Back to Journals » Clinical Ophthalmology » Volume 17
Eye Donation: Knowledge, Beliefs, Awareness, and Willingness Among Ambulance Drivers in Central India
Authors Joshi RS , Goel P, Adatiya VH, Seth AS, Rasal AV
Received 20 January 2023
Accepted for publication 24 April 2023
Published 1 May 2023 Volume 2023:17 Pages 1263—1269
DOI https://doi.org/10.2147/OPTH.S401768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Rajesh Subhash Joshi, Pranshu Goel, Vaishnavi Hitesh Adatiya, Ayushi Sanjay Seth, Ashwini Vitthalrao Rasal
Department of Ophthalmology, Government Medical College, Nagpur, Maharashtra, 440003, India
Correspondence: Rajesh Subhash Joshi, Department of Ophthalmology, Government Medical College, Nagpur, Maharashtra, 440003, India, Email [email protected]
Aim: To determine the awareness about and willingness to donate eyes among ambulance drivers in Central India.
Design: Prospective, observational, noncomparative, and cross-sectional survey study.
Setting: Tertiary eye care center in Central India.
Methods: The present study used a structured questionnaire distributed to ambulance drivers during the eye donation fortnight (August 25–September 8, 2022). The questionnaire comprised four domains: awareness, knowledge beliefs, and willingness to donate eyes. The collected data were entered into an Excel sheet and analyzed using SPSS software.
Results: Forty-seven ambulance drivers participated in the study. All participants were men. The results showed that 48.9% (n = 23) of the ambulance drivers had completed elementary or middle school education. Furthermore, 27 (57%) participants were aware of eye donation; however, only 14 (29.7%) realized its importance. The source of information was mobile phones (n = 20, 42.6%). The common reason for the nondonation of eyes was lack of awareness (n = 14 29.7%). Thirty-five (74.5%) ambulance drivers were willing to donate their eyes, and the most common reason was the gratification derived from helping blind people.
Conclusion: The study revealed the need to improve awareness and knowledge about eye donation among the participants. Arranging short sessions round the year, addressing the myths associated with eye donation, and sharing motivational stories may help create awareness. Display of information and booklets on eye donation in the ambulance is likely to help in obtaining more corneas for transplantation.
Keywords: corneal transplantation, eye donation, eye donation fortnight, awareness of eye donation
Introduction
Corneal blindness is the major cause of blindness and is attributed to corneal ulceration, penetrating corneal injury, nutritional deficiency, trachoma, postsurgical bullous keratopathy, and corneal degeneration.1–3 The population-based Central India Eye and Medical Study from the rural area has shown that 2% of the rural population is blind owing to corneal problems. In this study, the total population studied was 4711.4 Corneal Opacity Rural Epidemiological Study has shown the prevalence of corneal diseases to be 3.7% (95% confidence interval [CI] 3.4–4.1%).3 The Andhra Pradesh Eye Disease Study (APEDS) has shown a significant burden of corneal blindness in rural populations, of which 95% is preventable.5 Corneal transplant surgery is the only treatment for corneal opacity. According to the National Programme for Control of Blindness (NPCB), there are currently 120,000 corneal blind people in India, and every year, an additional 25,000–30,000 cases are added.6 Presently, in India, the donor eye collection is 22,000 eyes every year, which is insignificant with respect to the requirement.7
Currently, the only way to obtain more corneas is by creating awareness on eye donation. The reason for inadequate eye donations need not necessarily be a lack of awareness. There could be other factors, such as physical, cultural, social, or psychological barriers, involved in the apathy toward the donation of eyes. During the COVID-19 pandemic, eye banking in India and all over the world was seriously affected.8,9 A survey conducted by Nathawat et al has reported a steep decline in corneal collection. There was a decline in eye donation of 78.27% and 79.14% in March–May 2020 compared with the same period in 2019.8 Now, this phase has passed. However, there is a pressing need to compensate for the backlog of corneal transplantation. Therefore, we aimed to evaluate the knowledge, attitudes, beliefs, awareness, and willingness regarding eye donation among ambulance drivers in Central India. We believe that ambulance drivers are the first ones to come in contact with seriously ill people and those who have met with road traffic accidents as well as their relatives. The role of ambulance drivers in this connection has not been explored. It may not be a part of their role. However, they may communicate with the relatives of seriously ill patients. To the best of our knowledge, the literature search did not reveal such a study (Medline search 4/8/2019).
Materials and Methods
This prospective, cross-sectional, observational survey was performed in the metropolis city of Central India during the eye donation fortnight of the year 2022 (August 25–September 8) among ambulance drivers. The study was approved by the ethical committee of the Government Medical College and hospital, Nagpur, India (Ethical committee letter No.1875 EC/Pharmac/GMC/NGP). Each participant provided written informed consent prior to participation in the study. The study adhered to the tenets of the Declaration of Helsinki. A pretested questionnaire was administered to ambulance drivers in the city with the preamble of the corneal blindness scenario in India. The questionnaire was validated and pretested by the subject experts. The questionnaire contained a demographic profile, awareness about eye donation, and their willingness and motivation for eye donation. The full questionnaire is furnished in Appendix-1.2 The questionnaire was filled out physically in the native language. The data were entered into an Excel® sheet (software version 14.1.0 [110310]/2011) (Microsoft Corporation, Redmond, WA, USA), and statistical analysis was performed with SPSS version 13.0 (SPSS Inc, Chicago, IL, USA).
Results
Forty-seven ambulance drivers participated in the study. The overall response rate was 94% (47/50). All participants were men. Their age distribution is presented in Table 1. The majority of the ambulance drivers were in the age group of 31–40 years (n = 20, 42.6%), followed by 20–30 years (n = 15, 31.9%). Details of their level of education are listed in Table 2. The findings indicated that 48.9% (n = 23) of ambulance drivers had completed elementary or middle school education, followed by high school (10+2) education (n = 15, 31.9%). Only one driver had completed postgraduation. It was noted that 27 (57%) of the 47 ambulance drivers were aware of eye donation. However, only 14 (29.7%) drivers were aware of the fact that eye donation is important and that eyes can be donated after death. Twenty (43%) ambulance drivers were aware of the existence of an eye bank. Furthermore, 74.5% (n = 35) of the ambulance drivers were willing to donate their eyes. Details of the response to the questionnaire are given in Table 3.
 |
Table 1 Showing Age Distribution of Ambulance Drivers |
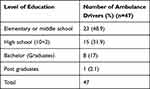 |
Table 2 Showing level of Education |
 |
Table 3 Responses to the Questionnaire on Eye Donation |
Table 4 shows the source of information on eye donation. The most common source was mobile phones (n = 20, 42.6%), followed by television (n = 6, 12.8%), radio, cinema hall posters, and family members (n = 3, 6.4%). Reasons cited for not donating the eyes are shown in Table 5. The most common reason was lack of awareness (n = 14, 29.7%), followed by delay in performing religious rights and dislike for separating the eyes (n = 10, 21.3%). The reasons for eye donation are depicted in Table 6. Thirty-five (74.5%) ambulance drivers were willing to donate their eyes, citing the most common reason as the gratification derived from helping blind people (17,48.6%). Other reasons were eye donation being a virtuous gesture (n = 8, 22.9%) and the donated eye giving vision to the blind (n = 4, 11.4%). The complete details are presented in Table 6.
 |
Table 4 Source of Information Regarding Eye Donation |
 |
Table 5 Reasons for Not Donating Eyes |
 |
Table 6 Reasons for Eye Donation (n = 35) @ |
Discussion
The present study examined the awareness and knowledge regarding eye donation among ambulance drivers in Central India. In the face of an increase in the demand for eye donation, the findings of the study are valuable. Awareness about eye donation targeting the population, which will help to contribute to the cause, is of prime importance.
The results of this study showed that awareness and knowledge about corneal donation are associated with a positive outlook toward eye donation. In the wake of the lack of awareness on eye donation, when the questionnaire was floated among ambulance drivers with information about corneal blindness in India, 74.5% (n = 35) were willing to donate their eyes after death. A similar observation has been shared by Gupta et al in their study on eye donation awareness among nursing students.10 Alanazi et al showed that a high level of awareness about eye donation is associated with the willingness to donate eyes.11 They reported that participants who had sufficient information about corneal donation were more likely to donate their eyes than those who did not believe that they had sufficient information.11 Similar observations have been recorded in several studies.12,13
Awareness about eye donation is an important part of the eye donation movement. In the current study, a lack of awareness on eye donation was seen in 57% (n = 27) of the participants, which suggests the need to create eye donation awareness among them. We could not compare the findings of our study as there are no available studies on eye donation awareness among ambulance drivers. However, a similar reason has been cited in other studies on eye donation awareness.11–13 A study on the rural population in India opined that lack of awareness about eye donation is a key factor that hinders eye donation.2 Krishnaiah et al, in their study on awareness about eye donation among the rural population of India, observed that only 30.7% of the population was aware of eye donation.2 Similar findings were noted by Priyadarshini et al in a preliminary survey conducted at the Aravind Eye Care system in the southern part of India.14 On the contrary, Singh et al, in their study on awareness about eye donation in urban slum populations, reported excellent awareness. However, the willingness to donate was very low.15
The need of the hour is to target ambulance drivers who transport seriously ill and road traffic accident patients to the hospital. Information on the importance of eye donation, who can donate eyes, where eyes can be donated, and who are benefitted from the donation should be made readily available, and awareness about eye donation should be created from time to time. Display of the information and the booklets about eye donation in the ambulance will help in the procuring of corneas from donors.
Delay in performing the religious rights (n = 10, 21.3%), dislike for separating the eyes (n = 10, 21.3%), and objection by family members (n = 6, 12.8%) were the other reasons cited for the non-willingness to donate eyes. Similar reasons have been mentioned in various studies across India and abroad.2,10–17 This finding suggests that myths regarding eye donation still exist and need to be addressed. In our study, 48.9% (n = 23) of the ambulance drivers had elementary or middle school education and only one driver (2.1%) had completed postgraduation. A research on awareness about eye donation among nursing and medical students showed little influence of myths on eye donation.18 The education level of the participants helps reduce the belief in myths associated with eye donation.18–20 However, the most important part of eye donation is to motivate family members after death.
Approximately 57% (n = 27) of the ambulance drivers were aware of the existence of eye donation, and 29.7 (n = 14) were aware that eyes could be donated after death and that eye donation is important.
The knowledge about eye donation was found to be low in our study compared with other studies. Singh et al, in their study on eye donation in the urban slum population in New Delhi, reported that 65.72% of the participants were aware of eye donation.15 Kacheri et al recorded an awareness rate of 93.3% on eye donation among paramedical and allied health science students in a South Indian teaching hospital.21 Sushma et al noted an awareness rate of 99.2% among medical and paramedical students in a tertiary care hospital.22 These reports signify that we should take efforts to incorporate knowledge about eye donation at the high school level, irrespective of the stream of the study. The knowledge about the donation of eyes after death was poor in our study compared with the study by Kacheri et al (n = 85/150, 56%), Bhandary et al (88%), Singh et al (99.4%), Ronaki et al (80.3%), and Biswas et al (81%).16,19,21,23,24 Poor knowledge about eye donation was also seen in the study by Lal et al in which only 33% of the participants were aware of eye donation after death.25
Our study revealed that 27.6% (n = 13) of the participants were aware of the optimal time for the removal of eyes after death, which is less than that reported by Kacheri et al (67%), Singh et al (41.1%), and Chowdhury et al (69%).18,21,23
In the current study, barely 43% (n = 20) of the participants were aware of the existence of eye banks in the city. There has been variability in the awareness about the existence of eye banks in various studies. Bharti et al, in their study on awareness about eye donation among the first year studies of medicine and allied branches, observed that majority of the students (94%) were unaware of the existence of eye banks in the vicinity.26 A similar observation (94%) was also made by Kumar et al.27 Lal et al documented that 44.4% of the students were unaware of the presence of eye banks in Goa.24 Singh et al also reported low (67.4%) awareness about eye banks among medical students,28 which could be attributed to the lack of knowledge about the geographical aspects of the city.
Most studies have stated that television is an important source of information regarding eye donation.10,18,25,29 However, in the present study, most participants relied on mobile phones (n = 20, 42.6%) for information about eye donation. This fact should be taken into consideration. Mobile phones are indeed handy tools for acquiring information.
Of the 35 participants (74.5%) who were willing to donate their eyes, 48.6% (n = 17) mentioned gratification obtained from helping a blind person and 22.9% (n = 8) cited eye donation being a virtuous gesture. Other reasons quoted by the participants were donated eyes giving vision to the blind, a friend or relative having donated their eyes, and influence of a movie. Similar reasons have been stated in various studies.20–25
The present study was conducted during the eye donation fortnight celebration to encourage eye donation in this part of the country. A follow-up study after 1 year with the same participants will help assess the impact of the study.
All participants in the present study were men, which led to the bias of failing to assess women. To the best of our knowledge, we could not find a woman ambulance driver in the city. Another limitation of the study was the small sample size, which was unavoidable as there were limited number of ambulance drivers in the city. Extrapolation of the data from the present study should be done cautiously as the participants belong to the urban area and variabilities in opinion may prevail across geographical locations.
The response rate was good (94%, 47/50), which could be ascribed to the clear explanation of the scenario regarding the shortage of eye donations in the country, answering all quarries related to the survey, and encouraging the cause on a one-to-one basis while completing the survey forms. Denial to complete the survey was the only reason cited by the non-willing participants.
Conclusion
The findings of the present study revealed the need to improve awareness and knowledge about eye donation among the studied participants. Although awareness was low, most of the participants were willing to donate their eyes. Arranging short sessions round the year on eye donation and the myths associated with it and sharing motivational stories may help create awareness. The most common source for information on eye donation was mobile phones. We need to keep pace with changing times. This new medium will help encourage eye donation.
We need to target ambulance drivers who transport seriously ill and road traffic accident patients to the hospital. Display of information and booklets on eye donation in the ambulance will help in increasing awareness and obtaining more corneas.
Notwithstanding these efforts, it may take a long time to motivate people and achieve the target of eliminating corneal blindness.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Madan AH, Joshi RS, Wadekar PD. Ocular trauma in pediatric age group at a tertiary eye care center in central Maharashtra, India. Clin Ophthalmol. 2020;14:1003–1009. doi:10.2147/OPTH.S244679
2. Krishnaiah S, Kovai V, Nutheti R, Shamanna BR, Thomas R, Rao GN. Awareness of eye donation in the rural population of India. Indian J Ophthalmol. 2004;52:73–78.
3. Gupta N, Vashist P, Tandon R, Gupta SK, Dwivedi S, Mani K. Prevalence of corneal diseases in the rural Indian population: the Corneal Opacity Rural Epidemiological (CORE) study. Br J Ophthalmol. 2015;99:147–152. doi:10.1136/bjophthalmol-2014-305945
4. Nangia V, Jonas JB, Gupta R, Khare A, Sinha A. Visual impairment and blindness in rural central India: the central India eye and medical study. Acta Ophthalmol. 2013;91(5):483–486. doi:10.1111/j.1755-3768.2012.02447.x
5. Dandona L, Dandona R, Srinivas M, et al. Blindness in Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci. 2001;42:908–916.
6. National programme for control of blindness; 2017. Available from: http://pbhealth.gov.in/pdf/Blindness.pdf.
7. Dafne LP, Dangre DM, Patil AB, Wangikar VD. Who cares for eye donation. Int J Public Health Hum Rights. 2012;2(1):11e15.
8. Nathawat R, Sharma N, Sachdev MS, Sinha R, Mukherjee G. Immediate impact of COVID-19 on eye banking in India. Indian J Ophthalmol. 2021;69(12):3653–3657. doi:10.4103/ijo.IJO_1171_21
9. Manara AR, Mumford L, Callaghan CJ, Ravanan R, Gardiner D. Donation and transplantation activity in the UK during the COVID-19 lockdown. Lancet. 2020;396(10249):465–466. doi:10.1016/S0140-6736(20)31692-5
10. Gupta A, Jain S, Jain T, Gupta K. Awareness and perception regarding eye donation in students of a nursing college in Bangalore. Indian J Community Med. 2009;34:122–125. doi:10.4103/0970-0218.51235
11. Alanazi LF, Aldossari SH, Gogandy MA, Althubaiti GA, Alanazi BF, Alfawaz AM. Attitude, beliefs and awareness towards corneal donation in Saudi Arabia. Saudi J Ophthalmol. 2019;33:121–129. doi:10.1016/j.sjopt.2019.02.003
12. Paraz CM, Truong HT, Sai DK, Cajucom-Uy HY, Chan CL, Kassim SM. Knowledge and attitudes toward corneal donation among Singaporean youth: a cross-sectional study. Eye Vis. 2016;3:17. doi:10.1186/s40662-016-0049-3
13. Wang X, Jin L, Wang J, et al. Attitudes and knowledge concerning corneal donation in a population-based sample of urban Chinese adults. Cornea. 2016;35(10):1362–1367. doi:10.1097/ICO.0000000000000943
14. Priyadarshini B, Srinivasan M, Padmavathi A, Selvam S, Saradha R, Nirmalan PK. Awareness of eye donation in an adult population of southern India. A Pilot Study. Indian J Ophthalmol. 2003;51:101–104.
15. Singh A, Gupta N, Ganger A, Vashist P, Tandon R. Awareness regarding eye donation in an urban slum population: a community-based survey. Exp Clin Transplant. 2018;16:730–735. doi:10.6002/ect.2017.0077
16. Bhandary S, Khanna R, Rao KA, Rao LG, Lingam KD, Binu V. Eye donation - awareness and willingness among attendants of patients at various clinics in Melaka, Malaysia. Indian J Ophthalmol. 2011;59(1):41–45. doi:10.4103/0301-4738.73727
17. Yew YW, Saw SM, Pan JC, et al. Knowledge and beliefs on corneal donation in Singapore adults. Br J Ophthalmol. 2005;89:835–840. doi:10.1136/bjo.2004.057372
18. Chowdhury RK, Dora J, Das P. Awareness of eye donation among medical and nursing students: a comparative study. Indian J Ophthalmol. 2021;69(6):1511–1515. doi:10.4103/ijo.IJO_2053_20
19. Ronanki VR, Sheeladevi S, Ramachandran BP, Jalbert I. Awareness regarding eye donation among stakeholders in Srikakulam district in South India. BMC Ophthalmol. 2014;14:25. doi:10.1186/1471-2415-14-25
20. Egnasious J, Srinivasan K, Ramesh SV, Noushad B. Knowledge, awareness, perception, and willingness towards eye donation among the literate working population. Asian J Ophthalmol. 2018;16:7–18. doi:10.35119/asjoo.v16i1.336
21. Kacheri A, Mudhol R, Chougule S, Reny R, Kamath S, Kamath R. Eye donation: awareness, knowledge, willingness, and barriers among paramedical and allied health science students at a tertiary care teaching hospital in South India. ScientificWorldJournal. 2022;2022:5206043. doi:10.1155/2022/5206043
22. Sushma H, Warad VG, Kshetrapal M. Knowledge, attitude and practice about eye donation among medical and paramedical students in tertiary eye care hospital. Kerala J Ophthalmol. 2016;28:112. doi:10.4103/kjo.kjo_30_16
23. Singh MM, Rahi M, Pagare D, Ingle GK. Medical students’ perception on eye donation in Delhi. Indian J Ophthalmol. 2007;55:49–53. doi:10.4103/0301-4738.29495
24. Lal B, Usgaonkar U, Narvekar H, Venugopal D. Awareness and knowledge on eye donation among allied health sciences, medical, and nursing students in Goa. J Curr Ophthalmol. 2018;30(3):255–262. doi:10.1016/j.joco.2018.02.002
25. Biswas J, Bandyopadhyay S, Das D, Mandol KK, Saha I, Ray B. A study in awareness about eye health care and eye donation among secondary level students of North Kolkata, India. Kathmandu Univ Med J. 2010;8(31):317–320. doi:10.3126/kumj.v8i3.6219
26. Bharti MK, Reddy SC, Tajunisah I, Ali NA. Awareness and knowledge on eye donation among university students. Med J Malaysia. 2009;64:41–45.
27. Kumar S, Shukla US, Agarwal P. Awareness and knowledge on eye donation among students at Bhopal. Natl J Community Med. 2012;3:685e689.
28. Singh M, Bhardwaj A, Ahluwalia S, Saini S, Qadri S. Eye donation: perception and promoting factors among medical students. Indian J Community Health. 2012;24:175e178.
29. Jayashree MP, Pujar C, Gadag VR, Salagar M, Pattnaik M. Comparison of awareness of eye donation among medical and paramedical students. J Clin Res Ophthalmol. 2017;4:6–9.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
