Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Factors associated with antenatal depression in pregnant Korean females: the effect of bipolarity on depressive symptoms
Authors Park CM, Seo H, Jung Y, Kim M, Hong S, Bahk W, Yoon B, Hur MH, Song JM
Received 10 March 2014
Accepted for publication 17 April 2014
Published 9 June 2014 Volume 2014:10 Pages 1017—1023
DOI https://doi.org/10.2147/NDT.S63855
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Chul Min Park,1 Hye-Jin Seo,2 Young-Eun Jung,3 Moon-Doo Kim,3 Seong-Chul Hong,4 Won-Myong Bahk,5 Bo-Hyun Yoon,6 Min Hee Hur,7 Jae Min Song3
1Department of Obstetrics and Gynecology, School of Medicine, Jeju National University, Jeju, 2Department of Psychiatry, Yeonkang Hospital, Jeju, 3Department of Psychiatry, 4Department of Preventive Medicine, School of Medicine, Jeju National University, Jeju, 5Department of Psychiatry, Yeouido St Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, 6Department of Psychiatry, Naju National Hospital, Naju, 7School of Medicine, Jeju National University, Jeju, Korea
Background: This cross-sectional study sought to identify factors associated with antenatal depression in pregnant Korean females, including sociodemographic parameters, social support, social conflict, and bipolarity.
Methods: Eighty-four pregnant women were recruited to complete questionnaires on sociodemographic factors, obstetric history, depressive symptoms, and bipolarity. Depressive symptoms were assessed using the Korean version of the Edinburgh Postnatal Depression Scale. Bipolarity was assessed using the Korean version of the Mood Disorder Questionnaire.
Results: Nineteen participants (22.6%) had positive Mood Disorder Questionnaire scores, suggesting the presence of bipolarity, and were significantly more likely to score high on the Edinburgh Postnatal Depression Scale. Antenatal depression was associated with bad marital communication and marital dissatisfaction.
Conclusion: These results suggest that spousal interactions play a significant role in antenatal depression, and pregnant women with bipolarity may be more depressed than those without bipolarity.
Keywords: antenatal depression, bipolarity, pregnancy, Korea
Introduction
Pregnancy is associated with many psychological, physical, and hormonal changes, during which women are vulnerable to psychiatric illness, particularly depression. Major depressive disorder is found in 8%–12% of all pregnant women, and clinically significant depressive symptoms that do not meet the criteria for major depressive disorder are present in about 20%.1
Antenatal depression, ie, depression during pregnancy, can increase the incidence of other psychopathologies. Women with antenatal depression have a 6.5-fold increased risk of postpartum depression,2 and about one half of women with depressed mood during pregnancy also experience depressed mood postpartum, with about one third of cases of postnatal depression starting during pregnancy.3,4
Untreated antenatal depression has adverse outcomes for both the fetus and mother. Complications of antenatal depression include inadequate weight gain, increase in substance abuse, lack of prenatal care, low infant birth weight, decreased Apgar scores, decreased fetal head circumference, and premature birth.5–7 Antenatal depression may also negatively affect the emotional and cognitive development of the fetus.8 A longitudinal study demonstrated that children of mothers who were depressed during pregnancy were more likely to be difficult to soothe as babies and to be hyperactive by 4 years of age.9 Because antenatal depression has these unfavorable outcomes, it must be identified and treated. Despite the potential clinical impact of antenatal depression, the majority of recent studies have focused on postpartum depression, with few addressing antenatal depression.
In addition, multiple studies have investigated the relationship between postpartum depression and bipolarity, but few have addressed the relationship between antenatal depression and bipolarity. Given that bipolar disorder usually begins in adolescence or early adulthood, women are at risk of having mood episodes throughout the reproductive years.9 Studies have found that approximately 9.6%–20.4% of women in nonclinical populations have manic symptoms immediately following delivery.10 The issue of whether bipolar illness improves during pregnancy is controversial; however, pregnancy is not protective for all women with bipolar disorder.11 Women with bipolar disorder are at high risk for symptom exacerbation during the immediate postpartum period, as indicated by a nearly seven-fold higher risk of admission for a first episode and a nearly two-fold higher risk for a recurrent episode in puerperal women, compared with nonpostpartum and nonpregnant women.11
Identification of factors associated with antenatal depression would facilitate its prevention and management. Therefore, the purpose of this study was to identify factors associated with antenatal depression, including sociodemographic parameters, social support, social conflicts, and bipolarity.
Materials and methods
Participants and assessment methods
During the 12-month study period between May 2011 and April 2012, pregnant women without a lifetime history of psychiatric illness, including depressive disorder, were recruited consecutively from two obstetrics clinics and the obstetrics department of a single hospital in Jeju, Korea. All were assessed for lifetime psychiatric diagnosis using a semistructured interview composed of various screening checklists. Some of the women were excluded from the study on the basis of their psychiatric screening. All subjects gave their informed consent to participate in this study after the procedure had been fully explained to them. Ninety pregnant women were initially willing to participate, but six candidates refused to complete the self-report questionnaire, leaving 84 enrolled subjects.
The study participants completed a questionnaire regarding their sociodemographic and clinical characteristics, including data on age, duration of education, religious practices, household income, employment status, subjective socioeconomic status, obstetric history, communication with their partner, relationship satisfaction, family history of psychiatric illness, and any current obstetric or medical problems.
Depressive symptoms were assessed using the Korean version of the Edinburgh Postnatal Depression Scale (EPDS).12 The EPDS screening is sensitive and specific for postnatal depression, and has been validated for use in the antenatal setting.13 The EPDS is a self-report instrument composed of ten items rated on a four-point scale screening for depressed mood, anhedonia, guilt, anxiety, and suicidal ideation. A high score indicates increased depressive symptoms within the previous 7 days, and the cutoff point of EPDS to detect depression among pregnant females is a score of 9/10 based on a previous validation study in pregnant Korean females.12
Bipolarity was assessed using the Korean version of the Mood Disorder Questionnaire (K-MDQ), which is a three-part, self-report questionnaire that screens for a lifetime history of manic or hypomanic episodes.14 Part 1 is composed of 13 “yes” or “no” questions regarding manic symptoms. Part 2 determines whether multiple manic symptoms are experienced simultaneously. Part 3 assesses the degree of functional impairment. Typically, a positive K-MDQ result is defined as a score of at least 7 (7 positive symptoms) with symptoms that co-occur in the setting of moderate or severe functional impairment (sensitivity 0.28, specificity 0.97).15 Recently, it has been suggested that the K-MDQ cutoff should be a score of ≥7 regardless of the results of the supplementary questions (parts 2 and 3).16 The alternative scoring algorithm has excellent sensitivity (89%) and specificity (84%).16 In this study, we defined a positive K-MDQ screen as a minimum of 7 of 13 co-occurring symptoms.
Social support and social conflicts were assessed using the Korean version of a social support and social undermining scale, consisting of two subscales with six social support items and five social undermining items. This scale was developed by Abbey et al17 and the Korean version was adapted by Yoo and Kwon.18 The social support and undermining scale was used to measure participants’ perception of social support and social undermining by significant others. Participants were asked to indicate responses on five-point Likert scales. Higher scores indicated more social support and a greater degree of social undermining. The study was approved by the institutional review board of the Jeju National University Hospital.
Data analysis
Descriptive statistics were used to summarize participant characteristics. For categorical variables, the significance of differences in EPDS scores between groups was determined using the independent Student’s t-test and differences among groups by one-way analysis of variance. Correlations between EPDS scores and social support or social conflict were evaluated using Pearson’s correlation coefficient. Multivariate regression analysis was used to identify factors associated with antenatal depression. Factor analysis was conducted using a principal axis factor analysis with varimax rotation. All statistical analyses were performed using Statistical Package for the Social Sciences version 18.0 software (SPSS Inc., Chicago, IL, USA), and statistical significance was determined using an alpha level of 0.05 (two-tailed tests).
Results
As shown in Table 1, the study comprised 84 pregnant women of mean age 30.6±4.0 years with a mean gestational age of 30.1±4.4 weeks. All were married and lived with their partner. The sociodemographic and obstetric characteristics of the study participants are shown in Table 1. Most of the women were educated beyond college level (73.8%), had a monthly household income of <2 million won (51.2%), planned their current pregnancy (83.3%), did not have a family history of psychiatric illness (95.2%), and had no current obstetric or medical problems (94.0%). None of the participants abused substances such as alcohol, tobacco, or drugs during pregnancy. The majority (78.6%) reported being of middle socioeconomic status. The rate of unemployment was 16.7%. More than half of the participants were multiparous. Spousal communication was reported as “good” by 45.2% of women and “bad” by 15.5%. Marital satisfaction was reported by 31% of women, with 17.9% reporting being dissatisfied with their marriage.
  | Table 1 Sociodemographic and obstetric characteristics of participants (n=84) |
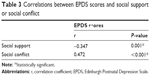
There were no significant differences in likelihood of antenatal depression, determined by EPDS scores, arising from age, education, religious practices, socioeconomic status, monthly household income, employment status, gestational age, parity, pregnancy intention, family history of psychiatric illness, and current obstetric or medical problems. However, there were significant relationships between antenatal depression, spousal communication, and marital satisfaction (Table 2), indicating that spousal interactions play a greater role in antenatal depression than sociodemographic and obstetric variables. EPDS scores had a significant negative correlation with social support and a positive correlation with social conflict (Table 3).
  | Table 3 Correlations between EPDS scores and social support or social conflict |
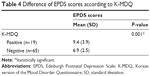
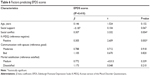
Nineteen participants (22.6%) had positive K-MDQ scores, suggesting the presence of bipolarity, and K-MDQ-positive subjects were significantly more likely to score high on the EPDS (Table 4). In factor analysis of the K-MDQ, three factors were found to account for 56.9% of the total variance. Factor 1 with the highest eigenvalue (36.08%) included “more energy”, “more activity”, “more self-confidence”, “more socially minded or outgoing”, and “more talkative”, which are all energetic behavioral symptoms of mania (Table 5). The multiple regression model showed that social conflict and positive K-MDQ scores were significantly correlated with high EPDS scores (Table 6). The model predicted 41% of EPDS scores.
  | Table 5 Factor analysis of K-MDQ |
Discussion
This study investigated factors associated with antenatal depression, including bipolarity. There was a positive correlation between poor spousal communication, marital dissatisfaction, and high EPDS scores (depression). The severity of antenatal depression was not significantly different according to education, religious practices, subjective socioeconomic status, household income, employment status, gestational age, parity, or pregnancy intention. These results suggest that the relationship with a partner is more influential in antenatal depression than are sociodemographic or obstetric factors. Significant correlations were also found between EPDS score and social support/conflict. In other words, the degree of antenatal depression is associated with social support and conflict.
Previous studies have demonstrated a link between a poor relationship with a partner, lack of social support, including by the partner, and antenatal depression.1,4 The results of these earlier studies are consistent with our present findings, and suggest that pregnant women regard their partner as an important source of emotional support.1 Partners are usually required to participate in the pregnancy as well as childbirth, and to take part in the preparations for birthing and the early life of the infant. During this time, the partner is an important assistant and provides support for the pregnant woman.
Social support, including from the partner, may shield pregnant women from stressors.19 Women undergo constant changes during pregnancy, childbirth, and motherhood, making this a psychologically vulnerable time. Therefore, some pregnant women may experience extreme stress and emotional distress. Emotional support from the significant people in their lives might improve their ability to cope with these stressors. From a biological perspective, emotional distress may cause functional abnormalities in neural pathways.1 Emotional support might normalize the brain alterations involved in the pathologic process of antenatal depression.20
In a review article by Lancaster et al factors associated with antenatal depression were prenatal anxiety, stressful negative life events, overall life events, history of depressive disease, lack of support from the partner, lack of social support, unwanted pregnancy, and quality of the relationship with the partner.21 However, routine daily stress, socioeconomic status, unemployment, abuse of illegal substances, and obstetric history were not related to antenatal depression.21 Excluding unwanted pregnancy, our results were similar. In the review by Lancaster et al whether or not the pregnancy was planned was unrelated to antenatal depression in some of the studies reviewed, whereas in others, unplanned pregnancy showed a medium correlation with depressive symptoms in a bivariate analysis.21 Awareness by clinicians of the factors associated with antenatal depression would allow identification of women at risk of depression, facilitating early intervention.
Pregnancy and childbirth trigger many psychological, physical, and hormonal changes, and the risk of onset of a mood disorder and relapse is increased, especially during the perinatal period. The prevalence of major depressive disorder during pregnancy and the postpartum period ranges from 5.5% to 33.1%.22 In the general population, 10%–15% of women experience postpartum depression after delivery. In a study of 2,252 pregnant women, 23% of those with bipolar disorder relapsed during pregnancy, and 52% of bipolar women relapsed during the postpartum period.22 In women with a prior diagnosis of major depressive disorder, a 4.6% and 30.0% relapse rate was observed during pregnancy and postpartum period, respectively.23 In a recent study of 120,378 women diagnosed with any type of psychiatric disorder (excluding bipolar affective disorder) during their first psychiatric contact, 3,062 had an inpatient or outpatient diagnosis of bipolar affective disorder at a later time point.24 Approximately 14% of women whose first psychiatric contact was during the first postpartum month received a bipolar diagnosis within 15 years, compared with 4% of women with a first psychiatric contact not related to childbirth. A psychiatric episode in the immediate postpartum period significantly predicted conversion to bipolar affective disorder during the 15-year follow-up period.24 This result indicates that presentation of a psychiatric disorder in the postpartum period is likely to be an early manifestation of bipolar affective disorder.
Psychiatric disorders that occur during the postpartum period may be a marker of underlying bipolar illness, but the majority of women are diagnosed with a psychiatric illness other than bipolar disorder.
Therefore, accurate diagnosis of bipolar disorder is often delayed. Most of the earlier studies were limited to the postpartum period. However, awareness by clinicians of the features of bipolarity during pregnancy (not only during the postpartum period) would facilitate diagnosis of bipolar disorder during pregnancy because some patients may experience onset of symptoms antenatally, which are exacerbated after delivery.24
The present study was the first to investigate the association between bipolarity and antenatal depression in women without a lifetime history of psychiatric disorders in Korea. The 19 K-MDQ-positive participants (22.6%) also had significantly higher EPDS scores. In other words, K-MDQ-positive participants were more depressed than K-MDQ-negative participants. This implies that pregnant women with features of bipolarity have more severe depressive symptoms. In a multivariate regression model, K-MDQ score and social conflict were associated with antenatal depression. The presentation of bipolar depression can range from a major depressive episode of mild intensity to a severe one.25 In one paper, severe depression was considered to be a specific feature of bipolar disorder, with the author suggesting that part of the severity comes from the bipolarity itself.25
An accurate diagnosis of bipolar disorder is often delayed because it is commonly misdiagnosed as unipolar major depressive disorder.16 Mood disorders during pregnancy, including both bipolar disorder and unipolar depressive disorder, will present with depressive symptoms.23 The present study indicates that although both disorders present with depressive symptoms, severely depressed pregnant women may also have features of bipolarity. Therefore, bipolar disorder should be considered in women with antenatal depression, and clinicians should remain open to the possibility of bipolar disorder to ensure accurate diagnosis and treatment.
There are several limitations to this study. First, it was comprised of a small sample of women from several clinics at a specific location and may not be representative of the general pregnant population in Korea. Jeju-do is an island far from mainland South Korea, which may have affected our results. Subjects volunteered to participate in this study, so the study findings may not be representative of all pregnant women. Second, the study used self-report questionnaires rather than specific diagnostic criteria by an expert. Therefore, self-report bias might have influenced the results. For example, a woman who is depressed during pregnancy may be more likely to perceive a lack of social or partner support. Third, we did not evaluate health-related factors that may have influenced mood stability, such as exercise, sleep, body mass index, and food intake. A further concern is that we did not evaluate the association between trimester and depressive symptoms. Finally, the cross-sectional nature of the study design limits the interpretation of its results. Our findings should be considered preliminary, and future longitudinal studies are needed to investigate the accuracy of diagnosis and course of bipolarity in K-MDQ-positive subjects.
Conclusion
Factors associated with antenatal depression include lack of social support, social conflict, marital satisfaction, spousal communication, and bipolarity. Pregnant women with bipolarity were more depressed than those without bipolarity. Bipolar disorder should be considered in pregnant women with depression. Physicians should be aware of factors associated with antenatal depression to provide effective management.
Acknowledgment
This work was supported by a research grant from Jeju National University in 2010.
Disclosure
The authors report no conflicts of interest in this work.
References
Jeong HG, Lim JS, Lee MS, Kim SH, Jung IK, Joe SH. The association of psychosocial factors and obstetric history with depression in pregnant women: focus on the role of emotional support. Gen Hosp Psychiatry. 2013;35:354–358. | ||
Heron J, O’Connor TG, Evans J, Golding J, Glover V; ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80:65–73. | ||
Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord. 2000;59:31–40. | ||
Pajulo M, Savonlahti E, Sourander A, Helenius H, Piha J. Antenatal depression, substance dependency and social support. J Affect Disord. 2001;65:9–17. | ||
Chang HY, Keyes KM, Lee KS, et al. Prenatal maternal depression is associated with low birth weight through shorter gestational age in term infants in Korea. Early Hum Dev. 2014;90:15–20. | ||
Marcus SM. Depression during pregnancy: rates, risks and consequences – Motherisk Update 2008. Can J Clin Pharmacol. 2009;16:e15–22. | ||
Austin MP, Leader L. Maternal stress and obstetric and infant outcomes: epidemiological findings and neuroendocrine mechanisms. Aust N Z J Obstet Gynaecol. 2000;40:331–337. | ||
Glover V. Maternal stress or anxiety in pregnancy and emotional development of the child. Br J Psychiatry. 1997;171:105–106. | ||
Sharma V, Pope CJ. Pregnancy and bipolar disorder: a systematic review. J Clin Psychiatry. 2012;73:1447–1455. | ||
Sharma V, Xie B, Campbell MK, et al. A prospective study of diagnostic conversion of major depressive disorder to bipolar disorder in pregnancy and postpartum. Bipolar Disord. 2014;16:16–21. | ||
Yonkers KA, Wisner KL, Stowe Z, et al. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry. 2004;161:608–620. | ||
Kim YK, Hur JW, Kim KH, et al. Clinical application of Korean version of Edinburgh Postnatal Depression Scale. J Korean Neuropsychiatr Assoc. 2008;47:36–44. | ||
Bergink V, Kooistra L, Lambregtse-van den Berg MP, et al. Validation of the Edinburgh Depression Scale during pregnancy. J Psychosom Res. 2011;70:385–389. | ||
Hirschfeld RM, Williams JB, Spitzer RL, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. | ||
Hirschfeld RM, Calabrese JR, Weissman MM, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64:53–59. | ||
Frey BN, Simpson W, Wright L, Steiner M. Sensitivity and specificity of the Mood Disorder Questionnaire as a screening tool for bipolar disorder during pregnancy and the postpartum period. J Clin Psychiatry. 2012;73:1456–1461. | ||
Abbey A, Abramis DJ, Caplan RD. Effects of different sources of social support and social conflict on emotional well-being. Basic Appl Soc Psychol. 1985;6:111–129. | ||
Yoo SE, Kwon JH. The effects of perfectionism, social support, stress, and coping style on depression in the middle-aged woman. Korean J Clin Psychol. 1997;16:67–84. | ||
Deichert NT, Fekete EM, Boarts JM, Druley JA, Delahanty DL. Emotional support and affect: associations with health behaviors and active coping efforts in men living with HIV. AIDS Behav. 2008;12: 139–145. | ||
Etkin A, Pittenger C, Polan HJ, Kandel ER. Toward a neurobiology of psychotherapy: basic science and clinical applications. J Neuropsychiatry Clin Neurosci. 2005;17:145–158. | ||
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202:5–14. | ||
Le Strat Y, Dubertret C, Le Foll B. Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord. 2011;135:128–138. | ||
Viguera AC, Tondo L, Koukopoulos AE, Reginaldi D, Lepri B, Baldessarini RJ. Episodes of mood disorders in 2,252 pregnancies and postpartum periods. Am J Psychiatry. 2011;168:1179–1185. | ||
Munk-Olsen T, Laursen TM, Meltzer-Brody S, Mortensen PB, Jones I. Psychiatric disorders with postpartum onset: possible early manifestations of bipolar affective disorders. Arch Gen Psychiatry. 2012;69: 428–434. | ||
Henry C. [Severe depression: specific features of bipolar disorder]. Encephale. 2009;35 Suppl 7:S261–S263. French. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.