Back to Journals » International Journal of Women's Health » Volume 15
Factors Influencing Follicular Output Rate and Follicle-to-Oocyte Index in POSEIDON-Defined Low-Prognosis Women in Vietnam: A Cross-Sectional Study
Authors Le MT , Nguyen ND, Tran NQT, Le DD , Nguyen QHV , Cao TN
Received 1 January 2023
Accepted for publication 24 March 2023
Published 6 April 2023 Volume 2023:15 Pages 523—532
DOI https://doi.org/10.2147/IJWH.S403353
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Minh Tam Le,1,2 Nguyen Dac Nguyen,1,2 Nhu Quynh Thi Tran,1 Duong Dinh Le,3 Quoc Huy Vu Nguyen,2 Thanh Ngoc Cao1,2
1Center for Reproductive Endocrinology and Infertility, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 2Department of Obstetrics and Gynecology, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam; 3Department of Public Health, Hue University of Medicine and Pharmacy, Hue University, Hue, Vietnam
Correspondence: Minh Tam Le, Center for Reproductive Endocrinology and Infertility, Hue University of Medicine and Pharmacy, Hue University, 06 Ngo Quyen street, 53000, Vietnam, Email [email protected]
Objective: This study aimed to identify the factors that influence follicular output rate (FORT) and follicle-to-oocyte index (FOI) among infertile Vietnamese women, as described by the Poseidon classification of poor responders.
Methods: This cross-sectional analysis includes women who received IVF/ICSI treatment at Hue University Hospital, Vietnam, between January 2017 and December 2019. The study population was divided into four groups: Group 1 (age < 35, AFC ≥ 5 and AMH ≥ 1.2 ng/mL, number of oocytes retrieved in the previous cycle ≤ 9), group 2 (age ≥ 35; AFC ≥ 5 and AMH ≥ 1.2 ng/mL, number of oocytes retrieved in the previous cycle ≤ 9), group 3 (age < 35; AFC < 5 and/or AMH < 1.2 ng/mL) and group 4 (age ≥ 35; AFC < 5 and/or AMH < 1.2 ng/mL). All of the patients underwent controlled ovarian stimulation utilizing GnRH antagonist.
Results: A total of 243 cases were recruited into groups 1 (n = 44), 2 (n = 33), 3 (n = 54), and 4 (n = 112). There were statistically significant differences between the four groups in terms of age, infertility type, menstrual cycle, body mass index (BMI) and waist-hip ratio (WHR), endocrine tests, and total retrieved oocytes (p 0.05). The average number of oocytes per participant was 7.27, with the highest number occurring in group 1 (10.77) and the lowest occurring in group 4 (5.59). There was a relationship between FORT and BMI (ß: − 0.146, p=0.039), FSH starting dose (ß: 0.146, p=0.030), and AMH (ß:0.166, p=0.015). No statistically significant correlation was detected between FOI and other variables.
Conclusion: The starting dose of FSH for ovarian stimulation and AMH concentration were positively associated with FORT in individuals with a poor prognosis, whereas BMI was negatively correlated with FORT; No other parameters were found to correlate with FOI.
Keywords: follicular output rate, FORT, follicle-to-oocyte index, FOI, Poseidon, ovarian response
Introduction
Infertility affects 15% of couples of reproductive age, and assisted reproductive technology is widely recognized as an effective treatment for infertile couples who wish to have a healthy child.1 However, 9–25% of infertile patients undergoing in vitro fertilization (IVF) exhibited poor ovarian response (POR).2 Those with a poor response to ovarian stimulation (OS) have a low success rate.3 Due to the repeated treatment cycles, the cost of in-vitro fertilization (IVF) treatment for women with poor ovarian response would be greater than for those with normal ovarian response. Consequently, infertile couples may experience greater anxiety, stress, and financial hardship.4 A meta-analysis in 2022 highlighted the aspect of psychological support for couples undergoing IVF cycles. When approaching fertility treatment, both men and women were more likely to experience psychological problems such as anxiety, depression, and stress.5
With over 40 different definitions of poor responders, the diagnostic criteria for POR remain disputed.6 The Bologna criteria were presented by the European Society for Human Reproduction and Embryology (ESHRE) in 2011 as the first attempt to provide an unified and international definition of poor response.7 However, the Bologna criteria did not take into consideration the different and variable baseline demographics and features of POR.8,9 Despite having normal ovarian features, some normal responders categorized by the Bologna criteria exhibited a suboptimal or unsatisfactory response to controlled ovarian stimulation (COS). Another problem is the vast variety of biomarkers used to classify POR patients: AMH cutoffs of 0.5–1.1 ng/mL and antral follicle count (AFC) cutoffs of 5–7.
To diminish the heterogeneity of the Bologna categorization, the POSEIDON (Patient-Oriented Strategies Encompassing Individualized Oocyte Number) criteria were developed through a joint effort among researchers.9,10 On the basis of ovarian biomarkers, age, and past ovarian response, four groups have been established. The POSEIDON classification distinguishes individuals with a favorable prognosis and normal ovarian reserve from those with a poor prognosis and low ovarian reserve (Groups 1 and 2: AFC > 5 and AMH > 1.2 ng/mL, Groups 3 and 4: AFC 5 and AMH 1.2 ng/mL).9 Hypo-responders are unpredictably poor or suboptimal responders with a low response to FSH stimulation, necessitating greater cumulative FSH dosages.11 (Groups 1 and 2). AFC and AMH are therefore insufficiently reliable for forecasting the response OS.12,13
In recent years, follicular output rate (FORT) has been proposed as a predictor of ovarian response to ovulation and oocyte development. FORT is defined as the ratio of preovulatory follicle count (PFC) on hCG day to small antral follicle count (AFC) at baseline.14,15 In addition, the follicle-to-oocyte index (FOI) may also serve as a quantitative and independent indicator of therapeutic efficacy. The FOI value was derived by dividing the number of oocytes retrieved by the AFC by 100, and FOI values below 50% are regarded as indicative of low ovarian sensitivity.16 In the literature, comparisons of FORT and FOI values between various patient categories indicated by the POSEIDON criteria remained limited, especially from Asian population. The objective of this study was to determine which factors influence the FORT and FOI values of low responders according to POSEIDON stratification.
Materials and Methods
Study Design
This cross-sectional study was conducted between January 2017 and December 2019 at Hue Center for Reproductive Endocrinology and Infertility, Hue University Hospital, Vietnam. Women with both ovaries, no ovarian disorders (such as cysts or endometriomas), and no prior ovarian surgery were included in the study. Cases with polycystic ovary syndrome or more than twenty retrieved oocytes were eliminated. To estimate the sample size for this study, we utilized the conventional sampling approach based on inclusion and exclusion criteria. During the duration of study, a total of 751 cases comprised the sample. We excluded 503 patients with a normal prognosis as well as five cases with insufficient information. Finally, we recruited 243 patients with a poor prognosis according to the Poseidon criteria. The age, clinical history, physical examination, and endocrine testing of every patient were documented. The Hue University of Medicine and Pharmacy Ethics Committee accepted the study with approval number H2021/414. All participants provided their written, informed permission.
The patients’ height and weight were measured. Body mass index (BMI) was calculated by dividing the weight (kilograms) by the square of height (meters). According to the Asian BMI categories, BMI data were categorised as obesity (≥ 25 kg/m2), overweight (23.0–24.9 kg/m2), normal (18.5–22.9 kg/m2), and underweight (<18.5 kg/m2). The AFC was evaluated via a transvaginal ultrasound scan at the beginning of the menstrual cycle (days 1–2) by counting the antral follicles with a diameter greater than 2mm but less than 10mm. Anti-Müllerian hormone [AMH (ng/mL)], luteinizing hormone [LH (mIU/mL)], follicle-stimulating hormone [FSH (mIU/mL)], and estradiol levels [E2 (pg/mL)] were measured using electrochemiluminescence and Elecsys and Cobas E immunoassay analyzers (Cobas 4000/6000, Roche Diagnostics, Indianapolis, IN, USA. All measurements were performed in accordance with the manufacturer’s instructions in the laboratory of Hue University Hospital.
Low Prognosis According to POSEIDON Stratification
Using quantitative and qualitative factors, the POSEIDON criteria categorized individuals with a poor prognosis into four groups. The normal response was classified as cycles with 9 to 20 retrieved oocytes, whereas the low response consisted of cycles with less than 9 recovered oocytes.10 Group 1 (age < 35, AFC ≥ 5 and AMH ≥ 1.2 ng/mL, number of oocytes retrieved in the previous cycle ≤ 9), group 2 (age ≥ 35; AFC ≥ 5 and AMH ≥ 1.2 ng/mL, number of oocytes retrieved in the previous cycle ≤ 9), group 3 (age < 35; AFC < 5 and/or AMH < 1.2 ng/mL) and group 4 (age ≥ 35; AFC < 5 and/or AMH < 1.2 ng/mL).
Controlled Ovarian Stimulation and Oocyte Retrieval
All cases received controlled ovarian stimulation (COS) with a flexible GnRH antagonist strategy and Gonal F® (Merck, Germany) at a starting dose of 225 IU – 450 IU. Cetrotide® 0.25 mg (GnRH antagonist, Merck) was initiated when a follicle reached 14 mm in diameter. Ovitrelle® 250mcg (recombinant human chorionic gonadotropin, Merck, Germany) was injected as soon as 2 preovulatory follicles (16–22 mm in diameter) were seen. Transvaginal ultrasound-guided aspiration was used to recover oocytes 36 hours following hCG injection.
Index Analysis
FORT was calculated by dividing the preovulatory follicle count (PFC) on hCG day by the small antral follicle count at baseline (3–8mm in diameter).17 The FORT value was categorized as low (33rd percentile), medium (33rd-67th percentile), or high (> 67th percentile).14 The FOI value was calculated by dividing the number of retrieved oocytes by the AFC and was classified into two groups: FOI < 0.50 (low ovarian sensitivity) and FOI ≥ 0.50 (normal ovarian sensitivity).18
Statistical Analysis
The characteristics of the study population were evaluated using descriptive statistics. Using the Kolmogorov–Smirnov and Shapiro–Wilk tests, the normal distribution of all parameters was determined. Due to the non-distribution parameters, the Kruskal–Wallis test was applied to compare the differences in variables across the four groups. A Chi-square test was used to assess whether or not category variables are related. If the variable’s sample size was less than 20, the Chi-square test was replaced with the Fisher exact test. Results were presented as odds ratios (ORs) with confidence intervals (CIs) of 95% or two-sided P values. When the p-value is less than 0.05, statistical significance is indicated. All analyses were conducted using version 20.0 of SPSS (IBM Co., Armonk, NY, USA).
Results
Table 1 displays the general characteristics of prognostic categories. The mean age, body mass index, and waist-to-hip ratio were 36.12 years, 20.84 kg/m2, and 0.82, respectively. Age, BMI, and WHR were significantly different across the four groups (p < 0.05). In baseline endocrine and stimulation parameters, baseline FSH, LH, E2, E2 on day hCG, and total retrieved oocytes were substantially different between groups (p < 0.05). In addition, there was a statistically significant difference between infertility type and menstrual cycle (p < 0.05). 130 (53.50%) of the 243 individuals participated in the research had primary infertility, whereas 201 (82.72%) had regular menstrual cycles.
 |
Table 1 Baseline Characteristics of Study Participant Classified by the Poseidon Groups |
Table 2 demonstrates a statistically significant difference (p < 0.001) in the number of recovered oocytes and stimulation response between the four groups. The average number of oocytes was 7.27, with the highest number occurring in group 1 (10.77) and the lowest in group 4. (5.59). 60 individuals (24.7%) exhibited a normal response to stimulation, while 183 patients exhibited an poor response (75.3%). The frequency of patients with normal response was greatest in group 1 (50%) and lowest in group 3 (22.2%). The average FORT and FOI values were 0.86 and 1.10, respectively. There was no significant difference between the four POSEIDON low-prognosis groups in terms of FORT and FOI (p > 0.05).
 |
Table 2 Oocytes Retrieval, FORT and FOI Between the POSEIDON Groups |
When comparing patients in groups 1 and 2, there was a strong correlation between FORT and ovarian response: patients with high FORT retrieved more oocytes than those with medium and low FORT. This difference was not statistically significant (p > 0.05) between the third and fourth groups. As indicated in Table 3, all four groups exhibited a significant association between FOI values and recovered oocytes (p < 0.05).
 |
Table 3 Association Between FORT/FOI and Ovarian Response Between the POSEIDON Groups |
Additionally, Figure 1 displays the FORT values for the POSEIDON groups. Patients in group 1 of POSEIDON had the highest FORT index. In contrast, the proportion of group 4 patients with a low FORT index was the highest. Figure 2 also displayed FOI values in different patient groups. Patients belonging to distinct POSEIDON categories did not differ significantly in terms of FOI characteristics. Figure 3 displays the association between FORT and FOI values in the research population. We found a statistically significant correlation between these two indices (r=0.464; p=0.001).
 |
Figure 1 The FORT value between the POSEIDON groups. |
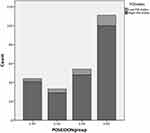 |
Figure 2 The FOI value between the POSEIDON groups. |
 |
Figure 3 The correlation between the FOI and FORT values. |
The factors associated with FORT and FOI are listed in Table 4. In a linear regression analysis, age, BMI, WHR, baseline FSH, the starting dose of FSH, length of OS, type of infertility, and AMH value were included. It was revealed that BMI (ß: −0.146, p=0.039), FSH starting dose (ß: 0.146, p=0.030), and AMH (ß:0.166, p=0.015) were associated with FORT. Regarding FOI value, we found no statistically significant association.
 |
Table 4 Related Factors of Follicular Output Rate and Follicle-to-Oocyte Index |
Discussion
AMH, which is secreted by granulosa cells and plays a role in folliculogenesis, is a frequently used biomarker for ovarian reserve.19,20 It has also been associated with the number of antral follicles at baseline, the outcomes of ART,21 and the age of the female.22,23 Groups 1 and 2 with normal ovarian reserve had significantly more retrieved oocytes and MII oocytes than groups 3 and 4. This difference was statistically significant (Table 1, p < 0.001): the older the women in the groups, the fewer oocytes were retrieved. In addition, there was substantial evidence of a positive correlation between AMH and the number of oocytes retrieved in both people with a low and a high response.12,23 Regardless of COH duration or total FSH dose, another study demonstrated a relation between FORT and AMH levels (r=20.30; p=0.001), indicating a positive relationship.17 Table 4 demonstrates that as AMH increases, so does FORT, and vice versa (B=0.166, p=0.015, Table 4).
In a recently published study, correlations were observed between FORT and AMH levels, AFC, and the number of tiny antral follicles but not between FORT and age, BMI, or baseline endocrine testing.17 Rehman determined that a one-unit rise in FORT will increase the number of recovered oocytes, MII, and fertilized oocytes.16 In addition, both the quality and quantity of embryos were substantially associated with FORT results. There was a correlation between FORT levels and pregnancy rates (64.2% vs 49.3% in pregnant and non-pregnant women, respectively).16 A study of 303 IVF/ICSI patients revealed that clinical pregnancy rates ranged from 29.9%, 43.3% to 57.8% in low, medium, or high FORT groups, respectively. Therefore, FORT was found to be an independent predictor of COS and pregnant outcomes.24 In groups 1 and 2, we identified a positive connection between FORT and the number of oocytes retrieved. Compared to patients with medium and low FORT, those with a high FORT (> 67th) had more oocytes recovered (87.5% vs 57.31% and 31.8% in group 1; 100% vs 66.7% and 11.1% in group 2). Even though the correlation was seen in groups 3 and 4, the difference was not statistically significant. It might be hypothesized that patients with normal ovarian reserve and a suboptimal response to ovarian stimulation could be predicted to require oocyte retrieval using FORT. The number of normal response cases in the abnormal endocrine test groups was insufficient to detect a significant difference in FORT levels between the three groups regarding OS response. To investigate this difference between four groups according to the POSEIDON categorization, a larger sample size is required.
Similar to Genro et al,17 we found that BMI and FSH starting dose were associated with the FORT value, but there was no correlation between FORT and age or baseline FSH. This finding may indicate that antral follicles do not lose their ability to respond to FSH with ovarian age, suggesting that POR in older women is due to a decline in the follicular pool rather than a loss of follicle sensitivity to FSH. According to Chen et al, patients with POR should also be adapted to the OS regimen.25 In our study, there was no variation in the dose of ovarian stimulation between the POSEIDON groups, although there was a difference between the groups with differing FORT outcomes. In distinct POSEIDON patient groups, we did not overregulate ovarian stimulation methods. Although some patients’ prognostic markers of ovarian response were extremely low, we increased the initial dose to the maximum level and prolonged the period of stimulation.
Obesity increases the production of ovarian progesterone and testosterone while decreasing the release of ovarian insulin-like growth factor I (IGF-I), according to a rat study.26 This may explain why the ovarian gonadotropin stimulation is diminished, necessitating higher starting doses.27 However, being overweight or obese has a negative effect on IVF success. Obese women retrieved considerably fewer oocytes and had lower fertilization rates than normal-weight persons.28,29 This has a negative impact on the effectiveness of ovulation induction and the likelihood of pregnancy. In our study, BMI was also found to be negatively connected to FORT value.
In addition, the follicle-to-oocyte index (FOI) may serve as a quantitative and independent measure of therapeutic success.18 This index can be used alone or in conjunction with FORT to measure ovarian OS resistance. According to Chen, who administered a single OS methodology to all patients in the first cycle, the highest 24 FOI values were observed in POSEIDON group 3, followed by POSEIDON group 1, and group 2.8 In this study, we discovered a significant correlation between FOI values and retrieved oocytes in all four groups (p < 0.05): the greatest FOI values were seen in the typical responder groups (> 9 retrieved oocytes). However, there were no differences in FOI among the four POSEIDON groups. Clearly, utilizing POSEIDON could aid in the proper evaluation of POR patients and the development of individualized treatment plans, including the selection of a GnRH analog, gonadotropin type, and gonadotropin dose.
Patients in our study were divided into four groups based on female age, ovarian biomarkers, and past ovarian response history using the POSEIDON criteria. This criterion for selection suggests that the population research is based on a low prediction rather than an actual low response. This should be regarded a limitation when interpreting the present investigation’s conclusions. Another drawback of our study is that it was conducted descriptively cross-sectionally, but not prospectively to track pregnancy outcomes and live birth rates in each research group.
Our study provides the very first information in Vietnam regarding the parameters associated with the FORT and FOI indices and the poor prognosis of IVF patients. In the context of other supportive methods in IVF cycles that proved very limited, such as the use of inositol to improve the number of retrieval oocytes30 or the injection of embryo culture supernatant to the endometrial cavity to improve embryo implantation rates in IVF cycles,31 the control of risk factors that adversely affect the number of oocytes after retrieval is a crucial factor in improving the likelihood of pregnancy in IVF patients.
In conclusion, the initial dose of FSH for ovarian stimulation and AMH concentration exhibited a positive correlation with FORT in persons with a poor prognosis, whereas BMI had a negative correlation with FORT; however, no other parameters were identified to correlate with FOI. This study revealed that it is crucial to control the patient’s weight and alter the initial dose of FSH based on the ovarian response markers to ovarian stimulation. Individualizing the treatment protocol for IVF patients, particularly those with a poor prognosis, will lower the duration of treatment and the patients’ economic, psychological, and financial burden.
Data Sharing Statement
All data are available and submitted upon requests.
Ethics Approval
This study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Hue University (Approval Nr. H2021/414). The present study was conducted in accordance with the Declaration of Helsinki. All information and data were encrypted and confidential. All participants provided informed consent. All samples were handled and processed strictly, as stipulated by an approved local review board protocol.
Consent for Publication
All authors have been involved in the research and have consent for publication.
Acknowledgments
This work was partially supported by Hue University under the Core Research Program (Research Group on Reproductive Medicine, Grant No. NCM.DHH.2022.01). The grantor had no influence on the content of the publication.
Disclosure
The authors have no competing financial or other interests to declare in relation to this manuscript.
References
1. Bablok L, Dziadecki W, Szymusik I, et al. Patterns of infertility in Poland - multicenter study. Neuro Endocrinol Lett. 2011;32(6):799–804.
2. Eftekhar M, Aflatoonian A, Mohammadian F, et al. Adjuvant growth hormone therapy in antagonist protocol in poor responders undergoing assisted reproductive technology. Arch Gynecol Obstet. 2013;287(5):1017–1021. doi:10.1007/s00404-012-2655-1
3. Saldeen P, Källen K, Sundström P. The probability of successful IVF outcome after poor ovarian response*. Acta Obstet Gynecol Scand. 2007;86(4):457–461. doi:10.1080/00016340701194948
4. Esteves SC, Roque M, Bedoschi GM, et al. Defining low prognosis patients undergoing assisted reproductive technology: POSEIDON criteria—the why. Front Endocrinol. 2018;9. doi:10.3389/fendo.2018.00461
5. Burgio S, Polizzi C, Buzzaccarini G, et al. Psychological variables in medically assisted reproduction: a systematic review. Prz Menopauzalny. 2022;21(1):47–63. doi:10.5114/pm.2022.114404
6. Polyzos NP, Devroey P. A systematic review of randomized trials for the treatment of poor ovarian responders: is there any light at the end of the tunnel? Fertil Steril. 2011;96(5):1058–1061.e7. doi:10.1016/j.fertnstert.2011.09.048
7. Busnelli A, Papaleo E, Del Prato D, et al. A retrospective evaluation of prognosis and cost-effectiveness of IVF in poor responders according to the bologna criteria. Hum Reprod. 2015;30(2):315–322. doi:10.1093/humrep/deu319
8. Papathanasiou A. Implementing the ESHRE “poor responder” criteria in research studies: methodological implications. Hum Reprod. 2014;29(9):1835–1838. doi:10.1093/humrep/deu135
9. Alviggi C, Andersen CY, Buehler K, et al; Poseidon Group (Patient-Oriented Strategies Encompassing IndividualizeD Oocyte Number). A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril. 2016;105(6):1452–1453. doi:10.1016/j.fertnstert.2016.02.005
10. Humaidan P, Alviggi C, Fischer R, et al. The novel POSEIDON stratification of “low prognosis patients in assisted reproductive technology” and its proposed marker of a successful outcome. F1000Res. 2016;5:2911. doi:10.12688/f1000research.10382.1
11. Alviggi C, Conforti A, Caprio F, et al. In estimated good prognosis patients could unexpected “hyporesponse” to controlled ovarian stimulation be related to genetic polymorphisms of FSH receptor? Reprod Sci. 2016;23(8):1103–1108. doi:10.1177/1933719116630419
12. Broer SL, van Disseldorp J, Broeze KA, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update. 2013;19(1):26–36. doi:10.1093/humupd/dms041
13. Patrizio P, Vaiarelli A, Levi Setti PE, et al. How to define, diagnose and treat poor responders? Responses from a worldwide survey of IVF clinics. Reprod Biomed Online. 2015;30(6):581–592. doi:10.1016/j.rbmo.2015.03.002
14. Gallot V, Berwanger da Silva AL, Genro V, et al. Antral follicle responsiveness to follicle-stimulating hormone administration assessed by the Follicular Output RaTe (FORT) may predict in vitro fertilization-embryo transfer outcome. Hum Reprod. 2012;27(4):1066–1072. doi:10.1093/humrep/der479
15. Broer SL, Broekmans FJM, Laven JSE, et al. Anti-müllerian hormone: ovarian reserve testing and its potential clinical implications. Hum Reprod Update. 2014;20(5):688–701. doi:10.1093/humupd/dmu020
16. Rehman R, Mustafa R, Baig M, et al. Use of follicular output rate to predict intracytoplasmic sperm injection outcome. Int J Fertil Steril. 2016;10(2):169–174. doi:10.22074/ijfs.2016.4906
17. Genro VK, Grynberg M, Scheffer JB, et al. Serum anti-müllerian hormone levels are negatively related to Follicular Output RaTe (FORT) in normo-cycling women undergoing controlled ovarian hyperstimulation. Hum Reprod. 2011;26(3):671–677. doi:10.1093/humrep/deq361
18. Alviggi C, Conforti A, Esteves SC, et al. Understanding ovarian hypo-response to exogenous gonadotropin in ovarian stimulation and its new proposed marker-the Follicle-To-Oocyte (FOI) index. Front Endocrinol (Lausanne). 2018;9:589. doi:10.3389/fendo.2018.00589
19. Weenen C, Laven JSE, Von Bergh ARM, et al. Anti-müllerian hormone expression pattern in the human ovary: potential implications for initial and cyclic follicle recruitment. Mol Hum Reprod. 2004;10(2):77–83. doi:10.1093/molehr/gah015
20. Tal R, Seifer DB. Ovarian reserve testing: a user’s guide. Am J Obstet Gynecol. 2017;217(2):129–140. doi:10.1016/j.ajog.2017.02.027
21. Jee BC, Ku SY, Suh CS, et al. Serum anti-müllerian hormone and inhibin B levels at ovulation triggering day can predict the number of immature oocytes retrieved in in vitro fertilization cycles. J Korean Med Sci. 2008;23(4):657–661. doi:10.3346/jkms.2008.23.4.657
22. Goswami M, Nikolaou D. Is AMH level, independent of age, a predictor of live birth in IVF? J Hum Reprod Sci. 2017;10(1):24–30. doi:10.4103/jhrs.JHRS_86_16
23. Broer SL, Dólleman M, Opmeer BC, et al. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta-analysis. Hum Reprod Update. 2011;17(1):46–54. doi:10.1093/humupd/dmq034
24. Grynberg M, Labrosse J. Understanding Follicular Output Rate (FORT) and its implications for POSEIDON criteria. Front Endocrinol. 2019;10. doi:10.3389/fendo.2019.00246
25. Chen L, Wang H, Zhou H, et al. Follicular output rate and follicle-to-oocyte index of low prognosis patients according to POSEIDON criteria: a retrospective cohort study of 32,128 treatment cycles. Front Endocrinol. 2020;11. doi:10.3389/fendo.2020.00181
26. Sirotkin AV, Fabian D, Babeľová Kubandová J, et al. Body fat affects mouse reproduction, ovarian hormone release, and response to the follicular stimulating hormone. Reprod Biol. 2018;18(1):5–11. doi:10.1016/j.repbio.2017.12.002
27. Kasum M, Orešković S, Čehić E, et al. The role of female obesity on in vitro fertilization outcomes. Gynaecol Endocrinol. 2018;34(3):184–188. doi:10.1080/09513590.2017.1391209
28. Zhang D, Zhu Y, Gao H, et al. Overweight and obesity negatively affect the outcomes of ovarian stimulation and in vitro fertilization: a cohort study of 2628 Chinese women. Gynaecol Endocrinol. 2010;26(5):325–332. doi:10.3109/09513591003632100
29. Sawal A, Gajbe U, Singh B, et al. Effect of feminine obesity on the outcome of oocyte in subfertile females. IJCRR. 2020:22–24. doi:10.31782/IJCRR.2020.2224
30. Bezerra Espinola MS, Laganà AS, Bilotta G, Gullo G, Aragona C, Unfer V. D-chiro-inositol induces ovulation in non-Polycystic Ovary Syndrome (PCOS), non-insulin-resistant young women, likely by modulating aromatase expression: a report of 2 cases. Am J Case Rep. 2021;7(22):e932722.
31. Prapas Y, Petousis S, Panagiotidis Y, et al. Injection of embryo culture supernatant to the endometrial cavity does not affect outcomes in IVF/ICSI or oocyte donation cycles: a randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):169–173. doi:10.1016/j.ejogrb.2012.03.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
