Back to Journals » International Journal of General Medicine » Volume 15
Expression Characteristics and Significant Diagnostic and Prognostic Values of ANLN in Human Cancers
Authors Ahmad M, Khan M , Asif R, Sial N, Abid U , Shamim T , Hameed Z, Iqbal MJ, Sarfraz U, Saeed H, Asghar Z , Akram M , Ullah Q, Younas QUA, Rauf L, Hadi A , Maryam S , Hameed Y , Khan MR, Tariq E, Saeed S
Received 9 November 2021
Accepted for publication 24 December 2021
Published 23 February 2022 Volume 2022:15 Pages 1957—1972
DOI https://doi.org/10.2147/IJGM.S343975
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mukhtiar Ahmad,1,* Mehran Khan,2,* Rizwan Asif,3,* Nuzhat Sial,4,* Usman Abid,5,* Tahira Shamim,6 Zahid Hameed,7 Muhammad Junaid Iqbal,8,* Uroosa Sarfraz,8 Hina Saeed,1,* Zara Asghar,2 Madeeha Akram,2 Qamar Ullah,9 Qurat ul Ain Younas,10 Laraib Rauf,11 Alishba Hadi,1 Sajida Maryam,12 Yasir Hameed,1 Muhammad Rashid Khan,13,* Eman Tariq,14 Saba Saeed15,*
1Department of Biochemistry and Biotechnology, Islamia University of Bahawalpur, Bahawalpur, Pakistan; 2Department of Pharmacy, Islamia University of Bahawalpur, Bahawalpur, Pakistan; 3Department of Microbiology, Government College University Faisalabad, Faisalabad, Pakistan; 4Department of Zoology, Islamia University of Bahawalpur, Bahawalpur, Pakistan; 5Department of Pharmaceutics, Bahauddin Zakariya University, Multan, Pakistan; 6University College of Conventional Medicine, Islamia University of Bahawalpur, Bahawalpur, Pakistan; 7Department of Bioinformatics and Biotechnology, International Islamic University, Islamabad, Pakistan; 8Department of Biosciences, COMSATS University Islamabad, Islamabad, Pakistan; 9Department of Livestock and Dairy Development, Peshawar, Pakistan; 10Department of Zoology, Cholistan University of Veterinary and Animal Sciences, Bahawalpur, Pakistan; 11Department of Healthcare Management, Riphah International University, Islamabad, Pakistan; 12Arid Agriculture University, Rawalpindi, Pakistan; 13University College of Eastern Medicine, Islamia University of Bahawalpur, Bahawalpur, Pakistan; 14Department of Chemistry, University of Swabi, Swabi, Pakistan; 15Department of Zoology, University of the Punjab, Lahore, Pakistan
*These authors contributed equally to this work
Correspondence: Yasir Hameed, Department of Biochemistry and Biotechnology, Islamia University of Bahawalpur, Bahawalpur 63100, Pakistan, Email [email protected]
Introduction: In light of the increased demand for reliable cancer-associated biomarkers and ANLN oncogenic potential, the present study aimed to investigate ANLN’s role in 24 human cancers.
Methods: The UALCAN, Kaplan–Meier (KM) plotter, TNM Plot, GENT2, GEPIA, HPA, cBioPortal, STRING, Enrichr, TIMER, Cytoscape, DAVID, MuTarget, and CTD online databases and bioinformatic tools were used in this study.
Results: In three of the cancers analyzed, ANLN expression was downregulated in tumor tissue, while it was overexpressed in the 21 other types of tumor tissue relative to controls. In CESC, ESCA, HNSC, and KIRC patients, ANLN overexpression was correlated with shorter overall survival, relapse-free survival, and metastasis. This suggests that ANLN is significantly involved in the development and progression of these four cancers. Further expression analysis revealed upregulation of ANLN in CESC, ESCA, HNSC, and KIRC patients with different clinical characteristics, regardless of the heterogeneity barrier. Gene Ontology and Kyoto Encyclopedia of Genes and Genomes enrichment analysis revealed that ANLN-associated genes were coexpressed with ANLN and were included in diverse BP, MF, and KEGG terms. Moreover, some interesting correlations were also documented between ANLN expression and its promoter-methylation level, genetic alterations, other mutant genes, and CD8+ T- and CD4+ T-cell infiltration. Moreover, we also identified ANLN-associated transcription factors, miRNAs, and chemotherapeutic drugs.
Conclusion: This pan-cancer study revealed the novel diagnostic and prognostic role of ANLN across four cancers, regardless of heterogeneity.
Keywords: cancer, ANLN, diagnostic, prognostic, biomarker
Introduction
Cancer is a multifactorial disease with various potential causes.1 In 2020, around 8.7 million cancer deaths were reported worldwide and the disease declared the second-leading cause of death after cardiovascular disorders.2 Although these massive figures show that the battle against cancer has not been won yet, recent advances in personalized medicine and treatment strategies like immunotherapy have significantly improved the survival of cancer patients.3 However, cancer is still rising significantly and results in tremendous social and economic burdens around the world. As such, exploring the underlying biological mechanisms of carcinogenesis and investigating the possible potential diagnostic and prognostic biomarkers of cancer is urgent.
 |
Table 1 GO and KEGG enrichment analysis of ANLN-enriched genes |
Anillin (ANLN) is an actin-binding protein that was originally discovered in Drosophila and is primarily involved in cytokinesis.4 The ANLN gene is located at the 7p14.2 position in the human genome and is involved in the recruitment of numerous key cell division–associated genes, such as F-actin, myosin II, and septins, and is thus regarded as the major organizer of the cytokinetic machinery.5 It has been reported that mutations and expression variations in ANLN contribute significantly to the development and progression of human cancers.6 So far, ANLN dysregulation has been reported in different human cancers, ie, in breast, colorectal, liver, lung, endometrial, kidney, ovarian, brain, and pancreatic cancers.7 A bioinformatics-based study revealed that the ANLN gene can be an ideal prognostic biomarker for evaluating the survival of cervical cancer patients.8,9 In addition, ANLN was found to cause chemotherapy resistance in breast cancer cells by directly reducing the effectiveness of doxorubicin during a clinical trial.10 As ANLN upregulates in tumor tissue and its expression increases as the disease progresses, this gene holds great promise as a potential biomarker of cancer development and progression.7,11,12 Due to the increasing prevalence of cancer cases worldwide, elucidation of underlying molecular mechanisms and the discovery of more sensitive diagnostic and prognostic biomarkers of cancer is critical to managing the disease.
In this study, we carried out a systematic expression analysis and evaluated the diagnostic and prognostic values of ANLN. Additionally, we also analyzed the correlation of ANLN expression with its promoter-methylation level, other mutant genes, and CD4+ and CD8+ T cells. Finally, using online databases, we identified transcription factors (TFs), miRNAs, and important chemotherapeutic drugs targeting ANLN.Our results revealed the unique role of ANLN in cervical squamous-cell carcinoma (CESC), esophageal carcinoma (ESCA), head-and-neck squamous-cell carcinoma (HNSC), and kidney renal clear-cell carcinoma (KIRC), as well as suggesting this gene as a reliable diagnostic and prognostic biomarker in these cancers.
Methods
Ethics
This study was reviewed and approved by the ethics committee of Islamia University of Bahawalpur, Bahawalpur, Pakistan.
UALCAN Analysis
The UALCAN web tool facilitates multiomic analysis with respect to both MET500 and TCGA cancer genomic data.13 In this work, we performed pan-cancer differential expression and promoter-methylation analysis of ANLN across multiple human cancer types using UALCAN. mRNA-expression level were normalized as transcripts per million reads, while promoter-methylation level were normalized as β values. As with all statistical analyses herein, Student’s t-test was employed and P<0.05 taken as significant.
KM Plotter–Based Analysis
Kaplan–Meier (KM) plotter (https://kmplot.com/analysis) is a user-friendly online tool designed for survival analysis of the gene of interest in 21 different cancer patients. This tool contains mRNA-expression data and survival information of cancer patients obtained from the Gene Expression Omnibus (GEO).14 Briefly, ANLN was searched to obtain KM overall survival (OS) and relapse-free (RFS) plots of the available 21 cancer subtypes. P-values, 95% CIs, and HRs) were determined.
TNM Plot
This database (https://www.tnmplot.com) is designed to analyze the relative expression of any gene of interest in normal, cancerous, and metastatic tissue.15 It contains data on 3,691 normal, 29,376 tumor, and 453 metastatic samples from the GEO and 730 normal, 9,886 tumor, and 394 metastatic samples from TCGA. We used TNM Plot to analyze ANLN expression in normal and metastatic tissue from different cancers.
TIMER-, GENT2-, GEPIA-, and HPA-Based Expression-Validation Analysis
TIMER (http://timer.cistrome.org), GENT2 (http://gent2.appex.kr), GEPIA (http://gepia.cancer-pku.cn), and the Human Protein Atlas (HPA) database (https://www.proteinatlas.org) are cancer transcriptomic data-analysis websites.16–19 In the current study, we used TIMER, GENT2, and GEPIA for mRNA- and protein-expression validation of ANLN using new independent cohorts of cancer patients. In TIMER, GENT2, and GEPIA, mRNA expression was normalized as transcripts per million reads, while in the HPA protein expression was graded as not detected, low, medium, or high based on the intensity of staining and fraction of the stained cells.
MExpress
MExpress (https://mexpress.be) helps to analyze correlations between promoter-methylation levels and expression.20 In this study, correlations between ANLN expression and promoter-methylation levels in cancer patients were computed using this tool with the help of Pearson correlation analysis.
cBioPortal
cBioPortal is a web tool that facilitates the multiomic analysis using TCGA cancer-genome data.21 This tool provides comprehensive detail regarding copy-number variation (CNV) and genetic mutations in the gene of interest. Additionally, this tool also evaluates the association between gene mutation and the prognosis of cancer patients. We used cBioPortal to evaluate and analyze the ANLN genetic alterations and CNVs in TCGA’s data set of cancers.
PPI-Network Construction, Visualization, Gene Ontology (GO), and Kyoto Encyclopedia of Genes and Genomes (KEGG) Pathway-Enrichment Analysis
The STRING database (http://string-db.org) is an online source for constructing PPI networks of genes of interest.22 We utilized this user-friendly tool to construct a PPI network of ANLN-enriched genes. This was further visualized with Cytoscape software.23 Then, GO and KEGG analysis of the ANLN-enriched genes were performed using DAVID (http://david.ncifcrf.gov/summary.jsp).24
Correlation of ANLN with Related Genes
GEPIA (http://gepia.cancer-pku.cn) was utilized to compute correlations between ANLN and related genes with the help of the “Correlation Analysis” module.
ANLN and CD4+ and CD8+ T Cells
TIMER (http://timer.cistrome.org) helps in the evaluation of immune-cell infiltration and clinical/therapeutic effects.25 This resource helped us to compute Spearman correlations between ANLN expression and CD4+ T- and CD8+ T-cell infiltration in cancer patients.
Enrichr Database Analysis
Enrichr (https://maayanlab.cloud/Enrichr)26 facilitates analysis of gene(s) of interest using enrichment terms, eg, functional, targeted miRNAs, and pathway-enrichment terms. In this study, we identified ANLN-targeted miRNAs and TFs using this web source. The top-ten significantly enriched terms are given in the Results section.
MuTarget Analysis
The MuTarget (https://www.mutarget.com/result) platform is principally designed to associate gene expression with mutational status in cancer samples.27 We identified mutant genes responsible for expression alterations in ANLN using this tool. Based on Mann–Whitney P-values and mean FC, significant genes were selected for testing, where we used default thresholds of P≤0.05 and 0.714>FC>1.4.
ANLN Gene–Drug Interaction-Network Analysis
The Comparative Toxicogenomics Database (CTD; http://ctdbase.org) is used to retrieve information on chemotherapeutic drugs that can change the expression of genes of interest.28 ANLN was queued in CTD and a gene–drug interaction network visualized with Cytoscape to recognize ANLN-interacting drugs that may help in the treatment of distinct human cancers by regulating ANLN expression.
Results
Expression-Level Analysis of ANLN in Distinct Types of Human Cancer
To find differences in ANLN expression in tumors and normal tissue, TCGA expression profiles across 24 types of tumor samples and paired normal tissue were utilized through the UALCAN platform. Results demonstrated that ANLN was down-regulated in glioblastoma, skin cutaneous melanoma, and thymoma, while it was overexpressed in all the remaining 21 types of cancer samples compared to normal controls, including CESC, ESCA, HNSC, and KIRC (Figure 1).
ANLN Prognostic Potential in Different Types of Cancer
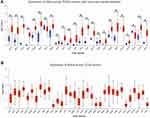
KM Plotter was used to investigate the prognostic potential of ANLN in different types of cancer. Overexpression of ANLN was significantly associated with decreased OS and RFS duration of CESC (HR 1.77, 95% CI 1.1–2.83, P=0.016; HR 2.14, 95% CI 0.98–4.68, P=0.05), ESCA (HR 2.64, 95% CI 1.36–5.15, P=0.003, HR 271493743.64, 95% CI0–Inf; P=0.028), HNSC (HR 1.36, 95% CI 1.2–1.81, P=0.034; HR 2.08, 95% CI 0.88–4.09, P=0.0087), and KIRC (HR 2.25, 95% CI 1.68–3.04, P=8.2–8, HR 1.83, 95% CI 0.65–5.16, P=0.024) patients (Figure 2A and B). ANLN overexpression was also positively correlated with metastasis of CESC, ESCA, HNSC, and KIRC (Figure 2C). Taken together, these data suggest that ANLN might contribute significantly to the development and progression of CESC, ESCA, HNSC, and KIRC, and thus the next part of our study mainly focused on the unique role of ANLN in these four cancer types.
Transcription and Translational Expression–Level Validation of ANLN Using New Independent Cohorts
To further validate ANLN expression at transcription and translational levels, we reanalyzed its expression using new independent cohorts of CESC, ESCA, HNSC, and KIRC via TIMER, GENT2, GEPIA, and the HPA. Reanalysis also revealed significant overexpression of ANLN at both transcription and translational level in the new cohorts of patients relative to normal controls (Figure 3).
ANLN Overexpressed in CESC, ESCA, HNSC, and KIRC Patients with Different Clinicopathological Features
The distinct cancer types (CESC, ESCA, HNSC, and KIRC) in which ANLN showed significant negative correlations with OS and RFS duration were reanalyzed to verify the significance of ANLN expression in normal and cancerous samples with clinicopathological parameters: cancer stage, patient age, patient ethnicity, and nodal metastasis. ANLN was significantly overexpressed in all CESC, ESCA, HNSC, and KIRC patients with different clinicopathological parameters compared to the normal controls (Figure 4). Taken together, this implies that ANLN is overexpressed in CESC, ESCA, HNSC, and KIRC patients, regardless of the heterogeneity barrier.
Promoter-Methylation Analysis of ANLN
It is known that inactivation of tumor-suppressor genes due to hypermethylation of the promoter region leads to cancer.29 To assess ANLN promoter methylation in defined cancer types, we utilized the UALCAN database. The results suggested that the promoter level of ANLN was significantly lower in CESC, ESCA HNSC, and KIRC samples (Figure 5). Therefore, the overall data suggested a negative correlation between ANLN expression and promoter methylation in CESC, ESCA, HNSC, and KIRC samples compared to the normal controls.
 |
Figure 5 Promoter-methylation analysis of ANLN in CESC, ESCA, HNSC, and KIRC via UALCAN. (A) CESC; (B) ESCA; (C) HNSC; (D) KIRC. *P<0.05. |
Promoter Methylation–Level Validation of ANLN Using New Independent Cohorts
To validate ANLN promoter methylation in the new independent cohorts of CESC, ESCA, HNSC, and KIRC, we used MExpress. It was observed that promoter methylation values obtained from the different methylation probes in CESC, ESCA, HNSC, and KIRC were also significantly negatively correlated with ANLN expression levels (Figure 6).
 |
Figure 6 Promoter methylation–level validation of ANLN in CESC, ESCA, HNSC, and KIRC via MEXPRESS. (A) CESC; (B) ESCA; (C) HNSC; (D) KIRC. *P<0.05, **P<0.001, ***P<0.0001. |
Copy-Number Variations and Mutational Analysis of ANLN
Information related to ANLN genetic alterations — deep amplification, deep deletion, genetic mutation, and fusion — in CESC, ESCA, HNSC, and KIRC was obtained from TCGA CESC, ESCA, HNSC, and KIRC (TCGA, PanCancer Atlas) data sets consisting of 297, 182, 523, and 512 cancerous samples, respectively. Results revealed that ANLN harbored genetic alterations in only 0.8% cases of CESC, 5% cases of ESCA, 2.8% cases of HNSC, and 0.6% cases of KIRC, with maximum missense mutations in CESC, HNSC, and KIRC and maximum deep amplification in ESCA (Figure 7).
PPI Network of ANLN, GO, and KEGG Analysis
We constructed a PPI of ANLN-associated genes via STRING and visualized it through. In total, ten ANLN interacting genes were identified through this network. We then performed GO and KEGG enrichment analysis of ANLN-associated genes. ANLN-associated genes were significantly involved in mitotic cytokinesis, positive regulation of cytokinesis, mitotic nuclear division, microtubule-based movement, and regulation of small GTPase–mediated signal-ransduction biological process (BP) terms, protein-kinase binding, microtubule binding, ATP binding, and microtubule motor-activity molecular function (MF) terms, and KEGG terms: progesterone-mediated oocyte maturation, oocyte meiosis, and the cell cycle (Figure 8 and Table 1).
Correlation Analysis Between ANLN and Associated Gene Expression
We used GEPIA to analyze correlations between ANLN and associated gene (explored via STRING) expression in CESC, ESCA, HNSC, and KIRC. ANLN expression was strongly positively correlated with expression levels of PHOA, RACGAP1, KIF23, KIF20A, KIF11, ECT2, DLGAP5, CDK1, CDC5L, and BUB1 (Figure 9). Based on these results, we speculated that along with ANLN, dysregulation of its other associated genes may also play a tumor-promoting role in CESC, ESCA, HNSC, and KIRC.
 |
Figure 9 Correlation analysis of ANLN and associated gene expression in CESC, ESCA, HNSC, and KIRC samples. |
ANLN and Infiltrating Levels of CD8+ and CD4+ T Cells
Functions of and interactions between the innate and adaptive immune systems are vital for anticancer immunity. Cytotoxic T cells expressing cell-surface CD8+ and CD4+ T cells are the most powerful effectors in anticancer immune response and form the backbone of current successful cancer immunotherapies.30 In the current study, Spearman correlations between expression of ANLN and CD8+ and CD4+ T cells was calculated using TIMER. Results revealed a significant egative correlation between the mRNA expression of ANLN and CD8+ T–cell levels in CESC, ESCA, and HNSC and significant positive correlation in KIRC (Figure 10). On the other hand, a significant positive correlation between mRNA expression of ANLN and CD4+ T–cell levels was also found in CESC, ESCA, HNSC, and KIRC (Figure 10).
Identification of miRNAs and TFs That Potentially Regulate ANLN
Enrichr was utilized to predict the ANLN targeted TFs, and miRNAs. In total, the ten most significant TFs (E2F1, E2F3, TP53, E2F4, YBX1, TRP53 [mouse], RBL2 [mouse], FOXM1, MYC, and ARID3A) and ten miRNAs (hsa-miR215-5p, hsa-miR192-5p, hsa-miR193b-3p, hsa-miR34a-5p, hsa-miR92a-3p, hsa-miR16-5p, hsa-miR18b-5p, hsa-miR6507-5p, hsa-miR221-3p, and hsa-miR24-1-5p) were identified that potentially regulate ANLN expression (Figure 11). Taken together, these clues highlight that ANLN expression can be regulated by a variety of factors.
 |
Figure 11 ANLN-targeted TFS and miRNAs in human cancers. (A) ANLN-targeted TFS; (B) ANLN-targeted miRNAs. |
Correlations Between ANLN and Other Mutant Genes
To identify mutant genes responsible for ANLN overexpression, we used MuTarget and selected the top three mutant genes for CESC, ESCA, HNSC, and KIRC patient. As shown in Figure 12, the top three mutant genes positively correlated with the expression of ANLN were LMO1, WHSC1L1, and SPRY1 in CESC, FMNL2, DNM2, and CACNA11 in ESCA, GYPA, SLCO1B1, and CRACR2A in HNSC, and XIRP2, ZGRF1, and FAM178A in KIRC. Collectively, these results suggest that ANLN expression has strong correlations with different mutant genes in CESC, ESCA, HNSC, and KIRC.
Gene–Drug Interaction-Network Analysis of ANLN
In order to explore the relationship between ANLN and available cancer therapeutic drugs, a gene–drug interaction network was developed using CTD. ANLN expression can be influenced by a variety of drugs. For example, estradiol and ionomycin can elevate the expression level of ANLN, while sunitinib and cyclosporine can reduce ANLN expression (Figure 13).
Discussion
Although ANLN has been explored in few cancers,7,11,12 its role in other subtypes of human cancer has yet to be uncovered. In the current study, we identified significant associations between ANLN expression and CESC, ESCA, HNSC, and KIRC. We found that ANLN was downregulated in three types of cancer tissue and overexpressed in another 21 types relative to controls and its overexpression was significantly correlated with the decreased OS and RFS duration, and advanced metastasis of CESC, ESCA, HNSC, and KIRC. Altogether, these results support that ANLN may play a key role in the initiation and development of CESC, ESCA, HNSC, and KIRC. Therefore, in the present study, our main focus was these four cancers. Due to heterogeneity, CESC, ESCA, HNSC, and KIRC may remain a serious therapeutic issue for clinicians and doctors. Therefore, we further evaluated the clinicopathological feature–specific expression of ANLN in CESC, ESCA, HNSC, and KIRC patients. ANLN was also significantly overexpressed in CESC, ESCA, HNSC, and KIRC patients with clinicopathological features of different cancer stage, age, ethnicity, and nodal metastasis. Therefore, since ANLN expression was higher in CESC, ESCA, HNSC, and KIRC samples relative to controls, we believe that it is more important to reduce the expression of ANLN using different chemotherapeutics drugs to treat CESC, ESCA, HNSC, and KIRC patients.
Next, we tried to explore the possible causes of ANLN overexpression, so we carried out correlation analyses between ANLN overexpression and promoter-methylation level, CNV, and genetic mutations in CESC, ESCA, HNSC, and KIRC. ANLN harbored genetic alterations in very small proportions of the cancer patients (0.8% of CESC, 5% of ESCA, 2.8% of HNSC, and 0.6% of KIRC), with maximum missense mutations in CESC, HNSC, and KIRC and maximum deep amplification in ESCA. Therefore, we speculate that these genetic changes might participate in ANLN overexpression at a low level. Moreover, ANLN promoter-methylation analysis revealed that promoter-methylation level of ANLN was significantly (lower in CESC, ESCA, HNSC, and KIRC samples. Therefore, we speculate that ANLN overexpression can be the result of significant hypomethylation in CESC, ESCA, HNSC, and KIRC. To the best of our knowledge, this study is the first to correlate ANLN expression with genetic alterations and promoter-methylation levels in CESC, ESCA, HNSC, and KIRC.
Gynecological cancer, including CESC, is a leading cause of cancer-related deaths in women. Various studies have been conducted worldwide to identify CESC-specific diagnostic and prognostic biomarkers, eg, Berger et al31 identified various mutated genes and CNV abnormalities in CESC by analyzing GEO datasets. Song et al32 developed a long noncoding RNA–miRNA–mRNA network in CESC using GEO data sets and provided novel insights into CESC biology. However, none of the biomarkers has been generalized so far in CESC patients with various clinicopathological features for diagnosis and predicting the prognosis of CESC. We showed significant upregulation of ANLN expression in CESC patients with various clinicopathological features, ie, different cancer stage, age, ethnicity, and nodal metastasis compared to the normal controls.
Recently, various ESCA-related molecular biomarkers have been investigated, including ASPM, AURKA, BUB1, CDC20, CENPF, DLGAP5, NEK2, TOP2A, TPX2, and UBE2C.33 However, none of these biomarker has been generalized in ESCA patients with various clinicopathological features for diagnosis and predicting the prognosis of ESCA. In the present study, we revealed significant upregulation of ANLN expression in ESCA patients with the aforementioned clinicopathological features.
At present, different molecular biomarkers, including LAMC1, LAMC2, LAMC3, and HOX, used for diagnosis and predicting the prognosis of HNSC, have certain limitations.34 None of the biomarkers has been generalized in HNSC patients with various clinicopathological features for diagnosis and predicting the prognosis of HNSC. However, In the present study, we showed a significant upregulation of ANLN expression in HNSC patients with the aforementioned clinicopathological features.
For differentiating KIRC patients from normal individuals, expression profiling of TIMP3 and HMGCS1 genes and hsa-miR21-5p and hsa-miR365a-3p miRNAs were suggested to be reliable by Huang et al.35 However, none of these or any other biomarker has been generalized so far in KIRC patients of various clinicopathological features for diagnosis and predicting the prognosis. We found significant upregulation of ANLN expression in KIRC patients with the aforementionedclinicopathological features compared to the normal controls. In sum, overexpression, promoter-methylation levels, OS, and RFS suggest ANLN to be a novel diagnostic and prognostic potential biomarker of CESC, ESCA, HNSC, and KIRC patients with different clinical variables.
TFs and miRNAs are important regulators of gene expression, and abnormalities in their expression are known to cause cancer.36,37 To discover possible roles of TFs and miRNAs in the dysregulation of ANLN, we predicted potential TFs and miRNAs of ANLN using Enrichr. Our results revealed the ten most significant TFs to be E2F1, E2F3, TP53, E2F4, YBX1, TRP53 [mouse], RBL2 [mouse], FOXM1, MYC, and ARID3A and the ten most significant miRNAs to hsa-miR215-5p, hsa-miR192-5p, hsa-miR193b-3p, hsa-miR34a-5p, hsa-miR92a-3p, hsa-miR16-5p, hsa-miR18b-5p, hsa-miR6507-5p, hsa-miR221-3p, and hsa-miR24-1-5p as potential regulator of ANLN expression. This important information might also help in understanding ANLN’s oncogenic role in more detail.
Immunotherapy is one of the most reliable treatment options for cancer patients.38 However, only a small proportion of cancer patients actually benefit from immunotherapy. CD8+ and CD4+ T cells are important components of the immunotherapy; therefore, based on these immune cells, the discovery of novel biomarkers is a clinical priority. In our study, we analyzed whether ANLN correlated with CD8+ and CD4+ T cells or not. We found interesting positive and negative correlations between ANLN expression and CD8+ and CD4+ T cells, which may open up new avenues for the treatment of CESC, ESCA, HNSC, and KIRC patients, especially those who are not getting benefits from the existing immunocheckpoint inhibitors/regulators. However, an ANLN and immune cell infiltration–based study is needed on a large scale for further confirmation of these results.
Despite the use of single-gene indicators, multigene diagnostic and prognostic approaches have recently gained traction.39 CESC, ESCA, HNSC, and KIRC patients with different types of mutation still lack any sensitive, accurate therapy. Therefore, using MuTarget, we identified mutant genes responsible for altering ANLN expression. The top three mutant genes in each of CESC, ESCA, HNSC, and KIRC were LMO1, WHSC1L1, and SPRY1 in CESC, FMNL2, DNM2, and CACNA11 in ESCA, GYPA, SLCO1B1, and CRACR2A in HNSC, and XIRP2, ZGRF1, and FAM178A in KIRC. By linking these mutant genes with ANLN expression, it is easier to identify potential multigene-based therapies in CESC, ESCA, HNSC, and KIRC.
A PPI network of ANLN-associated genes via STRING revealed a set of ten ANLN-associated genes. GO and KEGG analysis of these highlighted their involvement in mitotic cytokinesis, positive regulation of cytokinesis, mitotic nuclear division, microtubule-based movement, and regulation of small GTPase–mediated signal-transduction BP terms, while protein-kinase binding, microtubule binding, ATP binding, and microtubule motor–activity MF terms, and KEGG terms for progesterone-mediated oocyte maturation, oocyte meiosis, and the cell cycle. Moreover, a correlation analysis between ANLN and ANLN-associated gene expression revealed a strong positive correlation further validating our findings regarding GO and KEGG analysis and paved the way for further exploration of ANLN molecular function. We also identified drugs that could be useful in the treatment of CESC, ESCA, HNSC, and KIRC by targeting ANLN for expression regulation.
Conclusion
ANLN is an actin-binding protein that participates in cytokinesis. Here, we systematically utilized several gene-expression databases and bioinformatic tools to verify the diagnostic and prognostic roles of ANLN in CESC, ESCA, HNSC, and KIRC patients with different clinical variables for the first time. Our findings suggested that ANLN is a diagnostic and prognostic biomarker of CESC, ESCA, HNSC, and KIRC patients. However, further studies are required to confirm these findings.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hausman DM. What is cancer? Perspect Biol Med. 2019;62(4):778–784. doi:10.1353/pbm.2019.0046
2. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1459–1544.
3. Hanahan D. Rethinking the war on cancer. The Lancet. 2014;383(9916):558–563.
4. Field CM, Alberts BM. Anillin, a contractile ring protein that cycles from the nucleus to the cell cortex. J Cell Biol. 1995;131(1):165–178.
5. Hickson GR, O’Farrell PH. Anillin: a pivotal organizer of the cytokinetic machinery. Biochem Soc Trans. 2008;36(3):439–441.
6. Gbadegesin RA, Hall G, Adeyemo A, et al. Mutations in the gene that encodes the F-actin binding protein anillin cause FSGS. J Am Soc Nephrol. 2014;25(9):1991–2002.
7. Hall PA, Todd CB, Hyland PL, et al. The septin-binding protein anillin is overexpressed in diverse human tumors. Clin Cancer Res. 2005;11(19):6780–6786.
8. Xia L, Su X, Shen J, et al. ANLN functions as a key candidate gene in cervical cancer as determined by integrated bioinformatic analysis. Cancer Manag Res. 2018;10:663.
9. Zhang M, Wang F, Xiang Z, Huang T, Zhou WB. LncRNA XIST promotes chemoresistance of breast cancer cells to doxorubicin by sponging miR‐200c‐3p to upregulate ANLN. Clin Exp Pharmacol Physiol. 2020;47(8):1464–1472.
10. Dai X, Mei Y, Chen X, Cai D. ANLN and KDR are jointly prognostic of breast cancer survival and can be modulated for triple negative breast cancer control. Front Genet. 2019;10:790.
11. Piekny AJ, Maddox AS The myriad roles of Anillin during cytokinesis. Paper presented at: Seminars in cell & developmental biology, 2010.
12. Olakowski M, Tyszkiewicz T, Jarzab M, et al. NBL1 and anillin (ANLN) genes over-expression in pancreatic carcinoma. Folia Histochemica Et Cytobiologica. 2009;47(2):249–255.
13. Chandrashekar DS, Bashel B, Balasubramanya SAH, et al. UALCAN: a portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia (New York, N Y). 2017;19(8):649–658.
14. Maciejczyk A, Szelachowska J, Czapiga B, et al. Elevated BUBR1 expression is associated with poor survival in early breast cancer patients: 15-year follow-up analysis. j Histochem Cytochem. 2013;61(5):330–339.
15. Bartha Á, Győrffy B. TNMplot.com: a web tool for the comparison of gene expression in normal, tumor and metastatic tissues. Int J Mol Sci. 2021;22:5.
16. Park S-J, Yoon B-H, Kim S-K, Kim S-Y. GENT2: an updated gene expression database for normal and tumor tissues. BMC Med Genomics. 2019;12(5):101.
17. Li T, Fan J, Wang B, et al. TIMER: a web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Res. 2017;77(21):e108–e110.
18. Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45(W1):W98–w102.
19. Thul PJ, Lindskog C. The human protein atlas: a spatial map of the human proteome. Protein Sci. 2018;27(1):233–244.
20. Koch A, De Meyer T, Jeschke J, Van Criekinge W. MEXPRESS: visualizing expression, DNA methylation and clinical TCGA data. BMC Genomics. 2015;16(1):636.
21. Cerami E, Gao J, Dogrusoz U, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–404.
22. von Mering C, Huynen M, Jaeggi D, Schmidt S, Bork P, Snel B. STRING: a database of predicted functional associations between proteins. Nucleic Acids Res. 2003;31(1):258–261.
23. Shannon P, Markiel A, Ozier O, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–2504.
24. Huang DW, Sherman BT, Tan Q, et al. The DAVID Gene Functional Classification Tool: a novel biological module-centric algorithm to functionally analyze large gene lists. Genome Biol. 2007;8(9):R183–R183.
25. Li T, Fu J, Zeng Z, et al. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 2020;48(W1):W509–W514.
26. Kuleshov MV, Jones MR, Rouillard AD, et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44(W1):W90–W97.
27. Á N, Győrffy B. muTarget: a platform linking gene expression changes and mutation status in solid tumors. Int j Cancer. 2021;148(2):502–511.
28. Mattingly CJ, Colby GT, Forrest JN, Boyer JL. The Comparative Toxicogenomics Database (CTD). Environ Health Perspect. 2003;111(6):793–795.
29. Luczak MW, Jagodziński PP. The role of DNA methylation in cancer development. Folia Histochemica Et Cytobiologica. 2006;44(3):143–154.
30. Ziai J, Gilbert HN, Foreman O, et al. CD8+ T cell infiltration in breast and colon cancer: a histologic and statistical analysis. PLoS One. 2018;13(1):e0190158.
31. Berger AC, Korkut A, Kanchi RS, et al. A comprehensive pan-cancer molecular study of gynecologic and breast cancers. Cancer Cell. 2018;33(4):690–705.e699.
32. Song J, Ye A, Jiang E, et al. Reconstruction and analysis of the aberrant lncRNA‐miRNA‐mRNA network based on competitive endogenous RNA in CESC. J Cell Biochem. 2018;119(8):6665–6673.
33. Zhou W, Wu J, Liu X, et al. Identification of crucial genes correlated with esophageal cancer by integrated high-throughput data analysis. Medicine. 2020;99:20.
34. Jiang P, He S, Li Y, Xu Z. Identification of therapeutic and prognostic biomarkers of Lamin C (LAMC) family members in head and neck squamous cell carcinoma. Med Sci Monitor. 2020;26:e925735–e925735.
35. Huang M, Zhang T, Yao Z-Y, et al. MicroRNA related prognosis biomarkers from high throughput sequencing data of kidney renal clear cell carcinoma. BMC Med Genomics. 2021;14(1):72.
36. Waheed S, Zeng L. The critical role of miRNAs in regulation of flowering time and flower development. Genes (Basel). 2020;11(3):319.
37. Martinez NJ, Walhout AJM. The interplay between transcription factors and microRNAs in genome-scale regulatory networks. Bioessays. 2009;31(4):435–445.
38. Riazi Rad F, Ajdary S, Omranipour R, Alimohammadian MH, Hassan ZM. Comparative analysis of CD4+ and CD8+ T cells in tumor tissues, lymph nodes and the peripheral blood from patients with breast cancer. Iran Biomed J. 2015;19(1):35–44.
39. Győrffy B, Hatzis C, Sanft T, Hofstatter E, Aktas B, Pusztai L. Multigene prognostic tests in breast cancer: past, present, future. Breast Cancer Res. 2015;17(1):1–7.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.