Back to Journals » Risk Management and Healthcare Policy » Volume 17
Exploring the Experiences and Support of Nurses as Second Victims After Patient Safety Events in China: A Mixed-Method Approach
Authors Tang W , Xie Y, Yan Q, Teng Y, Yu L, Wei L, Li J, Chen Y, Huang X, Yang S, Jia K
Received 25 November 2023
Accepted for publication 29 February 2024
Published 12 March 2024 Volume 2024:17 Pages 573—586
DOI https://doi.org/10.2147/RMHP.S451766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Haiyan Qu
Wenzhen Tang,1 Yuanxi Xie,1 Qingfeng Yan,2 Yanjuan Teng,1 Li Yu,1 Liuying Wei,3 Jinmei Li,4 Yuhui Chen,1 Xiaolin Huang,1 Shaoli Yang,1 Kui Jia1
1The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi Zhuang Autonomous Region, 530021, People’s Republic of China; 2The Sanming Second Hospital, Sanming, Fujian Province, 366099, People’s Republic of China; 3Nanning Fourth People’s Hospital, Nanning, Guangxi Zhuang Autonomous Region, 530021, People’s Republic of China; 4Wanxiu District Chengnan Community Health Service Center, Wuzhou, Guangxi Zhuang Autonomous Region, 543000, People’s Republic of China
Correspondence: Kui Jia, The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi Zhuang Autonomous Region, 530021, People’s Republic of China, Email [email protected]
Aim: To investigate the current status of experience and support of nurses as second victims and explore its related factors in nurses.
Design: A sequential, explanatory, mixed-method study was applied.
Methods: A total of 406 nurses from seven tertiary hospitals in China were chosen as participants between September to October 2023. The Chinese version of the Second Victim Experience and Support Questionnaire (SVEST), Somatic Complaints of Sub-health Status Questionnaire (SCSSQ) and Generalized Anxiety Disorder (GAD-7) were applied to collect quantitative data. Eight nurses were selected for a qualitative study through in-depth interviews. Through interpretive phenomenological analysis, the interview data were analysed to explore the experience and support of nurses as second victims.
Results: Practice distress (15.74 ± 4.97) and psychological distress (15.48 ± 3.74) were the highest dimensions, indicating Chinese nurses experienced second victim-related practice and psychological distress. Nurses with different gender, age, education, marital status, income, working hours, professional titles, and unit types have different levels of second victim-related experience and support (p < 0.05). In addition, the score of SVEST was positively associated with SCSSQ (r = 0.444) and GAD-7 (r = 0.490) (p < 0.05). This qualitative study found that the experience and support of nurses as second victims included nurses’ perceptions and needs for patient safety events; psychological, physical and practice distress of nurses; and nurses and hospitals coping style after patient safety events.
Discussion: Our findings suggest that nurses who are second victims of patient safety events experience severe practice and psychological distress, indicating that nursing managers should pay attention to psychological and practice distress of nurses after patient safety events and provide effective preventive measures.
Keywords: Nurses, second victims, patient safety events, mixed method
Patient safety events are defined by The World Alliance For Patient Safety Drafting Group as events or circumstances that may or have caused unnecessary personal harm to patients, including reportable conditions, near-misses, no-harm events or harmful events (adverse events).1 A recent survey found that 45.26% of nurses had experienced at least one patient safety incident that significantly negatively impacted their mental health in China.2 In addition, A recent study revealed that 76.88% of Chinese nurses encountered patient safety incidents.3 In patient safety incidents, patients and their families are the first victims, while nurses are affected by the incident itself, the way it is handled, medical errors and/or patient-related injuries. They thus become the second victims, which may produce a series of health problems such as anxiety, sleep disorders and job burnout.4,5 A systematic review of health care workers in intensive care units as second victims showed that the most common symptom was guilt and that approximately 20% of workers did not recover from second-victim symptoms for more than a year or did not even recover at all.6 In addition, second victims can experience significant professional distress, which prompts them to contemplate switching careers.7
A recent study conducted in China found that nurses who had encountered patient safety events expressed a strong desire for support and guidance in their future work.3 The findings of Wen et al indicated that nurses who were second victims expressed a greater desire for peer support,8 while Nijs et al discovered that found that organizational support was most desired by nurses.9 Providing appropriate support and help to the second victim can effectively relieve their emotional stress, but if their unit and colleagues have a negative attitude towards such incidents, then it may aggravate the emotional distress of the second victim.4 However, at present, the support provided by medical institutions and peers to nurses as second victims is inadequate.10
Clarifying the status of nurses’ experiences and support as secondary victims after patient safety incidents, as well as the relationship between safety incidents and physical and mental symptoms, is necessary to improve the health of nurses. Current studies have used quantitative methods to examine the experiences and support of nurses as second victims or qualitative methods.11,12 However, fully understanding the current state of second-victim experience and support with a single quantitative or qualitative study is difficult. Quantitative research can only obtain the second victim’s experience and support scores, and it cannot understand and review personal experiences in depth. Qualitative research can compensate for this shortcoming.
Therefore, to better understand the experience and support of nurses as second victims, this study used a sequential explanatory mixed-methods, integrating qualitative and quantitative research methods.
The specific objectives of this study were to (a) investigate the status quo of nurses’ experiences and support as second victims; (b) explore the factors that influence the scores of nurses’ experiences and support as second victims; (c) assess the correlation between the nurses’ experiences and support of second victims and physical and psychological symptoms.
Through this work, we aim to inform the development of targeted second-victim experiences and support interventions to improve the physical and mental health of nurses.
Methods
This study employed a sequential mixed methods explanatory design, which involved a quantitative phase followed by the qualitative phase.
Part 1: Quantitative Component of the Study
Design and Participants
A cross-sectional survey was performed. From September to October 2023, nurses from seven tertiary hospitals located in different geographical areas of China (Eastern China, Central China and Western China) were selected as participants through convenient sampling for online questionnaire surveys. All of the hospitals were well-known in the area, and they were large tertiary general hospitals with over 800 beds. The inclusion criteria were as follows: (1) the nurses have worked for at least 1 year; (2) the nurses experienced patient safety events; and (3) informed consent and voluntary participation were ensured. The exclusion criteria were as follows: (1) the nurses were interns, postgraduates, on rotation or on leave.
The sample size is calculated according to the formula for estimating the sample size of a cross-sectional survey:  .13 Uα/2 is 1.96, σ represents the expected standard deviation of the second victim is 0.9 and δ represents the allowable error is 0.1, n= (1.96*0.9/0.1) =311. In addition, with the 10% shedding rate taken into account, the sample size was 342 cases. A total of 406 online questionnaires were collected, with an effective response rate of 100%.
.13 Uα/2 is 1.96, σ represents the expected standard deviation of the second victim is 0.9 and δ represents the allowable error is 0.1, n= (1.96*0.9/0.1) =311. In addition, with the 10% shedding rate taken into account, the sample size was 342 cases. A total of 406 online questionnaires were collected, with an effective response rate of 100%.
Data Collection Tools
The basic data questionnaire included gender, age, marital status, education level, monthly income, unit types, working years, job titles and hours worked per week.
The version of the Second Victim Experience and Support Questionnaire (SVEST) was developed by Burlison in 201714 and was translated by Chen in 2020.15 It contains 24 items, which can be divided into six dimensions: psychological, physiological, and practice distress, colleague, management, and non-work support. A high score corresponds to greater distress caused by the patient security events to the second victim, and less support received. The Cronbach’s α in this study was 0.822.
The Somatic Complaints of Subhealth Status Questionnaire (SCSSQ) was developed by Han Biao et al in 2007.16 The scale contains 16 items and is suitable for self-assessment of sub-health somatic symptoms. A high total score on the scale corresponds to more serious sub-healthy physical symptoms of the subjects. In this study, the Cronbach’s α coefficient was 0.954.
Generalized Anxiety Disorder-7 (GAD-7) is a seven-item self-rating scale to assess the severity of anxiety.17 The higher scores indicating higher levels of anxiety. The Chinese version of GAD-7 was translated and revised by He.18 The Cronbach’s α coefficient was 0.957 in this study.
Statistical Analysis
SPSS 26.0 was used for statistical analysis. In descriptive analysis, the measurement data conforming to normal distribution were represented by  , while the skew distribution data were represented by P50 (P25-P75). Counting data were described by frequency and component ratio. T-test, and one-way ANOVA were used to compare the SVEST scores of nurses with different social-demographic information. If the variable is skewed, then non-parametric test analysis is used. The relationship between SVEST and SCSSQ and GAD-7 was examined by Pearson correlation analysis. Multiple linear regression was used to assess the predictor of SVEST. P < 0.05 was considered statistically significant.
, while the skew distribution data were represented by P50 (P25-P75). Counting data were described by frequency and component ratio. T-test, and one-way ANOVA were used to compare the SVEST scores of nurses with different social-demographic information. If the variable is skewed, then non-parametric test analysis is used. The relationship between SVEST and SCSSQ and GAD-7 was examined by Pearson correlation analysis. Multiple linear regression was used to assess the predictor of SVEST. P < 0.05 was considered statistically significant.
Part 2: Qualitative Component of the Study
Design and Participants
The qualitative phase was carried out after the quantitative study was completed. The interviewees in this stage were selected from 406 participants in the quantitative phase who agreed to participate in the second phase of the study and had high SVEST scale scores. From the thirty participants who agreed to participate in the qualitative interview and had a high SVEST score, the purpose sampling method was adopted, and the respondents’ age, education, education level and other factors were taken into account. The sample size was determined to achieve the repetition of the research topic, and a total of eight nurses were finally included.
Data Collection Tools
On the basis of the research purpose and literature review, the interview outline was initially drawn up, and the opinions of the (deputy) chief nurse, psychological nursing experts and members of the research group were consulted and revised. Two nurses who had experienced patient safety events were pre-interviewed, and the interview outline was optimised according to the results of the pre-interview. Therefore, the final interview outline is provided in Table S1.
This face-to-face interview took place in a quiet, independent environment. Before the formal interview, the researcher explained the purpose and content of the study to the interviewees. During the interview, the interviewers listened carefully, observed the interviewees’ facial expressions and behaviours, and made timely records. Each conversation lasted 20 to 35 minutes.
Statistical Analysis
After the interview, the researcher sorted out and transcribed the data within 24 hours. The data were translated word for word into text, and a document was created and printed. Colaizzi’s seven-step data analysis method was used for data analysis.19
Results
Descriptive Analysis of General Demographic Data of the Participants
A total of 94.83% of the participants were female, 45.07% were 20–30 years old, 61.58% were married, 85.71% had a college degree and 40.89% were supervisor nurses. A total of 37.44% had a monthly income of 5000–7000 (CNY). The largest number of participants came from the surgery department, with 25.12%, and 29.80% of the participants had work experience of less than five years (Table S2).
SVEST Scores of Participants
The total score of SVEST is (65.61 ± 11.47), and the highest scoring dimension was practice distress (15.74 ± 4.97), followed by psychological distress (15.48 ± 3.74). In terms of items, psychological distress had the highest mean score (3.87 ± 0.94), followed by practice pdistress (3.18 ± 0.99). Management support received the highest support score (2.00 ± 0.79). Table 1 shows the SVEST score of 406 participants.
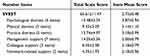 |
Table 1 SVEST Scores of Participants (n=406) |
Comparison of SVEST Scores Among Participants with Different Backgrounds
No difference was found in the total score of SVEST among participants with different demographic information. In the psychological distress data, nurses who were female, older or divorced scored higher (p < 0.05). Nurses with a college degree had higher levels of physical distress (p < 0.05). Participants who were younger, divorced, had been working for less than five years and had professional titles reported higher professional distress (p < 0.05).
Nurses who were male or worked in paediatrics received less management support (p < 0.05). Male, younger, divorced or senior nurses reported less colleague support (p < 0.05). Nurses who were male, had an income less than 5000 CNY or worked in the ICU experienced less non-work-related support (p < 0.05) (Table 2).
 |
Table 2 SVEST Scores of Nurses in Different Backgrounds Were Compared (n=406) |
Predictors of SVEST Score
Linear regression analysis was used to incorporate the significant findings from univariate analysis (Table S3–S8). In terms of psychological distress, the results revealed that only unit types was a significant predictor. In addition, length of working was a predictor of practice distress, and gender was a predictor of nonwork-related support.
Correlation Between SVEST, SCSSQ and GAD-7
Table 3 presents the results of the correlation analysis. The SVEST scores were positively associated with SCSSQ (r = 0.444) and GAD-7 (r = 0.490) (p < 0.05), as well as with fatigue (r = 0.434), pain (r = 0.375), sleep issues (r = 0.406) and gastrointestinal discomfort (r = 0.388) (p < 0.05).
 |
Table 3 The Correlation of SVEST, SCSSQ, and GAD-7 in the Study (N =406) |
Results in Qualitative Phase
On the basis of data saturation, eight nurses who had experienced patient safety events were selected as respondents (Table 4). An analysis of these participants revealed three main themes: nurses’ perceptions and needs for patient safety events; psychological, physical, and practice distress of nurses after patient safety events; and nurses and hospitals coping style after patient safety events. Table 5 shows the opening coding results.
 |
Table 4 Interviewees’ General Information (N = 8) |
 |
Table 5 Open Coding Results |
Theme 1: Nurses’ Perceptions and Needs for Patient Safety Events
Cognition Deficit
In this study, there were still two nurses who lacked knowledge and understanding of patient safety events.
P5: I think the patient safety incident is safety first, to ensure the personal safety of patients and the safety of treatment.
P8: I think the safety incident we can encounter in our ward is nothing more than a sudden fall of patients and trauma, I don’t know whether the wrong infusion is a safety incident ah?
Desire for Support
In this study, 4 nurses expressed the hope that supporting from surroundings.
P3: Our hospital hopes and encourages all of us to report safety events, and hopes that all adverse events will be reported, including hidden dangers. After reporting it, there is actually great pressure on nurses. We hope the hospital can improve the humanistic care system, and consider us more from our nurses’ point of view.
P4: I really hope to get the understanding of patients, department leaders, friends, and colleagues, which is a big psychological demand.
P5: After the security events, we also need psychological counseling. I hope the hospital and the department can provide a platform, which can relieve the tension.
Theme 2: Psychological, Physical and Practice Distress of Nurses After Patient Safety Events
Psychological Distress
After the occurrence of patient safety events, nurses are prone to negative emotions such as anxiety, tension and fear, and fear that patient safety events will happen again, but will fade with time.
P1: “Psychological words will have fear, for example, the last time a patient committed suicide, I am very afraid because work is too busy, and then a little delay, have not had time to inspect, there will be patients may commit suicide, so they are very afraid, in this case, if the patient committed suicide, the family does not pursue it, then if the family has pursued it, That’s not a lot of trouble coming out.
P2: I was anxiety, thinking about this thing all the time, will be afraid that the patient will find this problem and come back to ask me.
P3: Fear, nervousness, cold sweat, recoil, the feeling of jumping.
P4: First of all, I was very nervous and anxious at that time. I was very afraid that after the adverse event was reported, it would cause a series of adverse effects, even on my own career, and I was also very afraid of the impact on his body.
P7: I was afraid of leadership criticism, because before this, similar things had happened in the department, and then the leadership would talk to me, because I was a new nurse at that time, it was quite stressful for me. I’m also afraid that my bonus will be docked.
P8: I will be very anxious and afraid that the family members of the children will complain to the hospital about me.
Physical Distress
In this study, two nurses reported that sleep disturbances occurred after a patient safety incident, but the effects were not lasting.
P4: The day of the security incident did not sleep very well, because until the next day I still had a little diaphragm in my heart, cannot say diaphragm, still a little scared.
P7: Security events also have some impact on sleep, but over time, the impact on my personal sleep will gradually diminish.
P8: In the period after the mistake, I would go to sleep at night thinking about it, turning over and over and not falling asleep.
In addition, two nurses said they had difficulty concentrating after a patient safety incident.
P2: After that, I felt absent-minded in everything I did. My mind wandered a lot.
P8: I didn’t have trouble remembering things before, but for a while after the security incident, it was easy for me to forget, for example, what my plan was for the next day (wry smile).
Practice Distress
In this study, all four nurses reported that they were more cautious and careful in their future work after a patient safety incident.
P3: “When it comes to work, I will be more and more cautious, so I will move more and more slowly. With the growth of working years, my work speed will become slower, afraid of mistakes, repeatedly look, cross-check. Although the speed has slowed down, the rigor of the work has gradually increased because there is always a fear of making mistakes.
P4: After that incident (patient safety incident), I will be more cautious in the work after that. Whenever they help me turn over and someone else touches my patient, I will carefully check the situation of the patient again.
P6: I feel that this incident can more restrict my daily work behavior, and in the future, I should pay more attention to this patient safety incident and avoid the occurrence of safety incidents.
P7: The impact of the security incident on my work will always be there, that is, I will remember it vividly. In the future work, I will deliberately pay attention to the safety incidents that occurred in the past, and there are negligence and problems in my own nursing work at that time. For example, now, if I were to receive a similar patient who was resuscitated after anesthesia, I would evaluate the patient dynamically, whether her sedation score met the preset requirements. Second, I will also carefully check that the restraints are in place after changing positions to prevent this situation from happening again.
Two nurses questioned themselves after a patient safety incident, questioning their suitability for the profession.
P4: I even doubt whether I am suitable for this career, but also doubt my ability, ah, I think why I am not as focused on the work as others, and why I am not as smooth as others, so natural.
P8: I wonder if I am really suitable for this career and why I can make mistakes even in such a routine job. But as time goes on, I will reconcile.
In addition, three nurses were concerned about whether their careers would be affected.
P1: If there is a dispute between a doctor and a patient, it may result in an impact on your career, such as dismissal.
P4: First of all, I was very nervous at that time. I was very afraid that after the adverse event was reported, it would lead to a series of adverse effects, even on my own career.
P5: When such a patient safety incident goes wrong, I am worried that it will be recorded by the department after it happens, and it will also have an impact on my future career.
Theme 3: Nurses, and Hospitals Coping Style After Patient Safety Events
Coping Styles of Nurses
In this study, two nurses said that after a patient safety incident, they would talk to friends in order to get everyone’s understanding and comfort.
P4: I just described the way I would talk to my friends and family after what happened.
P7: After this happened, I will unconsciously talk to my friends, will take the initiative to express their worries and worries, and then relieve their inner anxiety. Also, talk to teachers in some departments who have been there longer.
In addition, three nurses said that after a patient safety incident, they paid more attention to improving their professional knowledge and skills to try to avoid similar things in the future.
P1: We should be familiar with the core system of the hospital, and we must operate in accordance with the core system of nursing, inspection and observation, so as to prevent potential and possible patient safety incidents.
P4: After encountering these problems, I also continuously improved my professional ability by learning, not only from my own initiative, but also from the department leaders and colleagues.
P7: After this patient safety incident, I also looked up information about sedation evaluation online.
Coping Strategy of Department and Hospital
This study shows that hospitals and departments have provided positive ways to deal with patient safety incidents to reduce the occurrence of patient safety incidents as much as possible.
P3: After a safety incident, the intervention of the hospital and the department is to rectify, and what lessons can be learned, for example, if there is a problem with the clinical process, then reformulate the process.
P5: After the patient safety incident, the department will carry out corresponding discussion and rectification, and then find out the cause of the patient safety incident.
P7: The department will organize discussions on such events. For unplanned extubation, the hospital will organize the relevant PDCA team to discuss with the quality control circle and quality improvement team. In addition, the pipe fixation team will conduct relevant training on the fixation method of tracheal intubation.
Discussion
This study highlights the importance of paying attention to nurses as second victims after patient safety events, a mixed-approach design was used to explore the current level of nurse experience and support as second victims. This quantitative research found that the psychological, physical and practice distress of nurses as second victims after patient safety events was higher than in a previous survey of psychiatric nurses in China,20 and the psychological distress was higher than that of Singaporean nurses8 and Spanish midwives and obstetricians.21 Yan et al found that nurses had higher levels of second-victim experience and support than other health professionals did.22 This finding proves that the psychological, physical and practice distress of nurses in China are higher than those of other health care providers, which is consistent with the results of foreign studies.23 Therefore, understanding the level of nurse experience and support as a second victim after patient safety events is important.
Qualitative research also found that nurses, as second victims of patient safety incidents, may experience negative emotions and heavy burden of symptoms, which complements quantitative research results. This study shows that nurses experience a series of psychological feelings such as anxiety, fear and helplessness after safety incidents, which is consistent with the results of Elliott’s study, indicating that patient safety incidents have a great impact on nurses’ psychology.24 Moreover, some nurses reported temporary sleep disturbances after experiencing patient safety events, consistent with recent studies, which noted that the second victim may experience physical symptoms such as sleep disturbances, tiredness and changes in blood pressure.25,26 Ultimately, our quantitative and qualitative studies affirmed that nurses experienced high levels of physical, psychological and professional distress as second victims.
In addition, the quantitative findings revealed that the highest level of management support was received by 406 nurses who had encountered patient safety events, followed by college support, which is similar another study, indicating that effectively alleviating the distress caused by patient safety incidents is to assign a professional team to intervene or consult with colleagues.27 Specifically, the results of our qualitative study also indicated nurses clearly express the need and desire for understanding and support from people in their surroundings, including conducting group discussions, offering short break, and analyzing clinical errors, which is similar with previous studies.3,12,27 In addition, several reviewees hoped that hospitals could set up relevant consulting institutions, hold regular lectures, and give guidance and interventions to the situation of the second victim, to provide emotional support for them. However, a study of Korean nurses who had been involved in a patient safety incident found that they were more eager for strategic support than psychological support.28 Furthermore, consistent with other research,29 the interview findings revealed that family and friends exert significant influence in the aftermath of a patient safety incident, including engaging in conversations with individuals in their immediate vicinity.
Psychological distress was notable, with a score of (3.87 ± 0.94), which is more pronounced than that of physicians (2.9 ± 1.2).30 Meanwhile, correlation analysis proved that the second-victim experience and support were related to anxiety symptoms (r = 0.490). This finding aligns with similar research showing that patient safety events brings out a robust psychological shadow from nurses, who may feel negative psychological emotions afterwards, such as worry, anxiety, embarrassment and regret.31,32 Many reasons are given for the psychological distress of nurses, which may be related to cumbersome work tasks, increased clinical operations and greater contact with patients. Moreover, they are faced with complex social and psychological pressure.33 Our study also found strong physiological reactions such as sleep disturbances and difficulty concentrating. This result may be related to the working environment and intensity experienced by nurses.34,35 In addition, patient safety events can increase nurses’ practice distress, consistent with previous studies.36,37 Sun et al confirmed that patient safety incidents would significantly increase the turnover intention of nurses.36 A cross-sectional study in South Korea showed that 34.3% of nurses contemplated changing duties or jobs after patient safety incidents.38
The 406 Chinese nurses in this study, as the second victim of patient safety incidents, were less likely to receive support than in other studies.8,20 Low support would have a negative impact on the physical and mental health of nurses. In the dimension of support, the mean score of non-work-related support was the highest (2.18 ± 0.96) and the mean score of management support was the lowest (2.00 ± 0.79), indicating that nurses, as the second victim of patient safety events, mainly relied on management support and less non-work-related support, which is inconsistent with previous studies.23,39 This result may be because 45.07% of the nurses in this survey were under 30 years old, and young nurses received less emotional support from colleagues and relatives due to their short working hours, unstable interpersonal relationships and fear of being misunderstood by relatives and friends. Studies have shown that after patient safety incidents, effective emotional support from colleagues, friends and relatives can become a strong backing for the second victim, which is crucial to help them recover from their traumatic experience.40,41 Our findings showed that the management support score (2.00 ± 0.79) was higher than in other studies,20,23 suggesting that most nurses were supported by the hospital system as second victims. A previous study showed that a high sense of organisational support and a good organisational atmosphere can improve nurses’ job satisfaction, which can effectively reduce the negative emotions and pressure brought by patient safety incidents to the second victim.42
Unlike the second victim’s psychological distress scores from different backgrounds, the degree of psychological distress varies according to gender, age and marital status. Our study revealed that female nurses were more likely than male nurses to report psychological distress, which was similar to the results of previous studies.20,43 This finding may be related to the fact that females are more likely than males to experience negative emotions such as weak stress resistance and severe depression. Older nurses scored higher in psychological distress, consistent with a recent study.2,20 Psychological distress peaks in middle age and then improves again with age in what is often referred to as a “midlife crisis” in psychological health, according to a survey of people’s mental health during the COVID-19 pandemic.44 In addition, divorced nurses experienced higher psychological distress, which was consistent with the findings of related studies on nurses in Singapore.8 This condition may be related to the fact that divorce can be accompanied by a change in economic and social roles, which can bring great stress and anxiety.
In addition, nurses with master’s degrees suffer less physical distress, which may be due to the different nature and content of their work. Nurses with advanced degrees are more engaged in management work, while nurses with a bachelor’s degree or below are more engaged in clinical work.20 Age, length of working hours and professional title were negatively correlated with practice distress, which may be related to the low theoretical knowledge reserve of young nurses or the low overall ability to handle situations and resist pressure. However, another study has shown a positive correlation between age and distress levels.20 The relationship between age and practice distress among nurses needs to be further evaluated by more studies in the future.
This study has several limitations. Firstly, the sample size of this study is small. Large-sample and multi-centre investigations in various regions of China need to be conducted in the future. Second, the experiences and support of second victims were examined through cross-sectional surveys, so we cannot determine how the impact of safety incidents on nurses has changed over time. Nevertheless, to our knowledge, this work is the first hybrid study to describe the experience and support of nurses as second victims after a patient safety incident. A cross-sectional survey was used to describe the second victim’s experience and support level and to compare the differences in scores across different demographic data. Qualitative interviews were used to gain insight into the second victim’s experience.
Conclusion
This explanatory sequential mixed-method study demonstrates that nurses, as the second victim of patient safety incidents, suffer the most serious psychological distress and receive the most management support. Nursing managers should pay attention to the negative emotions of nurses in patient safety incidents, take into account the causes influencing the second victim phenomenon, and offer assistance and appropriate preventive measures based on nurses’ needs and expectations to help reduce the distress experienced by the second victim.
Data Sharing Statement
All data are available in the manuscript.
Ethics Approval
This study was reviewed and approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (2023-E654-01). This study adheres to the provisions and ethical principles outlined in the Declaration of Helsinki.
Patient Consent for Publication
All subjects engaged in the study provided informed consent, including anonymized responses.
Acknowledgments
We are special grateful to all researchers who participated in this study during the study period.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sherman H, Castro G, Fletcher M, et al. Towards an international classification for patient safety: the conceptual framework. Int J Qual Health Care. 2009;21(1):2–8. doi:10.1093/intqhc/mzn054
2. Huang R, Sun H, Chen G, Li Y, Wang J. Second-victim experience and support among nurses in mainland China. J Nurs Manage. 2022;30(1):260–267. doi:10.1111/jonm.13490
3. Shuangjiang Z, Huanhuan H, Ling X, Qinghua Z, Mingzhao X. Second victim experience and support desire among nurses working at regional levels in China. J Nurs Manage. 2022;30(3):767–776. doi:10.1111/jonm.13563
4. Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325–330. doi:10.1136/qshc.2009.032870
5. Li X, Che CC, Li Y, Wang L, Chong MC. The mediating role of coping styles in the relationship between second victim experience and professional quality of life among nurses: a cross-sectional study. BMC Nurs. 2023;22(1):312. doi:10.1186/s12912-023-01473-9
6. Naya K, Aikawa G, Ouchi A, et al. Second victim syndrome in intensive care unit healthcare workers: a systematic review and meta-analysis on types, prevalence, risk factors, and recovery time. PLoS One. 2023;18(10):e0292108. doi:10.1371/journal.pone.0292108
7. Seys D, Scott S, Wu A, et al. Supporting involved health care professionals (second victims) following an adverse health event: a literature review. Int J Nurs Stud. 2013;50(5):678–687. doi:10.1016/j.ijnurstu.2012.07.006
8. Mok WQ, Chin GF, Yap SF, Wang W. A cross-sectional survey on nurses’ second victim experience and quality of support resources in Singapore. J Nurs Manage. 2020;28(2):286–293. doi:10.1111/jonm.12920
9. Nijs K, Seys D, Coppens S, Van De Velde M, Vanhaecht K. Second victim support structures in anaesthesia: a cross-sectional survey in Belgian anaesthesiologists. Int J Qual Health Care. 2021;33(2). doi:10.1093/intqhc/mzab058
10. Schrøder K, Assing Hvidt E. Emotional responses and support needs of healthcare professionals after adverse or traumatic experiences in healthcare-evidence from seminars on peer support. Int J Environ Res Public Health. 2023;20(9):5749. doi:10.3390/ijerph20095749
11. Shao Y, Li S, Wei L, et al. Nurses’ second victim experience, job insecurity, and turnover intention: a latent profile analysis. Research in Nursing & Health. 2023;46(3):360–373. doi:10.1002/nur.22313
12. Stone M. Second victim support: nurses’ perspectives of organizational support after an adverse event. J Nurs Admin. 2020;50(10):521–525. doi:10.1097/NNA.0000000000000928
13. Ni P, Chen JL, Liu N. Sample size estimation for quantitative studies in nursing research. Chin J Nurs. 2010;45(4):3.
14. Burlison JD, Scott SD, Browne EK, Thompson SG, Hoffman JM. The second victim experience and support tool: validation of an organizational resource for assessing second victim effects and the quality of support resources. J Patient Safe. 2017;13(2):93–102. doi:10.1097/PTS.0000000000000129
15. Chen JJ, Yang Q, Zhao QH, Zheng SJ, Xiao MC. Experience and support of nurses as the second victims in patient safety incidents. Chin J Nurs. 2020;55(06):894–899.
16. Han B, Sun J, Liu W, et al. Establishment of sub-health state somatic symptom self-rating scale and test of reliability and validity. Chin Mental Health J. 2007;21(6):382–385.
17. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
18. He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Arch Psychiatry. 2010;22(04):200–203.
19. Liu M. Using an example to illustrate Colaizzi’s phenomenological data analysis method. J Nurs Sci. 2019;34(11):90–92.
20. Xu H, Cao X, Jin QX, Wang RS, Zhang YH, Chen ZH. Distress, support and psychological resilience of psychiatric nurses as second victims after violence: a cross-sectional study. J Nurs Manage. 2022;30(6):1777–1787. doi:10.1111/jonm.13711
21. Santana-Domínguez I, González-De La Torre H, Verdú-Soriano J, Berenguer-Pérez M, Suárez-Sánchez JJ, Martín-Martínez A. Feelings of being a second victim among Spanish midwives and obstetricians. Nurs Open. 2022;9(5):2356–2369. doi:10.1002/nop2.1249
22. Yan L, Tan J, Chen H, et al. Experience and support of Chinese healthcare professionals as second victims of patient safety incidents: a cross-sectional study. Perspect Psychiatr Care. 2022;58(2):733–743. doi:10.1111/ppc.12843
23. Mohd Kamaruzaman AZ, Ibrahim MI, Mokhtar AM, Mohd Zain M, Satiman SN, Yaacob NM. The effect of second-victim-related distress and support on work-related outcomes in tertiary care hospitals in kelantan, Malaysia. Int J Environ Res Public Health. 2022;19(11). doi:10.3390/ijerph19116454
24. Elliott R, Fry M. Psychological capital, well-being, and patient safety attitudes of nurses and midwives: a cross-sectional survey. Nursing & Health Sciences. 2021;23(1):237–244. doi:10.1111/nhs.12808
25. Wands B. Second Victim: a Traumatic Experience. AANA J. 2021;89(2):168–174.
26. Ajri-Khameslou M, Abbaszadeh A, Borhani F. Emergency nurses as second victims of error: a qualitative study. Adv Emerg Nurs J. 2017;39(1):68–76. doi:10.1097/TME.0000000000000133
27. Ganahl S, Knaus M, Wiesenhuetter I, Klemm V, Jabinger EM, Strametz R. Second victims in intensive care-emotional stress and traumatization of intensive care nurses in western Austria after adverse events during the treatment of patients. Int J Environ Res Public Health. 2022;19(6):3611. doi:10.3390/ijerph19063611
28. Choi EY, Pyo J, Ock M, Lee H. Profiles of second victim symptoms and desired support strategies among Korean nurses: a latent profile analysis. J Adv Nurs. 2022;78(9):2872–2883. doi:10.1111/jan.15221
29. Gazoni FM, Amato PE, Malik ZM, Durieux ME. The impact of perioperative catastrophes on anesthesiologists: results of a national survey. Anesthesia Analg. 2012;114(3):596–603. doi:10.1213/ANE.0b013e318227524e
30. Torbenson VE, Riggan KA, Weaver AL, et al. Second victim experience among OBGYN trainees: what is their desired form of support? South Med J. 2021;114(4):218–222. doi:10.14423/SMJ.0000000000001237
31. Lee W, Pyo J, Jang SG, Choi JE, Ock M. Experiences and responses of second victims of patient safety incidents in Korea: a qualitative study. BMC Health Serv Res. 2019;19(1):100. doi:10.1186/s12913-019-3936-1
32. Chan ST, Khong PCB, Wang W. Psychological responses, coping and supporting needs of healthcare professionals as second victims. Int Nurs Rev. 2017;64(2):242–262. doi:10.1111/inr.12317
33. Strametz R, Fendel JC, Koch P, et al. Prevalence of second victims, risk factors, and support strategies among German nurses (SeViD-II Survey). Int J Environ Res Public Health. 2021;18(20):10594. doi:10.3390/ijerph182010594
34. Kable A, Kelly B, Adams J. Effects of adverse events in health care on acute care nurses in an Australian context: a qualitative study. Nursing & Health Sciences. 2018;20(2):238–246. doi:10.1111/nhs.12409
35. Seys D, De Decker E, Waelkens H, et al. A comparative study measuring the difference of healthcare workers reactions among those involved in a patent safety incident and healthcare professionals while working during COVID-19. J Patient Safe. 2022;18(7):717–721. doi:10.1097/PTS.0000000000000992
36. Sun L, Lu Q, Gao W, et al. Study on the influence of patient safety culture on the pain and turnover intention of Chinese nurses in adverse nursing events. Nurs Open. 2023;10(10):6866–6874. doi:10.1002/nop2.1936
37. Shomalinasab E, Bagheri Z, Jahangirimehr A, Bahramnezhad F. The nurses’ second victim syndrome and moral distress. Nurs Ethics. 2023;30(6):822–831. doi:10.1177/09697330221142079
38. Choi EY, Pyo J, Lee W, et al. Nurses’ experiences of patient safety incidents in Korea: a cross-sectional study. BMJ Open. 2020;10(10):e037741. doi:10.1136/bmjopen-2020-037741
39. Finney RE, Torbenson VE, Riggan KA, et al. Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey. J Nurs Manage. 2021;29(4):642–652.
40. Bohomol E. Nurses as second victims: a Brazilian perspective. Nursing & Health Sciences. 2019;21(4):538–539. doi:10.1111/nhs.12630
41. Li SS. A qualitative study of nursing managers’ attitudes toward the second victim in adverse nursing events. Chin J Nurs. 2019;54(8):5.
42. Ma M, Peng D, Zeng J, et al. The effect of emergency department nurses’ intelligence level on second victim experience and support. J Nurs Sci. 2022;37(21):65–68.
43. Van Gerven E, Bruyneel L, Panella M, Euwema M, Sermeus W, Vanhaecht K. Psychological impact and recovery after involvement in a patient safety incident: a repeated measures analysis. BMJ Open. 2016;6(8):e011403. doi:10.1136/bmjopen-2016-011403
44. Moreno-Agostino D, Fisher HL, Goodman A, et al. Long-term psychological distress trajectories and the COVID-19 pandemic in three British birth cohorts: a multi-cohort study. PLoS Med. 2023;20(4):e1004145. doi:10.1371/journal.pmed.1004145
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
