Back to Journals » Journal of Pain Research » Volume 13
Factors Associated with Life Satisfaction in Older Adults with Chronic Pain (PainS65+)
Authors Dong HJ , Larsson B , Dragioti E , Bernfort L, Levin LÅ , Gerdle B
Received 14 October 2019
Accepted for publication 28 January 2020
Published 5 March 2020 Volume 2020:13 Pages 475—489
DOI https://doi.org/10.2147/JPR.S234565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Video abstract presented by Huan-Ji Dong.
Views: 382
Huan-Ji Dong,1 Britt Larsson,1 Elena Dragioti,1 Lars Bernfort,2 Lars-Åke Levin,2 Björn Gerdle1
1Pain and Rehabilitation Centre, Department of Health, Medicine, and Caring Sciences, Linköping University, Linköping, Sweden; 2Unit of Health Care Analysis, Division of Society and Health, Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, SE-581 85, Sweden
Correspondence: Huan-Ji Dong
Pain and Rehabilitation Centre, University Hospital, Linköping SE 581 85, Sweden
Tel +46 73 048 8933
Fax +46 10 103 4906
Email [email protected]
Background: Chronic pain in later life is a worldwide problem. In younger patients, chronic pain affects life satisfaction negatively; however, it is unknown whether this outcome will extend into old age.
Objective: This study examines which factors determine life satisfaction in older adults who suffer from chronic pain with respect to socio-demographics, lifestyle behaviors, pain, and comorbidities.
Methods: This cross-sectional study recruited a random sample of people ≥ 65 years old living in south-eastern Sweden (N= 6611). A postal survey addressed pain aspects and health experiences. Three domains from the Life Satisfaction Questionnaire (LiSat-11) were used to capture the individual’s estimations of overall satisfaction (LiSat-life), somatic health (LiSat-somhealth), and psychological health (LiSat-psychhealth).
Results: Respondents with chronic pain (2790, 76.2± 7.4 years old) rated lower on life satisfaction than those without chronic pain, with medium effect size (ES) on LiSat-somhealth (r = 0.38, P < 0.001) and small ES on the other two domains (r < 0.3). Among the respondents with chronic pain, severe pain (OR 0.29– 0.59) and pain spreading (OR 0.87– 0.95) were inversely associated with all three domains of the LiSat-11. Current smoking, alcohol overconsumption, and obesity negatively affected one or more domains of the LiSat-11. Most comorbidities were negatively related to LiSat-somhealth, and some comorbidities affected the other two domains. For example, having tumour or cancer negatively affected both LiSat-life (OR 0.62, 95% CI 0.44– 0.88) and LiSat-somhealth (OR 0.42, 95% CI 0.24– 0.74). Anxiety or depression disorders had a negative relationship both for LiSat-life (OR 0.54, 95% CI 0.38– 0.78) and LiSat-psychhealth (OR 0.10, 95% CI 0.06– 0.14).
Conclusion: Older adults with chronic pain reported lower life satisfaction but the difference from their peers without chronic pain was trivial, except for satisfaction with somatic health. Pain management in old age needs to consider comorbidities and severe pain to improve patients’ life satisfaction.
Keywords: chronic pain, life satisfaction, older adults, comorbidity
Introduction
Chronic pain in later life is a worldwide problem. The prevalence of chronic pain is known to increase with advancing age, ranging between 25% and 76% in the general elderly population and up to 93% of elderly in residential care.1 Since the world population is aging rapidly and life expectancy is increasing, more and more older people will face facing chronic pain and its consequences.2 In younger patients, chronic pain can result in activity limitations in everyday life both during work and leisure time,3–5 and these limitations might extend into the old age, increasing the incidence of frailty.6 In addition, chronic pain in younger patients decreases life satisfaction.4,7 Currently, little is known about how chronic pain affects life satisfaction in older adults; an area that needs more research.
Life satisfaction reflects how people perceive the difference between their reality and their needs or desires with respect to several important domains of functioning and activity/participation.8 In general, life satisfaction is a construct of subjective wellbeing related to how people evaluate the quality of specific aspects of their lives such as work, marriage, health, recreation, religion as well as the quality of the more general aspects of their lives such as happiness, morale, zest for life, and peace of mind.9 In the pain management and rehabilitation context, it is known that the rational aspect of life satisfaction is a result of an individual’s coping and adaption process.10,11 There is reason to believe that older adults perceive their life satisfaction lower than young people due to their accumulating exposure of disease burden and the general negative effects of aging. However, research has found that in high-income countries people in later life were more satisfied with their lives than middle-aged people.12,13 Moreover, older adults with chronic pain despite greater physical impairment were found to have comparable health status, similar pain intensity, and better mental health compared to younger patients.14
An older population has many aspects other than socio-demographic characteristics that differ from a younger population.12,15-17 For example, comorbidity and multimorbidity,18 including pain-related comorbidities,19,20 are very common in the older adults. Studies have found that older adults with chronic medical illnesses/conditions have lower life satisfaction.21,22 In addition, life satisfaction is influenced by lifestyle factors. In general, life satisfaction in aging populations is related to lifestyle behaviours.12,23 For example, smoking, alcohol consumption, and obesity are known to be related to chronic pain,24–26 but these are seldom addressed in pain research on life satisfaction.
Many studies have focused on general aging populations15,21,27,28 and specific aging characteristics29–31 to investigate life satisfaction in relation to social, physical, mental, and financial aspects. However, only a few studies have investigated life satisfaction in relation to chronic pain in the older adults. For example, Karadag Arli et al reported that pain in older patients is one of the most frequently reported health problems that negatively affect life satisfaction,22 and Yang et al demonstrated that pain is the most common condition in geriatric syndrome associated with low life satisfaction.32 However, these conclusions are based on the comparisons of older adults with or without pain symptoms and do not analyze crucial factors such as specific pain characteristics within the groups with chronic pain.
Given this background, more knowledge is needed about factors contributing to life satisfaction in older adults with chronic pain. Such knowledge may stimulate the development of prevention and intervention strategies to help older adults maintain and increase life satisfaction despite chronic pain. To fill this gap in knowledge, this study investigates the following research questions:
- How do older adults with and without chronic pain experience life satisfaction?
- What factors (e.g., lifestyle behaviors, pain aspects, and comorbidities) are associated with overall life satisfaction (life as a whole), somatic health, as well psychological health in the older people with chronic pain?
Methods
Study Population
This study is part of a large Swedish population-based study of the elderly (cohort PainS65+).33–36 Data collection was a cross-sectional design with a stratified random sample of 10,000 older adults (≥65 years old) based on five age strata (65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, and 85 years and older) from the Swedish Total Population Register for the two large cities (Linköping and Norrköping) in a south-eastern county (Östergötland) of Sweden.33–36 Data were collected by Statistics Sweden (SCB). A postal survey addressing pain aspects and health experiences were mailed in October 2012 and data collection closed in January 2013. Two reminders at two-week intervals were mailed if necessary.
Measurements
Life Satisfaction
The survey included three items from the Fugl-Meyers Life Satisfaction Questionnaire (LiSat-11), which captures the respondent’s estimation of satisfaction with life as a whole (LiSat-life) as well as satisfaction on ten specific domains.11 The present study evaluates satisfaction with life as a whole (LiSat-life), somatic health (LiSat-somhealth), and psychological health (LiSat-psychhealth). Each item is rated on a 6-point response Likert scale ranging from very dissatisfied to very satisfied: 1 = very dissatisfied; 2 = dissatisfied; 3 = rather dissatisfied; 4 = rather satisfied; 5 = satisfied; and 6 = very satisfied. The scale was dichotomized into satisfied (very satisfied and satisfied) and dissatisfied (very dissatisfied, dissatisfied, rather dissatisfied, and rather satisfied), a dichotomization used by the developers of this instrument8 as well as others.7,30 The LiSat-11 has been validated for Swedish adults (men and women aged 18–74 years),11 and the reliability test for the present study (Cronbach’s alpha 0.80) suggested good internal consistency.
Chronic Pain Aspects
Chronic pain was defined by a single question and one follow-up question with respect to the presence and time course of pain: “Do you usually have pain?” (yes/no) and “If yes, has your pain lasted fewer than 3 months or more than three months?”. The subjects who responded that they had pain for more than 3 months were categorized as chronic pain and those who responded that they had no pain or pain for less than 3 months were categorized as no chronic pain.
The respondents with chronic pain were asked to assess their pain intensity and severity over the preceding 7 days using an 11-point numeric rating scale (NRS) (0 = no pain and 10 = worst imaginable pain). Good validity in experimental conditions was reported.37 Scores 0–3, 4–6, and 7–10 correspond to no/mild, moderate, and severe pain. These labels rather than the scores might more adequately represent the respondents’ perceptions in clinical practice. The cut-offs for NRS for definitions of pain severity vary in the literature.38–41 In this study, we selected the cut-offs because severe pain makes it difficult for individuals to partake in daily living activities.41,42
To assess pain spreading, we asked the respondents to mark their painful sites for the previous 7 days on a body manikin divided into 45 sections on the front and on the back.43,44 From these sections, we identified 23 anatomical pain sites and developed an index for the total number of anatomic pain sites (APS), ranging from 0 to 23.45 Higher values indicate higher spreading of pain (multi-site pain).
Lifestyle Behaviors
We used the instrument Health Curve (Hälsokurvan)46 to gather data on health behaviors. Four questions from the instrument were used to assess smoking and snuff use with respect to frequency (from never to daily), number of cigarettes per day (1 to 9; 10 to 19; and 20 or more), and number of snuff boxes per week (1 to 3 per week and 7 or more per week). Five questions were used to assess alcohol habits. For those who confirmed alcohol consumption, Cut-down, Annoy, Guilty, and Eye-opener (CAGE) questions were used to screen possible alcohol addiction problems. A score of ≥ 2 was considered as high alcohol consumption, indicating potential problems with alcohol abuse.47
Body mass index (BMI = weight (kg)/height (m2)) was calculated based on self-reported body height and weight. BMI was classified according to the criteria developed by the World Health Organization (WHO): <18.5 = underweight; 18.5–24.9 = normal range; 25.0–29.9 = overweight; and ≥30.0 = obesity.
Comorbidities
Assessing comorbidities were assessed using 12 items covering different common comorbidities: 1) traumatic accident/injuries; 2) rheumatic arthritis and osteoarthritis; 3) cardiovascular diseases (including high blood pressure, angina pectoris, and heart attacks); 4) diseases of airways or lungs; 5) low mood and depression; 6) anxiety; 7) diseases of the gastrointestinal organs; 8) diseases of the nervous system including eyes and hearing problems; 9) diseases of the urogenital organs; 10) skin diseases; 11) tumors and cancer; and 12) metabolic diseases (including diabetes, obesity, anorexia bulimia, and struma). The respondents have five answer options: a) No; b) Yes, both according to my and my doctor’s opinions; c) Yes, according to my own opinion; d) Yes, according to my doctor’s opinion; and e) Do not know. The presence of a comorbidity was determined using the answers from b or d as these were doctor assessments.
Other Factors
Age, sex, and educational level were gathered from the respondents’ answers in the survey. Statistics Sweden (SCB) supplied information about marital status, country of origin, and yearly income (Swedish Crowns 0–150 000, 150 001–220 000, and 220 001 and over33) from the Swedish population register.
The MPI (Multidimensional Pain Inventory) is a self-report questionnaire constructed to measure psychosocial, cognitive, and behavioral effects of chronic pain. In the present study, questionnaire measured psychosocial, cognitive, and behavioral effects of chronic pain.48,49 We chose five scales concerning leisure activities according to the Swedish version of MPI (MPI-S).50 These subscales were summarized and divided by the number of items answered (not all subjects answered items concerning car and relatives) to form a leisure index (MPI-leisure) according to the validation of the Swedish version of MPI-S. A higher index indicates a higher level of leisure activity.
All the participants were asked whether they had sleep problems or not. They were also asked to rate their sleep problems using the Insomnia Severity Index (ISI). ISI is a reliable and valid instrument for detecting cases of insomnia and has excellent internal consistency.51 Each item is rated on a 5-point Likert scale (0–4). A sum of the seven items generates the score between 0 and 28. A score of 15 and over is defined as clinical insomnia.51,52 In this study, sleep disorders were determined as self-perceived sleep problems or clinical insomnia (ISI ≥15).
Initially, we chose three questions from the Oslo-3 Social support Scale (OSS-3) to measure social support.53,54 Due to frequent answers of “not know, no idea” in two questions, we ended up using only one question: “How many people are so close to you that you can count on if you have great personal problems? (none, 1–2, 3–5, or 5+)”.
Statistics
The statistics were performed using the statistical package IBM SPSS Statistics (version 25.0; IBM Inc., New York, USA). Level of significance was set to <0.05 in all tests. Continuous data are reported as the mean and standard deviation (SD) or median (interquartile range, IQR) based on the gaussian distribution. The categorical data are represented as n (%). Student’s independent t test and Mann–Whitney U-test were used for the continuous variables and Chi-square tests were used for categorical data. Spearmen’s rho non-parametric rank correlation was used to analyse correlations of three LiSat-11 domains with continuous and ordinal variables. To investigate within group differences, we used Mann–Whitney U-test and calculated effect size (ES, r=z/√N)55 to quantify the differences between respondents with or without chronic pain. The ES (r) was considered large if ≥0.5, medium if 0.3–0.5, and small if 0.1–0.3.55,56 Floor and ceiling effects were calculated and considered present if more than 40% of the patients scored the lowest or highest score on the three LiSat domains.57 Multivariate logistic regression, a forward (likely ratio, LR) method, was used by entering each variable forwardly and removing the least significant variables from the model until all remaining variables were significant (P < 0.05 or P ≥ 0.1 for entry or removal, respectively). LiSat-life, LiSat-somhealth, and LiSat-pschhealth were treated as binary dependent variables: 1 = satisfied and 0 = not satisfied. We used the Hosmer and Lemeshow test where a P-value greater than 0.05 indicated good fit of the model. Socio-demographic variables, lifestyle behaviours, pain profiles, general activity level, social support, and comorbidities served as independent variables. Multicollinearity was assessed by examining tolerance and the variance inflation factor (VIF).58,59 We further examined problems of collinearity among the categorical variables using the phi (Φ, Φ ≥ 0.30 indicating high correlation).60 Two pairs –education level and yearly income and anxiety and depression disorders – showed high correlations. We selected income level as it had fewer missing data than education. We also transformed the anxiety and depression variables to a new variable (1 = depression and/or anxiety) to represent mood disorder. Sensitivity analysis was conducted to measure the association between the scores of LiSat domains as continuous variables and the binary outcomes from the logistic regressions (see supplementary document).
Results
The postal survey was completed by 6611 older adults (response rate of 66.1%) of which 2790 (about 42%) reported chronic pain. Detailed information about the socio-demographics, lifestyle behaviors, and comorbidities for the whole sample population and respondents without chronic pain are described elsewhere.33–35
For the respondents with chronic pain (n = 2790), mean age was 76.2 (SD 7.4) and the majority were women (61.1%) and currently married (55.8%). About 20% had college/university education (Table 1). The yearly income levels were evenly divided with approximately 33% in each of the three categories. Less than one-tenth smoked (8.1%) and 4.8% had high alcohol consumption. In total, more than three out of four respondents were either normal weight (40.6%) or overweight (36.5%) (Table 1). The most common comorbidities were cardiovascular diseases (53.9%) and rheumatic disorders (44.4%). Some of the demographic characteristics in this study sample (n = 2790) are also described elsewhere.52,61
Life Satisfaction
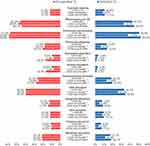
A total of 6510 respondents provided data on life satisfaction. The median scores of LiSat-life, LiSat-somhealth, and LiSat-psychhealth were 5 (IQR 4 to 5), 4 (IQR 4 to 5), and 5 (IQR 5 to 6), respectively, indicating rather satisfying to satisfying. The respondents with chronic pain (n = 2747) rated lower satisfaction than those without chronic pain (n = 3763) in all three domains (P <0.001, ES between 0.14 and 0.38), with the largest difference for LiSat-somhealth (medium ES r = 0.38) and smallest for LiSat-psychhealth (ES r = 0.14). All ES remained in the same ranges with age and gender stratification. As shown in Figure 1, significantly lower proportions of the respondents with chronic pain scored “satisfied” (scores 5–6) in the three items, especially somatic health which had the lowest percentage (22.9%). Furthermore, among the respondents with chronic pain, those satisfied with overall life were also more likely to be satisfied with somatic health (557/1432, 38.9%, P < 0.001) and psychological health (1268/1430, 88.7%, P < 0.001) than respondents with dissatisfied life (Table 1). No ceiling or floor effects of the three LiSat-11 domains were identified, with 0.7–2.2% scoring the lowest level and up to 28.6% scoring the highest level.
Respondents with Chronic Pain: Demographics, Pain Aspects, and Comorbidities
Table 1 gives the background characteristics with comparisons between respondents satisfied (scores 5–6) and dissatisfied with life (scores 1–4) according to LiSat-life among the respondents with chronic pain. The respondents with the following characteristics were more likely to be satisfied with life: being younger, married, higher education, higher income, never smoking, overweight, and many trusted friends (Table 1).
In comparison with those dissatisfied with life (LiSat-life, scores 1–4), the respondents with overall life satisfaction (LiSat-life, scores 5–6) had lower mean values of pain intensity (mean 4.7, SD 2.0, P < 0.001) and pain spreading (total number of APS, median 3, IQR 1 to 4, P < 0.001) as well as higher mean values of general activity level (mean 2.6, SD 1.0, P < 0.001). Almost one-third of those with dissatisfied life had severe pain (353/1201, 29.4%, P < 0.001) and more than one half had sleep disorders (736/1256, 58.6%, P < 0.001). The significant but weak correlations of LiSat-life estimates (scores 1–6) with pain intensity, pain spreading and activity level are shown in Table 1 (Spearman’s rho = 0.128–0.274). In comparison, the strongest correlation was found between pain intensity and satisfaction on somatic health (LiSat-somhealth, Spearman’s rho =0.369).
Figure 2 shows the distribution of comorbidities among the respondents with respect to life satisfaction on life as a whole (LiSat-life), somatic health (LiSat-somhealth), and psychological health (LiSat-psychhealth). Overall, each comorbidity was significantly associated with one or more aspects of life satisfaction. Some comorbidities, including cardiovascular diseases, depressive disorders, anxiety disorders, gastrointestinal diseases, CNS disorders, urogenital disorders, and tumor/cancer diseases showed significant associations with all three aspects of life satisfaction. We found that respondents were more likely to be dissatisfied with somatic health if they were diagnosed with diseases (P < 0.001), but this was not always the case for dissatisfaction with life as a whole or psychological health.
Factors Associated with Life Satisfaction
Logistic regression was used to analyze factors associated with life satisfaction among the respondents with chronic pain (Table 2). As shown in Table 2, oldest age (85+ years old, OR 0.41–0.57), currently smoking (OR 0.51–0.56), severe pain (OR 0.29–0.59), pain spreading (OR 0.87–0.95) and sleep disorders (OR 0.53–0.70) were inversely associated with life satisfaction on all three domains investigated – i.e., LiSat-life, LiSat-somhealth. and LiSat-psychhealth. Highest yearly income (OR 1.81–1.97) and increased activity level (OR 1.33–1.44) were positively related to satisfaction on all the three domains.
 |
Table 2 Logistic Regression Analysis of Factors Predicting Life Satisfaction in the Older Adults with Chronic Pain |
Some variables were associated with one or two domains of life satisfaction. For example, being a woman (OR 1.55, 95% CI 1.23–1.94) and currently married (OR 2.0, 95% CI 1.64–2.43) increased the possibility to be satisfied with overall life. Being a woman (OR 1.36, 95% CI 1.05–1.76) also slightly increased likelihood to be satisfied with somatic health. Moreover, born outside Europe (OR 0.55, 95% CI 0.34–0.87) predicted being dissatisfied with psychological health. High alcohol consumption (OR 0.60–0.64) was negatively associated with overall life satisfaction as well as psychological health satisfaction, while being obese (OR 0.64, 95% CI 0.45–0.92) was associated with being less likely to be satisfied with somatic health. Having more than five trusted friends (OR 1.76, 95% CI 1.05–2.97) predicted satisfaction with psychological health.
Several comorbidities were negatively associated with life satisfaction, especially with somatic health satisfaction. As summarized in Table 2, eight comorbidities were inversely associated with satisfied somatic health, and four of these also indicated negative impacts on some other domains. For example, having a diagnosis of tumor or cancer affected satisfaction with overall life (OR 0.62, 95% CI 0.44–0.88) as well as somatic health (OR 0.42, 95% CI 0.24–0.74). Suffering from mood disorders (anxiety or depression) not only had a robust effect on psychological health dissatisfaction (OR 0.1, 95 CI 0.06–0.14) but also contributed to dissatisfaction with overall life (OR 0.54, 95% CI 0.38–0.78) as well. Only one comorbidity – having history of trauma injuries (OR 1.46, 95% CI 1.03–2.08) – showed weak but significant association to satisfaction with psychological health. When trauma and pain severity interactions were regressed, no significant association was evident with their interaction effect (data not shown).
Discussion
This large-scale cross-sectional study, embedded within the epidemiological survey on chronic pain prevalence and consequences (PainS65+), investigated life satisfaction in the older adults with chronic pain. Compared to clinical patient populations, one strength of this study is the random sampling and age strata methodology implemented in the survey (sampling weights regarding age strata, sex, and city were calculated by SCB), so we could examine a wide age range with old-old and oldest-old ages included. We provided a distinctive profile of the associated factors of satisfaction on overall life (LiSat-life), somatic health (LiSat-somhealth), and psychological health (LiSat-psychhealth) regarding sociodemographic characteristics, lifestyles, pain aspects, and their consequences as well as comorbidities. Our results indicate that pain management and rehabilitation in older adults might need to give more attention to comorbidities and severe pain in order to reach better life satisfaction.
Life Satisfaction in the Older Adults with and Without Chronic Pain
Using LiSat-11, previous clinical studies have reported that patients with chronic pain have low life satisfaction4,7,10 and the prevalence of dissatisfied persons among these patients were much higher than in the general population.4 This difference was much smaller in the aged general population. One of the most influential factors affecting life satisfaction for elderly people is wisdom, which is defined as having “expert knowledge in the fundamental pragmatics of life”, the tendency towards reflection on one’s own behavior and that of others, and exhibiting kindness and empathy rather than egotism.62 In our study, respondents with chronic pain rated lower life satisfaction than those without chronic pain, but the effect size was only small (LiSat-life and LiSat-psychhealth) to medium (LiSat-somhealth domain). The different ranges remained the same when we stratified by age and gender. In line with other studies, older adults were generally satisfied or rather satisfied with their life.22,27,29,30 Although previous research suggests older adults with chronic painful conditions rated their physical health lower,14,63,64 we only found medium effect size in satisfaction with somatic health (LiSat-somhealth), possibly due to more comorbidities.21,32,65 It should be noted that our sample was randomly selected from an aged population sample, including older adults in sheltered accommodations, but not specifically from nursing homes where residents report low life satisfaction levels.66
Factors Associated with Life Satisfaction in the Older Adults with Chronic Pain
Few studies have illustrated factors associated with life satisfaction in aging populations with chronic pain. Our study focused on several aspects. Similar to general aging populations,12,22 some socio-demographic characteristics such as advancing ages, being a woman, married status, and high-income level (as well as high education) were related to overall life satisfaction. Among the younger patients with chronic pain, these factors did not show significant effects.4,7 Notably, in prior studies, subjects with pain who were born outside northern Europe reported lower life satisfaction in both general populations as well as in young patient samples with chronic pain.4,8 In comparison, our study showed the country of origin for older adults with chronic pain did not significantly affect their overall life satisfaction or satisfaction with somatic health. The only borderline significance was found in relation to psychological health (regression model in LiSat-psychhealth). One reasonable speculation is that the difference between first-generation immigrants and those born in Sweden is much smaller in later life because of the integration and more similar life conditions those born in Sweden experience by the time they reach old age.
This study also considered the roles of lifestyle behaviors in association with the three domains of life satisfaction, since lifestyle behaviors are closely related to chronic pain67–70 as well as well-being.12,23 Behavioral factors are often treated as modifiable factors that suggest potentials for intervention in pain management. We found that smoking behavior negatively affected satisfaction on all three domains of the LiSat-11, while obesity showed a marginally negative impact on satisfaction with somatic health and high alcohol consumption contributed modestly to satisfaction with overall life and psychological health. In summary, these results gave insight into non-optimal lifestyles together with chronic pain that favor older adults’ dissatisfaction with their lives. Our analysis, unfortunately, did not include physical activity due to the relatively high number of missing cases. However, MPI-leisure index to some extent reflects the importance of being active in everyday life for high life satisfaction despite chronic pain.
We found that pain intensity and pain spreading influenced older adults’ life satisfaction in all three domains of the LiSat-11. The high pain intensity (NRS 7–10, severe pain) showed largest negative effects on satisfaction with somatic health, which was also found in other studies.4,71 Associations between pain intensity and overall life satisfaction have not been consistent in clinical studies.4,7,71-73 Some studies found no correlation on psychological health.4,7 Unlike our study, these studies did not always consider the pain distribution or pain spreading. Pain spreading, however, showed weaker effect than pain intensity in this study sample. One study measured pain distribution by estimating the percentage of the body surface. Modest correlation between pain spreading and LiSat-life (Spearman’s rho −0.194) was reported, but no significant association was found in multiple regression analysis.73 One explanation is that multiple pain sites, instead of being calculated as an index or percentage, need to be presented as grades such as local, regional, and widespread pain, which our previous studies found to be robustly associated with decreased quality of life and health.35,43 The effects might be more pronounced when larger dispensation of pain spreading is compared with single site pain. Together with the pain aspects, sleep disorders consistently affected life satisfaction negatively. This result ties well with previous studies wherein found connections of chronic pain and sleep disorders as well as other comorbidities (i.e. anxiety and depression).52,74 Therapy for sleep disorders deserves to be part of chronic pain management for older adults. In pain management, non-pharmacologic interventions need to be included, because it is a great challenge to pharmacologic treatment considering age-related physiological changes and drug interactions. For example, mind-body program showed clinically significant (30%) reduction in severe pain intensity,75 as well as better sleep, improved quality of life and enhanced well-being.76 In recent years, pain neuroscience education has also been used in the older adults to improve fear of movement and mobility management.77
As reported by other researchers, comorbidity and multimorbidity affect older adults’ life satisfaction negatively.21,32,65,78 It is not surprising that individuals might be more likely to be dissatisfied with somatic health when they have several comorbidities as was investigated in this study. The noteworthy findings are the identified comorbidities associated with the LiSat-11 domains, findings not reported in other studies.22,32 For example, the most common comorbidities (rheumatoid arthritis, osteoarthritis, and cardiovascular diseases) were only associated with somatic health satisfaction. Mental diseases such as depression or anxiety affected overall life satisfaction as well psychological health. Although this cross-sectional analysis could not identify whether the associations preceded or followed disease onset, our results provide an insight into the impact of chronicity on different aspects of well-being. Suffering from chronic pain leads to more health service consumption and physician contacts,33,43 which in turn may increase the possibility of having more medical diagnoses. Alternatively, receiving a lot of health services that address chronic illness per se might negatively influence dissatisfaction with somatic health for the elderly. Future research is needed to investigate how causality and the severity of chronic illness should be considered when estimating life satisfaction among the older adults with chronic pain, since negative effects may coexist and affect each other.
Same and Different Factors Associated with Different Domains of Life Satisfaction
Some factors are associated with all three domains of life satisfaction, including age, income level, smoking behaviors, pain aspects, sleep problems and general activity levels. Comorbidities, on the other hand, showed distinctions between the three domains. None of the comorbidities investigated here contributed to all the three domains of life satisfaction. Most comorbidities affected satisfaction with somatic health, but some comorbidities affected other domains. We might hypothesize that this difference is due to the combined effects of comorbidities as well as chronic pain and old age on individuals’ life satisfaction. It is also possible that pain increases as the comorbidities increase with age.22 When we stratified by chronic pain without any comorbidity (n = 284, data not shown), pain aspects were still robust negative effects on two domains (LiSat-somhealth and LiSat-psychhealth) and old age was only inversely related to LiSat-life. Alternatively, we could denote multimorbidity as a variable based on the definition of two or more comorbidities.79 In the regression models (data not shown), multimorbidity, pain aspects, and old age were significantly associated with all three domains of life satisfaction. One disadvantage of this approach is that we could not specify the impacts of different comorbidities.
Of all the investigated comorbidities, only one had a positive impact; the others showed negative effects. Having a history of trauma injuries was found to have a weakly positive effect on psychological health satisfaction. We further explored the interactions of trauma history and pain severity as well as trauma history and depression/anxiety in the models. The positive significance remained in the regression model. In those studies with younger patients, trauma history was negatively associated with satisfaction and the pain consequences of trauma was known to decrease life satisfaction.7,80 We speculate that older pain patients have better-coping strategies and life control, which also was reported by Wittink et al, in comparison to younger pain patients.14 However, this significance was not robust, and we had a large-scale sample. Further study with attention to psychological symptoms related to trauma experience in younger lives and life satisfaction in old age might provide more knowledge about pain management.
Naturally, it is reasonable to expect somatic comorbidities had negative effects on satisfaction of somatic health, as these diagnoses, are related to physical illness.65,78 The painful comorbidities (i.e., rheumatic diseases and osteoarthritis) and comorbidities substantially affecting daily activities (i.e., advanced heart disease and chronic obstructive pulmonary disease) had stronger impacts than other comorbidities, perhaps because they worsen functional limitations as well as chronic pain. Only one somatic comorbidity (pulmonary disease) was negatively associated with satisfaction on psychological health. This observation may indicate respiratory symptoms (i.e. cough, dyspnea), as well as pain, are unpleasant sensations with both physiological and psychological consequences.81,82 In comparison with many other chronic diseases, the rates of coexisted anxiety and depression may be more prevalent among patients with chronic obstructive pulmonary disease.83 There appears to strengthen the negative effect on satisfaction of psychological health. Depression or anxiety, together with another two somatic comorbidities (urogenital disorders, tumors and cancer) negatively affected overall life satisfaction. Other studies with general aging populations have also reported similar comorbidities (urinary incontinence, prostate problems and malignancy) relating to low life satisfaction.15,21,32 However, our findings are based on the older adults with chronic pain. A possible explanation is the potential cause–effect relationship to other factors, such as pain aspects and sleep disorders.
Study Limitations
Several limitations deserve consideration. First, as mentioned above, our cross-sectional analysis cannot draw any conclusion of causality or provide information on the life satisfaction affected by these associated factors over time. Second, the survey had a population-based study design, so it did not cover all in-depth information on the time of comorbidity diagnosis, severity, and progression of chronicity. However, we chose to use the clinical diagnosis rather than only subjective opinions even if this measurement could have missed some undiagnosed conditions. Our trust in medical diagnosis as a reliable information source aimed to capture the comorbidities that received attention from both individuals (to seek health service) and health professionals (to document the medical records). We might have underestimated the burden of self-perceived illness. Third, the information about older adults’ experience of isolation, loneliness, and activity limitation was not adequately collected compared with other studies.21,29,30 We did not analyze these common geriatric and aging challenges deeply in relation to chronic pain and life satisfaction. Nevertheless, some variables, such as marital status, number of trusted friends, and the MPI-leisure index, described to some extent a profile of support from others, social relationships, and activity levels. We are aware that life satisfaction is affected by multifaceted factors and older adults with chronic pain should not be treated as homogenous or a medical entity. The interactions of the aging process, social roles, as well as medical conditions together with chronic pain need to be addressed in pain research.
Conclusion
In this large-scaled population-based study, older adults were generally satisfied or rather satisfied with their lives. Those with chronic pain reported lower life satisfaction, but the difference among chronic pain patients is trivial, except for satisfaction on somatic health. Severe pain had robust negative impacts on all three domains of life satisfaction. Certain lifestyles and several comorbidities significantly affected different domains of life satisfaction. Promoting lifestyle behavior change in patients with chronic pain might lead to being more satisfied with life in old age. To help patients obtain higher life satisfaction, pain management (including non-pharmacological interventions) needs to raise concerns about comorbidities and severe pain.
Ethical Approvals
The study was approved by the Regional Ethics Research Committee in Linköping, Sweden (Dnr: 2012/154-31). Completion of the postal survey was deemed to be agreement of patient informed consent. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors acknowledge and thank the participants. The present study was sponsored by a grant from Grünenthal Sweden AB. The sponsor of the study had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit for publication. The authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Disclosure
Prof. Dr. Björn Gerdle reports grants from Grünenthal Sweden AB, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42(Suppl 1):i1–57. doi:10.1093/ageing/afs199
2. (EC) EC. Healthy ageing in relation to chronic pain in the EU. Systematic Literature Report May 2012 2012.
3. Gerdle B, Bjork J, Henriksson C, Bengtsson A. Prevalence of current and chronic pain and their influences upon work and healthcare-seeking: a population study. J Rheumatol. 2004;31(7):1399–1406.
4. Silvemark AJ, Kallmen H, Portala K, Molander C. Life satisfaction in patients with long-term non-malignant pain-relation to demographic factors and pain intensity. Disabil Rehabil. 2008;30(25):1929–1937. doi:10.1080/09638280701748773
5. Borsbo B, Peolsson M, Gerdle B. The complex interplay between pain intensity, depression, anxiety and catastrophising with respect to quality of life and disability. Disabil Rehabil. 2009;31(19):1605–1613. doi:10.1080/09638280903110079
6. Otones Reyes P, Garcia Perea E, Pedraz Marcos A. Chronic pain and frailty in community-dwelling older adults: a systematic review. Pain Manage Nurs. 2019;20(4):309–315. doi:10.1016/j.pmn.2019.01.003
7. Stalnacke BM. Life satisfaction in patients with chronic pain - relation to pain intensity, disability, and psychological factors. Neuropsychiatr Dis Treat. 2011;7:683–689. doi:10.2147/NDT.S25321
8. Fugl-Meyer AR, Melin R, Fugl-Meyer KS. Life satisfaction in 18- to 64-year-old Swedes: in relation to gender, age, partner and immigrant status. J Rehabil Med. 2002;34(5):239–246. doi:10.1080/165019702760279242
9. Diener E. Well-being (Subjective), psychology of. In: Smelser NJ, Baltes PB, editors. International Encyclopedia of the Social & Behavioral Sciences. Oxford: Pergamon; 2001:16451–16454.
10. Silvemark A, Källmén H, Molander C. Improved life satisfaction and pain reduction: follow-up of a 5-week multidisciplinary long-term pain rehabilitation programme. Ups J Med Sci. 2014;119(3):278–286. doi:10.3109/03009734.2014.908252
11. Fugl-Meyer AR, Bränholm I-B, Fugl-Meyer KS. Happiness and domain-specific life satisfaction in adult northern Swedes. Clin Rehabil. 1991;5(1):25–33. doi:10.1177/026921559100500105
12. Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet (London, England). 2015;385(9968):640–648. doi:10.1016/S0140-6736(13)61489-0
13. Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci. 2010;107(22):9985. doi:10.1073/pnas.1003744107
14. Wittink HM, Rogers WH, Lipman AG, et al. Older and younger adults in pain management programs in the United States: differences and similarities. Pain Med (Malden, Mass). 2006;7(2):151–163. doi:10.1111/j.1526-4637.2006.00113.x
15. Celik SS, Celik Y, Hikmet N, Khan MM. Factors affecting life satisfaction of older adults in Turkey. Int J Aging Human Devel. 2017;87(4):392–414. doi:10.1177/0091415017740677
16. Lim HJ, Min DK, Thorpe L, Lee CH. Multidimensional construct of life satisfaction in older adults in Korea: a six-year follow-up study. BMC Geriatr. 2016;16(1):197. doi:10.1186/s12877-016-0369-0
17. Hsu H-C. Trajectories and covariates of life satisfaction among older adults in Taiwan. Arch Gerontol Geriatr. 2012;55(1):210–216. doi:10.1016/j.archger.2011.08.011
18. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi:10.1016/j.arr.2011.03.003
19. Schafer I, von Leitner E-C, Schon G, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One. 2010;5(12):e15941. doi:10.1371/journal.pone.0015941
20. Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69(2):197–207. doi:10.1037/a0035794
21. Hu SXX, Lei WI, Chao KK, Hall BJ, Chung SF. Common chronic health problems and life satisfaction among Macau elderly people. Int J Nurs Sci. 2016;3(4):367–370. doi:10.1016/j.ijnss.2016.10.004
22. Karadag Arli S, Bakan AB, Varol E, Aslan G. Investigation of pain and life satisfaction in older adults. Geriatr Gerontol Int. 2018;18(1):5–11. doi:10.1111/ggi.2018.18.issue-1
23. Martín-María N, Caballero FF, Moreno-Agostino D, et al. Relationship between subjective well-being and healthy lifestyle behaviours in older adults: a longitudinal study. Aging Ment Health. 2018;1–9.
24. Bicket MC, Mao J. Chronic pain in older adults. Anesthesiol Clin. 2015;33(3):577–590. doi:10.1016/j.anclin.2015.05.011
25. van Hecke O, Torrance N, Smith BH. Chronic pain epidemiology - where do lifestyle factors fit in? Br J Pain. 2013;7(4):209–217. doi:10.1177/2049463713493264
26. Paley CA, Johnson MI. Physical activity to reduce systemic inflammation associated with chronic pain and obesity: a narrative review. Clin J Pain. 2016;32(4):365–370. doi:10.1097/AJP.0000000000000258
27. Ferring D, Balducci C, Burholt V, et al. Life satisfaction of older people in six European countries: findings from the European Study on adult well-being. Eur J Ageing. 2004;1(1):15–25. doi:10.1007/s10433-004-0011-4
28. Yang F, Gu D, Mitnitski A. Frailty and life satisfaction in Shanghai older adults: the roles of age and social vulnerability. Arch Gerontol Geriatr. 2016;67:68–73. doi:10.1016/j.archger.2016.07.001
29. Borg C, Hallberg IR, Blomqvist K. Life satisfaction among older people (65+) with reduced self-care capacity: the relationship to social, health and financial aspects. J Clin Nurs. 2006;15(5):607–618. doi:10.1111/jcn.2006.15.issue-5
30. Wilhelmson K, Fritzell E, Eklund K, Dahlin-Ivanoff S. Life satisfaction and frailty among older adults. Health Psychol Res. 2013;1(3):e32–e32. doi:10.4081/hpr.2013.1515
31. Chokkanathan S, Mohanty J. Health, family strains, dependency, and life satisfaction of older adults. Arch Gerontol Geriatr. 2017;71:129–135. doi:10.1016/j.archger.2017.04.001
32. Yang DC, Lee JD, Huang CC, Shih HI, Chang CM. Association between multiple geriatric syndromes and life satisfaction in community-dwelling older adults: a nationwide study in Taiwan. Arch Gerontol Geriatr. 2015;60(3):437–442. doi:10.1016/j.archger.2015.02.001
33. Bernfort L, Gerdle B, Rahmqvist M, Husberg M, Levin LA. Severity of chronic pain in an elderly population in Sweden–impact on costs and quality of life. Pain. 2015;156(3):521–527. doi:10.1097/01.j.pain.0000460336.31600.01
34. Dragioti E, Larsson B, Bernfort L, Levin LA, Gerdle B. Prevalence of different pain categories based on pain spreading on the bodies of older adults in Sweden: a descriptive-level and multilevel association with demographics, comorbidities, medications, and certain lifestyle factors (PainS65+). J Pain Res. 2016;9:1131–1141. doi:10.2147/JPR.S119845
35. Larsson B, Gerdle B, Bernfort L, Levin LA, Dragioti E. Distinctive subgroups derived by cluster analysis based on pain and psychological symptoms in Swedish older adults with chronic pain - a population study (PainS65+). BMC Geriatr. 2017;17(1):200. doi:10.1186/s12877-017-0591-4
36. Dong HJ, Larsson B, Levin LA, Bernfort L, Gerdle B. Is excess weight a burden for older adults who suffer chronic pain? BMC Geriatr. 2018;18(1):270. doi:10.1186/s12877-018-0963-4
37. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399–2404. doi:10.1016/j.pain.2011.07.005
38. Hirschfeld G, Zernikow B. Variability of “optimal” cut points for mild, moderate, and severe pain: neglected problems when comparing groups. Pain. 2013;154(1):154–159. doi:10.1016/j.pain.2012.10.008
39. Fejer R, Jordan A, Hartvigsen J. Categorising the severity of neck pain: establishment of cut-points for use in clinical and epidemiological research. Pain. 2005;119(1–3):176–182. doi:10.1016/j.pain.2005.09.033
40. Turner JA, Franklin G, Heagerty PJ, et al. The association between pain and disability. Pain. 2004;112(3):307–314. doi:10.1016/j.pain.2004.09.010
41. Jensen M. In: Curtis T, editor. The pain stethoscope: A Clinician’s Guide to Measuring Pain. London: Springer Healthcare Communications; 2011. doi:10.1007/978-1-908517-43-2
42. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi:10.1016/j.ejpain.2005.06.009
43. Grimby-Ekman A, Gerdle B, Bjork J, Larsson B. Comorbidities, intensity, frequency and duration of pain, daily functioning and health care seeking in local, regional, and widespread pain - a descriptive population-based survey (SwePain). BMC Musculoskelet Disord. 2015;16:165. doi:10.1186/s12891-015-0631-1
44. Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24(1):57–65. doi:10.1016/0304-3959(86)90026-6
45. Dragioti E, Larsson B, Bernfort L, Levin LA, Gerdle B. A cross-sectional study of factors associated with the number of anatomical pain sites in an actual elderly general population: results from the PainS65+ cohort. J Pain Res. 2017;10:2009–2019.
46. Persson LG, Lindstrom K, Lingfors H, Bengtsson C. A study of men aged 33–42 in Habo, Sweden with special reference to cardiovascular risk factors. Design, health profile and characteristics of participants and non-participants. Scand J Soc Med. 1994;22(4):264–272. doi:10.1177/140349489402200405
47. Persson LG, Lindstrom K, Lingfors H, Bengtsson C, Lissner L. Cardiovascular risk during early adult life. Risk markers among participants in “Live for Life” health promotion programme in Sweden. J Epidemiol Community Health. 1998;52(7):425–432. doi:10.1136/jech.52.7.425
48. Turk DC, Rudy TE. Towards a comprehensive assessment of chronic pain patients. Behav Res Ther. 1987;25(4):237–249. doi:10.1016/0005-7967(87)90002-7
49. Turk DC, Rudy TE. Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consult Clin Psychol. 1988;56(2):233–238. doi:10.1037/0022-006X.56.2.233
50. Bergstrom G, Jensen IB, Bodin L, Linton SJ, Nygren AL, Carlsson SG. Reliability and factor structure of the Multidimensional Pain Inventory–Swedish Language Version (MPI-S). Pain. 1998;75(1):101–110. doi:10.1016/S0304-3959(97)00210-8
51. Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi:10.1093/sleep/34.5.601
52. Dragioti E, Levin LA, Bernfort L, Larsson B, Gerdle B. Insomnia severity and its relationship with demographics, pain features, anxiety, and depression in older adults with and without pain: cross-sectional population-based results from the PainS65+ cohort. Ann Gen Psychiatry. 2017;16:15. doi:10.1186/s12991-017-0137-3
53. Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–451. doi:10.1007/s00127-006-0051-5
54. Dalgard OS, Bjork S, Tambs K. Social support, negative life events and mental health. Br J Psychiatry. 1995;166(1):29–34. doi:10.1192/bjp.166.1.29
55. Coolican H. Research Methods and Statistics in Psychology.
56. Cohen J. Statistical Power Analysis for the Behavior Sciences.
57. Streiner DLN. G.R. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford: Oxford University Press; 2008.
58. Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. J Interdiscipl Mathematics. 2010;13(3):253–267. doi:10.1080/09720502.2010.10700699
59. O’Brien R. A Caution Regarding Rules of Thumb for Variance Inflation Factors. 412007.
60. Fleiss JLLB, Paik MC. Statistical Methods for Rates and Proportions..
61. Dragioti E, Bernfort L, Larsson B, Gerdle B, Levin LA. Association of insomnia severity with well-being, quality of life and health care costs: a cross-sectional study in older adults with chronic pain (PainS65+). Eur J Pain. 2018;22(2):414–425. doi:10.1002/ejp.1130
62. Ardelt M. Wisdom and life satisfaction in old age. J Gerontol B Psychol Sci Soc Sci. 1997;52b(1):P15–P27. doi:10.1093/geronb/52B.1.P15
63. Acree LS, Longfors J, Fjeldstad AS, et al. Physical activity is related to quality of life in older adults. Health Qual Life Outcomes. 2006;4(1):37. doi:10.1186/1477-7525-4-37
64. El-Gabalawy R, Mackenzie CS, Shooshtari S, Sareen J. Comorbid physical health conditions and anxiety disorders: a population-based exploration of prevalence and health outcomes among older adults. Gen Hosp Psychiatry. 2011;33(6):556–564. doi:10.1016/j.genhosppsych.2011.07.005
65. Gana K, Bailly N, Saada Y, et al. Relationship between life satisfaction and physical health in older adults: a longitudinal test of cross-lagged and simultaneous effects. Health Psychol. 2013;32(8):896–904. doi:10.1037/a0031656
66. Pardal A, Espirito-Santo H, Lemos L, et al. 1556 – social support, mental health, and satisfaction with life in institutionalized elderly. Eur Psychiatry. 2013;28:1. doi:10.1016/S0924-9338(13)76565-9
67. John U, Hanke M, Meyer C, Volzke H, Baumeister SE, Alte D. Tobacco smoking in relation to pain in a national general population survey. Prev Med. 2006;43(6):477–481. doi:10.1016/j.ypmed.2006.07.005
68. Heim N, Snijder MB, Deeg DJ, Seidell JC, Visser M. Obesity in older adults is associated with an increased prevalence and incidence of pain. Obesity. 2008;16(11):2510–2517. doi:10.1038/oby.2008.407
69. Ekholm O, Gronbaek M, Peuckmann V, Sjogren P. Alcohol and smoking behavior in chronic pain patients: the role of opioids. Eur J Pain. 2009;13(6):606–612. doi:10.1016/j.ejpain.2008.07.006
70. Shi Y, Hooten WM, Roberts RO, Warner DO. Modifiable risk factors for incidence of pain in older adults. Pain. 2010;151(2):366–371. doi:10.1016/j.pain.2010.07.021
71. Bromley Milton M, Borsbo B, Rovner G, Lundgren-Nilsson A, Stibrant-Sunnerhagen K, Gerdle B. Is pain intensity really that important to assess in chronic pain patients? A study based on the Swedish Quality Registry for Pain Rehabilitation (SQRP). PLoS One. 2013;8(6):e65483. doi:10.1371/journal.pone.0065483
72. Merrick D, Sundelin G, Stalnacke BM. One-year follow-up of two different rehabilitation strategies for patients with chronic pain. J Rehabil Med. 2012;44(9):764–773. doi:10.2340/16501977-1022
73. Anke A, Damsgard E, Roe C. Life satisfaction in subjects with long-term musculoskeletal pain in relation to pain intensity, pain distribution and coping. J Rehabil Med. 2013;45(3):277–285. doi:10.2340/16501977-1102
74. Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56(5):497–502. doi:10.1016/j.jpsychores.2004.02.010
75. Morone NE, Greco CM, Moore CG, et al. A mind-body program for older adults with chronic low back pain: a randomized clinical trial. JAMA Intern Med. 2016;176(3):329–337. doi:10.1001/jamainternmed.2015.8033
76. Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person.” the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J Pain. 2008;9(9):841–848. doi:10.1016/j.jpain.2008.04.003
77. Rufa A, Beissner K, Dolphin M. The use of pain neuroscience education in older adults with chronic back and/or lower extremity pain. Physiother Theory Pract. 2019;35(7):603–613. doi:10.1080/09593985.2018.1456586
78. Schilling OK, Wahl H-W, Oswald F. Change in life satisfaction under chronic physical multi-morbidity in advanced old age: potential and limits of adaptation. J Happiness Stud. 2013;14(1):19–36. doi:10.1007/s10902-011-9313-3
79. Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. BMJ (Clinical Research Ed). 2015;350:h176.
80. Stalnacke BM. Psychological symptoms in patients with injury-related chronic pain. ISRN Psychiatry. 2012;2012:196069. doi:10.5402/2012/196069
81. Gracely RH, Undem BJ, Banzett RB. Cough, pain and dyspnoea: similarities and differences. Pulm Pharmacol Ther. 2007;20(4):433–437. doi:10.1016/j.pupt.2006.12.005
82. von Leupoldt A, Sommer T, Kegat S, et al. Dyspnea and pain share emotion-related brain network. NeuroImage. 2009;48(1):200–206. doi:10.1016/j.neuroimage.2009.06.015
83. Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58–69. doi:10.1016/j.jpainsymman.2005.06.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.