Back to Journals » Integrated Blood Pressure Control » Volume 14
Factors Associated with Early Postoperative Results of Total Anomalous Pulmonary Venous Connection Repair: Findings from Retrospective Single-Institution Data in Vietnam
Authors Hung DQ, Huy DX, Vo HL , Hien NS
Received 27 February 2021
Accepted for publication 17 May 2021
Published 1 June 2021 Volume 2021:14 Pages 77—86
DOI https://doi.org/10.2147/IBPC.S308778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Turgay Celik
Doan Quoc Hung,1,2 Dinh Xuan Huy,3 Hoang-Long Vo,1,2 Nguyen Sinh Hien3
1Hanoi Medical University, Hanoi, Vietnam; 2Department of Cardiovascular and Thoracic Surgery, Viet Duc University Hospital, Hanoi, Vietnam; 3Hanoi Heart Hospital, Hanoi, Vietnam
Correspondence: Hoang-Long Vo
Hanoi Medical University, No. 01, Ton That Tung Street, Dong Da, Hanoi, Vietnam
Email [email protected]
Introduction: There are scanty reports of the risk factors for pulmonary hypertensive crisis and low cardiac output syndrome after the operative repair of total anomalous pulmonary venous connection (TAPVC). We aim to evaluate early surgical outcomes of TAPVC and risk factors for pulmonary hypertensive crisis and low cardiac output syndrome.
Methods: We conducted a retrospective medical record review for all patients undergoing operative repair of TAPVC within 5 years. Outcome variables included pulmonary hypertensive crisis, low cardiac output syndrome and early mortality.
Results: Of 58 patients, we documented 77.59% supracardiac, 20.69% cardiac and 1.72% mixed site of connection. About 86.21% patients underwent elective surgery, and 13.79% patients required emergency surgery. Incidence rates were 27.59% for pulmonary hypertensive crisis and 6.90% for low cardiac output syndrome. Body weight below 6 kg, pneumonia, tachycardia, hepatomegaly, preoperative pulmonary congestion on chest x-ray, preoperative elevated mean pulmonary artery pressure, preoperative pulmonary venous obstruction, emergency surgery and prolonged aortic cross-clamping time were significant risk factors for postoperative pulmonary hypertensive crisis. Significant risk factors for postoperative low cardiac output syndrome included pneumonia, prolonged duration of preoperative mechanical ventilation and prolonged aortic cross-clamping time.
Conclusion: The early outcome of surgical repair of TAPVC was acceptable, with 96.55% survival rate. This current analysis suggests that a thorough evaluation of all preoperative and operative characteristics is imperative to achieve best medical and surgical outcomes.
Keywords: total anomalous pulmonary venous connection, pulmonary venous obstruction, pulmonary hypertensive crisis, low cardiac output syndrome, congenital heart disease
Introduction
Total anomalous pulmonary venous connection (TAPVC), a rare congenital heart defect, occurs in 1.1–3.0% of infants with cardiovascular malformations. With the advances in surgical techniques and medical management, the outcomes after surgical correction of TAPVC have, in general, improved over the past several decades. Surgical repair remains challenging with an early mortality rate as high as 10.7%,1–3 however, the occurrence rate of another surgical complications of TAPVC repair has recently decreased owing to accumulated knowledge of the disease and advanced perioperative management.4,5
Previous studies have, mostly, reported that post-repair pulmonary venous obstruction (PVO) and death as well as their risk factors. Furthermore, postoperative PVO was found to be an important risk factor for the death in patients undergoing the repair of TAPVC. Though pulmonary hypertensive crises and low cardiac output syndrome are also significant contributors to morbidity and mortality after congenital heart surgery, especially after TAPVC surgical repair, risk factors for these complications are still sparse in the literature. To date, a number of cardiovascular centers in Vietnam have also performed surgical repair of TAPVC; however, there is no convincing evidence regarding operative repair of TAPVC in treating the Vietnamese patients. A number of risk factors for early postoperative results after TAPVC surgical repair were mostly reported in developed countries, but there are still the inconsistencies, difference and inadequacy in input data between the surgical institutions. A preliminary evidence regarding risk factors for pulmonary hypertensive crises and low cardiac output syndrome from a developing country’ clinical experience is a very important contribution to such scanty problems. Hence, the purpose of current study was to evaluate, by a retrospective review of medical records, the early outcomes in surgical management of TAPVC and risk factors for pulmonary hypertensive crisis and low cardiac output syndrome after the repair of TAPVC.
Methods
Study Patients
Patient records at Hanoi Heart Hospital (Hanoi, Vietnam) were queried for all patients who underwent operative repair of TAPVC from January 2014 through December 2019. The Institutional Review Board of Hanoi Medical University approved the study. Before TAPVC surgical repair, informed consents were obtained from all individual participants included in the study. If the participants are under the age of 18, or otherwise legally or medically unable to provide written informed consent, then consent is obtained from their parents or guardian. During study period between January 2014 and December 2019, informed consent was waived owing to the study’s retrospective nature.
Data Collection
We carried out a retrospective medical record review for all patients. All possible risk variables were included on the basis of clinical judgment and the medical record’ availability in our hospital. Demographic data included sex, age, and weight. Clinical variables included clinical symptoms, preoperative mechanical ventilation, x-ray data and preoperative transthoracic echocardiographic data. Surgical variables included type of surgery, cardiopulmonary bypass time, and aortic cross‐clamp time. Postoperative clinical variables included duration of mechanical ventilation, duration of intensive care unit stay, reoperation, pulmonary hypertensive crisis, low cardiac output syndrome, early pulmonary vein stenosis and early death.
Surgical Techniques
All operations were performed under general anesthesia through full median sternotomy. Cardiopulmonary bypass was established via aorto-bicaval cannulation. Myocardial protection was carried on with intermittent antegrade warm blood cardioplegia and systemic hypothermia to 27°C - 32°C. Deep hypothermic circulatory arrest was not used.
Supra-cardiac type. The posterior wall of the left atrium (LA) was anastomosed to the pulmonary venous confluence side-to-side in a transverse fashion. The atrial septal defect (ASD) was then closed through right atriotomy with a pericardial patch to enlarge the LA.
Cardiac type. The ASD was extended through right atriotomy to un-roof the coronary sinus, and was then closed using a pericardial patch to baffle the anomalous veins into the LA.
Mixed type. A combination of the above techniques was used.
Study Definitions
Types of Surgery
Two choices for surgery were suggested in our patient cohort, depending on the physicians’ diagnosis. An elective surgery was defined that the surgery was scheduled in advance, while an emergency surgery was defined as those requiring surgery within 24 hours of the established diagnosis.
Outcome Variables
Pulmonary hypertensive crisis is defined as a mean pulmonary arterial pressure greater than 55 mmHg.6
Low cardiac output syndrome was defined as persistent hypotension, oliguria or anuria, metabolic acidosis, and delayed peripheral capillary refill time with a cardiac output (CO) of less than 2.0 L/min/m2.
Early mortality was defined as death occurring during the same hospital stay after the primary operation.
Statistical Analysis
All data were first performed a visual inspection for coding errors, outliers, or funky distributions. Demographic, clinical, operative, and outcome variables were reported using descriptive statistics. Continuous variables are expressed as the mean, standard deviation (SD) and interquartile range, while categorical variables are expressed as the number and percentage.
We used Fisher’s exact test to compare the differences in categorical variables between elective surgery and emergency surgery. Mann–Whitney U-test and t-test test methodologies were used to compare the differences in continuous variable amongst two types of surgery.
Univariate logistic regression method was applied to identify the variables that were associated with postoperative early results - pulmonary hypertensive crisis and low cardiac output syndrome. Odds ratios with 95% confidence intervals were constructed. The outcome variable is early mortality which does not qualify for established association model. All data were analyzed with Stata® 15 (StataCorp LLC, USA) for Windows.
Results
Preoperative Patient Characteristics
There were 58 selected patients in our study. The mean age was 25.22 months, 39 children (67.24%) aged under 1 years and 8 newborns (13.79%) were in study cohort. The mean weight was 8.66 kg and 27 children (46.55%) weighted less than 6 kg. The most common symptoms were dyspnea in 53.45% of patients, cyanosis in 48.28%, hepatomegaly in 32.76%, tachycardia in 25.86%, and pneumonia in 20.69%. Of the 58 patients, 45 had supracardiac (77.59%), 12 cardiac (20.69%) and 1 mixed (1.72%) site of connection. On the chest x-ray, 48.28% of the patients had pulmonary congestion. 68.97% patients had cardiothoracic ratio of 0.6 or under. The electrocardiogram showed right axis deviation (RAD) in 72.41% patients. Preoperatively, 10.34% of the patients had PVO and 15.52% required mechanical ventilation (Table 1).
 |
Table 1 Preoperative Patient Characteristics Between Elective Surgery and Emergency Surgery |
In this cohort, 50 patients (86.21%) underwent elective surgery and 8 patients (13.79%) required emergency surgery. Preoperatively, significant differences between patient group undergoing elective surgery and patient group requiring emergency surgery were indicated among under-1-year-old group (p = 0.032), mean age (p = 0.0005), body weight below 6 kg (p = 0.001), mean weight (p = 0.0008), preoperative mechanical ventilation (p = 0.015), pneumonia (p = 0.001), tachycardia (p = 0.003), hepatomegaly (p = 0.012), pulmonary congestion on chest x-ray (p = 0.02), preoperative PVO (p = 0.000) and mean left ventricular (LV) diameter (p = 0.0091). Detailed comparisons of the preoperative characteristics between the 2 groups are provided in Table 1.
Operative and Postoperative Characteristics
The overall mean CPB and aortic cross-clamp time were 72.45 ± 32.57 and 47.78 ± 24.64 minutes, respectively. The overall mean mechanical ventilation and intensive care unit stay were 71.28 ± 169.44 hours and 6.67 ± 8.69 days, respectively. No circulatory arrest was required in any patients. Early postoperative complications included pulmonary hypertensive crisis in 27.59% of the patients, low cardiac output syndrome in 6.90%, early post-repair pulmonary vein stenosis in 5.17%, and postoperative bleeding underwent reoperation in 5.17%. Both two early deaths after surgical repair were required preoperative emergency surgery (Table 2).
 |
Table 2 Operative and Postoperative Characteristics Between Elective Surgery and Emergency Surgery |
Comparisons of the operative and postoperative characteristics between the 2 groups are, in detail, provided in Table 2. Between the elective surgery group and emergency surgery group in operative and postoperative parameters, we found significant differences according to aortic cross-clamping time (p = 0.0007), CPB time (p = 0.0001), mechanical ventilation (p = 0.0004), intensive care unit stay (p = 0.0003), LV diameter (p = 0.0231), pulmonary hypertensive crisis (p = 0.03), low cardiac output syndrome (p = 0.000), early post-repair pulmonary vein stenosis (p = 0.047) and early death (p = 0.017).
Risk Factors for Postoperative Pulmonary Hypertensive Crisis
In the univariate analysis, increased risk factors for postoperative pulmonary hypertensive crisis are presented in Table 3. Body weight below 6 kg (OR 5.40, 95% CI 1.48–19.73, p = 0.011), pneumonia (OR 16.71, 95% CI 3.60–77.54, p = 0.000), tachycardia (OR 7.17, 95% CI 2.08–28.66, p = 0.002), hepatomegaly (OR 6.11, 95% CI 1.75–21.37, p = 0.005), preoperative pulmonary congestion on chest x-ray (OR 4.88, 95% CI 1.34–17.74, p = 0.016), preoperative elevated mean pulmonary artery pressure (PAP) (OR 1.20, 95% CI 1.09–1.32, p = 0.000), preoperative PVO (OR 18.64, 95% CI 1.97–176.43, p = 0.011), emergency surgery (OR 5.91, 95% CI 1.22–28.69, p = 0.028) and prolonged aortic cross-clamping (OR 1.03, 95% CI 1.001–1.06, p = 0.041) were risk factors influencing postoperative pulmonary hypertensive crisis.
 |
Table 3 Factors Associated with Postoperative Pulmonary Hypertensive Crisis: Univariate Logistic Analysis |
Risk Factors for Postoperative Low Cardiac Output Syndrome
In Table 4, univariable analysis indicated pneumonia (OR 15, 95% CI 1.40–161.05, p = 0.025), preoperative prolonged mechanical ventilation (OR 24, 95% CI 2.14–269.11, p = 0.01) and prolonged aortic cross-clamping time (OR 1.11, 95% CI 1.01–1.23, p = 0.042) were significant risk factors for postoperative low cardiac output syndrome.
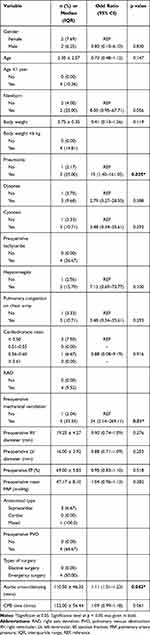 |
Table 4 Factors Associated with Postoperative Low Cardiac Output Syndrome: Univariate Logistic Analysis |
Discussion
Postoperative pulmonary hypertensive crisis is an important problem in the resuscitation after repair of TAPVC. Hypoxemia, metabolic acidosis, pain relief cause insufficient sleep or endotracheal suction all increase the likelihood of pulmonary vascular constriction and trigger pulmonary hypertensive crises. Symptoms of a pulmonary hypertensive crisis include hypotension, severely decreased saturation of oxygen and metabolic acidosis. During pulmonary hypertensive crisis, the maximum pulmonary artery pressure can increase approximately equal to or exceed the aortic pressure, leading to acute RV failure and rapid circulatory collapse. As the literature, the incidence of postoperative pulmonary hypertensive crisis varied depending on the specific population, estimated between 4% and 35%7–9 and the early mortality rate directly caused by pulmonary hypertensive crisis after surgery could be up to 16.7%. In our institution, postoperative pulmonary artery pressure in the patients was continuously monitored via the utility of pulmonary artery catheters that were routinely placed at the time of surgery. Hence, we documented the incidence of postoperative pulmonary hypertensive crisis was 27.59%. Besides, towards the univariate association analysis based on the distribution of post-repair pulmonary hypertensive crisis, we saw body weight below 6 kg, pneumonia, tachycardia, hepatomegaly, preoperative pulmonary congestion on chest x-ray, preoperative elevated mean PAP, preoperative PVO, emergency surgery and prolonged aortic cross-clamping time were significant associated with postoperative pulmonary hypertensive crisis. In fact, the risk factors for pulmonary hypertensive crisis after TAPVC repair were scarce according to reported literature. Importantly, for those suffering from postoperative pulmonary hypertensive crisis, we actively used the classic regimen to prevent and treat postoperative pulmonary hypertensive crisis, with the elimination of provoking factors that can trigger pulmonary hypertensive crisis, the use of deep sedation, the use of muscle relaxants, and the use of vasopressors. Especially, Milrinone 0.5mcg/kg/min was proposed as a common treatment for the patients documented postoperative pulmonary hypertensive crisis. In several severe cases, we used Epinephrine or Norepinephrine in combination because Milrinone increased the inotropic effects of Epinephrine. Milrinone can cause severe systemic hypotension, so the patients were closely monitored after operation for timely treatment. After extubation, the use of Revatio was indicated to aid in long-term reduction in pulmonary arterial pressure, and also avoid reactive pulmonary vasoconstriction as stopping using Milrinone. All responded well to the above treatment as demonstrated by a fall in their mean pulmonary pressure. Pulmonary artery catheter was withdrawn at 48 hours and 72 hours postoperatively once haemodynamic stability and without thrombotic disorders. Although the routine use of inhaled nitric oxide (NO) was proved as a safe an effective therapy to reduce the risk of pulmonary hypertensive crisis with no toxic effects, the NO was not used in our medical setting due to the inconsistency and difficulty in inadequate parameter assessment for the patients before using NO.
Low cardiac output syndrome is a common problem after open-heart surgery with many different groups of causes including reduction in the force developed by heart muscle after surgery due to the damage to heart muscle, excessive systemic inflammatory response after extracorporeal circulation or cardiomyoprotection, residual lesions reducing LV filling, and diastolic heart failure due to small LV diameter (only evaluated by LV internal diameter in diastole in our institution).6 In congenital heart surgery, especially after operative repair of TAPVC, the problem of small left ventricle causing postoperative low cardiac output syndrome was mentioned by Graham.10 However, in our institution, we believe that “the small left ventricle before surgery is relative” for the following two reasons: (i) the left ventricle itself in TAPVC does not have physical damage that reduces LV diameter, (ii) LV diameter is small because the pulmonary venous blood flow back to the left ventricle is incomplete, furthermore, due to the large dilated right ventricle pressing on the left ventricle. Postoperatively, apart from the complete return of pulmonary venous blood to the left ventricle, there is no longer RV pressure on the left ventricle. Therefore, diastolic heart failure after surgical repair is excluded. Similar to previous reports,11,12 we found there was a significant increase in mean LV diameter between pre- and post-operation (19.50 ± 6.20 mm vs 23.33 ± 6.46 mm). Although there were no cases of small LV diameter in this study, low cardiac output syndrome was still diagnosed in 4 patients (6.90%). The low incidence of postoperative low cardiac output syndrome in our cohort (4.90%) was consistent with the recent studies.5,13 4 cases with low cardiac output syndrome may be involved in cardiomyoprotection during surgery or an excessive systemic inflammatory response in the first hours after surgery.
Several single-institution retrospective studies have shown that the survival rate after TAPVC repair has generally improved over the past several decades.5,14,15 In our study, the overall early mortality occurred in 2 (3.45%) patients within 30 days after the initial operation. The current mortality rate agrees with the recent reported study by Takeaki Harada (2.7%)5 or Keyan Zhao (4.9%).16 In our study, 2 deaths after TAPVC repair were under 12 months old, weighing less than 5 kg, having preoperative obstruction, required emergency surgery, undergoing prolonged aortic cross-clamping time and CPB time, occurred postoperative pulmonary hypertensive crisis, occurred early post-repair pulmonary vein stenosis reoperated and undergoing prolonged postoperative mechanical ventilation. Since there are only 2 deaths, we are unable to identify risk factors for early mortality in patients after surgical repair of TAPVC. In resource-scarce conditions in clinical practice from Vietnam, the above characteristics in 2 dead cases drawn from the present cohort can enable to more solidly contribute to numerous previous evidence regarding the increased risk factors for early mortality.5,13,16–18
We would like highlight that the current scanty evidence preliminarily explored risk factors for pulmonary hypertensive crisis and low cardiac output syndrome. Although this cohort was one of the first largest series of TAPVC cases from Vietnam, this study, which was based on a 5-year single-institution experience, has certain limitations with limited statistical power by sample size. A relatively small population need to be highlighted from this retrospective review of medical records and the present result did not enable to represent those of other centers. Because of the absence of several information in the patient medical records, this study was incapable of determining the levels of obstruction in the patients with PVO as well as the cases with pulmonary arterial hypertension who developed LCOS. According to the study protocol, patients were followed during the same hospital stay after the primary operation; hence, intermediate and long-term results will be reported separately due to the inconsistency of study variables among postoperatively followed-up patients. Besides, continued evaluation is needed to further understand mortality outcome associated with postoperative time.
Conclusions
As seen in our cohort, the early outcome of surgical repair of TAPVC was acceptable, with 96.55% survival rate. We, postoperatively, documented the incidence rates of pulmonary hypertensive crisis and low cardiac output syndrome were 27.59% and 6.90%, respectively. According to our study, body weight below 6 kg, pneumonia, tachycardia, hepatomegaly, preoperative pulmonary congestion on chest x-ray, preoperative elevated mean PAP, preoperative PVO, emergency surgery and prolonged aortic cross-clamping time were significant risk factors for postoperative pulmonary hypertensive crisis. Significant risk factors for postoperative low cardiac output syndrome included pneumonia, prolonged duration of preoperative mechanical ventilation and prolonged aortic cross-clamping time. This current analysis suggests a thorough evaluation of all preoperative and operative characteristics is imperative to achieve best medical and surgical outcomes.
Code Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Board of the Hanoi Medical University.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Friesen CLH, Zurakowski D, Thiagarajan RR, et al. Total anomalous pulmonary venous connection: an analysis of current management strategies in a single institution. Ann Thorac Surg. 2005;79(2):596–606. doi:10.1016/j.athoracsur.2004.07.005
2. Morales DLS, Braud BE, Booth JH, et al. Heterotaxy patients with total anomalous pulmonary venous return: improving surgical results. Ann Thorac Surg. 2006;82(5):1621–1628. doi:10.1016/j.athoracsur.2006.05.053
3. Kelle AM, Backer CL, Gossett JG, et al. Total anomalous pulmonary venous connection: results of surgical repair of 100 patients at a single institution. J Thorac Cardiovasc Surg. 2010;139(6):1387–1394. e3. doi:10.1016/j.jtcvs.2010.02.024
4. Matsuhisa H, Oshima Y, Higuma T, et al. Computed tomography-based surgical strategy for total anomalous pulmonary venous connection. Eur J Cardio-Thoracic Surg. 2020;58(2):237–245. doi:10.1093/ejcts/ezaa028
5. Harada T, Nakano T, Oda S, et al. Surgical results of total anomalous pulmonary venous connection repair in 256 patients. Interact Cardiovasc Thorac Surg. 2019;28(3):421–426. doi:10.1093/icvts/ivy267
6. Shah P. Manual of Pediatric Cardiac Intensive Care. JP Medical Ltd; 2013.
7. Gal TJ, Cooperman LH. Hypertension in the immediate postoperative period. Br J Anaesth. 1975;47(1):70–74. doi:10.1093/bja/47.1.70
8. Halpern NA, Alicea M, Krakoff LR, et al. Postoperative hypertension: a prospective, placebo-controlled, randomized, double-blind trial, with intravenous nicardipine hydrochloride. Angiology. 1990;41(11 Pt 2):992–1004.
9. Prys-Rroberts C. Anaesthesia and hypertension. Br J Anaesth. 1984;56(7):711–724. doi:10.1093/bja/56.7.711
10. Graham TP, Jarmakani JM, Canent RV
11. Ross FJ, Joffe D, Latham GJ. Perioperative and anesthetic considerations in total anomalous pulmonary venous connection. In: Seminars in Cardiothoracic and Vascular Anesthesia. Los Angeles, CA: SAGE Publications Sage CA; 2017.
12. Cheung Y, Lun KS, Chau AK, et al. Fate of the unligated vertical vein after repair of supracardiac anomalous pulmonary venous connection. J Paediatr Child Health. 2005;41(7):361–364. doi:10.1111/j.1440-1754.2005.00632.x
13. Elamry E, Alkady HM, Menaissy Y, et al. Predictors of in-hospital mortality in isolated total anomalous pulmonary venous connection. Heart Surg Forum. 2019;22(3):E191–E196. doi:10.1532/hsf.2415
14. Van de Wal H, Hamilton D, Godman M, et al. Pulmonary venous obstruction following correction for total anomalous pulmonary venous drainage: a challenge. Eur j Cardio-Thoracic Surg. 1992;6(10):545–549. doi:10.1016/1010-7940(92)90006-J
15. Louis JDS, Harvey BA, Menk JS, et al. Repair of “simple” total anomalous pulmonary venous connection: a review from the pediatric cardiac care consortium. Ann Thorac Surg. 2012;94(1):133–138. doi:10.1016/j.athoracsur.2012.03.006
16. Zhao K, Wang H, Wang Z, et al. Early-and intermediate-term results of surgical correction in 122 patients with total anomalous pulmonary venous connection and biventricular physiology. J Cardiothorac Surg. 2015;10(1):172. doi:10.1186/s13019-015-0387-6
17. Lemaire A. Total anomalous pulmonary venous connection: a 40 years’ experience analysis. Thorac Cardiovasc Surg. 2017;65(01):009–017.
18. Shi G, Zhu Z, Chen J, et al. Total anomalous pulmonary venous connection: the current management strategies in a pediatric cohort of 768 patients. Circulation. 2017;135(1):48–58. doi:10.1161/CIRCULATIONAHA.116.023889
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
