Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Factor Structure and Measurement Invariance of the Hospital Anxiety and Depression Scale Across the Peripartum Period Among Pregnant Japanese Women
Authors Ogawa M, Watanabe Y , Motegi T, Fukui N, Hashijiri K, Tsuboya R, Sugai T, Egawa J, Araki R, Haino K, Yamaguchi M, Nishijima K, Enomoto T , Someya T
Received 30 November 2020
Accepted for publication 1 January 2021
Published 26 January 2021 Volume 2021:17 Pages 221—227
DOI https://doi.org/10.2147/NDT.S294918
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Maki Ogawa,1 Yuichiro Watanabe,1 Takaharu Motegi,1 Naoki Fukui,1 Koyo Hashijiri,1 Ryusuke Tsuboya,1 Takuro Sugai,1 Jun Egawa,1 Rie Araki,2 Kazufumi Haino,3 Masayuki Yamaguchi,3 Koji Nishijima,4 Takayuki Enomoto,3 Toshiyuki Someya1
1Department of Psychiatry, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan; 2Nursing, Niigata University Medical and Dental Hospital, Niigata, Japan; 3Department of Obstetrics and Gynecology, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan; 4General Center for Perinatal, Maternal and Neonatal Medicine, Niigata University Medical and Dental Hospital, Niigata, Japan
Correspondence: Yuichiro Watanabe
Department of Psychiatry, Niigata University Graduate School of Medical and Dental Sciences, 757 Asahimachidori-Ichibancho, Chuo-ku, Niigata 951-8510, Japan
Tel +81-25-227-2213
Fax +81-25-227-0777
Email [email protected]
Purpose: The Hospital Anxiety and Depression Scale (HADS) is a self-report questionnaire widely used to assess anxiety and depression. To the best of our knowledge, only four studies have examined the factor structure of the HADS for assessing pregnant women, with conflicting results. This study aimed to assess the factor structure and measurement invariance of the HADS for use with pregnant Japanese women.
Participants and Methods: A total of 936 pregnant Japanese women completed the HADS questionnaire at three time points: the first and third trimester of pregnancy, and postpartum. We examined the factor structure of the HADS in Group 1 (n = 466) using exploratory factor analysis (EFA). We then compared the models identified in Group 1 with those from previous studies using confirmatory factor analysis (CFA) in Group 2 (n = 470). We performed multiple-group CFA for Group 2 to test the measurement invariance of the best-fit model across the three time points.
Results: The EFA for the Group 1 data at the three time points revealed a two-factor model. In the CFA, the two-factor model from Group 1 showed the best fit with the data at the three time points. In the multiple-group CFA for Group 2, we confirmed the configural and metric invariance of the two-factor model across the three time points.
Conclusion: Our findings provide evidence for a two-factor structure and weak measurement invariance of the HADS in pregnant Japanese women during the peripartum period.
Keywords: confirmatory factor analysis, exploratory factor analysis, Hospital Anxiety and Depression Scale
Introduction
The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-report questionnaire that was designed to assess anxiety and depression at non-psychiatric hospital clinics.1 The HADS contains anxiety and depression subscales, each consisting of seven items. This scale is used worldwide in several clinical and research settings.2 Numerous studies have examined the factor structure of the HADS in various ethnic populations such as Chinese,3 Dutch,4 and German2 participants with several thousand samples. However, these studies have produced conflicting results.2–7 Inconsistencies among studies may stem from differences in the study population (eg non-clinical individuals and cancer patients), ethnicity (eg Chinese, Dutch, and German) and method (eg exploratory factor analysis [EFA] and confirmatory factor analysis [CFA]). Therefore, the factor structure of the HADS should be identified individually for each population and ethnicity using both EFA and CFA with independent datasets.
The HADS has been widely used in pregnant women to identify peripartum anxiety and depression.8–20 To the best of our knowledge, four studies have examined the factor structure of the HADS for pregnant women.11,12,16,20 Karimova and Martin12 conducted an EFA in British and Uzbek women (n = each 50) when they were 12- and 34-weeks pregnant. They found that the factor structures varied between British and Uzbek women as well as between the two time points. Jomeen and Martin11 performed both EFA and CFA with the same dataset of 101 pregnant British women. However, no models showed a good fit with the data in the CFA. Waqas et al20 found a one-factor structure using both EFA and CFA with the same dataset of 500 pregnant Pakistani women. Lodhi et al16 reported that EFA of 200 pregnant Pakistani women resulted in an ambiguous two-factor structure. These inconsistencies indicate that further studies are required to determine the factor structure of the HADS in pregnant women. Further, while some studies conducted HADS twice during the peripartum period,12,13,15,18 no studies have tested the measurement invariance of the HADS across the peripartum period.
The factor structure of the HADS has been examined in Japanese populations of cancer patients, psychiatric outpatients, and undergraduate students. Kugaya et al21 supported the original two-factor structure (anxiety and depression subscales)1 using CFA in 128 cancer patients. Matsudaira et al22 identified a two-factor structure where two items had dual loadings using both EFA and CFA in the combined data from 408 psychiatric outpatients and 1069 undergraduate students. However, the factor structure of the HADS in pregnant Japanese women has not been determined.
To identify the factor structure of the HADS, it is necessary to use both EFA and CFA with independent datasets. Further, to validate the measurement invariance of the HADS across the peripartum period, a multiple-group CFA is required. Here, we performed EFA, CFA, and multiple-group CFA among 936 pregnant Japanese women at three time points: the first and third trimester of pregnancy, and postpartum.
Paticipants and Methods
Ethics Statement
This study followed the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Niigata University (approval number: 2016–0019) and the ethics committees of the participating obstetric institutions. Written informed consent was obtained from all participants.
Participants
This study is part of the Perinatal Mental Health Research Project23,24 and comprises a sub-analysis of data collected between March 2017 and March 2020. Participants were 936 pregnant Japanese women, recruited from 34 obstetric institutions in Niigata Prefecture.23,24 Each participant was randomly assigned to Group 1 (n = 466) or 2 (n = 470) for EFA and CFA, respectively.
Measurements
The HADS is a 14-item self-report questionnaire.1 Each item is graded on a 4-point Likert scale (0–3 points) and items 1, 3, 5, 6, 8, 10, 11, and 13 are reverse-scored. Anxiety and depression subscales consist of odd and even numbered items, respectively. Higher HADS scores indicate more severe symptoms. The Japanese version of the HADS25 was validated in a previous study.21 Participants in the present study completed the HADS questionnaire at three time points: the first trimester (approximately 12–15 weeks) and third trimester (approximately 30–34 weeks) of pregnancy and postpartum (4 weeks after childbirth).
Statistical Analysis
We examined the factor structure of the HADS in Group 1 using an EFA within Statistical Package for the Social Sciences (SPSS) v25.0 (IBM Japan, Tokyo, Japan). We determined the number of factors from a scree plot. We used the maximum likelihood method and the promax rotation for the EFA. We considered items with factor loadings greater than 0.35 in a particular factor to belong to that factor. Cronbach’s α was employed to evaluate internal consistency. Cronbach’s α ≥0.80 and ≥0.70 showed good and acceptable internal consistency, respectively.
We compared four models in Group 2 using a CFA within Analysis of Moments Structures (AMOS) v25.0.0 (IBM Japan, Tokyo, Japan). The four models were: the two-factor model from Zigmond and Snaith,1 the two-factor model from Matsudaira et al22, the one-factor model from Waqas et al20, and the two-factor model identified by the EFA of data from Group 1. We assessed the fit of each model to the data using the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). A good fit was indicated by CFI ≥ 0.95 and RMSEA ≤ 0.05, whereas an acceptable fit was indicated by CFI ≥ 0.90 and RMSEA ≤ 0.10. Akaike’s Information Criterion (AIC) and a chi-square, normalized by degrees of freedom (chi-squared/df), were also used to measure the goodness of fit. Lower AIC and chi-squared/df values indicate a better fit.
We performed a multiple-group CFA on the data from Group 2 to test the measurement invariance of the best-fit model across the three time points. We subsequently tested the configural, metric, and scalar invariance. A change in CFI (ΔCFI) ≤0.01 for two nested models was considered to confirm measurement invariance.
Results
Groups 1 and 2 were age-matched (mean age ± SD: 31.1 ± 4.7 and 31.2 ± 5.1 years, respectively). There were no significant differences in the mean total, anxiety, and depression HADS scores between Groups 1 and 2 at the three time points (Table 1).
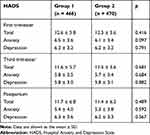 |
Table 1 HADS Total, Anxiety, and Depression Scores in Groups 1 and 2 |
First, we performed an EFA for the 466 participants in Group 1 (Table 2). Cronbach’s α for the 14-item HADS was 0.786, 0.809, and 0.833 in the first trimester, third trimester, and postpartum, respectively. A scree plot suggested two factors, with an eigenvalue greater than 1. Factor 1 included seven items (1, 3, 5, 8, 9, 11, and 13), with the exception of item 8 in the first trimester. This factor explained 0.182, 0.196, and 0.233 of the total variance in the first trimester, third trimester, and postpartum, respectively. Cronbach’s α for the seven items of Factor 1 was 0.778, 0.774, and 0.830 at the three time points, respectively. Factor 2 included seven items (2, 4, 6, 7, 10, 12, and 14), with the exception of item 10 in the third trimester. This factor explained 0.151, 0.162, and 0.191 of the total variance in the first trimester, third trimester, and postpartum, respectively. Cronbach’s α for the seven items of Factor 2 was 0.724, 0.719, and 0.769 at the three time points, respectively.
 |
Table 2 Exploratory Factor Analysis of HADS in Group 1 |
Second, we performed a CFA to compare the four models in Group 2 (Table 3). The two-factor model identified in Group 1 showed the best fit with the data. In the first trimester, CFI (0.935) showed an acceptable fit, whereas RMSEA (0.050) showed a good fit. In the third trimester, CFI (0.940) and RMSEA (0.051) showed acceptable fits. In the postpartum period, CFI (0.976) and RMSEA (0.033) showed good fits.
 |
Table 3 Confirmatory Factor Analysis of HADS in Group 2 |
Third, we performed a multiple-group CFA in Group 2 to assess the measurement invariance of our two-factor model across the peripartum period (Table 4). In the configural invariance model, CFI (0.952) and RMSEA (0.026) showed good fits. In the metric invariance model, CFI (0.943) showed an acceptable fit, whereas RMSEA (0.027) showed a good fit. Metric invariance was confirmed (ΔCFI = 0.009). In the scalar invariance model, CFI (0.903) showed an acceptable fit, whereas RMSEA (0.034) showed a good fit. However, scalar invariance was not confirmed (ΔCFI = 0.040). In the metric invariance model, all items had loadings ≥0.35 on a latent factor, with the exception of item 8 (Figure 1). The latent factors were correlated (r = 0.43).
 |
Table 4 Multiple-Group Confirmatory Factor Analysis of HADS in Group 2 |
Discussion
In the present study, EFA and CFA confirmed the two-factor structure of the HADS in 936 pregnant Japanese women at three time points: first trimester (approximately 12–15 weeks), third trimester (approximately 30–34 weeks), and postpartum (4 weeks after childbirth). Multiple-group CFA confirmed the configural and metric invariance of the two-factor model across the three time points, indicating weak measurement invariance. Factors 1 and 2 are regarded as anxiety and depression, respectively, with a moderate correlation. We observed good or acceptable internal consistency of the 14 HADS items: seven for Factor 1 and seven for Factor 2.
We used EFA and CFA to identify the two-factor structure of the HADS in 936 pregnant Japanese women across the peripartum period. Karimova and Martin12 performed an EFA of British and Uzbek women (n = each 50) when they were 12- and 34-weeks pregnant. In the British women, five- and two-factor structures were identified at the two time points, whereas two- and three-factor structures were found in the Uzbek women. Karimova and Martin claimed that the HADS was inappropriate for assessing pregnant women; however, their sample size was insufficient to conduct an EFA. Therefore, no definitive conclusion can be drawn from their study. Jomeen and Martin11 performed both EFA and CFA with the same dataset of 101 pregnant British women. While EFA revealed a three-factor structure, none of eight models tested using CFA exhibited a good fit with the data. Waqas et al20 performed both EFA and CFA with the same dataset of 500 pregnant Pakistani women. EFA showed a one-factor structure to be more interpretable than a two-factor structure, while CFA showed a one-factor structure, excluding items 11 and 14, to have a good fit (CFI = 0.95 and RMSEA = 0.05). Lodhi et al16 performed an EFA of 200 pregnant Pakistani women. They identified a two-factor structure where items 3, 6, 7, and 13 had dual loadings while item 14 did not belong to either factor with a low factor loading. Therefore, the two-factor model seems to be inappropriate. Differences in ethnicity are likely to explain the inconsistent findings among studies. Further studies should be carried out in various ethnic populations.
To the best of our knowledge, this is the first study to confirm the factor structure of the HADS in pregnant Japanese women. In our two-factor structure, items 7 (an anxiety item) and 8 (a depression item) loaded on Factor 2 (depression) and Factor 1 (anxiety), respectively. Kugaya et al21 supported the original two-factor structure (ie anxiety and depression subscales consisting of odd and even number items, respectively) using CFA in 128 cancer patients. Matsudaira et al22 performed EFA and CFA in 739 and 738 datasets, respectively, from the combined data of 408 psychiatric outpatients and 1069 undergraduate students. They identified the two-factor structure where items 6 and 7 had dual loadings. Taken together, these findings indicate that the HADS has a two-factor structure of anxiety and depression in the Japanese population, although the items constituting the two factors are not necessarily the same among studies. Of note, item 7 (“I can sit at ease and feel relaxed”) loaded as a depression factor in 20 of 36 studies using EFA.6 This anomalous factor loading may stem from the ambiguous wording of item 7.22
A major strength of this study is that the factor structure of the HADS was identified by EFA in a randomly selected group comprising half of the participants (Group 1; n = 466) and cross-validated using CFA in the other half (Group 2; n = 470). We also recognize the limitations of this study. First, the multiple-group CFA confirmed the configural and metric invariance of the HADS across the peripartum period, indicating weak but not strong measurement invariance. Second, participants were recruited from 34 obstetric institutions in Niigata Prefecture, Japan. However, the study population may not be representative of the general population of pregnant Japanese women. Further studies should be performed in a larger sample of pregnant Japanese women to confirm our findings.
Conclusion
Our findings provide evidence for a two-factor structure and weak measurement invariance of the HADS in pregnant Japanese women across the peripartum period.
Abbreviations
AIC, Akaike’s information criterion; CFA, confirmatory factor analysis; CFI, comparative fit index; EFA, exploratory factor analysis; HADS, Hospital Anxiety and Depression Scale; RMSEA, root mean square error of approximation.
Acknowledgments
The authors greatly appreciate the involvement of all participants and staff of the participating obstetric institutions: Kameda Daiichi Hospital, Niitsu Obstetrics and Gynecology Clinic, Tomita Obstetrics and Gynecology Clinic, Honda Ladies Clinic, Agano City Hospital, Chihara Clinic, Sekizuka Clinic, Hirohashi Obstetrics and Gynecology Clinic, Niigata Saiseikai Sanjo Hospital, Saiseikai Niigata Hospital, Itoigawa Sogo Hospital, Niigata Prefectural Tokamachi Hospital, Takeyama Hospital, Watanabe Kinen Clinic, Kashiwazaki General Hospital and Medical Center, Kido Hospital, Tachikawa Medical Center, Saintpaulia Women’s Clinic, Nagaoka Chuo General Hospital, Arakawa Ladies Clinic, Ueda Ladies Clinic, Uonuma Kikan Hospital, Murakami General Hospital, Sado General Hospital, Tokunaga Ladies Clinic, Nagaoka Red Cross Hospital, Niigata Prefectural Shibata Hospital, Ladies Clinic Ishiguro, Angel Mother Clinic, Joetsu General Hospital, Niigata City General Hospital, Ojiya General Hospital, Watanabe Clinic, and Niigata University Medical and Dental Hospital. We thank Jeremy Allen, PhD, and Sydney Koke, MFA, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
This work was supported by Grants-in-Aid for Scientific Research (19K08040 to NF) from the Japan Society for the Promotion of Science, by a grant from the Niigata Medical Association (to TM), and by a grant from the Medical Association of Niigata City (to MO).
Disclosure
Toshiyuki Someya reports grants and personal fees from Astellas Pharma Inc., Eli Lilly Japan K.K., Mitsubishi Tanabe Pharma Co., Mochida Pharmaceutical Co., Ltd., MSD K.K., Novartis Pharma K.K., Otsuka Pharmaceutical Co., Ltd., Shionogi Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd., outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
1. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x.
2. Herrmann C. International experiences with the hospital anxiety and depression scale–a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi:10.1016/s0022-3999(96)00216-4.
3. Chan YF, Leung DY, Fong DY, et al. Psychometric evaluation of the hospital anxiety and depression scale in a large community sample of adolescents in Hong Kong. Qual Life Res. 2010;19(6):865–873. doi:10.1007/s11136-010-9645-1.
4. Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. doi:10.1017/s0033291796004382.
5. Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/s0022-3999(01)00296-3.
6. Cosco TD, Doyle F, Ward M, et al. Latent structure of the hospital anxiety and depression scale: a 10-year systematic review. J Psychosom Res. 2012;72(3):180–184. doi:10.1016/j.jpsychores.2011.06.008.
7. Norton S, Cosco T, Doyle F, et al. The hospital anxiety and depression scale: a meta confirmatory factor analysis. J Psychosom Res. 2013;74(1):74–81. doi:10.1016/j.jpsychores.2012.10.010.
8. Abiodun OA. A validity study of the hospital anxiety and depression scale in general hospital units and a community sample in Nigeria. Br J Psychiatry. 1994;165(5):669–672. doi:10.1192/bjp.165.5.669.
9. Berle JØ, Mykletun A, Daltveit AK, et al. Neonatal outcomes in offspring of women with anxiety and depression during pregnancy. A linkage study from The Nord-Trøndelag Health Study (HUNT) and medical birth registry of Norway. Arch Womens Ment Health. 2005;8(3):181–189. doi:10.1007/s00737-005-0090-z.
10. Çankaya S. The effect of psychosocial risk factors on postpartum depression in antenatal period: a prospective study. Arch Psychiatr Nurs. 2020;34(3):176–183. doi:10.1016/j.apnu.2020.04.007.
11. Jomeen J, Martin CR. Is the hospital anxiety and depression scale (HADS) a reliable screening tool in early pregnancy? Psychol Health. 2004;19(6):787–800. doi:10.1080/0887044042000272895
12. Karimova G, Martin C. A psychometric evaluation of the hospital anxiety and depression scale during pregnancy. Psychol Health Med. 2003;8(1):89–103. doi:10.1080/1354850021000059296.
13. Kita S, Haruna M, Matsuzaki M, et al. Associations between intimate partner violence (IPV) during pregnancy, mother-to-infant bonding failure, and postnatal depressive symptoms. Arch Womens Ment Health. 2016;19(4):623–634. doi:10.1007/s00737-016-0603-y.
14. Kitamura T, Takegata M, Haruna M, et al. The mother-infant bonding scale: factor structure and psychosocial correlates of parental bonding disorders in Japan. J Child Fam Stud. 2015;24:393–401. doi:10.1007/s10826-013-9849-4.
15. Lee AM, Lam SK, Sze Mun Lau SM, et al. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110(5):1102–1112. doi:10.1097/01.AOG.0000287065.59491.70.
16. Lodhi FS, Elsous AM, Irum S, et al. Psychometric properties of the Urdu version of the Hospital Anxiety and Depression Scale (HADS) among pregnant women in Abbottabad, Pakistan. Gen Psychiatr. 2020;33(5):e100276. doi:10.1136/gpsych-2020-100276.
17. Qiao YX, Wang J, Li J, et al. The prevalence and related risk factors of anxiety and depression symptoms among Chinese pregnant women in Shanghai. Aust N Z J Obstet Gynaecol. 2009;49(2):185–190. doi:10.1111/j.1479-828X.2009.00966.x.
18. van de Loo KFE, Vlenterie R, Nikkels SJ, et al. Depression and anxiety during pregnancy: the influence of maternal characteristics. Birth. 2018;45(4):478–489. doi:10.1111/birt.12343.
19. Waqas A, Raza N, Lodhi HW, et al. Psychosocial factors of antenatal anxiety and depression in Pakistan: is social support a mediator? PLoS One. 2015;10(1):e0116510. doi:10.1371/journal.pone.0116510.
20. Waqas A, Aedma KK, Tariq M, et al. Validity and reliability of the Urdu version of the hospital anxiety & depression scale for assessing antenatal anxiety and depression in Pakistan. Asian J Psychiatr. 2019;45:20–25. doi:10.1016/j.ajp.2019.08.008.
21. Kugaya A, Akechi T, Okuyama T, et al. Screening for psychological distress in Japanese cancer patients. Jpn J Clin Oncol. 1998;28(5):333–338. doi:10.1093/jjco/28.5.333.
22. Matsudaira T, Igarashi H, Kikuchi H, et al. Factor structure of the hospital anxiety and depression scale in Japanese psychiatric outpatient and student populations. Health Qual Life Outcomes. 2009;7:42. doi:10.1186/1477-7525-7-42.
23. Motegi T, Fukui N, Hashijiri K, et al. Identifying the factor structure of the mother-to-infant bonding scale for post-partum women and examining its consistency during pregnancy. Psychiatry Clin Neurosci. 2019;73(10):661–662. doi:10.1111/pcn.12920.
24. Motegi T, Watanabe Y, Fukui N, et al. Depression, anxiety and primiparity are negatively associated with mother–infant bonding in Japanese mothers. Neuropsychiatr Dis Treat. 2020;16:3117–3122. doi:10.2147/NDT.S287036.
25. Kitamura T. Hospital anxiety and depression scale. Arch Psychiatr Diagn Clin Eval. 1993;4:371–372.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

