Back to Journals » Patient Preference and Adherence » Volume 17
Factors Associated with Patient Trust in the Pharmacy Team: Findings from a Mixed Method Study Involving Patients with Asthma & COPD
Authors te Paske R , van Dijk L , Yilmaz S, Linn AJ, van Boven JFM , Vervloet M
Received 9 August 2023
Accepted for publication 5 December 2023
Published 14 December 2023 Volume 2023:17 Pages 3391—3401
DOI https://doi.org/10.2147/PPA.S429969
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Roland te Paske,1,2 Liset van Dijk,1,2 Selina Yilmaz,2 Annemiek J Linn,3 Job FM van Boven,4 Marcia Vervloet1
1Department of Healthcare from the Perspective of Patients, Clients and Citizens, Nivel (Netherlands Institute for Health Services Research), Utrecht, the Netherlands; 2Groningen Research Institute of Pharmacy, Unit of Pharmacotherapy, - Epidemiology & -Economics, University of Groningen, Groningen, the Netherlands; 3Amsterdam School of Communication Research, University of Amsterdam, Amsterdam, the Netherlands; 4Department of Clinical Pharmacy & Pharmacology, Groningen Research Institute for Asthma and COPD (GRIAC), University Medical Center Groningen, University of Groningen, Groningen, the Netherlands
Correspondence: Roland te Paske, Department of Health care from the perspective of Patients, Clients and Citizens, Nivel (Netherlands Institute for Health Services Research, Postbus 1568 (PO box), 3500 BN, Utrecht, the Netherlands, Email [email protected]
Purpose: The pharmacy team has been shifting its role from primarily dispensing medications to providing patient-centred pharmaceutical care. Establishing a trust relation between the pharmacy team and their patients is fundamental for this new role. This study aimed to (i) identify the level of trust in the pharmacy team among patients with asthma and/or COPD, (ii) assess whether the level of trust patients have in pharmacists differs from their trust in pharmacy technicians, and (iii) identify factors that contribute to building trust in the pharmacy team.
Patients and Methods: First, a focus group with six patients with asthma and/or COPD was conducted to explore which aspects they considered significant for establishing trust in the pharmacy team. Subsequently, these insights were used to develop an online questionnaire. A link to the online questionnaire was distributed among patients with asthma and/or COPD. Data were analysed using exploratory factor analyses to identify underlying constructs for trust. Regression analyses were conducted to evaluate whether these constructs affected trust (scale 1– 10) in the pharmacy team.
Results: A total of 290 patients completed the questionnaire. On average, they rated their trust in the pharmacy team with a score of 7.4 out of 10 (SD: 1.5), almost identical to their trust in the pharmacist and pharmacy technician. Patient trust in pharmacy teams is influenced by their perception of engagement, expertise in medication-related matters, and effective communication.
Conclusion: Trust in the pharmacy team was observed as moderately high, indicating that there is room for improvement. Due to the changing role of the pharmacy team, its members should strive to enhance their patient-centred skills ensuring ongoing efforts to build and maintain trust with patients.
Keywords: trust in pharmacy team, pharmacy team’s engagement, pharmacist expertise, information and communication, patient-centred interaction, community pharmacy
Introduction
Pharmacy teams play a crucial role in offering support and educating patients on the optimal use of their medication.1,2 To be fully effective, the pharmacy team needs to rely on the trust of their patients. Trust, in general, serves as a prerequisite for patients to utilize the information provided by healthcare providers.3 Notably, the pharmacy should be a welcoming environment where patients feel comfortable asking questions about medication, share any medication-related concerns, and receive support for medication adherence.2,4 With this ethos in mind, there has been a notable shift within the community pharmacy team’s focus – moving away from a product-oriented approach towards a patient-centred one combined with offering cognitive pharmaceutical services.5 This shift places significant emphasis on patient education and counselling, recognizing this as integral components of the pharmacy’s mission. This changing role does not necessarily lead to an increase in trust. In the Netherlands, the percentage of patients who place trust in the pharmacy has gradually declined from 91% in 2008 to 83% in 2022.6 This decrease may indicate an underestimation of the pharmacy’s crucial patient-oriented role, potentially hampering the effectiveness of patient counselling by the pharmacy team.7–9 The general public may not be aware of this shift of the community pharmacy team’s focus and to some extent not yet be aware of what they can expect from the pharmacy team regarding patient-centred healthcare.7
In the Netherlands, the pharmacy team consists of both pharmacists and pharmacy technicians (PTs). The pharmacist serves as the medication-expert and provides pharmaceutical patientcare while the PT plays a vital role as point of contact within the pharmacy and provides medication education and counselling to patients. The role of the PT is evolving and expanding.10 Whether the pharmacist and PT are equally trusted by patients for their contributions, is however still unclear. Hitherto, a few studies have specifically focussed on trust patients have in the role of the pharmacy team as healthcare provider and they were primarily focused on a general patient population. Factors that were found to bolster patient trust in the pharmacy were communication-related factors,11 ethical principles and professionalism, such as confidentiality,12 and accessibility, affability, acknowledgement and respect.13 Also, patients’ perception of pharmacists’ communication and technical competences were identified as key components for building trust.14
These previous studies show that trust plays an important role in providing effective medication education. It can be argued that trust is particularly valuable when it comes to providing education regarding medication with more complex administration routes, such as inhaled medication. Proper use of inhaled medication remains an ongoing challenge for many patients with asthma and/or COPD and its improper use is associated with worse clinical and economic outcomes.15–18 Former studies showed that community pharmacies are well-equipped to deliver educational services to patients with asthma,19 and to patients with COPD.20 For the pharmacy team to optimally provide these services, trust is paramount. Also because high trust is associated with improving patients’ medication adherence.21,22
To our knowledge, there is a lack of understanding regarding the level of trust in the pharmacy team among patients with asthma and/or COPD, and whether their trust varies between pharmacists and PTs. This study therefore aims to (1) examine to what extent patients with asthma and/or COPD have trust in the pharmacy team, (2) whether trust differs between pharmacists and PTs, and (3) identify which factors contribute to trust in the pharmacy team.
Materials and Methods
Study Design
We used a mixed method study. Recognising the absence of existing measurement tools for these constructs, first a focus group (FG) was convened to guide the development of items capable of measuring trust and its associated factors. In the FG, patients with asthma and/or COPD were asked to elaborate on their views on pharmacy team members in their role as healthcare providers, the trust they have in the pharmacy team as well as which aspects they identify as important for trust.
Participant Recruitment for the Focus Group
Patients were invited to participate in the FG through a newsletter sent by the Dutch Lung Foundation, the major patient organization for patients with lung diseases. Inclusion criteria were that respondents were 18 years or older, had asthma and/or COPD and used inhaled medication. Patients were not eligible to participate in the FG if they were not able to join the online FG. Patients who expressed interest to participate in the FG via email were randomly selected to participate.
Data Collection of the Focus Group
Data were collected through a non-sequential online FG. Due to the global pandemic, the FG was conducted virtually using the Zoom platform and was recorded for analyses purposes. The FG was transcribed verbatim. Only the participants and researchers (one moderator; SY, and one co-moderator/note-taker/observant; RtP) were present during the FG. RtP has had extensive training on how to conduct FG properly, with plenty of experience. RtP supervised SY, to facilitate proper conduct of the FG discussion. RtP and SY prepared the FG together and discussed ground rules. The FG discussion took place on December 9, 2020, and took approximately one hour. Field notes were taken during the FG.
Content of the Focus Groups
A topic guide was developed in order to structure the FG, based on literature on trust and on pharmaceutical care for patients with asthma and COPD.11–14 The FG focussed on exploring participants’ trust in the pharmacy team, how the participants viewed the position of the pharmacy team regarding inhaled medication care, and the engagement of the pharmacy team in the participants’ medication use.
Focus Group Data Analysis
The transcript from the FG was coded individually and independently by RtP and MV using MaxQDA 2022. To ensure that the questionnaire items were rooted in the insights and themes extracted from qualitative data, a thematic analysis approach was adopted. The method entails, after becoming acquainted with the data, assigning meaningful codes to relevant segments of the transcripts. These codes were either inductively or deductively (based on the topic list) formulated. The codes were then used to construct the coding tree. Using the coding tree, the codes from the manuscript were then organised into themes, which consequently resulted into the development of the items of the questionnaire. A translated version of the coding tree can be found in Supplementary Figure 1.
Questionnaire
Based on the themes identified in the FG combined with input from relevant literature, an online questionnaire was developed to evaluate among a larger cohort of patients with asthma and/or COPD the level of trust in the pharmacy team, as well as the factors affecting trust. Respondents were informed of the aim of the study and asked to provide consent before they were able to start the questionnaire.
Data Collection
Data were collected over a six-week period in March and April 2021. Patient recruitment occurred through multiple channels. First, a direct invitation with a link to the questionnaire was sent to 247 ex-members of the National Panel of the Chronically Ill and Disabled (NPCD) from Nivel (Netherlands Institute for Health Services Research) via email.23 Second, an link to the questionnaire was included in a digital newsletter that was sent to members of the Dutch Lung Foundation, reaching approximately 1450 patients with lung diseases. Third, invitations, including the link to the questionnaire, were disseminated through various social media channels. Following a two-week period, email reminders were sent to both the members of NPCD and the Dutch Lung Foundation. Inclusion criteria were 1) that respondents used inhaled medication and 2) they were 18 years or older. No exclusion criteria were specified.
Measurements
The questionnaire included inquiries about respondents’ demographics, such as age, sex, education, employment status, and native language. Additionally, respondents were asked to provide health-related information, including their general health rating, presence of asthma and/or COPD, and the duration of inhaled medication use.
Trust
Respondents were requested to rate their trust on a scale ranging from 1 (minimal trust) to 10 (maximum trust) in the pharmacy team, the pharmacist, the PT, their inhaled medication, medication in general, their general practitioner (GP), and healthcare in general.
Factors Influencing Trust in the Pharmacy
The five main themes in the FG were: (i) expertise of the pharmacy team, (ii) personal relationship with the pharmacy, (iii) pharmacy team’s attention for patients / their engagement in patients’ medication use, (iv) communication with the pharmacy and (v) role of the pharmacy. More extensive details of the FG results are presented in the Results section. Based on these themes, five matrix questions were formulated to examine the factors influencing trust in the pharmacy team. These matrices encompassed a total of 39 sub-items. Participants rated their agreement with these items on a scale ranging from “totally disagree” (1 = minimum) to “totally agree” (5 = maximum). A translated list of the items featured in this study can be found in the Supplementary Tables 1–6.
Questionnaire Data Analysis
Data were analysed using Stata 16.1. Dependent variables were: trust in the pharmacy team, trust in the pharmacist, and trust in the PT. Independent variables were the constructs as identified with exploratory factor analysis (EFA).24 With EFA, we aimed to identify latent constructs that represented the underlying combined behaviour of the original interdependent items. EFA was especially useful since the original items had, between themselves, relatively high correlation coefficients.25 Oblique rotation was applied due to this correlation between the items. The cut-off point was a minimum factor loading of 0.4. An exception was made if the item scored just below 0.4 but still contributed to a higher reliability score of the latent construct. Control variables that were accounted for were the respondents’ age, general health, and type of lung disease. Multivariable regression analyses were conducted to construct a model that tested what aspects significantly contributed, either positively or negatively, to having trust in the pharmacy team. Two similar analyses, with different dependent variables, were conducted to gain insight into the factors that contributed to having trust in the pharmacist and the PT.
Results
Study Population of the Focus Group
Six people participated in the FG. Among these participants, three reported using inhaled medication for treatment of asthma and three for COPD. The group consisted of three male and three female participants, with an average age of 63 years (SD: 19.3). Five were pensioners, one had paid employment. All participants spoke Dutch. Two participants reported having a moderate health status, while the remaining four reported to have good health. On average, they had been using inhaled medication for 28 years (SD: 18.4).
Results of the Focus Group
There were five themes that emerged from the FG. These themes were addressed by the participants as having an impact on their trust in the pharmacy. Insight in the transcripts and coding of the FG may be requested from the authors. The following five themes were included in the questionnaire:
- Expertise: Participants indicated that the expertise of the pharmacy team was important for their trust in the pharmacy
- Personal relationship with the pharmacy: participants emphasized the importance of the pharmacy team knowing them personally
- Attention for / engagement with the patient: pharmacy team’s attention for the patient-, and their engagement in the patient’s medication use was highly valued by the participants
- Communication and contact with the pharmacy: adequate communication was highly valued as well
- The role of the pharmacy: the role that the pharmacy (team) played in supporting patients’ medication use was frequently but contradictory addressed. Some participants valued the pharmacy team as a healthcare provider that provides medication-related support, whereas other participants regarded the pharmacy as a shop for their medication.
Study Population of the Questionnaire
Out of 541 respondents who started the questionnaire, 221 completed less than 10% of the questionnaire and were therefore deleted from the analysis. In total, 320 respondents completed the questionnaire. Via the NPCD, 102 respondents were reached, 67 via the Dutch Lung Foundation, and 151 respondents were reached through an open link posted on social media. After deletion of respondents who had missing data on dependent, independent or control variables (N=30), 290 respondents remained in the dataset for analysis.
Table 1 includes the characteristics of the study population. Participants were on average 61 years old, the majority were female, had predominantly middle or high educational levels, were mostly pensioners, and almost all respondents had Dutch as their native language. On average, respondents indicated to have good to moderate health. Regarding the type of lung disease, the population was distributed about evenly (42% asthma and 41% COPD), and 17% of the respondents indicated to have both asthma and COPD. Years of inhaled medication use was on average 18 years (SD: 12.9).
 |
Table 1 Characteristics of the Study Population |
Trust in the Pharmacy Team, Pharmacist and Pharmacy Technician
The overall level of trust in the pharmacy team among patients with asthma and/or COPD was 7.4 (SD: 1.5) (Figure 1). The level of trust in the PT and in the pharmacist was roughly similar (7.4, SD: 1.6 and 7.3, SD: 1.9, respectively). For each dependent variable, between 86–89% of the respondents scored their trust 6 out of 10, or higher.
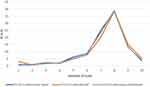 |
Figure 1 The level of trust in the pharmacy team, pharmacist and pharmacy technician. |
Identifying Latent Constructs
The clustering of items resulted in five possible underlying factors, namely patients’ perception of: (1) expertise of the pharmacy, (2) patient-centredness, (3) information and communication, (4) personal relationship and (5) opinion of peers. EFA revealed that all theoretically assumed constructs were confirmed to be valid latent constructs. Moreover, the patient-oriented construct revealed to diverge between “attention” and “engagement”. In the end, six latent constructs were identified. All constructs showed acceptable to excellent internal consistency levels (Table 2). RtP and MV refined the names of the latent construct after EFA results were obtained. Detailed results of the EFA with factor loadings per latent construct can be found in Supplementary Tables 1–6.
 |
Table 2 Results of Exploratory Factor Analysis |
Factors Contributing to Building Trust
Regression analyses revealed that higher perception of- expertise, pharmacy team’s engagement with the patient, and information provision and communication of the pharmacy team are positively associated with respondents’ trust in the pharmacy team (Table 3). The effect of expertise on trust is much stronger for the pharmacist, compared to the pharmacy team and the pharmacy technician. No significant differences in trust were found for the type of lung disease respondents had.
 |
Table 3 Effects on the Level of Trust for the Three Dependent Variables: Pharmacy Team, Pharmacist and Pharmacy Technician |
Discussion
The level of trust in the pharmacy team was found to be moderately high (grade of 7.4 out of 10) with no considerable difference in trust between the pharmacy team, pharmacist or PT. Pharmacy teams’ engagement with the patient, providing information and effective communication are important factors contributing to trust in the pharmacy team. Patients’ perception of expertise strongly contributed to building trust in the pharmacist, but weakly to trust in the pharmacy team as a whole.
In light of the first research question, our study revealed a moderately high level of trust in the pharmacy team, indicating that opportunities for enhancement persist. The two-yearly assessment of trust in healthcare in the Netherlands demonstrate similar substantial levels of trust in the pharmacy team among Dutch citizens.6 Despite the non-comparability of measurement methods between their assessments and ours, the convergence of outcomes suggests a certain degree of validity in our appraisal of trust in the pharmacy team.
We specifically focussed on patients with asthma and/or COPD, who rely on using inhaled medication, which is challenging to use- and adhere to optimally.26 Because of the difficult medication administration route of patients with asthma and/or COPD, it is important to understand whether there are population-specific factors that contribute to building trust, since different trust-building factors may be present among other populations. However, no specific trust-building factors for this population were found compared to previous studies.11–14 This implies that interventions aimed at bolstering patient trust within the pharmacy team should elicit comparable effects across a broad demographic diverse population.
Our population was distributed quite evenly regarding patients with asthma or COPD. Despite having similar medication related treatment, patients with asthma or COPD experience different symptoms and disease progression and might rely on different information and communication needs. Also, patients with COPD are more likely to have contact with a pulmonologist or pulmonary nurse as healthcare provider, as opposed to patients with asthma. However, in our study these differences appear not to have any influence of their trust in the pharmacy team, pharmacist or PT, answering our second research question.
In light of the evolving role of the pharmacy team from medication dispenser to healthcare provider,7 our findings indicate that patients with asthma and/or COPD value the contributions of each role within the pharmacy, answering the final research question. The factors associated with increased patients’ trust were 1) expertise, 2) patient engagement, and 3) effective communication. While pharmacists primarily serve as the medication expert, PTs are valued for their engagement with the patient and their ability to provide information and communicate effectively. These findings are in line with previous research, which also highlighted the importance of pharmacists’ technical competences and communication.14 Pharmacist behaviour was also found of utmost importance for trust building in another study.12 The extent to which the pharmacy was, according to patients, involved with the patients’ medication use, was also found to impact trust, but was then defined as affability and/or acknowledgement.13 Furthermore, leveraging a series of interpersonal communication behaviours and skills consistently, supports building trusting relationships between the pharmacy and patients.11 Our findings are in line with this research, since they also highlight the importance of effective communication by the pharmacy. If effective communication is key for building trust in the pharmacy, pharmacists and their teams should aim to improve their patient-centred communication skills. Repeated practice, video-recording, self-assessment and reflection and feedback are examples of strategies that could be implemented to improve patient-centred communication skills.27 Regular training for the pharmacy team in how improved patient-centred communication benefits their communication skills could also help,28 given those who practice their communication skills, provide better pharmaceutical care.29
Strengths and Limitations
This study has several strengths. The primary strength of this study is the use of a mixed methods design to identify factors that contribute to building trust. Detailed and contextualized insights from first-hand experiences of patients with asthma and/or COPD gained from the FG were combined with an assessment of trust and contributing factors among a larger cohort of patients through the questionnaire. Secondly, this study employed a more specific focus on a medication-taking population than previous studies, that generally examined a general patient population.
A limitation of this study is a potential for selection bias among respondents who participated in the FG and completed the questionnaire. We sent open invitations to participate in our research, which means that mostly motivated or engaged respondents responded to our invitations. This might have impacted our results, though patients both expressed positive and negative factors that play a role in their trust in the pharmacy. A second limitation of this study is the utilization of single-item measurements to assess trust in the pharmacy team, pharmacist, and pharmacy technician. Trust is a complex concept that is difficult to capture in a single item. Despite this uncertainty regarding the reliability of our measurements, the validity of the item(s) seem not be compromised, as the measurements of trust in the pharmacy team, pharmacist and do not notably diverge from trust in the pharmacy as measured in a previous study.6 Third, the average age of our study population was relatively high (60+ years). This might be a bias because older people might have a more conservative view towards the pharmacy than a younger population, because of the role that the pharmacy used to have.
Implications for Future Research and Practice
In 2022, a new Dutch integrated care agreement was instituted.30 This agreement strives for a more in-depth role for the pharmacy team as healthcare provider in pharmaceutical care. To be optimally acknowledged and trusted as healthcare provider by the general population, pharmacy team members should aim to further develop their patient-centred communication skills and seek to be more involved in patients’ medication taking journey. Moreover, previous research also found a positive relationship between patient-centred communication and trust, and identified trust to be an important mediator between patient provider communication and their perception of healthcare.31 Combined with the results from our study, this implies that improving patient-centred communication leads to greater patient trust in the patient-provider relationship, thereby also positively impacting the patient’s perception of healthcare.
Future research should also consider exploring whether a more in-depth concept of patient trust in the pharmacy team can be developed. Measurements like the trust PH-scale may be used and/or expanded upon.32 Secondly, in this study we mainly focussed on factors that affected trust positively. Future research could focus on factors that have a negative effect on trust in the pharmacy team.
Conclusion
Our study reveals that patients with asthma and/or COPD indicate to bestow trust in the different roles within the pharmacy, with the pharmacist serving as the medication expert and the pharmacy technician as the designated person to provide information and communication. Patient trust in the pharmacy enables the pharmacy team to facilitate patient care and attain optimal health outcomes. The pharmacy team should, according to asthma and COPD patients, persist in their efforts to uphold and potentially elevate their proficiency, patient engagement, and communication skills relevant for creating and sustaining the trust vested in them by their patients.
Abbreviations
COPD, Chronic Obstructive Pulmonary Disease; FG, Focus group; EFA, exploratory factor analysis; PT, Pharmacy technician; NPCD, National Panel of the Chronically ill and Disabled.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Ethics Approval and Informed Consent
Informed consent for participating in the study was obtained from all participants. For the FG, each participant gave consent for recording the session for data collecting purposes. For the questionnaire, all respondents were informed of the study objectives, and gave their informed consent before starting the questionnaire. The study does not fall within the scope of the Medical Research Involving Human Subjects Act and therefore does not require ethical approval, according to Dutch legislation. This study complies with the Declaration of Helsinki.
Consent for Publication
All participants in this study have provided informed consent. All authors provide consent for publication of this article.
Acknowledgments
We would like to express our gratitude to all the participants who took part in the focus group and completed the questionnaire.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was part of the On TRACk study that is funded by the Netherlands Organisation for Health Research and Development; ZonMw. Dossier number: 80-84800-98-18089.
Disclosure
MV has received funding from Teva, AstraZeneca, Biogen, for research unrelated to this study. JvB reports grants from Aardex, grants and personal fees from AstraZeneca, grants and personal fees from Chiesi, personal fees from GSK, grants and personal fees from Novartis, personal fees from Teva, from Trudell Medical, and vertex outside the submitted work and all paid to his institution (UMCG). LvD received funding for research unrelated to this study from Teva and Biogen. The authors report no other conflicts of interest in this work.
References
1. Tsuyuki RT, Beahm NP, Okada H, Al Hamarneh YN. Pharmacists as accessible primary health care providers: review of the evidence. Can Pharm J. 2018;151(1):4–5. doi:10.1177/1715163517745517
2. Melton BL, Lai Z. Review of community pharmacy services: what is being performed, and where are the opportunities for improvement? Integr Pharm Res Pract. 2017;6:79–89. doi:10.2147/IPRP.S107612
3. Thiede M. Information and access to health care: is there a role for trust? Soc Sci Med. 2005;61(7):1452–1462. doi:10.1016/j.socscimed.2004.11.076
4. Alaszewski A. Risk, Trust and Health. Taylor & Francis; 2003.
5. van de Pol JM, Geljon JG, Belitser SV, Frederix GW, Hövels AM, Bouvy ML. Pharmacy in transition: a work sampling study of community pharmacists using smartphone technology. Res Social Administrative Pharm. 2019;15(1):70–76. doi:10.1016/j.sapharm.2018.03.004
6. Hulst FJ, Brabers AEM, de en Jong JD. Barometer Vertrouwen in de Gezondheidszorg [Barometer Trust in Healthcare]; 2023. Available from: https://www.nivel.nl/consumentenpanel-gezondheidszorg/resultaten-vertrouwen.
7. van de Pol JM, van Dijk L, Koster ES, de Jong J, Bouvy ML. How does the general public balance convenience and cognitive pharmaceutical services in community pharmacy practice. Res Social Administrative Pharm. 2021;17(3):606–612. doi:10.1016/j.sapharm.2020.05.014
8. Vervloet M, Zwikker HE, Linn AJ, et al. The development and proof of principle test of TRIAGE: a practical question set to identify and discuss medication-related problems in community pharmacy. Pharmacy. 2020;8(4):178. doi:10.3390/pharmacy8040178
9. van Dijk M, Blom L, Koopman L, et al. Patient-provider communication about medication use at the community pharmacy counter. Int J Pharm Pract. 2016;24(1):13–21. doi:10.1111/ijpp.12198
10. Mattingly AN, Mattingly TJ. Advancing the role of the pharmacy technician: a systematic review. J Am Pharm Assoc. 2018;58(1):94–108. doi:10.1016/j.japh.2017.10.015
11. Gregory PA, Austin Z. How do patients develop trust in community pharmacists? Res Social Adm Pharm. 2021;17(5):911–920. doi:10.1016/j.sapharm.2020.07.023
12. Esmalipour R, Salary P, Shojaei A. Trust-building in the pharmacist-patient relationship: a Qualitative Study. Iran J Pharm Res. 2021;20(3):20–30. doi:10.22037/ijpr.2020.114113.14675
13. Gregory PAM, Austin Z. Understanding the psychology of trust between patients and their community pharmacists. Can Pharm J. 2021;154(2):120–128. doi:10.1177/1715163521989760
14. Siddiqua A, Kareem Abdul W, Ayan S, Al Azm L, Ali S. Antecedents of patients’ trust in pharmacists: empirical investigation in the United Arab Emirates. Int J Pharm Pract. 2018;26(1):63–72. doi:10.1111/ijpp.12359
15. Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. doi:10.1016/j.rmed.2011.01.005
16. Melani AS, Canessa P, Coloretti I, et al. Inhaler mishandling is very common in patients with chronic airflow obstruction and long-term home nebuliser use. Respir Med. 2012;106(5):668–676. doi:10.1016/j.rmed.2011.11.016
17. Lewis A, Torvinen S, Dekhuijzen PN, et al. The economic burden of asthma and chronic obstructive pulmonary disease and the impact of poor inhalation technique with commonly prescribed dry powder inhalers in three European countries. BMC Health Serv Res. 2016;16:251. doi:10.1186/s12913-016-1482-7
18. Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10. doi:10.1186/s12931-017-0710-y
19. Mahmoud A, Mullen R, Penson PE, Morecroft C. The management of asthma in adult patients in the community pharmacy setting: literature review. Res Social Administrative Pharm. 2021;17(11):1893–1906. doi:10.1016/j.sapharm.2021.04.001
20. Hu Y, Yao D, Ung COL, Hu H. Promoting community pharmacy practice for Chronic Obstructive Pulmonary Disease (COPD) management: a systematic review and logic model. Int J Chronic Obstr. 2020;Volume 15:1863–1875. doi:10.2147/COPD.S254477
21. Polinski J, Kesselheim A, Frolkis J, Wescott P, Allen-Coleman C, Fischer M. A matter of trust: patient barriers to primary medication adherence. Health Educ Res. 2014;29(5):755–763. doi:10.1093/her/cyu023
22. Brown MT, Bussell J, Dutta S, Davis K, Strong S, Mathew S. Medication adherence: truth and consequences. Am J Med Sci. 2016;351(4):387–399. doi:10.1016/j.amjms.2016.01.010
23. Boeije H. National panel of the chronically ill and disabled. Available from: https://www.nivel.nl/en/national-panel-chronically-ill-and-disabled-npcd.
24. Fabrigar LR, Wegener DT. Exploratory Factor Analysis. Oxford University Press; 2011.
25. Fávero LP, Belfiore P. Data Science for Business and Decision Making. Academic Press; 2019.
26. Dekhuijzen R, Lavorini F, Usmani OS, van Boven JF. Addressing the impact and unmet needs of nonadherence in asthma and chronic obstructive pulmonary disease: where do we go from here? J Allergy Clin Immunol. 2018;6(3):785–793. doi:10.1016/j.jaip.2017.11.027
27. Kerr A, Kelleher C, Pawlikowska T, Strawbridge J. How can pharmacists develop patient-pharmacist communication skills? A realist synthesis. Patient Educ Couns. 2021;104(10):2467–2479. doi:10.1016/j.pec.2021.03.010
28. Ilardo ML, Speciale A. The community pharmacist: perceived barriers and patient-centered care communication. Int J Environ Res Public Health. 2020;17(2):536. doi:10.3390/ijerph17020536
29. Vervloet M, Lambooij A, Koster E, et al. Betere baliegesprekken met COM-MA-training: aansluiten bij behoeften en voorkeuren van patiënten [Improved Front Desk Conversations with COM-MA Training: aligning with the needs and preferences of patients]. Pharm Weekbl. 2018;153(10):16–17.
30. Ministerie van Volksgezondheid W en S. Integraal Zorgakkoord: “Samen werken aan gezondezorg” - Rapport [Integral care agreement: working together for healthy healthcare]; 2022; Available from: www.rijksoverheid.nl.
31. Hong H, Oh HJ. The effects of patient-centered communication: exploring the mediating role of trust in healthcare providers. Health Commun. 2020;35(4):502–511. doi:10.1080/10410236.2019.1570427
32. Ngorsuraches S, Lerkiatbundit S, Li SC, Treesak C, Sirithorn R, Korwiwattanakarn M. Development and validation of the patient trust in community pharmacists (TRUST-Ph) scale: results from a study conducted in Thailand. Res Social Administrative Pharm. 2008;4(3):272–283. doi:10.1016/j.sapharm.2007.10.002
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
