic effects persist after treatment completion.19 In preschoolers with ADHD, the goals of this training may include increased focus and compliance, as well as the management of hyperactive-impulsive behaviors through effective parenting. The programmes vary in style and content but are generally manual-based and may involve discussion and the use of videos and role play.20 Reviews of the literature showed that parent behavioral training demonstrates the strongest evidence of efficacy for the treatment of preschool children with ADHD.19 Studies in the early phase of the project21 also confirmed that behavioral interventions show positive effects. However, another meta-analysis showed that the positive impact of parent training for ADHD ranged from no impact to strong.22 The AAP has noted that if a behavioral intervention does not lead to significant improvement, medication can be prescribed, but it is the secondary treatment for preschoolers.16 The national studies conducted after the AAP guidelines were published showed that approximately three-fourths of insured children aged 2–5 years received clinical care for ADHD and medication.23 This suggests the need to study factors related to the effects of behavioral interventions to make better treatment decisions and to carry out personalized treatment. For children who are predicted to have poor efficacy of behavioral intervention, other treatment methods, such as drug therapy, should be given in time to reduce symptoms, prevent secondary problems and enable a better start to school.
At a research hospital in Southeast China, pediatricians, child mental health physicians and psychotherapists offered behavioral interventions to children with ADHD for a period of one year. Data were collected from the children before and after the behavioral interventions, and a case‒control study was conducted according to the effectiveness of the behavioral intervention. We hypothesized that the effectiveness of the behavioral interventions would be influenced by parent implementation skills and teacher cooperation. The first aim of this study was to analyze the factors that influence the effects of behavioral intervention. The second aim of the study was to predict the effect of the behavioral intervention.
Methods
Procedure
Preschool children diagnosed with ADHD received behavioral interventions that continued for 12 months.
Study Setting and Design
This case–control study was conducted from May 2020 to August 2021 in a tertiary health care facility in Southeast China.
Participants
Preschoolers with ADHD were recruited to participate in this behavioral intervention study. The inclusion criteria were as follows: preschool children first diagnosed with ADHD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). None of the children had enrolled in an early intervention center or received treatment via medication or behavioral interventions.
The exclusion criteria were as follows: (a) a development quotient (DQ) score <75, (b) a history of seizures and/or taking medication to prevent seizures, (c) a childhood history or concurrent diagnosis of pervasive developmental disorder or organic mental disorders, and (d) placement in special education classrooms.
Group Situation
ADHD Rating Scale IV–parent version (ADHD-RS-IV): This scale has been validated as a useful instrument to assess ADHD symptoms among children and adolescents.24 The response to ADHD treatment was defined as an improvement in the ADHD-RS-IV score of ≥30%.25,26 In this study, the effective group was defined as children whose rates of decrease in ADHD-RS IV score and improvement in attention retention time were both greater than 30%; the ineffective group was defined as all other children.
Behavioral Intervention
The participating physicians designed the behavioral interventions according to the Chinese guidelines for the diagnosis and treatment of ADHD.18 The details were as follows: (a) Face-to-face parent training: Professional child psychologists offered weekly one-hour parent sessions for three months in the outpatient clinic. The participants were parents who had lived with a child with a confirmed diagnosis of ADHD for a long time and were responsible for the child’s primary and outpatient care. The purpose of the training was to help parents systematically understand ADHD, improve the parenting skills of parents and master the methods of family behavior management. Part of the course was background knowledge of ADHD, taking a close look at our problems, learning to like each other again, clear daily structures, making effective requests and not skimp on praise, learning how to play attentively, getting to know each other and exploring current externalizing symptoms of the child, focusing on positive experiences with the child, implementation of clear rules, social reinforcement and positive consequences of rules, examples of coping skills (eg, coping skills for reaction to stress and conflict with children) and interaction skill training for parents (eg, behavior management, self-regulation, improving organization, improving relationship, and use of encouragement). At the end of each session, parents received home assignments that were discussed at the beginning of the next session. Where parents failed to fully understand topics discussed before or experienced difficulties with techniques from particular sessions, an extra session was given. b) Attention training: After parent training, parents were trained at home under the guidance of physicians. Parents were trained to observe and record the children’s attention time at baseline and formulate an attention training goal (such as 10 minutes) based on the children’s symptoms and the results of the baseline scale assessment. Specifically, choose a quiet room in the family, children have a separate desk and chair, put the alarm clock on the children’s desk, and set to ring after 10 minutes. Parents arranged tasks that the child could perform independently at his or her age and told the child to perform independently within 10 minutes. Parents looked for signs of inattention, hyperactivity and other symptoms before the alarm. If not, it was recorded as achieving the training goal. The training was performed twice a day in two relatively fixed periods. Training was considered effective if the training target was met 90% of the time over a consecutive period. (c) Behavioral therapy: Behavioral therapy was provided at home by parents under the guidance of a physician. Parents and physicians worked together to develop and prioritize goals for behavior improvement. Parent-administered interventions attempt to enhance a parent’s understanding of child behavior management and the quality of parent‒child interactions, with the ultimate goal of optimizing the child’s developmental course. The behavioral training program included positive reinforcement, extinction and punishment methods:27 1) The positive reinforcement method involved strengthening good behavior through reward and other ways and giving positive reinforcement immediately when children had good behavior. 2) The extinction method: before treatment, it was necessary to determine what factors had a reinforcing effect on their children’s bad behaviors and reduce or eliminate some bad behaviors by planned neglect (stopping reinforcement). 3) The punishment method involved enforcing the appropriate consequences or punishment when the children failed to achieve the goal. In the process of behavioral intervention, the reward-outcome correspondence strategy was used until the completion of the task, and the expectation value of each task was gradually increased until the child’s behavior changed. The target behaviors were the change in ADHD symptom score after treatment.
Parents recorded the effect of children’s behavioral training in the form of daily report cards, implementation of token economy or points strategy, and cash points once every half month.
Teachers were also invited if conditions permitted. Behavioral intervention strategies in schools included priority seating arrangements, adjustments of class assignments, increased interaction/reminder, and classroom behavior management.27 The physicians also trained the teachers on how to deal with emergencies at school and encouraged the children with ADHD to follow rules and stick to tasks.
Children were followed up every half a month in the first 3 months of the intervention and once a month thereafter. The outpatient interview follow-up lasted for 33.793 minutes on average (SD=2.610).
Assessment
(a) Attention retention timings: In a quiet environment, children were required to complete drawing, writing or learning assignments based on their age. The parents observed the children and noted their completion times.
(b) ADHD-RS-IV:24 The higher the score, the more symptomatic the child. Su et al confirmed the reliability and validity of the Chinese scale in 2006.28 The assessments were performed by trained experienced physicians.
(c) Swanson, Nolan, and Pelham (SNAP-IV) checklist: This is an assessment tool for ADHD.29 Zhang et al20 confirmed the reliability and validity of the Chinese scale for children before school age in 2016. Children were assessed by two parents, usually the father and mother, at the same time and averaged.
(d) Performance score for parents: Physicians evaluated the implementation of parental behavioral interventions during outpatient interviews. This study assigned a score of 1–3; higher scores indicated better parent implementation, which was assessed monthly for 12 months and expressed as a total score.
Data Collection
Information on the children was collected retrospectively from the medical record system. If missing data or unqualified data in logical examination were found, the treating physician was immediately contacted for verification and correction.
Sample Size
The sample size was calculated using PASS 15.0 software. Based on the results of earlier studies, we concluded that a moderate impact amount of 0.5 should be detected in the clinically assessed ADHD-RS-IV, with a one-sided 5% significance level and 85% power. At least 25 participants were required for both the effective group and the ineffective group.
Quality Control
The physicians who participated in the behavioral interventions and outcome assessment were trained to a uniform standard. We kept a complete list of encoding, security and storage plans, including any associated processes, to improve data quality. The data monitoring committee was composed of personnel with no competing interests who reviewed all data records and statistical results at the end of the intervention.
Statistical Analyses
Statistical analyses were performed using SPSS 26.0. Continuous variables were expressed as the means ± standard deviations (SDs) or as medians [interquartile range], and Student’s t-tests or Wilcoxon rank-sum tests were performed depending on the normality of the variables’ distributions, as appropriate. The categorical variables were expressed as n (%), and the chi-square test was performed for comparison. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by multivariate analysis using backward logistic regression analysis. We used the Wald statistic, in which the variables with p≥0.15 were eliminated from the model one by one. Receiver operating characteristic (ROC) curves, sensitivity and specificity were utilized to assess the predictive performance. The level of significance was 0.05 for all analyses. Nomogram construction and C-index calculation were performed using R 4.0.5 software (http://www.R-project.org).
Results
During the recruitment period, a total of 98 preschool-age children with ADHD were enrolled, and 8 children were excluded (3 children with DQ scores <75, 1 child taking antiepileptic drugs, and 4 children in special education classrooms). After 12 months of the behavioral intervention, 4 children were lost to follow-up, and 86 were ultimately included in the analysis (Figure 1).
There were 50 children (58.140%) in the effective group and 36 children (41.860%) in the ineffective group. Among the 86 participants, 52 (60.465%) children were diagnosed with the inattention type (ADHD-I), 8 (9.302%) with the hyperactive-impulsive type (ADHD-H), and 26 (30.233%) with the combined type (ADHD-C). The children had a mean age of 59.675 months (SD=7.462) and a mean DQ score of 96.665 (SD=7.602). There were no significant group differences in age, gender, DQ scores or subtypes of ADHD (Table 1).
 |
Table 1 Descriptive Information of the Children in Both Groups |
Table 2 presented the interquartile ranges of the main evaluation indices of the children in the two groups. The ADHD-RS-IV and SNAP scores at baseline and the post-intervention ADHD-RS-IV scores of the effective group were lower than those of the ineffective group, but the attention retention times both at baseline and postintervention were higher than those of the ineffective group.
 |
Table 2 Interquartile Ranges of the Main Evaluation Indices of the Children in the Two Groups |
Table 3 presented the means, standard deviations, and bivariate correlations of all primary study variables. The attention deficit and hyperactivity impulsivity dimensions of the children’s ADHD scale were positively correlated with the corresponding dimensions of the SNAP scale, with correlation coefficients of 0.669 (p<0.001) and 0.812 (p<0.001), respectively.
 |
Table 3 Mean Standard Deviation and the Correlation Between the ADHD and SNAP-IV Scales |
Univariate analysis showed that compared with the effective group, the ineffective group had shorter attention retention times and higher SNAP scores at baseline, poor performance scores for parents, more than one complication, lack of teacher cooperation, and lower parental education levels, with significant differences (p<0.001). Variables with statistical significance in the univariate analysis (exclusion criteria p=0.15) were included in the multivariate analysis, which revealed that attention retention times, SNAP total scores at baseline, performance scores for parents, and teacher coordination with the intervention were the factors that influenced the intervention effect (Table 4).
 |
Table 4 The Analysis of the Effect of the Behavioral Intervention Using Univariable and Multivariable Logistic Regression |
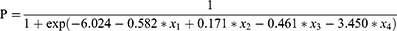
The estimated equation of the behavioral intervention effect for children with ADHD was as follows:
The p value represented the probability of poor behavioral intervention effects. x1, x2, x3 and x4 represented attention retention time at baseline, the SNAP total score at baseline, performance scores for parents, and teacher coordination, respectively.
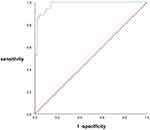
The ROC curve (Figure 2) was constructed by using the predicted probability of logistic regression as the state variable and the efficacy as the test variable, and the AUC value was 0.979 (95% CI: 0.955–1.000, P<0.001), indicating that the diagnostic value was good. The sensitivity and specificity were 86.0% and 97.2%, respectively.
The Hosmer‒Lemeshow goodness of fit test was used to evaluate the calibration ability of the prediction model. The results showed that the likelihood ratio 2 was 4.694 and the P value was 0.790, indicating that there was no significant difference between the predicted value and the observed value, and the calibration degree of the model had a good degree of fit.
Based on the results of multivariable analyses, a nomogram for the risk of ineffective treatment was formulated, as shown in Figure 3A. The performance score for parents was found to have the highest impact on the prediction of efficacy.
 |
Figure 3 Nomogram and calibration curve for the incident risk of the nonefficacy of behavioral interventions in preschool children with ADHD in China: (A) nomogram and (B) calibration plot. |
The discrimination of the nomogram yielded a c-index of 0.979. The mean absolute error of the calibration curve of the nomogram was 0.023, as shown in Figure 3B.
Discussion
This study analyzed factors influencing the effectiveness of a 12-month behavioral intervention in preschool children diagnosed with ADHD. We found that short attentional retention time at baseline, poor performance scores by parents, high SNAP total score, and noninvolvement of teachers in behavioral interventions were associated with a risk of low efficacy. In addition, although no statistical significance was shown in the multivariate analysis, the comorbidities and parental education level were significant in the univariate analysis. A prediction model of the behavioral intervention effect for children with ADHD was constructed. The AUC was 0.979, which reflected the good quality of the ROC curve. The nomogram and calibration curve of factors influencing the efficacy of behavioral interventions were plotted.
ADHD is a chronic health condition requiring long-term adherence to treatment. A study has shown that providing a behavioral intervention before initiating medication can lead to better outcomes than if medication is administered first.30 Moreno20 conducted a randomized controlled study and found that behavioral interventions had a greater effect on response control and attention improvement than neurofeedback therapy and pharmacological therapy. Franke conducted a randomized controlled trial to evaluate the effect of an online self-help program for parents in the treatment of ADHD in preschool children and found that hyperactivity/inattention, agitation/impulsivity, resistance/aggression, social functioning, and teacher-rated prosocial behavior in children were significantly improved.31 Teasdale32 studied the effect of a brief behavioral intervention for preschool children with ADHD for up to one year. The results demonstrated significant improvements in parent- and teacher-reported child hyperactivity and inattention, with sustained improvement at 6 months and 1 year postintervention. In preschool children, behavioral interventions are generally delivered directly to parents via BPT.33 The reported behavioral interventions included instruction manuals for parents and regular teleconferencing with professionals.34 Our study was different from the above. First, we further analyzed the factors affecting the effectiveness of behavioral interventions based on the long-term effectiveness shown in previous randomized controlled trials. Second, regular face-to-face outpatient interviews were conducted to understand parents’ intervention implementation skills and to guide them to improve their skills. Third, outpatient physicians evaluated and recorded the implementation of parental behavioral interventions, which were quantified by scores. Fourth, children’s attention time accurately recorded by parents was used as an objective indicator. Finally, for eligible children, we also invited teachers to participate in behavioral intervention through classroom management and other means.
The BPT intervention recommended by the AAP focuses on modifying parenting to treat children’s problem behaviors and has been consistently recognized as an effective treatment for disruptive behavior and ADHD.35 However, significant improvements in BPT were not universal. Clinical work has shown that not all children respond similarly to interventions or positive parental behaviors. For example, a recent German36 randomized trial of the first-line capacity of a behavioral intervention to reduce the need for medication in children with ADHD showed that 63% of the nonbehavioral intervention group was medicated at the endpoint, and 26% of the behavioral intervention group was also taking medication. It can be concluded that children with ADHD have different symptoms or comorbidities, which makes it unlikely that behavioral interventions will be equally effective for all individuals, so it is necessary to emphasize the need for individualized treatment programs.
A number of parent, child, and family factors were explored as factors that potentially influence BPT efficacy. child symptom characteristics may influence parents’ ability to implement parenting skills – a link that may be explained, in part, by increases in parenting-related stress.37 Parent involvement is critical to the success of BPT. Suboptimal parent engagement undermines the potency and effectiveness of the intervention and limits improvement in parent and child outcomes. It is estimated that 40% to 60% of parents of children with ADHD have difficulty fully participating in treatment.38 In classic BPT, parents attend treatment sessions without their child, and changes in child outcomes are dependent on changes in parent knowledge, beliefs, and behavior.39 This study found that attention retention time, baseline Swanson, Nolan, and Pelham total scores, performance score for parents, and teachers’ cooperation were the influencing factors of the effect of behavioral intervention. We conclude that parental understanding and implementation of the behavioral intervention is one of the main factors affecting the efficacy of the intervention in children. In the process of behavioral intervention, it is necessary to fully consider the understanding, cooperation and implementation of parents to improve the compliance of parents. Our interventions included on-site parent training, a combination of intensive discussions and individual counseling, and regular one-on-one outpatient interviews and assessments. These measures had the advantage of strengthening the interactions among physicians, parents and children, allowing the observation and collection of data regarding changes in the children’s symptoms in a timely manner, allowing the identification of and improvement in inappropriate parenting behaviors, providing parents with counseling and treatment strategies, and adjusting individualized behavior intervention programs. We used on-site interviews with outpatient physicians and recorded parents’ participation and implementation in a unified standard quantitative scoring method every month to ensure the reliability of the data analysis results. In the future, children’s baseline attention level and comorbidities should be routinely assessed before initiating behavioral interventions, and children with severe symptoms should have more frequent visits to closely monitor their behavioral improvement. For parents with low education levels or insufficient executive ability, more attention should be given to increasing the amount of training for parents, and in-depth interviews should be conducted to understand what aspects of parents cannot effectively implement behavior management. Individual parental guidance or additional behavioral attention management sessions for children were provided when necessary. In this study, children’s baseline attention time recorded by parents was used as an objective indicator to help parents recognize the degree of their children’s symptoms by comparing the attention time of normal children. On the other hand, we take the baseline attention level as the target basis for formulating attention training, which can assist parents in conducting attention training and effect evaluation at home so that children and parents can grasp the effect of behavioral intervention for the first time, and parents can give positive reinforcement in time to improve children’s enthusiasm and confidence and improve parents’ cognitive level and compliance.
The collaborative life skills (CLS) program40 was developed in the US and implemented by school mental health providers (SMHPs) with the participation of schools, parents and students. In randomized controlled trials with children with ADHD and ODD symptoms, parent- and teacher-reported posttreatment CLS gains, organizational skills and academic competence were maintained into the next school year. The difference in these studies was that the CLS programs were for school-age children, including those who were on medication, while in our study, the program was for preschool children who had not started medication. Because children are in kindergarten for approximately 6–7 hours every day, the influence of the teacher is a key factor. Recent findings highlight the need to strengthen teacher training for children with ADHD and to promote school involvement in children’s academic life.41 Combined with our study conclusions, the structure of behavioral interventions should be improved in the future, and school participation should be emphasized. Teachers, parents, and physicians should jointly develop behavioral intervention plans and regularly exchange information. A systemic framework should integrate the family, school and society in ADHD prevention and treatment.42
There is a clear need for behavioral therapies in clinical practice, as they may be the first choice for patients43 and families and can reduce the need for medications.43,44 The heterogeneity of symptoms and comorbidities in children with ADHD makes it unlikely that behavioral treatments will be equally effective for all individuals, emphasizing the need for more individualized treatment plans. However, there is a lack of a holistic approach to identify the predictors of behavioral interventions. Based on logistic regression, nomograms can estimate the probability of failure of behavioral therapy by integrating various risk predictors, which meets our needs for visualization tools. Through a user-friendly digital interface, improved accuracy, and easier-to-understand risk predictions compared to traditional mathematical formulas, rapid computational nomograms can seamlessly integrate risk assessment into clinical decision making.45 With the help of these simple, rapid, inexpensive and noninvasive tools, we hope to be able to timely and effectively identify children who do not respond to behavioral intervention alone. For children with severe baseline symptoms, difficulties for parents to implement behavioral intervention, and low probability of predicted effect, there is no need to continue to wait to complete all cycles of behavioral intervention. Other treatment options, such as drug therapy, can be considered in advance to improve the prognosis of children.
Advantages
The children with ADHD were recruited through the centers’ outpatient clinics, which were highly experienced in the treatment of ADHD children. We observed a very low lost-to-follow-up rate, probably due to regular outpatient visits. In the daily form, we developed an easy-to-operate behavioral intervention program that was easy to implement and promote. We used strictly measured attention retention times as an objective indicator. On the one hand, this measure can help parents observe their children’s performance at any time. On the other hand, this measure coordinates with a reduction in the ADHD-RS-IV behavior scale score and combined subjective and objective evaluations as an indicator to test the effect of interventions, with good reliability. We developed nomograms that can be used in the outpatient setting to quickly calculate the efficacy in children. The sample size of this study was relatively large, which provided sufficient statistical power in detecting correlations.
Limitations
Our data were collected at one hospital, and the parents in the study may have greater awareness of health care, which limits the generalization of the conclusion.
Conclusions
Our data showed that possible factors affecting the effect of behavioral interventions in preschool children with ADHD included basic attention retention time, performance score for parents, total SNAP score, and teacher cooperation. In the process of behavioral intervention, outpatient physicians should conduct in-depth interviews, regularly evaluate the implementation of parents, recommend that teachers participate in behavioral intervention, collect the baseline level of children, predict the probability of effective behavioral intervention based on the nomogram, adjust the individualized treatment plan in time, and start drug treatment as soon as necessary to provide a basis for clinical decision-making and improve the prognosis of children.
Abbreviations
ADHD, Attention deficit hyperactivity disorder; ODD, oppositional defiant disorder; CD, conduct disorder; DQ, development quotient; DFC, decrease dynamic FC.
Data Sharing Statement
Data are available upon reasonable request. The authors are not authorized to share unauthorized data with a third party. However, data for statistical analysis are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study was conducted under the ethical principles of the Declaration of Helsinki. The study was approved by the Human Subjects Ethics Committee of Fujian Maternity and Child Healths Hospital (reference number HREC 2016-009). Parents were informed about the study’s purpose and content. Written informed consent was obtained from the parents and caregivers. To ensure patient privacy, all participants’ personal or sensitive information was marked with an alphabetic or numeric code. All authors are in agreement with the content of the manuscript.
Acknowledgment
All authors thank the participant’s children and their parents for their active participation in the study.
Author Contributions
The corresponding author confirms that all listed authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Guiding Project of the Science and Technology Department of Fujian Province, China (No. 2023Y0056).
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders.
2. Thapar A, Cooper M. Attention deficit/hyperactivity disorder. Lancet. 2016;387(10024):1240–1250. doi:10.1016/S0140-6736(15)00238-X
3. Bernanke J, Luna A, Chang L, Bruno E, Dworkin J, Posner J. Structural brain measures among children with and without ADHD in the Adolescent Brain and Cognitive Development Study cohort: a cross-sectional US population-based study. Lancet Psychiatry. 2022;9(3):222–231. doi:10.1016/S2215-0366(21)00505-8
4. Coghill D, Hodgkins P. Attention-deficit/hyperactivity disorder versus children with diabetes and healthy controls. Eur Child Adolesc Psychiatry. 2016;25(3):261–271. doi:10.1007/s00787-015-0728-y
5. Fabiano GA, Schatz NK, Aloe AM, Chacko A, Chronis-Tuscano A. A systematic review of meta-analyses of psychosocial treatment for attention-deficit/hyperactivity disorder. Clin Child Fam Psychol Rev. 2016;18(1):77–97. doi:10.1007/s10567-015-0178-6
6. Mirza H, Roberts E, Al-Belushi M. School dropout and associated factors among omani children with attention-deficit hyperactivity disorder: a cross-sectional study. J Dev Behav Pediatr. 2018;39(2):109–115. doi:10.1097/DBP.0000000000000522
7. Lugo-Candelas C, Corbeil T, Wall M. ADHD and risk for subsequent adverse childhood experiences: understanding the cycle of adversity. J Child Psychol Psyc. 2021;62(8):971–978. doi:10.1111/jcpp.13352
8. Mulqueen JM, Bartley CA, Bloch MH. Meta-analysis: parental interventions for preschool ADHD. J Atten Disord. 2015;19(2):118–124. doi:10.1177/1087054713504135
9. Conner CK. Forty years of methylphenidate treatment in Attention Deficit/Hyperactivity disorder. J Atten Disord. 2002;6(1):S17–S30. doi:10.1177/070674370200601s04
10. Greenhill LL, Pliszka S, Dulcan MK. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry. 2002;41(2):26–49. doi:10.1097/00004583-200202001-00003
11. Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2014;43(4):527–551. doi:10.1080/15374416.2013.850700
12. Wang Y, Kessel E, Lee S. Causal effects of psychostimulants on neural connectivity: a mechanistic, randomized clinical trial. J Child Psychol Psyc. 2022;63(11):1381–1391. doi:10.1111/jcpp.13585
13. Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M; Subcommittee on children and adolescents with attention-deficit/hyperactive disorder. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144(4):e20192528. doi:10.1542/peds.2019-3997
14. Page TF, Pelham WE, Fabiano CA. Comparative cost analysis of sequential, adaptive, behavioral, pharmacological, and combined treatments for childhood ADHD. J Clin Child Adolesc Psychol. 2016;45(4):416–427. doi:10.1080/15374416.2015.1055859
15. Zheng Y, Liu J. Interpretation of the 2nd edition of Chinese Guidelines for the Prevention and Treatment of attention deficit hyperactivity disorder. Chinese Journal of Psychiatry. 2016;49(3):132–135.
16. Wolraich M, Hagan JF, Allan C, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi:10.1542/peds.2011-2654
17. Hart KC, Ros R, Gonzalez V, Graziano PA. Parent perceptions of medication treatment for preschool children with ADHD. Child Psychiatry Hum. 2018;49(1):155–162. doi:10.1007/s10578-017-0737-9
18. Zwi M, Jones H, Thorgaard C. Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev. 2011;12(7):CD003018. doi:10.1002/14651858.CD003018.pub3
19. Charach A, Carson P, Fox S, Ali MU, Beckett J, Lim CG. Interventions for preschool children at high risk for ADHD: a comparative effectiveness review. Pediatrics. 2013;131(5):e1584–e1604. doi:10.1542/peds.2012-0974
20. Zhang FF, Zhang JS, Shuai L. Reliability and validity test of parental version of SNAP-IV Rating Scale for preschoolers. Zhong Guo Er Tong Baojian Za zh. 2016;24(12):1253–1256.
21. Huang XX, Ou P, Qian QF, Huang Y. Long-term effectiveness of behavioral intervention in preschool children with attention deficit hyperactivity disorder in Southeast China-a randomized controlled trial. BMC Pediatr. 2021;21(1):561. doi:10.1186/s12887-021-03046-8
22. Moreno-Garcia I, Meneres-Sancho S, Camacho-Vara de Rey C, Servera M. A randomized controlled trial to examine the posttreatment efficacy of neurofeedback, behavior therapy, and pharmacology on ADHD measures. J Atten Disord. 2019;23(4):374–383. doi:10.1177/1087054717693371
23. Visser SN, Danielson ML, Wolraich ML. Vital signs: national and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2–5 years—United States, 2008–2014. MMWR Morb Mortal Wkly Rep. 2016;65(17):443–450. doi:10.15585/mmwr.mm6517e1
24. Zhang S, Faries DE, Vowles M. ADHD Rating Scale IV: psychometric properties from a multinational study as a clinician-administered instrument. Int J Methods Psychiatr Res. 2005;14(4):186–201. doi:10.1002/mpr.7
25. Steele M, Jensen PS, Quinn DM. Remission versus response as the goal of therapy in ADHD: a new standard for the field? Clin Ther. 2006;28(11):1892–1908. doi:10.1016/j.clinthera.2006.11.006
26. Yu T, Liu RX, Ding KJ. Changes in parenting stress in children with attention deficit hyperactivity disorder after methylphenidate hydrochloride treatment. Zhong Guo Xin Li Wei Sheng Za Zhi. 2019;33(8):601–606.
27. Hongzhu Z, Xiaobong Z. American Academy of Pediatrics 2011 edition Attention deficit hyperactivity disorder in children and adolescents Interpretation of a practical clinical guideline for the diagnosis, Evaluation, and management of disorders. Chin J Pract Pediatr. 2012;27(2):99–101.
28. Su IY, Geng YG, Wang H. Norm formulation and reliability and validity test of the Parental version of the Attention Deficit Hyperactivity Disorder Diagnostic Scale in Chinese urban children. Zhong Guo Shi Yong Er Ke Za Zhi. 2006;21(11):833–836.
29. Pelham WE, Murphy H. The SNAP Checklist: A Teacher Checklist for Identifying Children with Attention Deficit Disorders [Unpublished manuscript]. Florida State University; 1981.
30. Pelham WE, Fabiano GA, Waxmonsky JG. Treatment sequencing for childhood ADHD: a multiple-randomization study of adaptive medication and behavioral interventions. J Clin Child Adolesc Psychol. 2016;45:396–415. doi:10.1080/15374416.2015.1105138
31. Franke N, Keown LJ, Sanders MR. An RCT of an online parenting program for parents of preschool-aged children with ADHD symptoms. J Atten Disord. 2020;24(12):1716–1726. doi:10.1177/1087054716667598
32. Teasdale AE, Duran PA, Axelrad ME. Effectiveness of Clinic-Based Brief Behavioral Intervention (BBI) in long-term reduction of ADHD symptoms among preschoolers. J Clin Psychol Med S. 2023;30(2):403–414. doi:10.1007/s10880-022-09907-3
33. Antshel KM, Barkley R. Attention deficit/hyperactivity disorder. Handb Clin Neurol. 2020;174:37–45. doi:10.1016/B978-0-444-64148-9.00003-X
34. Dopfner M, Liebermann-Jordanidis H, Kinnen C. Long-term effectiveness of guided self-help for parents of children with ADHD in routine care-an observational study. J Atten Disord. 2021;25(2):265–274. doi:10.1177/1087054718810797
35. Comer JS, Chow C, Chan PT, Cooper-Vince C, Wilson LAS. Psychosocial treatment efficacy for disruptive behavior problems in very young children: a meta-analytic examination. J Am Acad Child Adolesc Psychiatry. 2013;52(1):26–36. doi:10.1016/j.jaac.2012.10.001
36. Coles EK, Pelham Iii WE, Fabiano GA. Randomized trial of first-line behavioral intervention to reduce need for medication in children with ADHD. J Clin Child Adolesc Psychol. 2020;49(5):673–687. doi:10.1080/15374416.2019.1630835
37. Hedelin B, Hall-Lord ML. Family functioning, psychological distress, and well-being in parents with a child having ADHD. SAGE Open. 2016;6(1):1–10.
38. Chacko A, Wymbs BT, Chimiklis A, Wymbs FA, Pelham WE. Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. J Abnorm Child Psychol. 2012;40(8):1351–1362. doi:10.1007/s10802-012-9666-z
39. Chorpita BF, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children’s mental health services: which elements for which outcomes? J Clin Child Adolescent Psychol. 2015;44(1):30–43. doi:10.1080/15374416.2013.814543
40. Pfiffner LJ, Rooney ME, Jiang Y, Haack LM, Beaulieu A, McBurnett K. Sustained effects of collaborative school-home intervention for Attention-Deficit/Hyperactivity disorder symptoms and impairment. J Am Acad Child Adolesc Psychiatry. 2018;57(4):245–251. doi:10.1016/j.jaac.2018.01.016
41. Demmer DH, Puccio F, Stokes MA, McGillivray JA, Hooley M. Influence of child gender on the prospective relationships between parenting and child ADHD. J Abnorm Child Psychol. 2018;46(1):113–125. doi:10.1007/s10802-017-0284-7
42. Xie X-W, Yang W-D. Review of evidence-based treatment guidelines for attention deficit hyperactivity disorder. Chin J Clin Psychol. 2021;29(3):661–664.
43. Daley D, Van Der Oord S, Ferrin M. Practitioner Review: current best practice in the use of parent training and other behavioral interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder. J Child Psychol Psychiatry. 2018;59(9):932–947. doi:10.1111/jcpp.12825
44. Coles EK, Pelham WE, Fabiano GA. Randomized trial of first-line behavioral intervention to reduce need for medication in children with ADHD. J Clin Child Adolesc. 2020;49(5):673–687. doi:10.1016/j.jaac.2019.12.009
45. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–e180. doi:10.1016/S1470-2045(14)71116-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.