Back to Journals » Advances in Medical Education and Practice » Volume 10
Exploring the gaps between education and pharmacy practice on antimicrobial stewardship: a qualitative study among pharmacists in Qatar
Authors Nasr ZG, Higazy A, Wilbur K
Received 15 December 2018
Accepted for publication 6 April 2019
Published 6 May 2019 Volume 2019:10 Pages 287—295
DOI https://doi.org/10.2147/AMEP.S198343
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Ziad G Nasr,1 Alya Higazy,1 Kerry Wilbur2
1College of Pharmacy, Qatar University, Doha, Qatar; 2Faculty of Pharmaceutical Sciences, the University of British Columbia, Vancouver, Canada
Background: Antimicrobial resistance is a public health issue and is the focus of antimicrobial stewardship (AMS) teams within health care institutions. However, AMS is not comprehensively and fully taught in medical or pharmacy curricula and little is known about the relevance of pharmacist training to meet AMS needs in the Middle East region. We aimed to explore the discord that may exist between infectious diseases education and actual clinical practice with regard to AMS knowledge and training skills in Qatar. Then, we sought to further explore pharmacist perceptions of their AMS roles in hospital environments.
Methods: A qualitative study was undertaken at Qatar University using three focus groups consisting of 15 pharmacy alumni who are currently practicing as clinical pharmacists in Qatar. Focus groups were facilitated using a topic guide developed by study investigators. Discussions were audio-recorded and transcribed verbatim. Results were analyzed using framework analysis.
Results: Two major themes related to the first objective emerged throughout the discussions and associated recommendations made to improve (i) infectious diseases (ID) module content and delivery and (ii) ID knowledge and skills application. Two themes related to the second objective included (i) impact of pharmacist’s interventions on decision-making and (ii) continuing professional development programming.
Conclusion: Our findings guide ongoing efforts to enhance ID content in the curriculum and will close gaps related to AMS training. Pharmacists are core AMS team members where there is an ongoing need to align continuing education for health professionals with realities of practice.
Keywords: antimicrobial stewardship, education, clinical practice, pharmacist, Middle East, infectious diseases
Corrigendum for this paper has been published
Introduction
Antimicrobial resistance (AMR) is a global public health issue requiring immediate action plans for containment [1]. Multidrug-resistant (MDR) organisms are easily spread, and patient infection with resistant organisms can result in prolonged illness, increased morbidity and mortality.1,2 According to the Centers for Disease Control and Prevention (CDC), at least 2,000,000 illnesses and 23,000 deaths are associated with AMR annually in the USA.3 Among Middle East countries, AMR is becoming more prevalent as the rate of infections with MDR pathogens such as methicillin-resistant Staphylococcus aureus, extended-spectrum beta-lactamase Klebsiella pneumonia, carbapenem-resistant Enterobacteriaceae (CRE) is on the rise.4–7 One of the strategies adopted by health care institutions to minimize AMR is the implementation of antimicrobial stewardship programs (ASPs).8 ASPs necessitate the incorporation of coordinated interventions designed to measure and improve appropriate antimicrobial use by promoting the selection of optimal antimicrobial regimens.8 Unfortunately, ASPs are limited in scope in the Middle East as many health care institutions still lack firm guidelines for proper antimicrobial utilization, essential instruments for local ASPs success.9 In fact, the Antibiotic Resistance Surveillance and Control in the Mediterranean Region project conducted in 2006 in the Middle East identified that only 33.3% of hospitals surveyed had antibiotic prescribing guidelines, and 53.3% of hospitals fed back resistance rates to prescribers.9
The CDC considers pharmacists to be core members of any ASP team as they provide drug expertise essential to improve antibiotic use.10 Pharmacists themselves agree. In a qualitative study of hospital pharmacists and antibiotic governance, participants perceived themselves as antibiotic “gatekeepers” and considered promoting rational use of antimicrobials to be an important part of their jobs.11 Studies from the Middle East region also support the importance of the clinical pharmacist’s role in ASPs.12 However, in order for pharmacists to adequately fulfill necessary roles on ASP teams and become antimicrobial stewards, pharmacy schools must adequately prepare student pharmacists during undergraduate and postgraduate studies prior to entry into actual practice.13,14 In fact, the World Health Organization stresses upon this fact so that current and future healthcare professionals receive appropriate education on proper antimicrobial use, infection control and containment of AMR.15 Unfortunately, antimicrobial stewardship (AMS) is not being comprehensively and fully taught in pharmacy school curricula.16 When surveyed, pharmacy students in South Africa and the USA had mixed opinions regarding their preparedness for the selection and use of antibiotics and most agreed more education and training on antimicrobials and AMS was needed.17,18 Also, future healthcare professionals responsible for using antimicrobials also received disparate AMS education in the UK.19 In Qatar, ASPs have been mandated in governmental hospitals early 2017 as part of medication management use policy and as a standard for the joint commission.20 A national AMS policy was put in place to be utilized by all hospitals under Hamad Medical Corporation.20 However, little is known about the relevance of pharmacist training to meet AMS needs in the Middle East region, although previously in Qatar, community pharmacists have expressed education as a barrier to their abilities to optimize antibiotic use.21
In 2007, the first domestic training program for pharmacists was launched at the national university, Qatar University (QU). The QU College of Pharmacy (CPH) offers Canadian-accredited baccalaureate (Bachelor of Science in Pharmacy, BScPharm) and graduate (Doctor of Pharmacy, PharmD) professional pharmacy degrees. The curriculum includes an infectious diseases (ID) module taught in the third professional year covering most important ID illnesses with a very minor introduction to AMS concept, all delivered through didactic lectures and integrated case-based learning (ICBL) sessions. The bulk of the content covers infections of the: central nervous system, heart, upper and lower respiratory tract, skin and skin structure, bone and joint, gastrointestinal tract, abdomen and peritoneum, urinary tract and prostate. Other topics include viral, fungal, and parasitic infections, sexually transmitted diseases, tuberculosis, HIV, sepsis and septic shock, febrile neutropenia, surgical prophylaxis and vaccines/toxoids/immunobiologics. The allocated time for individual ID courses is presented in Table 1. In the experiential training component of the program (occurring in the summers following professional years 2 and 3 and in the first term of the fourth (and final) professional year), undergraduates spend a total of 8 weeks in a hospital setting where they may be exposed to antibiotic prescribing practices. Students who continue their studies in the PharmD program will have an opportunity to spend 4 weeks in a specialized ID rotation, subject to site and preceptor availability. In this study, we first aimed to explore the gap that may exist between pharmacy education and actual clinical practice with regard to AMS training in a Middle East setting. Then, we sought to further explore pharmacist perceptions of AMS roles in hospital environments.
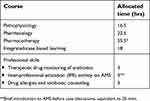 | Table 1 ID courses and allocated time |
Material and methods
Study design
A qualitative study design using focus groups was adopted to explore gaps between education and practice in regard to the perceptions of AMS training in Qatar, and pharmacists’ perceptions of AMS roles in clinical practice. Focus group discussions with a total of 15 pharmacists were conducted.
Study participants
All participants were QU CPH alumni currently practicing as clinical pharmacists in the country. One hundred and nineteen pharmacists have graduated from the BScPharm program with a total of 64 graduates from the PharmD program since 2011. Alumni who have at least 1 year of clinical experience in ID or exposure to antibiotic prescribing and presently care for patients in hospital settings were eligible to participate. No incentive was provided for participation. Our alumni database indicates approximately 25 pharmacists would meet the inclusion criteria. These pharmacists were invited to participate in the study through email. Pharmacists practicing in national specialty institutions (eg cardiology, mental health, ambulatory care) and do not deal with antimicrobials were not invited. Pharmacists were assigned to specific focus groups according to their inpatient workplace in general tertiary care teaching hospitals. Fifteen pharmacists were able to participate in three focus groups (N=4, 5 and 6, respectively).
Data collection
Focus groups were held at QU between February and May 2017. Sessions were attended by two authors (ZN and AH) who have training leading focus group discussions. AH facilitated the discussions while supplementary notes were taken by ZN. Interviews were conducted following an interview guide consisting of structured open and closed-ended questions. Topic guide questions were developed by the investigators (Table 2). Questions explored perceived gaps between education and practice with respect to AMS training, suspected rationale for any gaps in pharmacy education and barriers to knowledge translation into actual practice. We also sought to identify pharmacists’ perceptions of AMS and pharmacist-led interventions and whether any recommendations exist to enhance AMS education in the pharmacy curriculum for later application in clinical practice. The duration of each focus group ranged between 45 and 60 mins and was audio-recorded.
 | Table 2 Focus group topic guide questions |
Data analysis
Data were analyzed using the framework method described by Gale et al22. Data coding and analysis began in parallel with ongoing data collection giving the opportunity to explore certain concepts with participants in further detail in subsequent focus group discussions. AH transcribed the audio-recorded discussions verbatim. Transcripts were then independently coded by the researchers and analyzed using thematic content analysis.23 The research team members then met to review and discuss codes and identify potential themes following the coding of each focus group discussion. Themes were then reviewed for similarity and grouped together when appropriate. Data coding and analysis was supported by NVivo 11™ software (QSR International).
Results
The majority of the participants were female pharmacists (80%), who completed the post-baccalaureate PharmD program (93%). Two major themes relating to gaps between ID education and actual practice with regard to AMS training were identified throughout the discussions and associated recommendations made to improve (1) ID module content and delivery and (2) ID knowledge and skills application. Two major themes emerged with regard to pharmacists’ perceptions of AMS roles in hospital environments: (1) impact of pharmacist’s interventions on decision-making as an antimicrobial steward and (2) continuing professional development (CPD) programming. Quotes identified to be most representative of selected themes are presented below.
Gaps between AMS education and practice
ID module content and delivery
Participants indicated that the ID module taught at QU covers a wide range of disease states some of which are not widely seen in real practice and there was little focus on teaching and application of AMS concepts.
We get taught HIV in details but in practice, we barely deal with HIV patients.
Participant 2, focus group 3
I only recall having antimicrobial stewardship presented as a seminar in a CPD session but I don’t remember taking it in the curriculum.
Participant 2, focus group 3
Disconnect between the curriculum and practice was noted in other courses. Some pharmacists thought that cases incorporated in the ID-themed ICBL sessions are not always representative of real patient scenarios seen in actual practice and are mostly taught by QU faculty members rather than practicing clinical pharmacists with an ID background in Qatar. However, some others disagreed.
Someone involved to the local practice in Qatar is best to deliver ICBL sessions with real life cases because they will be able to judge and identify solutions in a practical way not in a theoretical way. If it was a practicing faculty member, this would be ideal.
Participant 2, focus group 3
Not everyone who works in the field is qualified to teach.
Participant 3, focus group 2
ID knowledge and skills application
Almost all interviewees agreed not having an ID rotation as a core rotation of the postgraduate program as a barrier to practicing AMS. All viewed this as a missed opportunity in the experiential component of their training and contributed to what they feel was a lack of preparation to effectively provide relevant care when they first assumed care roles in inpatient care.
I feel like I’m suffering right now, because I didn’t have any clinical experience in ID from before.
Participant 1, focus group 2
Paradoxically, pharmacists who were assigned to an ID rotation in their experiential training were not always satisfied. For example, some thought having an ID rotation in a specialized hospital (eg oncology) provided limited exposure to diverse ID patient cases.
Pharmacists ranked antimicrobials among the most prescribed medications in hospital settings on a daily basis. Thus, it is very important for students to receive sufficient exposure to ID in all courses including pharmacology (eg side effects and drug–drug interactions), pharmacotherapy and pharmacokinetics related to antimicrobial dosing and monitoring,; while allocating less hours to other courses oriented to research skill development. However, some pharmacists do believe that research is important in an in-patient component.
I believe research can have a big impact on practice, so students should know how to conduct research specific to AMS and ID in general early on in their curriculum. We dig deep in international guidelines and primary literature to support our recommendations to consultants and I consider this a big strength for us.
Participant 1, focus group 3
Pharmacists’ perceptions of AMS roles in hospital environments
Pharmacists impact as an antimicrobial steward
Participants discussed several facilitators and barriers to their works as clinical pharmacists as members of the general ID team and some of them as members of the AMS team in particular. Facilitators included acknowledging the role of the clinical pharmacist by the multidisciplinary team and having good communication with other teams regarding decision making in individual patient care.
I really think that pharmacists are well oriented about antibiotics and their dosing and monitoring and all that. There was a huge improvement over the past years. And now, there is a kind of trust between pharmacists and consultants. If we recommend anything that is clinically relevant, the team will immediately accept it.
Participant 3, focus group 2
Other facilitators included establishing good relations and links with several departments within the institution and the adoption of policies and guidelines regarding institution-specific ASP.
We have good relation with the microbiology department where they are updating us with any new culture results even before reporting it on the system, and this indeed facilitates taking an appropriate action and proactive decisions.
Participant 3, focus group 3
Barriers identified were mainly related to interprofessional challenges. These included resistance and hesitance from other teams to make changes recommended by the stewardship team.
They appreciate our role but there is resistance; like they don’t accept easily to de-escalate therapy especially to oral antibiotics even when the patient is clinically stable. But again, because most of our consultants are experts and they have big experience, we have to respect this also. With proper communication and discussion, I guess we are trying to overcome the resistance.
Participant 1, focus group 1
Continuing professional development programming
Almost all participants see continuing professional education as a core element for all health care professionals to stay up to date and enhance patient outcomes. Alumni thought that this can be executed through awareness campaigns, attending CPD sessions, workshops, seminars and conferences related to AMS. In addition, they all thought that as pharmacists, they should be able to provide evidence-based education about antimicrobials to other health care members in order to optimize prescribing practices.
Just like smoking cessation, we can do public awareness campaigns because AMR is a public issue and we should educate the community as well about it.
Participant 2, focus group 3
Discussion
This is the first study to evaluate pharmacists’ perceptions of the relationship between AMS education and clinical practice in a Middle East setting. Participants identified several gaps between their actual training and the ID-related functions they are now expected to fulfill in patient care. While pharmacists offered specific recommendations to augment AMS elements in an ID curriculum, they also acknowledged several facilitators and barriers to practice their roles as core members of the ASP and further improve AMS practices within hospitals. Our findings are consistent with shortcomings in AMS curricular content identified in pharmacy education in other regions where American students desired more education on AMS in preparation to contribute to best practices.18
Given the alarming increase in AMR, the need to address AMS and educate future pharmacists becomes compulsory. Pharmacists participating in this study recommended changes to the curriculum to improve student retention of ID-oriented information, including focusing on topics and case-based discussions using actual patient scenarios from real practices, and an increased emphasis on AMR and AMS concepts within the curriculum. These participants emphasized the need to teach disease states that are common and widely seen in Qatar and believed opportunities to exercise propositional knowledge in authentic contexts could be optimized. Indeed, several studies highlight the importance of problem- or case-based learning and assessment to simulate clinical performance (eg OSCEs).24 MacDougall et al have previously developed and implemented an AMS curriculum in undergraduate pharmacy and medical education that models an authentic work experience and provides students with a realistic simulation of AMS practices. As a result, the knowledge and attitudes of students regarding antimicrobial use, resistance and practices improved after participating in the curriculum.16 In fact, educational institutions worldwide conduct research work to assess the student’s baseline knowledge, attitude and perception of AMS during the last years of education before transitioning into clinical practice.17,18,25–27
Several organizations acknowledge that an interprofessional approach to stewardship is essential for the success of an ASP.28 AMS indeed is a multidisciplinary responsibility and students should be exposed to stewardship through interprofessional activities so that they become more aware of the importance of proper antimicrobial use as future clinical pharmacists. QU just recently initiated AMS-related interprofessional activities for medicine and pharmacy students (Table 1) and is planning to allocate more time for such activities. Also, the Doctor of Pharmacy program is working on having all students get involved in ASPs in case they were not offered a full ID rotation. This could be achieved by encouraging general internal medicine preceptors to expand student assignment to ID-related cases and by encouraging recruiting of clinical supervisors from ID care settings (eg Communicable Diseases Center) to introduce students to AMS concepts and application. Moreover, in 2015, the country’s major care center introduced an American-accredited post-graduate year one (PGY1) pharmacy residency program and is currently pursuing the implementation of a subsequent postgraduate year two (PGY2). Such residencies (as well as fellowships) will further train graduates to serve on ASPs and contribute to AMS-related research. Expansion of such programs is necessary to prepare health care professionals to sustain and further develop ASPs in Qatar.
Pharmacists are essential stewards when it comes to AMS practices, and their role as members of the AMS team is internationally recognized.10,27 Most ASPs have pharmacists in leading roles to care for and manage patient care responsibilities of AMS.28,29 In a multicenter study conducted across South Africa, timeliness of antibiotics due to pharmacists’ interventions improved by 37%.30 This can be accompanied by a behavioral culture change with physician’s antimicrobial prescribing to optimize evidence-based practices.31,32 Based on our results, communication among multidisciplinary teams with regard to AMS practices can serve both as a facilitator and a barrier for improving patient outcomes. Proper communication among multidisciplinary teams for impactful ASP interventions is always necessary.33 On the university level, QU has initiated American-accredited AMS and infection control program workshops for health care professionals in the country as part of the CPD-health practitioners program. Added to that, national governmental health care institutions are moving toward disseminating local ASP policies, and AMS experts constantly stress on the importance of culture and team dynamic in AMS.34
Participants had a consensus that continuing education plays a big role in overcoming several barriers related to the preparedness of trainees during their education and while performing AMS tasks in actual practice. In fact, education is crucial to develop interpersonal skills including competency, critical thinking and problem-solving skills for proper decision making during pharmacotherapy.35 In that way, future pharmacists will be able to achieve the best outcomes by their patient-centered interventions.36,37 Moreover, engagement in collaborative research with other health care members and stakeholders from other institutions related to educational and clinical practices is mandated in order to enhance the quality of life and improve outcomes of patients in the global community.38,39
Strengths of this study include a good representation of graduates from the sole college of pharmacy. The views expressed in the study show a clear desire of QU alumni pharmacists in Qatar to improve pharmaceutical education and enhance the preparedness of future pharmacists going into clinical practice. Also, findings from this study represented data from practicing QU alumni that will serve as a good reference to assess the current role of pharmacists’ as members of the AMS team and to understand the impact of their interventions on optimizing practices. Additionally, the focus group method permitted rich exchange among participants and opportunity to widely explore perspectives which may not have been identified in a questionnaire. The findings represent only perceptions of QU alumni and results cannot be presumed to represent the perceptions of all hospital pharmacists in Qatar. For example, the focus group participants practiced in three tertiary care teaching hospitals and we do not have perspectives of pharmacists working in any of the other smaller community or private hospitals. While checks for data saturation were not formally assessed, we feel the viewpoints are likely fully represented given approximately 60% of the eligible target population participated.39 Finally, while the lead researcher and focus group facilitator is a QU CPH faculty member, this did not appear to be a censoring factor for candid feedback given the nature of constructive comments shared in the discussions.
QU is currently moving forward in putting more emphasis on AMS education and dedicating more hours in the pharmacotherapy course by focusing more on teaching basic AMS concepts, interventions and measures’ assessment. Also, more emphasis will be given to AMS topic while delivering some CPD and IPE sessions. Moreover, the PharmD program is currently moving forward in making the ID rotation as a core rotation for each student enrolled in the program to get benefit from ID stewardship practices in training prior to establishing an actual clinical pharmacy practice. Future studies will be needed to evaluate the AMS education and preparedness of future QU alumni who wish to practice as ID stewards in health care institutions within Qatar.
Conclusions
The pharmacy program in Qatar provides students with the basic knowledge and skills related to ID. However, gaps exist between AMS education and actual needs for clinical practice. Perceived deficiencies in ID course content, challenges to information retention and lack of relevant experiential training opportunities were identified by alumni who also reiterated pharmacists’ importance of their role as AMS team members. Participants also identified the need to align continuing education for health professionals with realities of practice. The findings of this study guide ongoing efforts to enhance ID content in this curriculum and will close the gaps related to AMS training.
Abbreviation list
AMR, Antimicrobial Resistance; AMS, Antimicrobial Stewardship; ASP, Antimicrobial Stewardship Program; BScPharm, Bachelor of Science in Pharmacy; CDC, Centers for Disease Control and Prevention; CPD, Continuing Professional Development; CPH, College of Pharmacy; CRE, Carbapenem-Resistant Enterobactriaceae; ESBL, Extended Spectrum Beta Lactamase; HIV, Human Immunodeficiency Virus; ICBL, Integrated Case-Based Learning; ID, Infectious Diseases; MDR, Multi-Drug Resistant; MRSA, Methicillin-Resistant Staphylococcus Aureus; OSCE, Objective Structured Clinical Examination; PharmD, Doctor of Pharmacy; PGY1, Post Graduate Year One; PGY2, Post Graduate Year Two; QU, Qatar University; UK, United Kingdom; USA, United States of America; WHO, World Health Organization.
Ethics approval and informed consent
This study was reviewed and received research ethics approval by the Qatar University Institutional Review Board (QU-IRB 64-E/16), with an exemption from a full ethics review. Written informed consent was obtained from all participants.
Consent for publication
Verbal consent was obtained from all participants to publish.
Data sharing statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
This study was completed with funding from an Internal Student Grant from Qatar University.
The abstract of this paper was presented at the 2018 ACCP Global Conference on Clinical Pharmacy as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Journal of the American College of Clinical Pharmacy; DOI: 10.1002/JAC5.1059.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1.
2.
3.
4. ElMahdy TS, ElAhmady M, Goering RV. Molecular characterization of methicillin-resistant Staphylococcus aureus isolated over a 2-year period in a Qatari hospital from multinational patients. Clin Microbiol Infect. 2014;20(2):169–173. doi:10.1111/1469-0691.12240
5. Tokajian S. New epidemiology of Staphylococcus aureus infections in the Middle East. Clin Microbiol Infect. 2014;20(7):624–628. doi:10.1111/1469-0691.12691
6. Vali L, Dashti AA, Jadaon MM, ElShazly S. The emergence of plasmid mediated quinolone resistant qnrA2 in extended spectrum B-lactamase producing Klebsiella pneumoniae in the Middle East. Daru. 2015;23(1):34. doi:10.1186/s40199-015-0116-7
7. Zowawi HM, Sartor AL, Balkhy HH, et al. Molecular characterization of carbapenemase-producing Escherichia coli and Klebsiella pneumonia in the countries of the Gulf cooperation council: dominance of OX-48 and NDM producers. Antimicrob Agents Chemother. 2014;58(6):3085–3090. doi:10.1128/AAC.02050-13
8. Fishman N. Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, Pediatric Infectious Diseases Society. Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol. 2012;33:3223–3227.
9. Borg MA, Cookson BD, Gur D, et al. Infection control and antibiotic stewardship practices reported by south-eastern Mediterranean hospitals collaborating in the ARMed project. J Hosp Infect. 2008;70(3):228–234. doi:10.1016/j.jhin.2008.07.002
10.
11. Broom A, Plage S, Broom J, Kirby E, Adams J. A qualitative study of hospital pharmacists and antibiotic governance: negotiating interprofessional responsibilities, expertise and resource constraints. BMC Heath Serv Res. 2016;16:43. doi:10.1186/s12913-016-1290-0
12. Nasr Z, Paravattil B, Wilby KJ. The impact of antimicrobial stewardship strategies on antibiotic appropriateness and prescribing behaviours in selected countries in the Middle East: a systematic review. East Mediterr Health J. 2017;23(6):430–440.
13. Ernst EJ, Klepser ME, Bosso JA, et al. Recommendations for training and certification for pharmacists practicing, mentoring, and educating in infectious diseases pharmacotherapy. Pharmacotherapy. 2009;29:482–488. doi:10.1592/phco.29.1.82
14. Chahine EB, ElLababidi RM, Sourial M. Engaging pharmacy students, residents, and fellows in antimicrobial stewardship. J Pharm Pract. 2015;28(6):585–591. doi:10.1177/0897190013516506
15.
16. MacDougall C, Schwartz BS, Kim L, Nanamori M, Shekarchian S, Chin-Hong PV. An interprofessional curriculum on antimicrobial stewardship improves knowledge and attitudes toward appropriate antimicrobial use and collaboration. Open Forum Infect Dis. 2017;4(1):ofw225.
17. Burger M, Fourie J, Loots D, et al. Knowledge and perceptions of antimicrobial stewardship concepts among final year pharmacy students in pharmacy schools across South Africa. South Afr J Infect Dis. 2016;31(3):84–90.
18. Justo JA, Gauthier TP, Scheetz MH, et al. Knowledge and attitudes of doctor of pharmacy students regarding the appropriate use of antimicrobials. Clin Infect Dis. 2014;59(Suppl 3):162–169. doi:10.1093/cid/ciu537
19. Castro-Sanchez E, Drumright LM, Gharbi M, Farrell S, Holmes AH. Mapping antimicrobial stewardship in undergraduate medical, dental, pharmacy, nursing and veterinary education in the United Kingdom. PLoS One. 2016;11(2):e0150056. doi:10.1371/journal.pone.0150056
20. Frederico F, Al-Ajmi J Antimicrobial stewardship; bridging the gap between quality care and patient safety. 2016. Available from:
21. Black E, Catwright A, Bakharaiba S, El-Mekaty E, Alsahan D. A qualitative study of pharmacists’ perceptions of, and recommendations for improvement of antibiotic use in Qatar. Int J Clin Pharm. 2014;36:787–794. doi:10.1007/s11096-014-9960-7
22. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using framework method for the analysis of qualitative data in multidisciplinary health research. BMC Med Res Methodol. 2013;13:117. doi:10.1186/1471-2288-13-117
23. Patton MQ. Qualitative Research and Evaluation Methods.
24. Toklu HZ. Problem based pharmacotherapy teaching for pharmacy students and pharmacists. Curr Drug Deliv. 2013;10(1):67–70.
25. Ahmad A, Khan MU, Moorthy J, Jamshed SQ, Patel I. Comparison of knowledge and attitudes about antibiotics and resistance, and antibiotics self-practicing between bachelor of pharmacy and doctor of pharmacy students in southern India. Pharm Pract (Granada). 2015;13(1):523. doi:10.18549/PharmPract.2015.01.523
26. Ahmad A, Khan MU, Patel I, Maharaj S, Pandey S, Dhingra S. Knowledge, attitude and practice of B.Sc. pharmacy students about antibiotics in Trinidad and Tobago. J Res Pharm Pract. 2015;4(1):37–41. doi:10.4103/2279-042X.150057
27. Gilchrist M, Wade P, Ashiru-Oredopre D, et al. Antimicrobial stewardship from policy to practice: experiences from UK antimicrobial pharmacists. Infect Dis Ther. 2015;4(Suppl 1):51–64. doi:10.1007/s40121-015-0080-z
28. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antimicrobial stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–77. doi:10.1093/cid/ciw118
29.
30. Messina AP, van Den Bergh D, Goff DA. Antimicrobial stewardship with pharmacist intervention improves timeliness of antimicrobials across thirty-three hospitals in South Africa. Infec Dis Ther. 2015;4(Suppl 1):5–14. doi:10.1007/s40121-015-0082-x
31. Charani E, Edwards R, Sevdalis N, et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53(7):651–662. doi:10.1093/cid/cir445
32. Gabbay J, le May A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ. 2004;328(743):1013. doi:10.1136/bmj.328.7445.934
33. Foral PA, Anothone JM, Destache CJ, et al. Education and communication in an interprofessional antimicrobial stewardship program. J Am Osteopath Assoc. 2016;116(9):588–593. doi:10.7556/jaoa.2016.116
34. Toklu HZ. Pharmaceutical education vs. pharmacy practice: do we really teach what they need for practicing? Pharma Care Health Sys. 2015;2:e134.
35. Mestrovic A, Rouse MJ. Pillars and foundations of quality for continuing education in pharmacy. Am J Pharm Educ. 2015;79(3):45. doi:10.5688/ajpe79799
36. Toklu HZ, Hussain A. The changing face of pharmacy practice and the need for a new model of pharmacy education. J Young Pharm. 2013;5(2):38–40. doi:10.1016/j.jyp.2012.09.001
37. Giberson S, Yoder S, Lee MP Improving patient and health system outcomes through advanced pharmacy practice. A report to the U.S. Surgeon General Office of the Chief Pharmacist. U.S. Public Health Service; 2011. Available from:
38. Awaisu A, Kheir N, AlSalimy N, Babar ZUD. Pharmacists’ attitudes towards practice research: A review. In: Babar ZUD, editor. Pharmacy Practice Research Methods. Switzerland: Springer International Publishing; 2015:237–247.
39. Mason M. Sample Size and Saturation in PhD Studies Using Qualitative Interviews. Forum: Qualitative Social Research. 2010;11(3):Art 8.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
