Back to Journals » International Journal of General Medicine » Volume 16
Factors Affecting Hospitalization Length and in-Hospital Death Due to COVID-19 Infection in Saudi Arabia: A Single-Center Retrospective Analysis
Authors Al Omair OA , Essa A , Elzorkany K , Shehab-Eldeen S , Alarfaj HM, Alarfaj SM, Alabdulqader F, Aldoughan A, Agha M, Ali SI, Darwish E
Received 21 April 2023
Accepted for publication 12 July 2023
Published 1 August 2023 Volume 2023:16 Pages 3267—3280
DOI https://doi.org/10.2147/IJGM.S418243
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Omar A Al Omair,1 Abdallah Essa,2,3 Khaled Elzorkany,4,5 Somaia Shehab-Eldeen,2,3 Hamzah M Alarfaj,6 Sumaia M Alarfaj,7 Fatimah Alabdulqader,7 Alghaydaa Aldoughan,7 Mohammed Agha,8 Sayed I Ali,9 Ehab Darwish3,10
1Internal Medicine Department, College of Medicine, King Faisal University, Al-Ahsa, Kingdom of Saudi Arabia; 2Tropical Medicine Department, Faculty of Medicine, Menoufia University, Shebin Elkom, Egypt; 3Gastroenterology and Infectious Diseases Unit, College of Medicine, King Faisal University, Al-Ahsa, Kingdom of Saudi Arabia; 4Internal Medicine Department, Faculty of Medicine, Menoufia University, Shebin Elkom, Egypt; 5Nephrology Unit, College of Medicine, King Faisal University, Al-Ahsa, Kingdom of Saudi Arabia; 6King Faisal Specialist Hospital and Research Center, Riyadh, Kingdom of Saudi Arabia; 7Medical Student at the College of Medicine, King Faisal University, Al-Ahsa, Kingdom of Saudi Arabia; 8Chest Department, Faculty of Medicine, Menoufia University, Shebin Elkom, Egypt; 9Family Medicine Department, College of Medicine, King Faisal University, Al-Ahsa, Kingdom of Saudi Arabia; 10Tropical Medicine Department, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Correspondence: Somaia Shehab-Eldeen, Tropical Medicine Department, Faculty of Medicine, Menoufia University, Shebin Elkom, 32511, Egypt, Tel +201117251523, Email [email protected]
Background: The emerging COVID-19 coronavirus disease has widely spread, causing a serious worldwide pandemic. Disease severity and mortality risk can be predicted using an analysis of COVID-19 clinical characteristics. Finding out what influences patients’ hospitalization length and in-hospital mortality is crucial for decision-making and planning for emergencies. The goal of this study is to identify the factors that influence hospital stay length and in-hospital death due to COVID-19 infection.
Methods: This cross-sectional study was conducted from August to October 2020 and included 630 patients with a confirmed diagnosis of COVID-19 infection. Using odds ratios (OR) and 95% confidence intervals (CI), a multivariable logistic regression model was used to assess the variables that are linked to longer hospital stays and in-hospital deaths.
Results: Most patients were male (64.3%), and most were older than 40 years (81.4%). The mean length of hospital stay (LoHS) was 10.4± 11.6 days. The overall death rate among these COVID-19 cases was 14.3%. Non-survivors were older, had more comorbidities, had prolonged LoHS with increased ICU admission rates and mechanical ventilation usage, and had a more severe condition than survivors. ICU admission, low serum albumin, and elevated LDH levels were associated with longer LoHS, while ICU admission, DM, and respiratory diseases as comorbidities, total leukocytic count, and serum albumin were predictors of mortality.
Conclusion: Longer LoHS due to COVID-19 infection was linked to ICU admission, low serum albumin, and elevated LDH levels, while the independent predictors of in-hospital death were ICU admission, DM, and respiratory diseases as comorbidities, total leukocytic count, and serum albumin.
Keywords: COVID-19, Saudi Arabia, hospital stay, Al-Ahsa
Introduction
A novel beta-coronavirus known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused an outbreak of infection in Wuhan, China, in December 2019. The World Health Organization (WHO) has named the disease caused by SARS-CoV-2 as coronavirus disease 2019. (COVID-19).1
The novel coronavirus infected people in the same way as other coronaviruses, most notably the severe acute respiratory syndrome coronavirus (SARS-CoV), the bat SARS-like CoV, and the Middle East respiratory syndrome coronavirus (MERS-CoV). SARS-CoV-2, like SARS-CoV-1, enters human cells via the angiotensin-converting enzyme 2 (ACE-2) receptor.2 The primary mode of transmission of SARS-CoV-2 is via respiratory droplets produced by an infected person while coughing or sneezing.3
SARS-CoV-2 infection appears to have a broad clinical spectrum, encompassing asymptomatic infection, mild upper respiratory tract illness, and severe viral pneumonia with respiratory failure and even death, with many patients hospitalized with pneumonia.4–6
Recent studies have shown that the disease’s symptoms vary from one region to another because of their different demographics and other health problems.7 COVID-19 patients present with varying levels of severity. Mild and moderate cases represent more than 80% of total cases, and the duration of hospital admission for patients with COVID-19 varies widely from patient to patient. Hospital care varies from general ward-based care to intensive care, where patients may need intubation and mechanical ventilation.8–12 The healthcare system’s readiness was put to the test by this pandemic, which is dependent on indicators of severity and factors affecting the length of hospital admissions.7 Predicting and understanding hospital bed demand for patients with COVID-19 and focusing on the most seriously ill patients and those who are rapidly deteriorating gives crucial proof for contingency planning and decision-making.8,13 This study aims to identify various factors that influence hospital admission duration and in-hospital mortality due to the COVID-19 infection.
Subjects and Methods
Study Design and Setting
This retrospective study included 630 adult individuals, aged 18 years or older, hospitalized in King Fahad Hospital, Al-Ahsa, Saudi Arabia, in the period from August to October 2020. King Fahad Hospital is a 500-bed general hospital in Al-Hofuf, the biggest hospital in the city area of Al-Ahsa. It was one of the key referral hospitals in Al-Ahsa City to receive COVID-19 patients at the onset of the coronavirus pandemic in the area.
Study Population
Adult patients with COVID-19 of both sexes and of varying ages who were confirmed SARS-CoV-2 positive by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) testing upon admission were included in the study. Our analysis was limited to patients who had both fully complete electronic medical records (EMRs) and LoHS durations of more than a single day. Patients hospitalized for other conditions who were discovered to be positive during their stay were not included. The final study included 630 patients who met the predetermined criteria.
Data Collection
Trained research assistants extracted the data from patient files. A well-designed and organized checklist was used to extract patient medical records information. The following data were retrieved in addition to hospital admission and discharge dates: sociodemographic data like age, sex, smoking status, and nationality, clinical factors such as presenting symptoms, comorbidities (depending on whether the patient has a verified diagnosis of any of the following disorders: diabetes mellitus, hypertension, cardiovascular, respiratory, hepatic, or chronic kidney disease), laboratory results, and the outcome. The severity of COVID-19 was graded as mild to moderate, or severe. Patients with mild to moderate COVID-19 showed symptoms with or without pneumonia but no hypoxia, while if any of the following criteria were fulfilled, the condition was classified as severe: (1) dyspnea (≥30 breaths/min), (2) low blood oxygen saturation of less than 93%, (3) PaO2/FiO2 ratio 300, (4) pulmonary infiltration > 50% within 24–48 hours.14
Statistical Analysis
Data were analyzed using a statistical package for social science (SPSS) program for Windows version 24 (SPSS Inc. Chicago, IL, USA). The mean and standard deviation were used for normally distributed data; otherwise, the median and interquartile range were used for non-normally distributed ones, while categorical data were expressed as numbers and percentages. A Chi-square (X2) was used to compare two groups of categorical data. The Mann–Whitney test was used as appropriate to compare two groups of quantitative variables. Linear/logistic regression analyses were used to predict risk factors for longer hospital stay and mortality, with a confidence interval of 95% (p < 0.05) to represent the statistical significance of the results. The multivariate regression model included univariate logistic regression variables with p values < 0.05 as predictors of hospital stay or mortality. All statistical analyses used two-sided hypothesis tests with a P < 0.05 significance level.
Ethical Considerations
The Institutional Review Board at King Faisal University approved this study (KFU-REC-2023-MAR-ETHICS651) and waived patient consent due to the study’s retrospective nature. The study was performed according to the Helsinki Declaration, and all data were collected, coded, and analyzed to ensure data integrity and patient privacy.
Results
Sociodemographic, Clinical, and Laboratory Characteristics
This retrospective study included 630 patients hospitalized with COVID-19 at King Fahad Hospital, Al-Hofuf, KSA. As shown in Table 1, the majority of the patients were males (64.1%), and most patients admitted were older than 40 years (81.2%), with a median age of 55 years. The majority of patients were Saudi (78.1%) and others were of other nationalities. The most common comorbidities in COVID-19 patients were diabetes mellitus (DM) and hypertension (HTN), which represented 32.5% and 26.7%, respectively. The median duration of the hospital stay is 7 days, with a range of 1–155 days. About 16% of patients were admitted to the ICU, and the overall death rate among these COVID-19 cases was 14.3%.
 |
Table 1 Sociodemographic, Clinical, and Laboratory Characteristics of COVID-19 Cases |
The laboratory results showed that 46.5% of patients had low hemoglobin levels, 5.7% had thrombocytopenia, 6.2% had thrombocytosis, 18.3% had leukocytosis, and patients who had elevated ALT, AST, total bilirubin, urea, and creatinine were 19%, 37.9%, 7.5%, 31%, and 29.2%, respectively. 60% of patients had low serum albumin levels, and 74.6% had elevated LDH levels.
Comparing the COVID-19 Patients Categorized According to the Length of Their Hospital Stay
Table 2 shows that patients who stayed in the hospital longer were much older, had a higher rate of diabetes, ICU admissions, mechanical ventilation usage, and severe disease, and had a worse outcome. Regarding comparisons of the laboratory indices, patients with longer hospital stays had higher total leukocytic count (TLC), alanine aminotransferase (ALT), and random blood sugar (RBS) but significantly lower serum albumin levels.
 |
Table 2 Comparison Between the COVID-19 Patients Categorized According to Their Length of Hospital Stay |
Factors Linked to a Longer Hospital Stay
To find risk factors linked to long-term hospitalization, the multivariable model comprised nine candidate variables with a P≤ 0.05 in univariable analysis. According to the findings, ICU admission (P = 0.008, OR 9.434, 95% CI 1.78–49.7), low serum albumin (P <0.001, OR 1.7, 95% CI 1.03–1.1), and elevated LDH on hospital admission (P <0.001, OR 0.997, 95% CI 0.995–0.998) were independent risk factors linked to a longer hospitalization stay in COVID-19 patients as shown in Table 3.
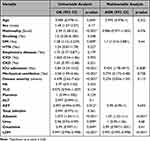 |
Table 3 Risk Factors for the Long Hospital Stay Among COVID-19 Patients |
Comparing the COVID-19 Patients Categorized According to Their Outcome
According to our findings, illustrated in Table 4, patients who died from COVID-19 were older than those who survived hospitalization and were discharged. They were more likely to have comorbidities such as DM and HTN, a longer hospital stay with more ICU admissions and mechanical ventilation usage, and more severe disease.
 |
Table 4 Comparison Between Survivors and Non-Survivors from COVID-19 Infection |
Laboratory tests showed that patients who did not survive had higher levels of TLC, AST, INR, blood urea, serum creatinine, RBS, and LDH, but much lower levels of serum albumin.
Factors Linked to in-Hospital Death
Multivariate regression model analysis showed that age (P= 0.023; OR 0.951; 95% CI 0.91–0.99), ICU admission (P< 0.001; OR 59.7; 95% CI 20.213–176.487), DM (P= 0.011; OR 4.849; 95% CI 1.440–16.332), respiratory diseases (p= 0.018; OR 7.464; 95% CI 1.411–39.468), TLC (P= 0.049; OR 0.924; 95% CI 0.854–1) and serum albumin (p= 0.001; OR 1.170; 95% CI 1.080–1.267) were independent risk factors associated with in-hospital mortality in COVID patients (Table 5).
 |
Table 5 Risk Factors for in-Hospital Death Due to COVID-19 Infection |
Discussion
The SARS-CoV-2 infection outbreak, which began at the end of 2019, has attracted the attention of the entire world. The new coronavirus, SARS-CoV-2, and the illness have been named by the World Health Organization (WHO) as coronavirus disease 2019 (COVID-19).15 Clinical manifestations of the illness might be asymptomatic, mild, or severe, and several cases end in death.16
On March 2, 2020, the Kingdom of Saudi Arabia (KSA) reported the first case of COVID-19.17 COVID-19 is a worldwide threat to people’s health. More detailed and specific characteristics are required to better understand this disease pandemic.18
The purpose of this study was to identify various factors that influence the duration of hospital admission and in-hospital death and to report the epidemiological features and characteristics of COVID-19 among patients who were admitted at King Fahad Hospital in Al-Ahsa, Eastern Province, Saudi Arabia, during the period from August to October 2020. This is very important for the understanding and management of COVID-19.
The study included 630 hospitalized patients diagnosed with COVID-19. The COVID-19 infection was more prevalent among those in the middle age group. This is consistent with another previous study that mentioned that, although the virus can infect any age group, the middle-aged group (40 to 60 years) was the most commonly infected group.19 This finding is not in accordance with some previous non-Saudi studies that mentioned ages above 60 as high-risk factors.20–22 This discrepancy could be explained by the fact that the population of Saudi Arabia is younger than that of European and Asian countries.
Our findings revealed that the infection affected more men than women. This was consistent with other studies’ findings that found similar results.5,23,24 But this contradicts other studies, which showed that females were more infected by SARS-CoV-2.25,26 The predominance of infection among males can be attributed to the higher number of men than women in the Saudi population. On the other hand, males are more involved in daily activities than females, which means they are more exposed to COVID-19 cases and more susceptible to infection. Another explanation for the higher rate of infection among males is that the X chromosome in females encodes some immune regulatory genes that cause lower viral load levels.27
In our study, most of the patients were Saudi (78.1%), while non-Saudi patients made up 21.9%. This contradicts a previous early study that found non-Saudi patients to be more affected, representing around 80% of the cases.28 The high rate of infection among non-Saudi patients was explained by higher exposure to infection due to sharing housing units.29 Our finding here is similar to other studies by Al Dossary et al and Al Mutair et al, who found more cases among the Saudi population.30,31 This can be explained by the fact that the number of Saudis in Saudi Arabia is at least double that of non-Saudis.
The most common comorbidities seen in our patients were diabetes mellitus (32.5%), hypertension (26.7%), cardiovascular diseases (7%), respiratory diseases (4.6%), chronic kidney diseases (4%), and liver diseases (0.3%). Similarly, Alahmari et al found diabetes to be their patients’ most prevalent comorbid condition, followed by hypertension.32 Also, Alwafi et al mentioned that the most common comorbidities were diabetes mellitus, hypertension, and heart diseases.33 Patients with chronic liver disorders (CLD) were also more likely to experience fatal outcomes, such as death or a longer hospital stay. The confirmed test results emphasize COVID-19’s detrimental effects on liver functions.34
The median duration of hospital admission for COVID-19 patients in this study was 7 days, whereas the average duration was 10.4 days. The average duration of hospital admission was longer in patients who died when compared to discharged patients (8.94 versus 19.24 days). The fact that patients who died spent more time in the hospital could be due to complications from underlying conditions or the severity of their illness. Our findings were similar to those of many other studies in Saudi Arabia. Alwafi et al reported that the median length of hospital stays among COVID-19 patients was 6 days (range 0–55 days).33 According to Alghamdi, the length of hospital stays of COVID-19 patients ranged from 4 to 15.6 days,35 while Alahmari et al found that the median length of hospital stays among COVID-19 patients was 7 days.32
In a systemic review done by Rees et al, they discovered that the median length of hospital stays in China is 14 days, compared to 5 days outside of China. The summary distributions for ICU are more similar (a median of 8 days in China and 7 days outside of China).36 Wang et al as well as Zhao et al reported the duration of hospital admission in patients with COVID-19 to be 10 and 13 days, respectively.4,18 The length of hospital stay for COVID-19 patients varies widely from one country to another and depends on the clinical situation of the patients, the local guidelines, and the capacity of hospitals.37,38
The results of our study showed that older age, severe disease, the need for mechanical ventilation, and admission to the ICU were all associated with a longer duration of hospital stay. Also, increased total leucocyte count, ALT, LDH, blood glucose, blood urea, and decreased serum albumin were associated with a prolonged duration of hospital admission. These findings suggest a correlation between prolonged hospitalization and significant physiological changes. It is important to understand these relationships to improve patient outcomes.
Age and the severity of the disease were found to be substantially correlated with the length of the hospital stay by Wang et al.39 In a different trial, patients with severe illness, mechanical ventilation, diabetes, or chronic kidney disease stayed in the hospital for noticeably longer.32 Higher creatinine levels and chronic liver or renal disease prior to admission, according to Guo et al, were linked to COVID-19 patients’ extended length of hospital stay (LoHS).40 In a separate study conducted in Saudi Arabia, leukocytosis, elevated LDH, elevated creatinine, and other comorbidities such as congestive heart failure and COPD were all linked to an increased risk of a longer hospital stay.33 Older age, diabetes mellitus, sickness severity, CRP, D-dimer, serum ferritin, serum Lactate Dehydrogenase (LDH), blood urea, and SGOT were all linked to a longer length of stay among COVID-19 patients who were hospitalized, according to Khatal et al.41
In a study conducted in India, oxygen saturation, the presence of more than two comorbidities, and specific laboratory indicators including LDH, ferritin, and D-dimer were found to be the most significant influences on LoHS.42 Alqassieh et al observed that patients with increased WBC had a shorter LoHS,43 which is contrary to our findings.
We did a multivariable analysis to find out what made COVID-19 patients stay in the hospital longer. We found that being admitted to the ICU, having a lower serum albumin level, and having a higher serum LDH level were all independent factors.
COVID-19 is distinguished by an inflammatory-related cytokine storm, which may enhance vascular permeability and allow albumin to escape from the interstitial space, leading to hypoalbuminemia.44 LDH production is triggered by viral infections or lung injuries, such as pneumonia associated with COVID-19. In cases of tissue damage, LDH levels are reportedly much higher, and these higher levels of LDH are reportedly correlated with the severity of inflammation.45,46 Furthermore, studies show that critically sick ICU patients also had much higher LDH levels than non-critical non-ICU patients.47,48 And patients in the intensive care units are more likely to get prolonged medical care.7
In the present study, the fatality rate among hospitalized patients with COVID-19 was 14.3%. This is similar to the range of 12–15% reported by other authors.49,50 Hospital mortality varies in different studies between 4.3% and 28%.4,50,51 The low overall mortality of COVID-19 in Saudi Arabia is attributed to the younger age of the Saudi population and to previous exposure to MERS-CoV. Exposure to MERS-CoV may partially protect against serious illness.52 In addition, the strict measures taken by the government and the high quality of the health care system played a major role in limiting disease spread and fatalities. Mortality in ICU-admitted patients is high (between 26% and 78%) in different countries.50,51,53
We found the mortality rate is higher in patients with chronic diseases, including diabetes mellitus, hypertension, respiratory diseases, cardiovascular diseases, chronic kidney diseases, and hepatic diseases. According to numerous studies, COVID-19 individuals with comorbidities were more likely to experience severe COVID-19 and frequently had a worse prognosis. Exacerbations of COVID-19 were more likely in patients with hypertension, diabetes, or chronic obstructive pulmonary disease (COPD).54–57
In the multivariable analysis, age, ICU admission, diabetes mellitus, respiratory diseases, total leukocyte count, and serum albumin were independent factors for in-hospital death in patients with COVID-19. Our findings are consistent with other research that has identified diabetes, heart disease, and hypertension as risk factors for fatalities.58–60 Al Mutair et al research shows that COVID-19 patients who are older than 50 years and have a history of high blood pressure, diabetes, or both have a higher death rate than younger patients who do not have diabetes and have normal blood pressure.61
In a different study on COVID-19 patients conducted in Saudi Arabia by Alswaidi et al, they discovered a large correlation between mortality and elderly and cardiovascular diseases.62 Ibrahim et al discovered a statistically significant link between ICU admission, cardiovascular disease, hypertension, renal failure, and COVID-19 death. The older population experienced a marked increase in COVID-19 deaths. The total leucocyte count and urea level were considerably greater in the COVID-19 death group compared to the recovered group.63 In older patients and those with concomitant illnesses, COVID-19 infection quickly escalates to acute respiratory distress syndrome, septic shock, metabolic acidosis, and coagulation failure, resulting in mortality.64
In this study, an increased WBC count, serum AST, INR, blood urea, serum creatinine, blood glucose, LDH, and decreased serum albumin were associated with a bad prognosis and higher mortality. The WBC count at admission is significantly correlated with death in COVID-19 patients. A higher level of WBC count should be given more attention in the treatment of COVID-19.65 Poor prognosis is associated with LDH levels, which represent tissue necrosis brought on by immunological hyperactivity in SARS.66
According to Pouw et al, severe patients had significantly higher levels of the neutrophil count, ALT, AST, lactate dehydrogenase (LDH), and serum creatinine than moderately ill individuals.67 SARS-CoV-2 may harm the tissues of the liver and heart, raising AST levels to varying degrees in severe patients.68 Acute kidney damage with elevated serum creatinine may be caused by the virus directly, as well as by hypoxia and shock.4 Patients with severe disease may develop Systemic Inflammatory Response Syndrome (SIRS) and Multi-organ Dysfunction Syndrome (MODS) due to the organ damage they have.57,69
This study has some limitations. The study’s retrospective design is the first factor. Second, given that this information was collected at the outbreak’s outset, it’s plausible that psychological and social variables may have played a role in the longer stays experienced by our patients. Third, the data was gathered prior to the availability of the COVID-19 vaccine and novel antiviral treatments, which significantly reduced illness severity and dissemination. Fourth, the data were acquired over a brief period of time from a single hospital, which restricted the experience to a specific location.
Conclusions
According to our findings, ICU admission, low serum albumin, and increased LDH upon hospital admission were found to be independent risk factors associated with a longer hospital stay in COVID-19 patients. Those patients continue to have a significant in-hospital mortality rate. The independent predictors of in-hospital mortality were ICU admission, diabetes, and respiratory illnesses as comorbidities, total leukocytic count, and serum albumin. This study’s findings may be used as a foundation for further research into the disease’s natural history, the creation of practical diagnostic tools for use in clinical practice, and the identification of persons at risk of presenting the disease’s severe form.
Data Sharing Statement
The data underlying this study is available from the first author upon reasonable request.
Acknowledgment
This study was funded by the Deanship of Scientific Research, King Faisal University, KSA (Project number GRANT3807).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
2. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. cell. 2020;181(2):271–280. e8. doi:10.1016/j.cell.2020.02.052
3. Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi:10.1056/NEJMc2004973
4. Wang D, Hu B, Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
5. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi:10.1016/S0140-6736(20)30211-7
6. Chen H, Xie Z, Zhu Y, et al. Chinese medicine for COVID-19: a protocol for systematic review and meta-analysis. Medicine. 2020;99:25.
7. Assiri RA, Bepari A, Patel W, et al. Exploration of sex and age-based associations in clinical characteristics, predictors of severity, and duration of stay among COVID-19 Patients at the University Hospital of Saudi Arabia. Healthcare. 2023;11:5.
8. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi:10.1016/j.tmaid.2020.101623
9. Cascella M, Rajnik M, Aleem A, et al. Features, evaluation and treatment coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020.
10. Jiang F, Deng L, Zhang L, et al. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19). J Gen Intern Med. 2020;35:1545–1549. doi:10.1007/s11606-020-05762-w
11. Aljuaid M, Alotair H, Alnajjar F, et al. Risk factors associated with in-hospital mortality patients with COVID-19 in Saudi Arabia. PLoS One. 2022;17(6):e0270062. doi:10.1371/journal.pone.0270062
12. Al-Otaiby M, Almutairi KM, Vinluan JM, et al. Demographic characteristics, comorbidities, and length of stay of COVID-19 patients admitted into intensive care units in Saudi Arabia: a nationwide retrospective study. Front Med. 2022;9:893954. doi:10.3389/fmed.2022.893954
13. Rosenbaum L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873–1875. doi:10.1056/NEJMp2005492
14. World Health Organization. Clinical Management of COVID-19: Interim Guidance, 27 May 2020. World Health Organization; 2020.
15. Froes F. And now for something completely different: from 2019-nCoV and COVID-19 to 2020-nMan. Pulmonology. 2020;26(2):114. doi:10.1016/j.pulmoe.2020.02.010
16. Adhikari SP, Meng S, Wu Y-J, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. doi:10.1186/s40249-020-00646-x
17. Barry M, Al Amri M, Memish ZA. COVID-19 in the shadows of MERS-CoV in the Kingdom of Saudi Arabia. J Epidemiol Glob Health. 2020;10(1):1. doi:10.2991/jegh.k.200218.003
18. Zhao W, Zha X, Wang N, et al. Clinical characteristics and durations of hospitalized patients with COVID-19 in Beijing: a retrospective cohort study. Cardiovasc Innovat Appl. 2021;6(1):33–44. doi:10.15212/CVIA.2021.0019
19. Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201(11):1380–1388. doi:10.1164/rccm.202002-0445OC
20. Liu K, Chen Y, Lin R, et al. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020;80(6):e14–e18. doi:10.1016/j.jinf.2020.03.005
21. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–1776. doi:10.1001/jama.2020.4683
22. Porcheddu R, Serra C, Kelvin D, et al. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020;14(2):125–128. doi:10.3855/jidc.12600
23. Li LQ, Huang T, Wang Y-Q, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–583. doi:10.1002/jmv.25757
24. Xia W, Shao J, Guo Y, et al. Clinical and CT features in pediatric patients with COVID‐19 infection: different points from adults. Pediatr Pulmonol. 2020;55(5):1169–1174. doi:10.1002/ppul.24718
25. Yehia BR, Winegar A, Fogel R, et al. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 US hospitals. JAMA network open. 2020;3(8):e2018039–e2018039. doi:10.1001/jamanetworkopen.2020.18039
26. Xie J, Zu Y, Alkhatib A, et al. Metabolic syndrome and COVID-19 mortality among adult black patients in New Orleans. Diabetes Care. 2021;44(1):188–193. doi:10.2337/dc20-1714
27. Conti P, Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J Biol Regul Homeost Agents. 2020;34(2):339–343. doi:10.23812/Editorial-Conti-3
28. Alqahtani AM, AlMalki ZS, Alalweet RM, et al. Assessing the severity of illness in patients with coronavirus disease in Saudi Arabia: a retrospective descriptive cross-sectional study. Front Public Health. 2020;8:593256. doi:10.3389/fpubh.2020.593256
29. Shaikh FS, Aldhafferi N, Buker A, et al. Comorbidities and risk factors for severe outcomes in COVID-19 patients in Saudi Arabia: a retrospective cohort study. J Multidiscip Healthc. 2021;14:2169–2183. doi:10.2147/JMDH.S317884
30. Al Dossary R, Alnimr A, Aljindan R, et al. Predictors of illness severity in COVID-19 cases in Saudi Arabia. Infect Drug Resist. 2021;Volume 14:4097–4105. doi:10.2147/IDR.S333300
31. Al Mutair A, Elhazmi A, Alhumaid S, et al. Examining the clinical prognosis of critically ill patients with COVID-19 admitted to intensive care units: a nationwide Saudi study. Medicina. 2021;57(9):878. doi:10.3390/medicina57090878
32. Alahmari AK, Almalki ZS, Albassam AA, et al. Factors associated with length of hospital stay among COVID-19 patients in Saudi Arabia: a retrospective study during the first pandemic wave. Healthcare. 2022;7:1201. doi:10.3390/healthcare10071201
33. Alwafi H, Naser AY, Qanash S, et al. Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc. 2021;Volume 14:839–852. doi:10.2147/JMDH.S304788
34. Li C, Chen Q, Wang J, et al. Clinical characteristics of chronic liver disease with coronavirus disease 2019 (COVID-19): a cohort study in Wuhan, China. Aging. 2020;12(16):15938. doi:10.18632/aging.103632
35. Alghamdi S. Clinical characteristics and treatment outcomes of severe (ICU) COVID-19 patients in Saudi Arabia: a single centre study. Saudi Pharm J. 2021;29(10):1096–1101. doi:10.1016/j.jsps.2021.08.008
36. Rees EM, Nightingale ES, Jafari Y, et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18:1–22. doi:10.1186/s12916-020-01726-3
37. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
38. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi:10.1016/S0140-6736(20)30744-3
39. Wang Z, Liu Y, Wei L, et al. What are the risk factors of hospital length of stay in the novel coronavirus pneumonia (COVID-19) patients? A survival analysis in southwest China. PLoS One. 2022;17(1):e0261216. doi:10.1371/journal.pone.0261216
40. Guo A, Lu J, Tan H, et al. Risk factors on admission associated with hospital length of stay in patients with COVID-19: a retrospective cohort study. Sci Rep. 2021;11(1):7310. doi:10.1038/s41598-021-86853-4
41. Khatal SJ, Sule SS, Ajinkya Jayaji Pandhare AJ, et al. Predictors of length of hospital stay in patients with COVID-19: a retrospective study. J Clin Diagn Res. 2023;17:1.
42. Thiruvengadam G, Lakshmi M, Ramanujam R. A study of factors affecting the length of hospital stay of COVID-19 patients by Cox-proportional hazard model in a South Indian tertiary care hospital. J Prim Care Community Health. 2021;12:21501327211000231. doi:10.1177/21501327211000231
43. Alqassieh RS, Bsisu IK, Al-Sabbagh MQ, et al. Clinical characteristics and predictors of the duration o f hospital stay in COVID-19 patients in Jordan [version 1; peer. F1000Research. 2020;9:1439. doi:10.12688/f1000research.27419.1
44. Yang L, Xie X, Tu Z, et al. The signal pathways and treatment of cytokine storm in COVID-19. Signal Transduct Target Ther. 2021;6(1):255. doi:10.1038/s41392-021-00679-0
45. Han Y, Zhang H, Mu S, et al. Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study. Aging. 2020;12(12):11245–11258. doi:10.18632/aging.103372
46. Ferrari D, Motta A, Strollo M, et al. Routine blood tests as a potential diagnostic tool for COVID-19. Clin Chem Lab Med. 2020;58(7):1095–1099. doi:10.1515/cclm-2020-0398
47. Eastin C, Eastin T. Clinical characteristics of coronavirus disease 2019 in China. J Emerg Med. 2020;58(4):711–712. doi:10.1016/j.jemermed.2020.04.004
48. Akdogan D, Guzel M, Tosun D, et al. Diagnostic and early prognostic value of serum CRP and LDH levels in patients with possible COVID-19 at the first admission. J Infect Dev Ctries. 2021;15(6):766–772. doi:10.3855/jidc.14072
49. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
50. Myers LC, Parodi SM, Escobar GJ, et al. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA. 2020;323(21):2195–2198. doi:10.1001/jama.2020.7202
51. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi:10.1001/jama.2020.6775
52. Barry M, AlMohaya A, AlHijji A, et al. Clinical characteristics and outcome of hospitalized COVID-19 Patients in a MERS-CoV Endemic Area. J Epidemiol Glob Health. 2020;10(3):214–221. doi:10.2991/jegh.k.200806.002
53. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to icus of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi:10.1001/jama.2020.5394
54. Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. doi:10.1016/j.jiph.2020.07.014
55. Yang J, Zheng YA, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
56. Guan WJ, Liang W-H, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi:10.1183/13993003.00547-2020
57. Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi:10.1016/S0140-6736(20)30628-0
58. Pan F, Yang L, Li Y, et al. Factors associated with death outcome in patients with severe coronavirus disease-19 (COVID-19): a case-control study. Int J Med Sci. 2020;17(9):1281–1292. doi:10.7150/ijms.46614
59. Yan Y, Yang Y, Wang F, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. 2020;8(1):e001343. doi:10.1136/bmjdrc-2020-001343
60. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020;9(2):575. doi:10.3390/jcm9020575
61. Al Mutair A, Al Mutairi A, Alhumaid S, et al. Examining and investigating the impact of demographic characteristics and chronic diseases on mortality of COVID-19: retrospective study. PLoS One. 2021;16(9):e0257131. doi:10.1371/journal.pone.0257131
62. Alswaidi FM, Assiri AM, Alhaqbani HH, et al. Characteristics and outcome of COVID-19 cases in Saudi Arabia: review of six-months of data (March-August 2020). Saudi Pharm J. 2021;29(7):682–691. doi:10.1016/j.jsps.2021.04.030
63. Ibrahim ME, AL-Aklobi OS, Abomughaid MM, et al. Epidemiological, clinical, and laboratory findings for patients of different age groups with confirmed coronavirus disease 2019 (COVID-19) in a hospital in Saudi Arabia. PLoS One. 2021;16(4):e0250955. doi:10.1371/journal.pone.0250955
64. Guo Y-R, Cao Q-D, Hong Z-S, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil Med Res. 2020;7:1–10. doi:10.1186/s40779-020-00240-0
65. Zhu B, Feng X, Jiang C, et al. Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study. BMC Infect Dis. 2021;21:1–5. doi:10.1186/s12879-021-06277-3
66. Tsui PT, Kwok ML, Yuen H, et al. Severe acute respiratory syndrome: clinical outcome and prognostic correlates. Emerg Infect Dis. 2003;9(9):1064. doi:10.3201/eid0909.030362
67. Pouw N, van de Maat J, Veerman K, et al. Clinical characteristics and outcomes of 952 hospitalized COVID-19 patients in The Netherlands: a retrospective cohort study. PLoS One. 2021;16(3):e0248713. doi:10.1371/journal.pone.0248713
68. Yang C, Qiu X, Zeng Y-K, et al. Coronavirus disease 2019: a clinical review. Eur Rev Med Pharmacol Sci. 2020;24(8):4585–4596. doi:10.26355/eurrev_202004_21045
69. Lakhani JD, Kapadia S, Choradiya R, et al. COVID-19 and Multiorgan Dysfunction Syndrome. IntechOpen; 2021.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
