Back to Journals » Infection and Drug Resistance » Volume 15
Factors Affect the Eradication Rate of Helicobacter pylori by Modified Quadruple Therapy: A Prospective Cohort Study
Authors Lan QL, Sun HY, Ye Y, Wang Y, Liu Y, Weng XJ
Received 14 January 2022
Accepted for publication 22 April 2022
Published 29 April 2022 Volume 2022:15 Pages 2339—2345
DOI https://doi.org/10.2147/IDR.S358464
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Suresh Antony
Qiao-Li Lan, Hao-Yue Sun, Yi Ye, Ying Wang, Ya Liu, Xue-Jian Weng
Department of Digestive System, Wenzhou People’s Hospital, The Third Affiliated Hospital of Shanghai University, The Wenzhou Third Clinical College of Wenzhou Medical University, Wenzhou, 325000, People’s Republic of China
Correspondence: Ying Wang, Department of Digestive System, Wenzhou People’s Hospital, The Third Affiliated Hospital of Shanghai University, The Wenzhou Third Clinical College of Wenzhou Medical University, Wenzhou, 325000, Zhejiang, People’s Republic of China, Tel +86 13758454419, Fax +86 057788059502, Email [email protected]
Objective: This study aimed to investigate related factors affecting the eradication rate of Helicobacter pylori (Hp) by modified quadruple therapy.
Methods: Between September 2020 and March 2021, 341 patients who were diagnosed with Hp infection and whose infections were confirmed by gastroscopy, a histological examination, and a C13-UBT without culturing and antimicrobial susceptibility studies received a two-week anti-Hp treatment, a modified quadruple therapy, in our department. The result of C13-UBT was rechecked 4 weeks after the drug withdrawal, and the patients were divided into two groups—a success group and a failure group—according to the final breath result. The general clinical information and related laboratory indexes of each patient were collected, and the factors affecting the eradication rate were analyzed.
Results: The total clinical eradication rate was 80.06% (273/341), and the failure rate was 19.94% (68/341), correspondingly. Univariate analysis identified statistically significant differences between the two groups in serum 25-hydroxyvitamin D levels, presence of oral diseases, positive cytotoxin-associated gene A (CagA), and medical compliance (P < 0.05). Meanwhile, the use of a proton pump inhibitor (PPIs) and antibiotics was statistically different (P < 0.05). Logistic regression analysis revealed that vitamin D level (< 20 ng/mL) [OR = 98.56, 95% CI (29.01– 334.83), P < 0.001] and medical compliance [OR = 148.18, 95% CI (37.64– 583.33), P < 0.001] were independent effecting factors for eradication rate.
Conclusion: Serum 25-hydroxyvitamin D level lower than 20 ng/mL may affect the success of eradication of Hp and is an independent risk factor for eradication failure.
Keywords: Helicobacter pylori, 25-hydroxyvitamin D, eradication rate, irregular medication
Introduction
Helicobacter pylori (Hp) is the first prokaryote that has been recognized by the World Health Organization as carcinogenic to human beings. It is closely related to the occurrence of gastrointestinal diseases, such as chronic gastritis, peptic ulcers, gastric cancer, and lymphoproliferative gastric lymphoma,1–4 and the probability of developing gastric cancer in people infected with Hp is 2–6 times higher than that of non-infected people. In China, the infection rate of Hp is approximately 56%.5
The progression pattern of gastric cancer is, in order, Hp infection, acute gastritis, chronic non-atrophic gastritis, chronic atrophic gastritis, metaplasia (small intestinal and colonic), dysplasia, and finally gastric cancer. Previous studies show that, once Hp has been successfully eradicated, the risk of gastric cancer can reduce by 73%.6,7 Hp infection is an independent risk factor for gastric metaplasia, and long-standing Hp infection increases the risk of intestinal metaplasia of the gastric mucosa by 9 times.4,6 Radical treatment of Hp infection can reduce the occurrence of gastric atrophy and gastric cancer. Although the use of quadruple therapy has become the mainstream, few regimens have consistently achieved high eradication rates. To find potential action methods and influencing factors to increase the eradication rate is the focus of research on the treatment of Helicobacter pylori.
Some studies indicate that Vitamin D (VitD) has the potential function in modifying host defense against foreign antigens and pathogens, and several VitD receptors (VDR) transcription-dependent activities have been identified as affecting the immune system regulation.8 For more than a century, vitamin D-mediated treatments for infectious diseases have been known. Additionally, adding vitamin D3 to the usual clarithromycin-based triple treatment might give an extra benefit in achieving much better eradication rates of H. pylori.9 However, the level of vitamin D in the patient’s body is affected by many factors such as diet and drug treatment, and the daily monitoring of the level of vitamin D in the body is less. At present, there are few studies on the influence of the level of vitamin D in patients before or during the radical treatment of Hp on the eradication rate of Hp.
Based on this theory, this study aimed to explore the effect of serum 25-hydroxyvitamin D level on the eradication of Hp, to provide some clinical data for early intervention in clinic to improve the eradication rate, by analyzing the factors affecting the eradication rate of Hp.
Main Clinical Data
General Information
A total of 341 patients who came to take physical examinations or underwent outpatient visiting were included in this study from September 2020 to March 2021 according to the inclusion/exclusion criteria.
Inclusion criteria: (1) Hp infection was confirmed by gastroscopy, a histological examination, and a C13-UBT without culturing and antimicrobial susceptibility studies; (2) Patients and their families agreed to participate in this study and signed the consent form.
Exclusion criteria: (1) Patients were under pregnant or lactating; (2) Combined with serious liver or kidney insufficiency; (3) Patients were intolerant to the modified quadruple therapy; (4) Patients who had formerly undergone H. pylori eradication therapy, taken antibiotics, anti-inflammatory, corticosteroids, immunosuppressive, and acid-suppressive medicine in the preceding 2 months; (5) Currently taking PPIs or Vitamin D supplements.
The study design was approved by the ethics committee of Wenzhou People’s Hospital and was confirmed to meet the required ethical and moral standards. This study was conducted following the Declaration of Helsinki.
Methods
Treatment of Modified Quadruple Therapy
According to the consensus of the Society of Gastroenterology, Chinese Study Group on Helicobacter pylori and Peptic Ulcer of our state,10 and considering the H. pylori resistance to the antimicrobials used in the local area,11 all patients were treated with modified quadruple anti-Hp therapy for 2 weeks.12
Details of the treatment of drugs usage were as follows: (1) the usage of bismuth potassium citrate (Lizhu Pharmaceutical Factory, Lizhu Group, China) was 220mg bid 30 minutes before a meal; (2) diverse choices of antibiotics are as follows and the taking time is about 1 hour after the meal: patients who were not allergic to penicillin were given amoxicillin (Zhongnuo Pharmaceutical [Shijiazhuang] Co., Ltd., China), 1.0g bid; along with tetracycline (Zhejiang Ruixin Pharmaceutical Co., Ltd., China), 250mg tid; furazolidone (Tianjin Lisheng Pharmaceutical Co., Ltd., China), 0.1g bid or levofloxacin (First Sankyo Pharmaceutical [Beijing] Co., Ltd., China) 0.5g qd. Patients with a penicillin allergy were given tetracycline combined with furazolidone; (3) the proton pump inhibitors (PPIs) used are as follows and are taken once before the breakfast and the dinner: esomeprazole (AstraZeneca Pharmaceutical Co., Ltd., UK), 20mg bid; omeprazole enteric-coated capsules (Zhejiang Jinhua Kangenbei Biological Pharmaceutics Co. Ltd., China), 20mg bid; rabeprazole sodium enteric-coated tablets (Jiangsu Haosen Pharma Co., Ltd., China), 10mg bid and lansoprazole enteric-coated capsules (Tianjin Takeda Pharmaceutical Co., Ltd., China), 30mg bid. PPIs were chosen for each patient using a random multi-sample design.
Grouping
The C13-urea breath test (C13-UBT) was rechecked 4 weeks after the withdrawal of the treatment on each patient. The patients were then divided into two groups—a failure group and a success group—according to the result.
Questionnaire and Observational Index
Before starting the eradication treatment, the history of vitamin D supplementation was reconfirmed, and the blood sample was collected and sent to the laboratory of our hospital to test the patient’s serum vitamin D level and the level of cytotoxin-associated gene A (CagA).
A self-designed questionnaire was used to collect information from the enrolled patients and different situations were classified and numbered to facilitate subsequent statistical processing. The following items were included and categorized: gender (female = 0; male = 1); body mass index (BMI; BMI 18.5–23.9 = 0, otherwise = 1); residential area (rural = 0; urban = 1); age (age 18–50 years = 0, age > 50 = 1); education level (primary school and below = 0, secondary school and above = 1); marital status (unmarried = 0, married = 1); annual income (≥ ¥50,000 yuan = 0, < ¥50,000 yuan = 1); family member infection (yes = 1, no = 0); vitamin D level (<20 ng/mL = 1; ≥20 ng/mL = 0); CagA (positive = 1, negative = 0); PPI selection (esomeprazole = 0, rabeprazole = 1, omeprazole = 2, lansoprazole = 3); antibiotic selection (amoxicillin + furazolidone = 0, amoxicillin + tetracycline = 1, amoxicillin + levofloxacin = 2, furazolidone + tetracycline = 3); gastroscopy (atrophic state = 1, non-atrophic state = 0); oral condition (presence of bad breath, caries, or periodontal disease = 1, none = 0); comorbidities, such as hypertension, diabetes, or other diseases that need to be treated with medication (presence = 1, absence = 0); smoking (yes = 1, no = 0); with drinking habits (yes = 1, no = 0); treatment (initial treatment = 0, retreatment = 1); medical compliance: taking medicines on time or not (irregular medication = 1, regular medication = 0); treatment outcome (failure = 1, cure = 0).
Statistical Analysis
Data were analyzed using statistical software SPSS 20.0. All collected data were processed as count data and expressed in the form of rate. A preliminary chi-square (χ2) analysis is performed to screen out potential influencing factors, and then those factors were incorporated into the regression equation to analyze the relationship between the relevant parameters and the success rate of radical cure. Step forward method was used and P <0.05 was considered statistically significant.
Results
Hp Eradication Rate and the Results of the Univariate Analysis
The Hp eradication rate was 80.06%, and the results of the univariate analysis of the potential effecting factors about the eradication rate, with statistically significant differences (P<0.05), were as follows: vitamin D level (less than 20 ng/mL), positive CagA, presence of oral diseases, medical compliance, and retreatment. There were no significant differences between the two groups in gender, age, BMI, education level, place of residence, income, marital status, the presence or absence of complications, smoking, consumption of alcohol, and the presence or absence of gastric atrophy (P>0.05) (see Table 1).
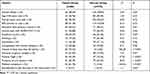 |
Table 1 Univariate Analysis of Eradication Treatment Failure in Patients with HP Infection |
PPIs and Antibiotics Selection
Patients who took the same PPI were grouped into the same PPIs group, and there were 4 groups as follows, the esomeprazole group, the rabeprazole group, the omeprazole group, and the lansoprazole group. Patients using rabeprazole were with the highest successful eradication rate (89.90%), and then followed by esomeprazole (89.02%), omeprazole (70.24%), and lansoprazole (65.82%). There was a statistically significant difference among the four groups, χ2=21.66, P<0.001.
There were four antibiotic combination regimens, the eradication cure rate was solution 2 (Amoxicillin 1.0g bid+Tetracycline 250mg tid) (88.66%), and the lowest was solution 3 (Amoxicillin 1.0g bid+Levofloxacin 0.5g qd) (66.04%), and there were statistically significant differences among the four antibiotic combinations, P=0.001 (see Table 2).
 |
Table 2 Success Rate of Hp Eradication with Four Different PPIs and Antibiotics |
Multivariate Logistic Regression Analysis of the Hp Eradication Rate
Multivariate logistic regression analysis was carried out, and the results with statistical significance in the univariate analysis were set as the independent variables. The results of the multivariate logistic regression analysis revealed that vitamin D level (<20 ng/mL) [OR=98.56, 95% CI (29.01–334.83), P<0.001] and medical compliance [OR=148.18, 95% CI (37.64–583.33), P<0.001] were independent effecting factors for eradication rate (see Table 3).
 |
Table 3 Multivariate Logistic Regression Analysis of Hp Eradication Failure |
Discussion
Several strains and host factors can affect the Hp eradication, including antibiotic resistance, virulence factors, and host genetic factors. In the present study, the univariate analysis identified five factors, vitamin D level (less than 20 ng/mL), positive CagA, presence of oral diseases, medical compliance, and retreatment, which were statistically significant differences between the failure group and the success group. The multivariate regression analysis identified that vitamin D level (<20 ng/mL) and medical compliance were independent effecting factors for eradication rate. These findings are consistent with previous studies. First, the latest meta-analysis results suggested that vitamin D was a protective factor to Hp infection, and vitamin D can improve the successful eradication rate of Hp;13 meanwhile, previous studies had found that vitamin D3 decomposition product (VDP), (1R, 3aR, 7aR)-1-[(1R)-1,5-imethylhexyl]octahydro-7a-methyl-4h-inden-4-one, can selectively kill Hp, and VDP may induce bacterial lysis by interacting with 14:0 fatty acids in Hp cell membrane components;14,15 other studies have found that the alkyl group of indene in the decomposition product of vitamin D3 has a key conformation interacting with the Hp membrane lipid component di-14:0 PtdEtn, eventually cleaving Hp cells; the absence of alkyl can therefore lead to the loss of the bactericidal effect on Hp.16,17 Second, the CagA can affect gastric mucosa inflammation and injury by activating inflammatory cell infiltration;18,19 one study suggested that oral cavities are an important gathering place of Hp in the human body, making oral diseases an important factor of secondary gastric Hp infection.20 However, in this study, authors failed to make a real-time polymerase chain reaction (PCR) to confirm the presence of Hp or the presence of DNA of Hp in the oral cavity, which may explain why the factor, presence of oral disease, was excluded in the multivariate logistic regression analysis.
With the popularization of the Hp eradication program and the application of non-standard anti-Hp treatment in clinical practice, Hp drug resistance has appeared more vigorously and become one of the main reasons for treatment failure. In both developed and developing countries, the level of antimicrobial resistance has increased significantly in recent years, while the eradication rate of Hp has decreased significantly. A previous study revealed that drug resistance to metronidazole and clarithromycin has gradually increased in China, reaching more than 50%.5 These medications were not used in the present study and this study used the approved modified quadruple therapy including geographically sensitive antibiotics. However, the antibiotic treatment regimens in this study were not unified and were not determined based on the results of culturing and the antimicrobial susceptibility studies, and were more empirically administered under the guidance of the consensus, which may cause some confounds in this study.
The present study compared the Hp eradication rates of four different PPIs, with that of rabeprazole being highest at 89.90%; this was followed by esomeprazole at 89.02%, omeprazole at 70.24%, and lansoprazole at 65.82% (P < 0.001). The ability of PPIs to inhibit gastric acid secretion is affected by individual gene polymorphism, so PPIs that are less affected by gene polymorphism were selected. The results of the present study are consistent with findings from previous studies, which revealed that the eradication rates of esomeprazole and rabeprazole were high.21,22 Rabeprazole was ranked first in the probability best test, with OR to be 1.29 (95% CI 1.08–1.56) when compared with omeprazole, followed by esomeprazole. It should be noted that there is no statistically significant difference in the overall radical cure rate among patients using different PPI regimens, suggesting that all four types of PPIs can be effectively applied to modified quadruple therapy and this result is consistent with the previous study that choice of PPI did not affect the eradication rate.23 However, when interpreting the results of the effect of different PPIs on the eradication rate in this study, it should be noted that there were also differences in the types of antibiotics used with different PPIs, which may also lead to some confoundings affecting the interpretation of the results.
What we must be concerned about is that this study only found that the vitamin D level below 20 ng/mL, which is an independent risk factor, is associated with the failure of a radical cure. However, how and when to add vitamin D supplements can increase the eradication rate of Hp has not yet been determined. To increase the serum level of vitamin D to more than 20 ng/mL before starting the eradication treatment, or after the initiation of the radical cure remains to be further studied.
It is important to note that some patients in the present study did not follow the prescribed anti-Hp treatment or took their PPIs and antibiotics irregularly due to adverse drug reactions, which increased the resistance to PPIs and antibiotics, making it more difficult to eradicate Hp. Therefore, it is recommended that it would be better to take actions to supervise and to guide the medication usage, to improve the eradication rate.
The study also has limitations. First, the sample size was relatively small, and it was an observational study, which only investigated the relationship between the vitamin D level before the radical cure and the eradication rate of Hp. The positive results of this study provide a basis for the implementation of an intervention study to verify the effectiveness of vitamin D supplementation with larger sample size; second, there are no specific restrictions on the PPIs used in this study, which may lead to observational bias. In the further studies, the choice of PPIs in the radical treatment regimen should be preferably limited; third, the data collected in this study were treated as categorical data rather than measurement data, at the cost of reduced power, which may be controversial; fourth, in this study, The selection of antibiotics was empirical and not based on the results of culturing and antimicrobial susceptibility studies; fifth, this study did not evaluate the presence of Hp infection in the oral cavity, which may be valuable in the further studies.
Conclusion
Serum vitamin D level may affect the eradication of Hp and it is an independent risk factor. Patients infected with Hp combined with a serum vitamin D deficiency may need vitamin D supplementation. It is also recommended that patients with Hp infection should be given medication guidance to enhance medication compliance.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sugano K. Screening of gastric cancer in Asia. Best practice & research. Clin Gastroenterol. 2015;29(6):895–905. doi:10.1016/j.bpg.2015.09.013
2. Khalilpour A, Kazemzadeh-narbat M, Tamayol A, et al. Biomarkers and diagnostic tools for detection of Helicobacter pylori. Appl Microbiol Biotechnol. 2016;100(11):4723–4734. doi:10.1007/s00253-016-7495-7
3. Sitas F. Twenty five years since the first prospective study by Forman et al. (1991) on Helicobacter pylori and stomach cancer risk. Cancer Epidemiol. 2016;41:159–164. doi:10.1016/j.canep.2016.02.002
4. Nagy P, Johansson S, Molloy-bland M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016;8:8. doi:10.1186/s13099-016-0091-7
5. Thung I, Aramin H, Vavinskaya V, et al. Review article: the global emergence of Helicobacter pylori antibiotic resistance. Aliment Pharmacol Ther. 2016;43(4):514–533. doi:10.1111/apt.13497
6. Yuan G, Chen Y, He S. Family history of gastric cancer and Helicobacter pylori treatment. N Engl J Med. 2020;382(22):2171.
7. Mathew JM. H pylori eradication therapy reduces gastric cancer in patients with or without gastric neoplasia. Ann Intern Med. 2020;173(6):JC32. doi:10.7326/ACPJ202009150-032
8. Sassi F, Tamone C, D’amelio P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients. 2018;10(11):1656. doi:10.3390/nu10111656
9. El Shahawy MS, Shady ZM, Gaafar A. Influence of adding vitamin D3 to standard clarithromycin-based triple therapy on the eradication rates of Helicobacter pylori infection. Arab J Gastroenterol. 2021;22(3):209–214. doi:10.1016/j.ajg.2021.08.002
10. Liu WZ, Xie Y, Lu H, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi:10.1111/hel.12475
11. Li Y, Lin R, Jin Y, et al. Genotyping Helicobacter pylori antibiotic resistance and virulence-associated genes in patients with gastric cancer in Wenzhou, China. Arab J Gastroenterol. 2021;22(4):267–271. doi:10.1016/j.ajg.2021.05.017
12. Rajavi Z, Sabbaghi H, Amini Sharifi E, et al. Comparison between patching and interactive binocular treatment in amblyopia: a randomized clinical trial. J Curr Ophthalmol. 2019;31(4):426–431. doi:10.1016/j.joco.2019.07.004
13. Antico A, Tozzoli R, Giavarina D, et al. Hypovitaminosis D as predisposing factor for atrophic type A gastritis: a case-control study and review of the literature on the interaction of Vitamin D with the immune system. Clin Rev Allergy Immunol. 2012;42(3):355–364. doi:10.1007/s12016-011-8255-1
14. Yildirim O, Yildirim T, Seckin Y, et al. The influence of vitamin D deficiency on eradication rates of Helicobacter pylori. Adv Clin Exp Med. 2017;26(9):1377–1381. doi:10.17219/acem/65430
15. Huang B, Yan S, Chen C, et al. Effect of 25-hydroxyvitamin D on Helicobacter pylori eradication in patients with type 2 diabetes. Wien Klin Wochenschr. 2019;131(3–4):75–80. doi:10.1007/s00508-018-1416-y
16. El Shahawy MS, Hemida MH, El Metwaly I, et al. The effect of vitamin D deficiency on eradication rates of Helicobacter pylori infection. JGH Open. 2018;2(6):270–275. doi:10.1002/jgh3.12081
17. Yang L, He X, Li L, et al. Effect of vitamin D on Helicobacter pylori infection and eradication: a meta-analysis. Helicobacter. 2019;24(5):1–7. doi:10.1111/hel.12655
18. Wanibuchi K, Hosoda K, Ihara M, et al. Indene compounds synthetically derived from vitamin D have selective antibacterial action on Helicobacter pylori. Lipids. 2018;53(4):393–401. doi:10.1002/lipd.12043
19. Han C, Ni Z, Yuan T, et al. Influence of serum vitamin D level on Helicobacter pylori eradication: a multi-center, observational, prospective and cohort study. J Dig Dis. 2019;20(8):421–426. doi:10.1111/1751-2980.12793
20. Knorr J, Ricci V, Hatakeyama M, et al. Classification of Helicobacter pylori virulence factors: is CagA a toxin or not? Trends Microbiol. 2019;27(9):731–738. doi:10.1016/j.tim.2019.04.010
21. Tohidpour A. CagA-mediated pathogenesis of Helicobacter pylori. Microb Pathog. 2016;93:44–55. doi:10.1016/j.micpath.2016.01.005
22. Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017;22(Suppl 1):e12403. doi:10.1111/hel.12403
23. Padula W. Letter concerning vision therapy: ocular motor training in mild traumatic brain injury. Ann Neurol. 2021;89(4):847–848. doi:10.1002/ana.26026
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
