Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Factors Associated with Chronic Obstructive Pulmonary Disease: A Hospital-Based Case–Control Study
Authors Twinamasiko B , Mutekanga A , Ogueri O, Kisakye NI, North CM, Muzoora C, Muyanja D
Received 21 June 2023
Accepted for publication 17 October 2023
Published 10 November 2023 Volume 2023:18 Pages 2521—2529
DOI https://doi.org/10.2147/COPD.S426928
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Bruce Twinamasiko,1 Andrew Mutekanga,1 Olilanya Ogueri,2 Nakitto Irene Kisakye,3 Crystal M North,4,5 Conrad Muzoora,1 Daniel Muyanja1
1Department of Internal Medicine, Mbarara University of Science and Technology, Mbarara, Uganda; 2Science Department, Phillips Academy, Andover, MA, USA; 3Department of Public Health, Kabale University, Kabale, Uganda; 4Division of Pulmonary and Critical Care Medicine, Massachusetts General Hospital, Boston, MA, USA; 5Department of Environmental Health, Harvard T.H. Chan School of Public Health, Boston, MA, USA
Correspondence: Bruce Twinamasiko, Tel +256772382195, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide. In this paper, we determined risk factors for COPD among patients presenting to pulmonology and medical outpatients’ clinics of Mbarara Regional Referral Hospital (MRRH).
Methods: In this case–control study, cases were patients with COPD confirmed by spirometry and controls were those with normal spirometry. The two groups were matched by age and gender.
Results: We enrolled 123 participants, of whom 41 were cases and 82 controls. A total of 51 women (41.5%) and 72 men (58.5%), of whom 25 were male cases (61%) and 47 were male controls (57%), were included. The results of our study suggest that the variables associated with the presence of COPD among participants attending MRRH were a history of having ever smoked and a prior history of atopy. This brings to our attention the fact that smoking remains a major risk factor for COPD in this setting, just as it is in developed countries.
Conclusion: Our study has shown that the factors associated with COPD are smoking and a history of atopy. Patients with a history of asthma and tuberculosis are also probably more likely to develop COPD than those without similar disease conditions.
Keywords: chronic bronchitis, emphysema, asthma, smoking
Introduction
Chronic obstructive pulmonary disease (COPD) is defined as a chronic respiratory disorder marked by persistent respiratory symptoms and airflow limitations. COPD significantly affects general well-being, which is important in view of its increasing incidence and associated morbidity and mortality. In COPD, the normal airflow is irritated by episodes of respiratory symptoms, with deteriorating intensifications that add to disease progression.1
Airflow obstruction and persistent respiratory symptoms are the hallmarks of COPD. Tobacco smoking is the main cause of COPD, but not the only one.2 A post-bronchodilator forced expiratory volume in one second/forced vital capacity (FEV1/FVC) ratio under 0.70 is expected for a diagnosis of COPD.3 A multifaceted management strategy that includes counseling and pharmacotherapy for smoking cessation, pulmonary rehabilitation, the treatment of comorbidities, the administration of influenza and pneumococcal immunizations, and the prescription of long-term oxygen therapy in hypoxemic patients should be complemented by inhaler therapy.4
COPD is one of the leading causes of death worldwide.5 As well as being one of the most significant causes of morbidity worldwide, COPD also has a significant impact on the patient’s health and socioeconomic situation.6 During 2005 to 2013, disability-adjusted life-years (DALYs) due to COPD ranked from eight to fifth among all causes.7
The burden of COPD in sub-Saharan Africa has been poorly studied. The main reasons why COPD prevalence studies are rare are the general lack of standardized epidemiological instruments and the need to perform good-quality post-bronchodilator spirometry, which requires considerable expertise and experience.8 In low- and middle-income countries (LMICs), COPD is recognized as a major health issue. There were 3.8 million deaths due to COPD in 2019, with around 90% of these occurring in LMICs. The WHO assesses that around 251 million individuals have COPD overall and that this burden is increasing9. Smoking is the main risk factor for COPD.10 The burden in LMICs is thought to be higher than in developed countries owing to relatively low COPD awareness. Although the use of biomass fuel has been suggested as a significant risk factor,11 any proof to support this declaration is currently weak. Other risk factors include exposure to dust and a history of serious lung infections, such as tuberculosis (TB).12 A study in Uganda reported that COPD was more prevalent in young people and women who were non-smokers.13 This further suggests that this population may be exposed to non-traditional COPD risk factors which have not been studied in depth.
This case–control study, therefore, aimed to determine risk factors for COPD among patients attending pulmonology and medical outpatients’ clinics of Mbarara Regional Referral Hospital (MRRH).
Materials and Methods
In this case–control study, cases were patients with COPD confirmed by spirometry using the NHANES III prediction equation14 and controls were those with normal spirometry. The two groups were matched by age and gender.
The study included adults aged 18 years and above presenting to pulmonology and medical outpatients’ clinics of MRRH in south-western Uganda. The participants in the control group were individuals who presented to medical outpatients’ clinics of MRRH, who had no history of respiratory symptoms. Individuals in the control group were aged 18 years or more, with normal spirometry, matched with cases by age (±5 years) and gender. We enrolled two controls for every case. Cases also completed 6 minute walk tests.
Our case–control study aimed to determine whether COPD is associated with past exposure to risk factors such as cigarette smoking. Cases were patients with COPD and controls were those without COPD or any respiratory symptoms enrolled from medical outpatient clinics. In a single study by Manoj Kumar Meghwani from India in 2013,15 36.3% of participants were exposed to cigarette smoking in the control group. We wished to detect an odds ratio of 3 with a power of 80%, and recruited two controls for each case.
Ethical Considerations
The research proposal was presented to and approved by the following bodies: the Department of Internal Medicine, the Faculty Research Ethics Committee of Mbarara University (FREC MUST), and the Institutional Research Ethics Committee. Informed consent was obtained from each study participant in the form of a fingerprint or signature. The right to withdraw from participation in the study without any consequences to the participant was guaranteed from the start. Study data were kept under lock and key, and only responsible clinicians were able to access patient information for clinical purposes. Patient identification numbers were used for data entry to ensure confidentiality. The investigation was low risk as no substances were administered to patients in any experimental manner. In addition, patients benefited from free spirometry work-up during this study. The study was conducted according to the principles of the Declaration of Helsinki.
Results
Description of Study Participants
We enrolled 123 participants, of whom 41 were cases and 82 controls. Participants’ baseline characteristics are shown in Table 1. A total of 51 women (41.5%) and 72 men (58.5%), of whom 25 were male cases (61%) and 47 were male controls (57%), were included. These proportions were compared by the chi-squared test, giving a p-value of 0.698, implying that the groups (both cases and controls) were similar for the gender variable. The lower limit for age was 27 years and the upper limit was 90 years. The median age for cases was 70 years (25th percentile 56 and 75th percentile 78 years). Controls had a median age of 68 years (25th percentile 55 and 75th percentile 77 years). Twenty-five cases (61%) and 48 controls (59%) were subsistence farmers; when comparisons between different occupations were made using the chi-squared test, a p-value of 0.968 was determined, suggesting a similar distribution of occupations among cases and controls. The other occupations included teachers, engineers, and boda riders.
 |
Table 1 Demographic Characteristics |
In total, 22 cases (53%) and 50 controls (61%) were from the districts of Mbarara and Isingiro. The “others” category included participants from the districts of Kiruhura, Sheema, Kabale, etc. A p-value of 0.221 was suggestive of similar cases and controls for the address variable.
The median body mass index (BMI) for cases was 21 kg/m2 (25th percentile 19 and 75th percentile 30 kg/m2). Controls had a median BMI of 22 kg/m2 (25th percentile 19 and 75th percentile 25 kg/m2). The median pre-bronchodilator FEV1/FVC was 56 for cases (25th percentile 50 and 75th percentile 63). Controls had a median pre-bronchodilator FEV1/FVC of 77 (25th percentile 72 and 75th percentile 81). A p-value of 0.000 was determined, suggesting a difference between groups (cases and controls) for the pre-bronchodilator FEV1/FVC variable. The median BODE index was 3 (25th percentile 1 and 75th percentile 5). The median percentage 4-year survival for the cases as derived from the BODE index was 67% (25th percentile 57 and 75th percentile 80).
Medical and Smoking Status
A summary of physician-diagnosed medical conditions and smoking exposure among cases and controls is presented in Table 2. Only four cases (10%) reported being positive for HIV, and six controls (7%) also reported living with HIV. A p-value of 0.639 was suggestive of having similar groups (cases and controls) with the HIV-positive variable. Six cases (15%) and two controls (2%) reported a history of a prior diagnosis of asthma. There was a difference in reported asthma between cases and controls, with a p-value of 0.010. Twenty cases (49%) and 19 controls (23%) reported a history of having ever had physician-diagnosed atopy. Three cases (7%) and one control (1%) reported a positive history of TB disease.
 |
Table 2 Medical and Smoking History |
In total, 28 cases (68%) and 34 controls (41%) reported having ever smoked tobacco products; and using the chi-squared test, there was a difference between the groups (cases and controls) regarding having ever used tobacco products. The median age at the start of smoking was 15 years for cases (25th percentile 12 and 75th percentile 18 years). Controls also had a median of 15 years, but with 25th percentile of 12 and 75th percentile of 20 years. The median duration of smoking was 35 years (25th percentile 18 and 75th percentile 45 years) for cases, while controls had a median duration of 26.5 years (25th percentile 10 and 75th percentile 38 years). There were more current smokers in cases [12 (29%)] than in controls [10 (12%)]. Comparing the two groups with a chi-squared test for the current-smoking variable, a p-value of 0.02 was found, suggesting a difference between the groups (cases and controls).
Biomass Exposure and Environmental Pollution
A summary of the findings from the analysis of environmental exposure variables among cases and controls is presented in Table 3. Participants reported mean outdoor environmental exposure of 10±2.7 hours for cases and 11±2.4 hours for controls. Comparing this variable between the groups (cases and controls) using the Student’s t-test, a p-value of 0.009 suggested a difference in the mean between the groups. The median duration of time spent cooking was 2 hours for cases (25th percentile 0 and 75th percentile 4 hours), while controls had a median duration of 1 hour (25th percentile 0 and 75th percentile 3 hours). Both cases and controls spent a median duration of 4 hours digging. The primary sources of fuel for cooking were firewood and charcoal: 34 cases (83%) and 67 controls (82%) used firewood, while seven cases (17%) and 15 controls (18%) used charcoal as a primary cooking fuel. The mean duration of primary fuel use was 45±17 years for cases and 42±16 years for controls. There was no difference in the mean duration of primary fuel use among cases and controls (p=0.375). In total, 21 cases (51%) and 44 controls (54%) reported having been primarily responsible for cooking in their homes. The median age at the start of cooking was 10 years (25th percentile 8 and 75th percentile 18 years) for cases, while controls reported a median of 12 years (25th percentile 10 and 75th percentile 15 years). The mean time spent by cases inside the kitchen daily was 3.8±2.2 hours, while controls spent 3.5±1.9 hours. Indoor cooking smoke exposure per year was calculated for those participants who reported being primarily responsible for cooking in their homes. Five cases (26%) and five controls (13%) were exposed to less than 500 hours of smoke per year, whereas 14 cases (74%) and 34 controls (87%) were exposed to more than 500 hours of indoor smoke per year. In addition, 24 cases (59%) and 48 controls (59%) reported having always burnt trash in their homes and gardens. The primary source of lighting in homes was reported as kerosene lamps, candles, and electricity: 33 cases (81%) and 65 controls (79%) used kerosene lamps. There was no difference between the groups (cases and controls) with regard to the primary source of light in the home (p=0.899).
 |
Table 3 Biomass Exposure and Environmental Pollution |
Factors Associated with COPD
The results of factors associated with COPD explored in the bivariate analysis model are summarized in Table 4. Cases who had a history of physician-diagnosed asthma were six (95% CI 1.21–29.73) times more likely to have COPD compared to gender- and age-matched controls. Cases with a prior history of atopy diagnosis were 3.3 (95% CI 1.39–7.72) times more likely to have COPD compared to controls. Cases who reported a history of smoking were 4.4 (95% CI 1.59–11.99) times more likely to have COPD than their matched controls. Cases who reported a history of TB disease were 5.9 (95% CI 0.62–57.68) times more likely to have COPD compared to controls, but the results did not show statistical significance. A similar trend was seen in cases who were subsistence farmers, those were using kerosene lamps as the primary source of light in their homes, and those who reported firewood use, but there was no proof of statistical significance.
 |
Table 4 Results of Bivariate Analysis Showing Risk Factors for COPD |
In the multivariate analysis (Table 5), our final model consisted of covariates with a p-value of ≤0.2. Cases who reported a history of smoking were 3.5 (95% CI 1.20–10.10) times more likely to have COPD and those with a history of atopy were 3.0 (95% CI 1.19–7.72) times more likely to have COPD than age- and gender-matched controls. Cases with a positive history of asthma and those who reported a history of TB were more likely to have COPD than matched controls, but this result did not show statistical significance.
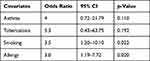 |
Table 5 Results of Multivariate Analysis Showing Risk Factors for COPD |
Discussion
The results of our study suggest that the variables associated with the presence of COPD among participants attending MRRH were a history of having ever smoked and a prior history of atopy. This brings to our attention the fact that smoking remains a major risk factor for COPD in our setting, just as it is in developed countries.
The positive association between COPD and smoking is historical and not surprising, even in our setting. Several other studies have documented an association between smoking and COPD in sub-Saharan Africa. Most of these studies have been cross-sectional in design. The FRESH AIR study, from Uganda, reported similar findings,13 as did a study conducted in Malawi.16 A study conducted in Kigali, Rwanda, also found a significant association between COPD and smoking.17
Our study found an association between atopy and COPD, which was an interesting one. The association remained statistically significant even in the final multivariate model. Although most literature has stated atopy to be a risk factor for asthma, there is evidence to suggest a high prevalence of atopy in patients with COPD and thus an association between COPD and atopy.18 In fact, COPD patients with atopy have been found to show greater improvements from using inhaled steroids than those without a history of atopy.19
The possibility of other non-traditional factors contributing to the COPD burden in our setting, as we had hypothesized, cannot be ignored. We were, however, not able to prove a statistically significant association between COPD and factors such as asthma history, HIV infection, TB disease history, and biomass exposure. However, there was a trend towards these factors increasing the likelihood of COPD. A study conducted among people living with HIV in south-western Uganda suggested a higher prevalence of COPD in HIV-positive patients and those who had a history of TB, but because of low numbers, it was not powered to measure associations.20 A systematic review carried out in 2013 also suggested a positive association between TB and COPD.21
We had hypothesized a possible association between biomass exposure and COPD; however, we were not able to obtain a statistically significant relationship in our analysis. A previous study conducted in rural Uganda reported high levels of PM2.5, which is potentially a surrogate measure for indoor air pollution due to biomass exposure.22 Whether this exposure to high levels of PM2.5 contributes to COPD independently of other exposures is still unknown, and there are ongoing follow-up studies using real time PM2.5 monitors that hope to answer this question. A systematic review and meta-analysis in 2009, which involved 23 studies, examined the risk of developing COPD from indoor air pollution, and reported an increased likelihood of COPD from exposure to wood smoke, biomass, or coal.23 Therefore, although we were not able to find a significant association between biomass exposure and COPD in our study, there is supportive evidence to suggest an association.
Our study has several limitations. It was powered to mainly answer the primary objective, which was the association between smoking and COPD, and this may have limited the power to detect other associations. The sample size was very small because of the nature of cases (rare to find), and the study duration was limited. Since it was a hospital-based case–control study focusing on COPD cases coming to the chest clinic, it is very hard to generalize the findings to the community. Lastly, this being a case–control study, it may be subject to recall bias.
Despite these limitations, our study has an important strength. This is the first hospital-based case–control study investigating COPD risk factors in Uganda. It could lay the groundwork for larger studies to be conducted in similar settings.
Conclusion
Our study has shown that the factors associated with COPD are smoking and a history of atopy. Patients with a history of asthma and tuberculosis are also probably more likely to develop COPD than those without similar disease conditions.
Data Sharing Statement
The datasets used during this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Mbarara University of Science and Technology’s faculty review board and institutional ethics review board. Informed written consent was obtained from every participant before recruitment to the study. All methods in this study were carried out in accordance with relevant guidelines and regulations.
Acknowledgments
We thank the study team, hospital administration, and the clinicians and nurses who agreed to be part of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received by the authors of this study.
Disclosure
The authors declare that they have no competing interests.
References
1. Hogea SP, Tudorache E, Fildan AP, Fira-Mladinescu O, Marc M, Oancea C. Risk factors of chronic obstructive pulmonary disease exacerbations. Clin Respir J. 2020;14(3):183–197. PMID: 31814260. doi:10.1111/drj.13129
2. Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of chronic obstructive pulmonary disease.Am J Respir Crit Care Med. 2010, 182(5):693–718. doi:10.1164/rccm.200811-1757ST
3. Richter DC, Joubert JR, Nell H, Schuurmans MM, Irusen EM. Diagnostic value of post-bronchodilator pulmonary function testing to distinguish between stable, moderate to severe COPD and asthma. Int J Chron Obstruct Pulmon Dis. 2008;3(4):693–699. doi:10.2147/copd.s948
4. Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173(3):ITC17–ITC32. PMID:32745458. doi:10.7326/AITC202008040
5. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–582. PMID: 28128970. doi:10.1164/rccm.201701-0218PP
6. Weissmann N. Chronic obstructive pulmonary disease and pulmonary vascular disease. A comorbidity? Ann Am Thorac Soc. 2018;15(Suppl 4):S278–S281. PMID: 30759003; PMCID: PMC6944394. doi:10.1513/AnnalsATS.201808-532MG
7. GBD 2019 Disease and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
8. Salvi SS, Manap R, Beasley R. Understanding the true burden of COPD: the epidemiological challenges. Prim Care Respir J. 2012;21(3):249–251. PMID: 22885564; PMCID: PMC6547972. doi:10.4104/pcrj.2012.00082
9. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi:10.1016/S0140-6736(14)61682-2
10. Awokola BI, Amusa GA, Jewell CP, et al. Chronic obstructive pulmonary disease in sub-Saharan Africa. Int J Tuberc Lung Dis. 2022;26(3):232–242. PMID: 35197163; PMCID: PMC8886964. doi:10.5588/ijtld.21.0394
11. Capistrano S, van Reyk D, Chen H and Oliver B. Evidence of Biomass Smoke Exposure as a Causative Factor for the Development of COPD. Toxics. 2017;5(4):36. doi: 10.3390/toxics5040036
12. Burney P, Patel J, Minelli C, et al. Prevalence and population attributable risk for chronic airflow obstruction in a large multinational study. Am J Respir Crit Care Med. 2020;203(11):1353–1365. doi:10.1164/rccm.202005-1990OC
13. Van Gemert F, Kirenga B, Chavannes N, et al. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. Lancet Glob Health. 2015;3(1):e44–e51. PMID: 25539969. doi:10.1016/S2214-109X(14)70337-7
14. Pellegrino R. Interpretative strategies for lung function tests. European Respiratory Journal. 2005;26(5): 948–968. doi:10.1183/09031936.05.00035205
15. Meghwani MK, Tiwari HC, Mishra R and Kumar S. Chronic Obstructive Pulmonary Disease and Its Risk Factors: A Case Control Study. JEMDS. 2013;2(34):6382–6386. doi:10.14260/jemds/1148
16. Njoroge MW et al . Changing lung function and associated health-related quality-of-life: A five-year cohort study of Malawian adults. eClinicalMedicine. 2021;41:101166. doi: 10.1016/j.eclinm.2021.101166
17. Musafiri S, Joos G, Van Meerbeeck JP. Asthma, atopy and COPD in sub-Saharan countries: the challenges. East Afr J Public Health. 2011;8(2):161–163. PMID: 22066305.
18. Fattahi F, ten Hacken NH, Löfdahl CG, et al. Atopy is a risk factor for respiratory symptoms in COPD patients: results from the EUROSCOP study. Respir Res. 2013;14(1):10. PMID: 23356508; PMCID: PMC3599617. doi:10.1186/1465-9921-14-10
19. Jamieson DB, Matsui A, Belli MC, et al. Effects of allergic phenotype on respiratory symptoms and exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(2):187–192. doi:10.1164/rccm.201211-2103OC
20. North CM, Allen JG, Okello S, et al. HIV infection, pulmonary tuberculosis, and COPD in Rural Uganda: a cross-sectional study. Lung. 2018;196(1):49–57. PMID: 29260309; PMCID: PMC6261662. doi:10.1007/s00408-017-0080-8
21. Allwood BW, Myer L, Bateman ED. A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration. 2013;86(1):76–85. doi:10.1159/000350917
22. Muyanja DJ, Allen J, Vallarino L, et al. Kerosene lighting contributes to household air pollution in rural Uganda. Indoor Air. 2017;27(5):1022–1029. doi:10.1111/ina.12377
23. Kurmi OP, Semple S, Simkhada P, Smith WCS, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65(3):221–228. doi:10.1136/thx.2009.124644
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
