Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Factors Associated with the Delay in Seeing a Doctor: Evidence of Chinese Middle-Aged and Older Adults
Received 8 October 2023
Accepted for publication 19 December 2023
Published 28 December 2023 Volume 2023:16 Pages 4239—4253
DOI https://doi.org/10.2147/JMDH.S443683
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shangren Qin,1 Xiaoyan Ni,2 Ye Ding3
1School of Public Health, Hangzhou Normal University, Hangzhou, Zhejiang, People’s Republic of China; 2Cangqian Street Community Health Service Center, Hangzhou, Zhejiang, People’s Republic of China; 3School of Public Health, Hangzhou Medical College, Hangzhou, Zhejiang, People’s Republic of China
Correspondence: Ye Ding, School of Public Health, Hangzhou Medical College, 8 Yikang Street, Hangzhou, 311399, People’s Republic of China, Tel +86-571-87692813, Email [email protected]
Background: There have been few studies concerning delayed medical attention among middle-aged and older adults, and in-depth analyses of delay duration and symptoms have been lacking.
Methods: In this cross-sectional study exploiting a face-to-face questionnaire survey, we investigated delays in seeing a doctor among ≥ 45-year-old people in Zhejiang, China over the past year, and analyzed relevant influencing factors through logistics regression.
Results: A total of 1034 people aged ≥ 45 years were enrolled, whose overall occurrence of delay in seeing a doctor was 28.24% (23.00% for older adults aged ≥ 60 years). Factors like the presence of 2 chronic diseases, intense social loneliness, and more health care needs contributed to the occurrence of delay in seeing a doctor (OR (95% CI) = 2.102 (1.252– 3.529); OR (95% CI) = 1.030 (1.002– 1.059); OR (95% CI) = 1.049 (1.002– 1.099). Contrastively, factors like convenient access to medical care and good self-reported health status inhibited such occurrence OR (95% CI) = 0.321 (0.199– 0.519); OR (95% CI) = 0.369 (0.183– 0.745). The foremost reason was wanting to wait and see if the problem would get better on its own (117, 40.07%). Respiratory system disease (14.90%), dental problems (13.82%), and cardiac disease (13.61%) constituted the top 3 types of diseases whose treatments were delayed. Additionally, for the majority of older adults, the delay duration was 1– 2 weeks (99, 33.90%), and the economic burden was the cause of the longest delay in seeing a doctor among middle-aged and older adults.
Conclusion: To alleviate the problem of delay in seeing a doctor among middle-aged and older adults, their families and society should enhance care for them and reduce their sense of social loneliness. Emphasis should be placed by the government on helping middle-aged and older adults with financial difficulties so that their medical convenience can be improved.
Keywords: middle-aged, older adults, delaying doctor visits, China, cross-sectional study
Introduction
China has entered into an aging society and will continue to age rapidly.1 According to China’s seventh national census, older adults aged ≥ 60 accounted for 18.70% of the total population in 2020, among which those aged ≥ 65 represented 13.5%, and life expectancy also increased accordingly.2 The World Bank predicts that by 2050, the proportion of older adults aged ≥ 65 in the total population will reach 26% in China.3 The aging of the population is a major challenge faced by China’s social economy.
The distribution of geriatric medical resources among different regions in China is unbalanced.4 To better match the aging population, region-specific aging security systems and health service industries should be developed by the Chinese government, especially in the western region of China.4 Under limited medical resources, the aging of the population causes failure to meet the medical needs of some older adults in time. For example, since Chinese families mostly have one child, the number of empty-nest elders is increasing.5 The proportion of non-use of healthcare services is higher in empty-nest older adults than that in non-empty-nest ones.6 Moreover, the older adults who received less financial/material support from their children were less likely to seek healthcare treatment.7 The less the older adults use medical services, the more likely they are to delay in seeing a doctor. In addition, the jurisdictions of China’s medical and older adult care services belong to different departments, and the integration of “medical institutions” and “older adult care institutions” is insufficient, so some older adults in retirement homes are unable to see a doctor timely.8 Therefore, it is true that older adults may experience a delay in seeing a doctor.
Delaying treatment may have a negative impact on a patient’s health and the effectiveness of the treatment.9 To reduce the occurrence of delay in seeing a doctor, many scholars have researched it.10,11 Pack and Gallo were the first to propose the concept of delay in seeing a doctor in 1938, which was defined as ≥3 months from the time when a patient first found symptoms to the time when he/she first visited a medical institution.12 Clinically, delay in seeing a doctor is defined as the latency in the process from the onset of symptoms to the acceptance of effective treatment, which comprises 3 parts: patient delay, transport delay, and in-hospital delay.13 Some scholars also define “delay in seeing a doctor” as the phenomenon in which a patient found abnormal physical symptoms in the past year and needed medical treatment, but is delayed due to various reasons.14
Currently, the occurrence status of delay in seeing a doctor has been reported in many studies.15 For example, in the United States, ~6% of disabled older adults delay seeing a doctor because of cost.14 In Vietnam, 49% of breast cancer patients delayed seeking medical attention by at least 3 months from the onset of symptoms.16 In Turkey, 36.1% of patients with non-small-cell lung cancer waited more than 1 month between the symptom onset and the medical attention seeking, with an average delay of 49.9 days. Moreover, 69.4% of them delayed seeing a doctor because they thought their symptoms were not serious and wanted to see if they would get better by themselves.17 During the COVID-19 pandemic, the monthly total outpatient visits of a community hospital in Taiwan declined by 39%, and the visits of older adults (≥80 years) decreased by 44%. In other words, most patients suffer from delayed medical treatment.18
Additionally, the influencing factors of delay in seeing a doctor have also been discussed extensively from the perspectives of Andersen’s behavioral model-related variables,19 disease attributes,20 psychological factors, and cognitive factors.21 Andersen’s behavioral model-related variables have been widely regarded as influencing factors in many studies on health services use.22 The predisposing factors of Andersen’s behavioral model include socio-demographic variables, while the enabling factors refer to resources that can impede or facilitate the use of health services (namely, income, access to health insurance or pension and wealth), and demand factors represent the demand for health care services. Andersen’s behavioral model-related variables are influencing factors of delay in seeing a doctor. For example, in India, senile and male people are more likely to actively seek medical treatment opportunities,23 while in the United States during the COVID-19 pandemic, Caucasian, non-Hispanic, and other groups with higher social status or economic levels slowed down their behavior of seeking medical attention due to more adequate social security benefits.24 Income is a major determinant of whether to see a doctor or not, and financially burdened patients have a longer delay in seeing a doctor.25 Disease attributes affect patients’ medical treatment behavior; for instance, medical demand varies hugely among people with or without congenital illness.26 According to another study, patients often delay seeing a doctor because of psychological factors like “fear of doctors or treatment” and “want to see if the problem will get better by itself”.27 Besides, patients are more likely to delay seeing a doctor if they lack awareness of the diseases.28
Despite the detailed scholarly discussion concerning the status quo and influencing factors of delay in seeing a doctor, extant studies focus mostly on the whole population, while there are limited studies targeting middle-aged and older adults. A majority of published works discuss the occurrence of delay in seeing a doctor for a single disease, while comparative analysis concerning the types of diseases developed by middle-aged and older adults with delayed medical attention is lacking. Moreover, existing studies rarely report information like the number of delayed days.
Hence, this study discusses the occurrence status and influencing factors of “delay in seeing a doctor” in the case of middle-aged and older Chinese in Zhejiang. Further, supplementary analysis is made on key information like causes of delay in seeing a doctor, the number of days delayed, and types of diseases for which seeing a doctor is delayed, to provide a theoretical basis for the government to deal with the dilemma of “failure to fulfill medical needs timely in the context of population aging”.
Methods
Study Design and Data
This study was designed as a cross-sectional survey. Initially, we described the status quo of delay in seeing a doctor among middle-aged and older adults aged ≥45, and compared the differences in the occurrence of such delay among various demographic characteristics through univariate analysis. Next, we explored the influencing factors of delay in seeing a doctor among middle-aged and older adults with a logistic regression model. Finally, we described key information such as the causes of delay in seeing a doctor, the number of days delayed, and the main diseases for which seeing a doctor was delayed.
The questionnaire was designed by the authors themselves. After completion of the questionnaire design, a preliminary survey was conducted, as well as a review by two experts in epidemiology and health statistics, before the formal application of the questionnaire. The questionnaire was filled in face-to-face in paper form. After obtaining the informed consent of each participant, the investigators asked questions and filled in the questionnaire according to the answers of the older adults.
The inclusion criteria of respondents herein were: 1. Permanent residents of Zhejiang, China; 2. Age ≥45 years; 3. Voluntary participation in the survey; 4. Conscious and able to understand and answer questions accurately.
Both probabilistic sampling (eg simple random sampling) and non-probabilistic sampling (eg convenience sampling) were used in this study. Step 1: Through simple random sampling, 4 out of 11 prefecture-level cities in Zhejiang, namely Hangzhou, Shaoxing, Ningbo, and Huzhou, were selected as the cities under survey. Step 2: According to the investigators’ place of domicile or residence, the target county-level cities (districts) were selected from the above 4 prefecture-level cities through convenience sampling, and the investigators were assigned accordingly. Step 3: Through accidental sampling and snowball sampling, investigators were well-trained and conducted a face-to-face questionnaire survey in places with dense middle-aged and older adults (eg morning exercise parks, food markets, hospitals) in county-level cities (districts).
The survey was conducted from June to November 2022, during which a total of 1100 questionnaires were collected. Due to the lack of gender, age, and other key information in some of them, the number of valid questionnaires totaled 1034, with a response rate of 94%. This study complies with the Declaration of Helsinki and was approved by the Ethics Committee of Hangzhou Medical College (Ethics code: LL2022-18). Informed consent was obtained from all subjects involved in the study.
Research Variables and Measures
Delay in Seeing a Doctor (Dependent Variable)
Concerning previous studies,9,14 this survey defined delay in seeing a doctor as the phenomenon in which a patient with medical needs failed to seek medical attention timely in the past year due to subjective or objective reasons.
In the questionnaire, we first asked respondents, “Have you had a time in the past year when you felt you needed to see a doctor, but for some particular reason put it off and had to wait?” If the respondents answered “Yes”, we then asked the following 3 questions: “1. Why did you put off seeing a doctor and wait? Please select the most important reason” “2. How long did you wait then to see a doctor?” “3. What was your main symptom when you went to see the doctor?”
Independent Variables
Initially, the core variables of this study were from Andersen’s behavioral model-related variables,22 which have been widely used in many studies on health services and include predisposing, enabling, and demand factors. Taking into consideration the research contents, the predisposing factors herein included age, gender, hukou, marital status, and educational level. Among them, hukou refers to the information that individuals register according to their type of residence. In China, each person can only register one hukou, which can be classified into urban or rural. Enabling factors included personal monthly income, medical insurance, pension insurance, and the convenience of seeing a doctor at ordinary times. Demand factors included self-reported health status and the number of chronic diseases developed.
Secondly, social support and loneliness have been proven to affect the use of medical services among older adults.29,30 Accordingly, we hypothesized that social support and loneliness would also affect delay in seeing a doctor in older adults, which were thus included as independent variables as well. All of the scales used for measuring social support and loneliness of middle-aged and older adults in this survey were from literature, and have been verified by Chinese scholars.31,32 For older adults to better understand the questions, all the backward questions of the original loneliness scale were adjusted to the forward question. The perceived social support scale was a Likert 7-point one, with a higher total score indicating more social support. The loneliness scale was a Likert 5-point one, with a higher total score indicating a stronger feeling of loneliness.
Finally, the health needs of older adults have been proven to affect their choice preference for medical service types.33 Therefore, we also included the needs of the older adults as independent variables. Concerning Maslow’s hierarchy of needs, we designed a scale to measure the needs of older adults, which had 19 items that were under 5 dimensions of life care, health care, spiritual comfort, security, and rights safeguarding. The need scale adopted Likert 5-point scoring, with a higher total score indicating a higher degree of need.
Reliability and Validity of the Scales
KMO and Bartlett’s test was employed to determine whether the 3 scales were suitable for factor analysis. According to the results detailed in Supplementary Table 1, The KMO values of the 3 scales were all greater than 0.8, while the Bartlett values were all less than 0.001, indicating that factor analysis could be performed on these 3 scales.
As shown by the factor analysis results of the perceived social support scale (Supplementary Table 2), the scale covered 12 items, where 3 factor components could be extracted, with a cumulative contribution rate of 81.91%. These 3 factors were family support, friend support, and other support.
The loneliness scale consisted of 10 items, where 2 factor components could be extracted, with a cumulative contribution rate of 61.01% (Supplementary Table 3). According to the theory proposed by Weiss,34 these 2 factors were called social loneliness and emotional loneliness. Although the specific items of the two factors were a little different from the original Chinese scale,31 the overall validity was acceptable.
As for the need scale, it contained 19 items, where 5 factor components could be extracted, with a cumulative contribution rate of 80.60% (Supplementary Table 4). After generalization and summarization, we named these 5 factors life care needs, health care needs, spiritual comfort needs, security needs, and needs for safeguarding rights.
Next, we measured the reliability of the 3 scales. Their Cronbach α coefficients were all above 0.8, indicating good reliability. In particular, the coefficients of the perceived social support scale were all greater than 0.9, indicating that this scale was highly reliable (Supplementary Table 5).
Statistical Analysis
Initially, we descriptively analyzed the phenomenon of delay in seeing a doctor among the middle-aged and older adults in China. Distribution differences in the occurrence of such delay among various demographic characteristics were compared by the chi-squared test, while the inter-group differences in scale scores were compared by the t-test.
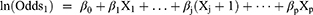
Next, the multicollinearity between independent variables was examined. The results showed that the variance inflation factor (VIF) values were all below 10, indicating the absence of collinearity between independent variables. Thus, we explored the influencing factors of delay in seeing a doctor among middle-aged and older adults with the logistic regression model. The basic model is as follows:
When the probability of an event (eg, people delay in seeing a doctor) happening is π, then 1-π is the probability of that event not happening. The odds of that event are the ratio of two probabilities. β0 is a constant term. β1 … βp are regression coefficients. X1 … Xp are the independent variables.
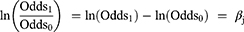
When Xj increases by 1 unit, ln (Odds) changes:
Therefore, OR is got as follows:
Afterward, the R×C chi-squared test and analysis of variance were used to describe the distributions of delay duration and reasons.
Finally, we calculated the constituent ratio of disease symptoms for which seeing a doctor was delayed. In addition, the interrelations between the reasons for the delay, delay duration, and disease symptoms were described by plotting the frequency heatmap.
All of the statistical tests were two-sided, and P <0.05 was considered statistically significant. The statistical software used was R software (version 3.6.3).
Results
A total of 1034 middle-aged and older adults aged ≥45 were enrolled in this survey. More than half of them were females (619, 59.86%), while the dominant age group was 45–59 years (386, 37.33%). The urban population accounted for 57.54% (595). Most of the respondents were married (874, 84.53%), and had a middle school education or below (657, 63.54%).
Current Status of Delay in Seeing a Doctor Among the Middle-Aged and Older Adults
Through the survey, we found that 292 middle-aged and older adults had delayed seeing a doctor in the past year, with an occurrence of 28.24% (Table 1). The occurrence of such delay among older adults ≥60 years was 23.00%.
 |
Table 1 Delay in Seeing a Doctor Among Chinese Middle-Aged and Elderly and Its Influencing Factors (N=1034) |
Age, hukou, and marital status were the predisposing factors in Andersen’s model. In terms of age, the occurrence of delay in seeing a doctor decreased with increasing age (P <0.001), and those aged 45–59 were the most likely to delay seeing a doctor. In terms of hukou, the occurrence of delay in seeing a doctor among the rural group (37.36%) was higher than that among the urban group (21.51%). Regarding marital status, married people were more likely to delay seeing a doctor (29.86%).
Income and the convenience of seeing a doctor were enabling factors in Andersen’s model. Middle-aged and older adults with lower monthly income and no pension insurance were more prone to delay seeing a doctor. Additionally, those who had more convenient access to medical care were less likely to delay seeing a doctor (P <0.001).
The number of chronic diseases developed and self-reported health status were need factors in Andersen’s model. We found that the occurrence of delay in seeing a doctor might rise with the increasing number of chronic diseases (P =0.017), while dropping with the heightening of self-reported health degrees. In other words, people with better self-reported health were less likely to delay seeing a doctor (P <0.001).
The scores of various scale factors also differed somewhat depending on whether seeing a doctor was delayed or not. First of all, the family support and other support scores of the delayed patients were lower than those of the non-delayed patients (P both <0.001). Secondly, compared with the non-delayed group, the delayed group felt stronger social and emotional loneliness (P <0.001, P =0.015). Lastly, the delayed group had more urgent needs for safeguarding rights (P =0.003).
Influencing Factors of Delay in Seeing a Doctor Among the Middle-Aged and Older Adults
In this survey, the correlations of various factors with delay in seeing a doctor were analyzed through logistics regression, and the results are listed in Table 1.
We found that middle-aged and older adults with convenient access to medical care were less likely to delay seeing a doctor than those with inconvenient access to medical care (OR (95% CI) =0.321 (0.199–0.519), P <0.001). The probability of delay in seeing a doctor among middle-aged and older adults suffering from 2 chronic diseases was 2.102 times that of those without chronic diseases (95% CI =1.252–3.529), suggesting that people having more chronic diseases were more likely to delay seeing a doctor. Besides, middle-aged and older adults with self-reported good health were less prone to delay seeing a doctor than those with self-reported poor health (OR (95% CI) =0.369 (0.183–0.745), P =0.005).
Additionally, social loneliness, life care needs, and health care needs were associated with delay in seeing a doctor. Middle-aged and older adults with stronger social loneliness and more health care needs exhibited higher probabilities of delay in seeing a doctor (OR (95% CI) =1.030 (1.002–1.059); OR (95% CI) =1.049 (1.002–1.099). Contrastively, those with stronger life care needs were less prone to delay seeing a doctor (OR (95% CI) = 0.957 (0.926–0.989)).
However, we found no association between sociodemographic characteristics (age, gender, marital status, etc.) and economic factors (income, health insurance, pension insurance, etc.) with delay in seeing a doctor.
Reasons for Delay in Seeing a Doctor Among the Middle-Aged and Older Adults
A total of 292 older adults who had delayed seeing a doctor in the past year answered the major reasons for their delayed medical attention. The reasons, in descending order of ratio, were as follows: Want to wait and see if the problem will get better on its own (117, 40.07%); Could not take time to see a doctor due to work, childcare or other reasons (57, 19.52%); Waiting too long for outpatient service/hospitalization (47, 16.10%); Could not afford to attend (39, 13.36%); No means of transportation or the hospital is too far away (22, 7.53%); Fear of doctors/treatment (10, 3.42%).
Figure 1 presents the descriptive results of the reasons for the delay in seeing a doctor. Middle-aged and older adults aged 45–59, with urban hukou, college education or above, and pension insurance were more prone to delay seeing a doctor because they “Could not take time to see a doctor” (28.26%, 28.13%, 37.50% and 22.78%). Among those who reported “monthly income <1000 yuan”, 41.67% delayed seeing a doctor because they “Could not afford it”. Meanwhile, those who usually had convenient access to medical care delayed seeing a doctor because they “Want to wait and see if the problem will get better on its own” (50.00%). Besides, we also found that those who chose “No means of transportation or the hospital is too far away” had lower needs in all the aforementioned 5 dimensions than others (Figure 1D).
The Delay Time in Seeing a Doctor Among the Middle-Aged and Older Adults
The interviewed middle-aged and older adults also responded to the delay time in seeing a doctor. The selection proportions of four time periods were 1–2 weeks (N=99, 33.90%), < 1 week (N=82, 28.08%), >4 weeks (N=78, 26.71%), and 3–4 weeks (N=33, 11.30%) from the highest to the lowest proportions.
The description results of the delay time are shown in Figure 2. As observed, there was no significant difference in the distribution of delay time among various factors. However, we discovered that the delay time of middle-aged and older adults with a monthly income < Ұ1000 seemed to be longer than that in other populations. Moreover, populations with a delay time > 4 weeks, had stronger needs from different aspects (Figure 2D).
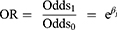
Major Disease Symptoms of Middle-Aged and Older Adults with Delay in Seeing a Doctor
The major disease symptoms of middle-aged and older adults with delays in seeing a doctor are presented in Figure 3. According to the selection proportions, the top five diseases from the highest to lowest proportions were 1. Respiratory system disease (14.90%), 2. Dental problems (13.82%), 3. Cardiac disease (13.61%), 4. Digestive system disease (11.66%), and 5. Endocrine system disease (10.37%).
 |
Figure 3 The major disease symptoms for delay in seeing a doctor. |
Interrelations Among Reasons for the Delay, Delay Time, and Disease Symptoms
To understand the pairwise interrelations among reasons for the delay, delay time, and disease symptoms, the frequency heat map was plotted, where the heat degree (shade of color) represents the magnitude of frequency. The interrelations between the two variables were analyzed by observing the heat degrees of different dimensions.
Figure 4A shows the frequency heat map for the interrelation between the reasons for delay and disease symptoms. We discovered that diseases related to delay in seeing a doctor due to “Want to wait and see if the problem will get better on its own” were mostly respiratory system diseases, dental problems, and cardiac diseases.
Figure 4B displays the frequency heat map for the interrelation between delay time and disease symptoms. The results indicated that the diseases related to delay time > 4 weeks were mostly digestive system diseases, dental problems, and cardiac diseases. The delay time of respiratory system disease was relatively short, mostly < 1 week or 1–2 weeks. The delay time of dental problems was mostly distributed at both extremes, mainly < 1 week or > 4 weeks.
Figure 4C presents the frequency heat map for the interrelation between reasons for the delay and delay time. According to our results, the delay time in seeing a doctor due to “Could not afford” was mostly > 4 weeks, while that due to “Could not take time to see a doctor” and “Waiting too long for outpatient service/ hospitalization” was mostly < 1 week or 1–2 weeks.
Discussion
This study explored the occurrence of delay in seeing a doctor and its influencing factors among Chinese middle-aged and older adults, and supplemented important information such as reasons for the delay in seeing a doctor, delay time and major disease symptoms among middle-aged and older adults.
Current Situation of Delay in Seeing a Doctor Among the Middle-Aged and Older Adults
As discovered in this survey, the occurrence of delay in seeing a doctor among middle-aged and older adults was 28.24%, of which, that in the older adults aged ≥ 60 years was 23.00%. In addition, the occurrence of “Unmet Healthcare Needs” among Malaysians aged ≥ 60 years in the past year was 6.6%,35 while that among Koreans aged ≥ 65 years was 17.4%.36 The “Unmet Healthcare Needs” mentioned in the aforementioned two studies included two parts, namely, “needed care was never received” and “needed care was received at a later time”. In other words, the occurrence rates of delay in seeing a doctor in the last year among Malaysians aged ≥ 60 years and Koreans aged ≥ 65 years are lower than the literature reports (<6.6% and <17.4%). Furthermore, in the USA, 11.69% of people aged ≥ 65 years had a delay in seeing a doctor.30 Thus, the occurrence of delays in seeing a doctor among middle-aged and older Chinese people is higher than that in other countries.
Influencing Factors for Delay in Seeing a Doctor Among the Middle-Aged and Older Adults
As pointed out in the literature, middle-aged and older adults aged 45–59 years are the high-risk population of “not seeing a doctor when ill”.27 Although our univariate analysis results verified that the middle-aged population of 45–59 years had the highest occurrence of delay in seeing a doctor, multivariate analysis results revealed no statistical significance of age. In addition, some literature also suggests that women are the high-risk population for the delay in seeing a doctor,37,38 but no consistent results were obtained in this study.
Further, our logistic regression results also demonstrated that, compared with the population with inconvenient access to medical services, the phenomenon of delay in seeing a doctor was rare in the middle-aged and older adults with convenient access to medical services. Such results are similar to some existing studies.39 This indicates that poor transportation is significantly related to delays in seeing a doctor. Therefore, transportation convenience should be taken into consideration by the government when improving medical service accessibility.
Additionally, as suggested by our results, middle-aged and older adults with more chronic diseases, poorer self-reported health conditions, and more healthcare needs were more likely to have a delay in seeing a doctor. It is also reported in other studies that, when the self-reported health condition decreases by 4.5% among older adults, the probability of “unmet healthcare needs” increases by 1%.40
In addition, we also discovered in our survey that, middle-aged and older adults with stronger needs for life care had less delay in seeing a doctor. Specifically, life care in this survey included the needs for housework, catering, and assistance with showers and haircuts. We speculate that these older adults with stronger needs are being taken care of by specially assigned persons or professional institutions. Therefore, when they are sick, the care provider can go with them to see a doctor, thereby leading to a lower occurrence of delay in seeing a doctor.
Reason Distribution, Disease Symptoms and Delay Time in Seeing a Doctor Among Middle-Aged and Older Adults
This paper investigated the reason distribution, delay time, and disease symptoms related to delay in seeing a doctor among middle-aged and older adults. As a result, the most frequently selected reason was “Want to wait and see if the problem will get better on its own”. This suggests that more efforts should be made to improve health knowledge and health literacy among middle-aged and older adults since sufficient health knowledge contributes to promoting the judgment of disease severity by older adults, and good health literacy helps to promote the formation of healthy behaviors among them (like seeing a doctor in time).41 Additionally, as found by Korean scholars, the low-income population usually has “unmet healthcare needs” due to the costs, while the younger population may have “unmet healthcare needs” due to being “too busy”,42 consistent with our results.
Among the most frequently selected diseases related to delay in seeing a doctor in this paper, the top three types were respiratory system disease (14.90%), dental problems (13.82%), and cardiac disease (13.61%). In these three types of diseases, cardiac disease has an occult onset and is easily neglected.43 For instance, the symptom of painless myocardial infarction manifests as sudden chest pain, which can induce cardiac shock within a short period if not treated timely, thus causing irreversible injury. Therefore, the government should attach great importance to health education on various diseases for middle-aged and older adults, especially cardiovascular diseases. Educators should inform middle-aged and older adults of the necessity of seeing a doctor in time if any cardiovascular symptom occurs, to avoid missing the optimal treatment time.
Combined with disease cause analysis, we discovered that the delay time in seeing a doctor was frequently > 4 weeks due to economic causes. It indicates that economic pressure is the reason for the longest delay time in seeing a doctor among middle-aged and older adults. However, different from subjective reasons (like “want to wait”), such objective reasons (economic pressure) can be solved within a short time. The government may specifically support such people with delays in seeing a doctor due to economic pressure, and good achievements can be made.
Strengths and Drawbacks
The strengths of this paper are as follows. 1. The research population was Chinese middle-aged and older adults. At present, research regarding the delay in seeing a doctor among Chinese middle-aged and older adults is lacking. Consequently, the research population in this study is innovative. 2. The research contents included information like delay time and cause of delay. Noteworthily, this paper also summarized the disease symptom information of all cases with delay in seeing a doctor, which is distinct from the currently published research on delay in seeing a doctor related to multiple single diseases.
Nonetheless, certain limitations should be noted in this work. 1. This was a cross-sectional study, which was associated with restricted causal inference ability. 2. We collected information about the delay in seeing a doctor from the respondents depending on their memory within the last year, which might have recall bias. 3. We only investigated the occurrence of delay in seeing a doctor among middle-aged and older adults in the past year but did not analyze the times of delay in seeing a doctor in the last year, which should be further supplemented in future studies. 4. Both probabilistic sampling and non-probabilistic sampling were used in this study. Non-probabilistic sampling might raise biases.
Conclusion
This paper conducted a questionnaire survey to explore the occurrence of delays in seeing a doctor among middle-aged and older adults in Zhejiang Province, China, as well as the influencing factors. Besides, our results supplemented information like delay time, cause of delay, and disease symptoms. According to our results, the occurrence rate of delay in seeing a doctor among middle-aged and older adults aged ≥ 45 years was 28.24%, while that in the older adults aged ≥ 60 years was 23.00%. Factors like the experience of multiple chronic diseases, strong social loneliness, and more health care needs promoted the occurrence of delay in seeing a doctor. By contrast, factors including convenient access to medical services and good self-reported physical condition suppressed the occurrence of delays in seeing a doctor. The most common reason for the delay in seeing a doctor among middle-aged and older adults was “Want to wait and see if the problem will get better on its own”. Meanwhile, the top three diseases related to delay in seeing a doctor were respiratory system disease, dental problems, and cardiac disease. Moreover, the delay time was mostly 1–2 weeks among the older adults, while economic pressure was the reason why middle-aged and older adults delayed seeing a doctor the longest.
From the theoretical perspective, this paper supplements the analysis of delay in seeing a doctor among Chinese middle-aged and older adults based on the existing research and adds the disease symptoms related to delay in seeing a doctor. At the application level, this paper suggests that 1. The family and the society should strengthen their care of middle-aged and older adults, and reduce their social loneliness. 2. Related health agencies should reinforce health education of disease knowledge and medical guidance for middle-aged and older adults, especially for cardiovascular diseases. 3. The government should improve access to medical services, for instance, attach importance to convenient transportation and increase medical facilities suitable for older adults. 4. The government may provide key support to middle-aged and older adults with economic hardship, pay attention to their healthcare needs, and improve their access to medical services.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study complies with the Declaration of Helsinki and was approved by the Ethics Committee of Hangzhou Medical College (Ethics code: LL2022-18). Informed consent was obtained from all subjects involved in the study.
Acknowledgments
We would like to thank all the investigators who helped us with the survey.
Funding
This study was funded by General Project of the Department of Education of Zhejiang Province [grant number: Y202249243], Basic Scientific Research Funds of Department of Education of Zhejiang Province [grant number: KYQN202206] and Hangzhou High-Level Talent Special Support Project [grant number: 4265C50622026]. The financial sponsor played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Disclosure
The authors declare that they have no competing interests.
References
1. Wang H, Chen H. Aging in China: challenges and opportunities. China CDC Wkly. 2022;4(27):601–602. doi:10.46234/ccdcw2022.130
2. National Bureau of Statistics. Report of the seventh population census data in China. Available from: http://www.stats.gov.cn/tjsj/zxfb/202105/t20210510_1817176.html.
3. World Bank. World bank report offers options for elderly care in China. Available from: https://www.worldbank.org/en/news/press-release/2018/12/13/world-bank-report-offers-options-for-elderly-care-in-china.
4. Wang Z, Ye W, Chen X, et al. Spatio-temporal pattern, matching level and prediction of ageing and medical resources in China. BMC Public Health. 2023;23(1):1155. doi:10.1186/s12889-023-15945-9
5. Zhang Y. Are empty-nest elders unhappy? Re-examining Chinese empty-nest elders’ subjective well-being considering social changes. Front Psychol. 2020;11:885. doi:10.3389/fpsyg.2020.00885
6. Zhou C, Ji C, Chu J, et al. Non-use of health care service among empty-nest elderly in Shandong, China: a cross-sectional study. BMC Health Serv Res. 2015;15(1):294. doi:10.1186/s12913-015-0974-1
7. Wen C, Zhang Q. The role of intergenerational support in shaping oral healthcare-seeking behavior among older adults in China. Front Public Health. 2023;11:1234539. doi:10.3389/fpubh.2023.1234539
8. Chen Z, Yu J, Song Y, Chui D. Aging Beijing: challenges and strategies of health care for the elderly. Ageing Res Rev. 2010;9(Suppl 1):S2–S5. doi:10.1016/j.arr.2010.07.001
9. Smith S, Connolly S. Re-thinking unmet need for health care: introducing a dynamic perspective. Health Econ Policy Law. 2020;15(4):440–457. doi:10.1017/S1744133119000161
10. Liu K, Ge R, Luo D, et al. Delay analysis of pulmonary tuberculosis in the eastern coastal county of China from 2010 to 2021: evidence from two surveillance systems. Front Public Health. 2023;11:1233637. doi:10.3389/fpubh.2023.1233637
11. Wang X, Li Y, Fu Q, Zhou M. Trends of a decade in risk factors of patient delay among pulmonary tuberculosis patients during fast aging and urbanization - analysis of surveillance data from 2008 to 2017 in Wuhan, China. BMC Public Health. 2023;23(1):803. doi:10.1186/s12889-023-15707-7
12. Pack GT, Gallo JS. The culpability for delay in the treatment of cancer. Am J Cancer. 1938;33(3):443–462.
13. Li J, Zhao Q, Liu X, Wu Y. Analysis of the current research situation on pre-hospital delay of patients with acute myocardial infarction. J Nurs Adm. 2012;12(2):3.
14. Lee JC, Hasnain-Wynia R, Lau DT. Delay in seeing a doctor due to cost: disparity between older adults with and without disabilities in the United States. Health Serv Res. 2012;47(2):698–720. doi:10.1111/j.1475-6773.2011.01346.x
15. Lee JS, Lee JY, Kim YD, Song JM, Choi WH. Primary repair of untreated cleft palate in an elderly patient: a case report. J Korean Assoc Oral Maxillofac Surg. 2021;47(1):47–50. doi:10.5125/jkaoms.2021.47.1.47
16. Nguyen SM, Nguyen QT, Nguyen LM, et al. Delay in the diagnosis and treatment of breast cancer in Vietnam. Cancer Med. 2021;10(21):7683–7691. doi:10.1002/cam4.4244
17. Yurdakul AS, Kocaturk C, Bayiz H, et al. Patient and physician delay in the diagnosis and treatment of non-small cell lung cancer in Turkey. Cancer Epidemiol. 2015;39(2):216–221. doi:10.1016/j.canep.2014.12.015
18. Jeng Y, Chen FH, Jen GH, et al. Impact of COVID-19 pandemic on accessibility of Taiwanese medical care. Am J Manag Care. 2021;27(9):e330–e335.
19. Hosseini SS, Rejali M, Kheirabadi GR, Aliyari R. Predictive factors of delay in contact with a psychiatrist in depressive disorders: a sample of Iranian patients. Int J Prev Med. 2014;5(3):360–364.
20. Wu X, Chen C, Chao X, et al. Status of pre-hospital delay and influencing factors of delay time in patients with colorectal cancer. Chin General Pract. 2017;20(33):4109–4114.
21. Xu Y, Wang X, Li H, Jiang Q. Status quo and its influencing factors of social alienation in elderly patients with chronic obstructive pulmonary disease. Nurs J Chin People’s Liberat Army. 2021;38(04):41–44.
22. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi:10.2307/2137284
23. Barman D, Mishra M. How does eye care seeking behaviour change with increasing age and visual impairment? Intersectional analysis of older adults in the Indian Sundarbans. BMC Geriatr. 2020;20(1):71. doi:10.1186/s12877-020-1438-y
24. Callison K, Ward J. Associations between individual demographic characteristics and involuntary health care delays as a result of COVID-19. Health Aff. 2021;40(5):837–843. doi:10.1377/hlthaff.2021.00101
25. Kurichi JE, Pezzin L, Streim JE, et al. Perceived barriers to healthcare and receipt of recommended medical care among elderly Medicare beneficiaries. Arch Gerontol Geriatr. 2017;72:45–51. doi:10.1016/j.archger.2017.05.007
26. Prokup JA, Andridge R, Havercamp SM, Yang EA. Health care disparities of Ohioans with developmental disabilities across the lifespan. Ann Fam Med. 2017;15(5):471–474. doi:10.1370/afm.2108
27. Qin S, Ding Y. Why not see a doctor when ill? Evidence from the Chinese elderly. BMC Health Serv Res. 2019;19(1):365. doi:10.1186/s12913-019-4212-0
28. Qian H, Zhou L, Sun Y, Qian Y, Hu S. Status of the delayed medical behavior, disease cognition and self-efficacy among patients with osteonecrosis of the femoral head. Nurs J Chin People’s Liberat Army. 2016;33(22):12–16.
29. Aierken A, Ding X, Pan Y, Chen Y, Li Y. Association between dependency on community resources and social support among elderly people living in rural areas in China: a cross-sectional study. BMC Geriatr. 2022;22(1):589. doi:10.1186/s12877-022-03247-5
30. Zhang J, Xu L, Li J, et al. Loneliness and health service utilization among the rural elderly in Shandong, China: a cross-sectional study. Int J Environ Res Public Health. 2018;15(7):1468.
31. Su SW. Study on the Relationship Between Social Support, Loneliness and Health of Chinese Older Adults Under Different Aged Care Models [doctorate]. Southern Medical University; 2019.
32. Chen W, Lu C, Yang XX, Zhang JF. Multivariate generalization analysis of social support scale. Psychol Explorat. 2016;36(01):75–78.
33. Rodwell J. Health need factors are the key drivers of hospitalization among the elderly living alone: an analysis of longitudinal data. Int J Environ Res Public Health. 2022;19(22):15315. doi:10.3390/ijerph192215315
34. Weiss R. Loneliness: The Experience of Emotional and Social Isolation. MIT press; 1975.
35. Shah SA, Safian N, Ahmad S, et al. Unmet healthcare needs among elderly Malaysians. J Multidiscip Healthc. 2021;14:2931–2940. doi:10.2147/JMDH.S326209
36. Kim YS, Lee J, Moon Y, et al. Unmet healthcare needs of elderly people in Korea. BMC Geriatr. 2018;18(1):98. doi:10.1186/s12877-018-0786-3
37. Yamada T, Chen CC, Murata C, et al. Access disparity and health inequality of the elderly: unmet needs and delayed healthcare. Int J Environ Res Public Health. 2015;12(2):1745–1772. doi:10.3390/ijerph120201745
38. Ahn YH, Kim NH, Kim CB, Ham OK. Factors affecting unmet healthcare needs of older people in Korea. Int Nurs Rev. 2013;60(4):510–519. doi:10.1111/inr.12055
39. Choi Y, Nam K, Kim CY. Association between convenience of transportation and unmet healthcare needs of rural elderly in Korea. J Prev Med Public Health. 2019;52(6):355–365. doi:10.3961/jpmph.19.172
40. Ko H. Unmet healthcare needs and health status: panel evidence from Korea. Health Policy. 2016;120(6):646–653. doi:10.1016/j.healthpol.2016.04.005
41. Liu YB, Liu L, Li YF, Chen YL. Relationship between health literacy, health-related behaviors and health status: a Survey of Elderly Chinese. Int J Environ Res Public Health. 2015;12(8):9714–9725. doi:10.3390/ijerph120809714
42. Hwang J. Understanding reasons for unmet health care needs in Korea: what are health policy implications? BMC Health Serv Res. 2018;18(1):557. doi:10.1186/s12913-018-3369-2
43. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.