Back to Journals » Journal of Multidisciplinary Healthcare » Volume 7
Exploring physical health perceptions, fatigue and stress among health care professionals
Authors Rice V, Glass N, Ogle KR, Parsian N
Received 19 December 2013
Accepted for publication 29 January 2014
Published 1 April 2014 Volume 2014:7 Pages 155—161
DOI https://doi.org/10.2147/JMDH.S59462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Vanessa Rice,1 Nel Glass,2 KR Ogle,2 Nasrin Parsian2
1School of Exercise Science, 2School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Melbourne, VIC, Australia
Abstract: Nurses, midwives, and paramedics are exposed to high degrees of job demand, which impacts health status and job satisfaction. The aim of this study was to explore the experiences and perceptions of health with a group of nurses, midwives and paramedics in Australia. Specifically, this paper reveals the findings related to the dataset on physical health. In this regard, the researchers sought to explore the relationship between physical health and job satisfaction, and the relationship between health status and stress levels. The study adopted a mixed methodology and used two methods for data collection: one-on-one interviews exploring the relationship between physical health and job satisfaction, and a survey questionnaire focusing on self-rated stress management. The individual interviews were conducted for further exploration of the participants' responses to the survey. There were 24 health care participants who were drawn from metropolitan and regional Australia. The findings revealed participants: had a desire to increase their physical activity levels; had different perspectives of physical health from those recommended by government guidelines; and viewed physical health as important to job satisfaction, yet related to stress and fatigue.
Keywords: workforce, job satisfaction, health status
Introduction
As nurses, midwives, and paramedics are exposed to physical health demands and high levels of stress in their occupations, job satisfaction appears problematic. Workplace environments characterized by high job demands, intensity in care delivery, job burnout, and loss of staff due to health issues, have resulted in a continuum of health disruption for practitioners.1,2
The World Health Organization defined health as a state of complete physical, mental, and social well-being and not merely the absence of disease.3 Physical health incorporates physical activity, nutrition, and recovery. Physical activity has been defined as “bodily movement produced by skeletal muscles that require energy” and exercise as a type of planned, structured, and repetitive activity to maintain or improve physical fitness.4 While the recommendation of 150–300 minutes per week of moderate intensity physical activity on most days of the week is required to maintain health, it has been reported that not all health care workers are meeting this minimum requirement.5,6 The prevalence of overweight and obesity has been reported in health care workers.7,8 Fifty percent of a paramedic’s shift is spent sitting, contributing to obesity.7 Further, night-shift health care workers have been reported to have a higher cumulative incidence of metabolic syndrome (9.0%) compared with daytime workers (1.8%).9 Furthermore, being overweight has been related to an increased incidence of musculoskeletal injuries among health care workers.10–13
Other factors contributing to poor physical health are long hours and shift work, resulting in fatigue and exhaustion, impacting upon clinical decision making and workplace responsibilities. Rogers et al14 indicated that the risk of medical errors increased in workers who were fatigued. Nurses who exercised weekly had less fatigue and better recovery outcomes compared with those who did not exercise.15 Fatigue features consistently in the literature on health care work performance; for example, in terms of cardiopulmonary resuscitation (CPR) performance, it was also found that fatigue was related to a decrease in the depth of compressions.16,17
Work environments with limited resources and high workloads due to staff shortages are threatening wellbeing and are causal to mounting stress, distress, emotional exhaustion, and burnout.18,19 These limitations have contributed to work hours being directed away from direct patient care, compromised patient safety, lack of organizational commitment to nurses, and limited managerial support.20–23 Furthermore, these factors contribute to job dissatisfaction. Recent research with midwives found 90% of participants have reported feeling worn out, 86% were emotionally exhausted, 85% had high levels of frustration at work,24 and only 9.3% reported feeling energetic.25 Chronic fatigue levels in paramedics are at a peak and were found significantly higher than three groups of nonclinical shift workers, and their opportunities for physical activity are restricted due to ambulance service assignments.26
Nurses, midwives, and paramedics provide care for individuals who are ill, injured, or involved with a life-threatening trauma or death and dying.26–32 Delivering care in these situations is stressful for practitioners as well as patients and families, and causes psychonoxious effects.2,33 Midwives’ stress often results in burnout, particularly in those aged under 35 years and/or practicing in their first 20 years.24,25 For paramedics, stress as a consequence of care delivery is coupled with depression and anxiety.26,32,34 When compared with nonclinical shift workers, paramedics were found to have rates of depression, anxiety, and stress above a normal range.26 The same is true for rural paramedics.32
Retention of employees is an ongoing problem that confronts health professionals, due to the adverse effects of job stress. The two key areas that impact retention are job satisfaction and the workplace environment.35,36 Professional invalidation, low wages, and limited career progression have also intensified the problem for nurses and paramedics.37–40 While workplace retention has been researched, few investigations have incorporated the perspective of health professionals. In particular, there is a dearth of research that focuses on health status, health responsibility, and job satisfaction. More detailed insight related to workplace wellness, from the individual perspective, will contribute to understanding wellbeing more broadly.41,42
Exploring health professionals’ perceptions of their own physical health stress and its possible relationships to job satisfaction was an important aim of the current research. While stress management within the health care field is not an entirely new research topic, less attention has focused on self-perceptions of health status and stress. Furthermore, this research built on previous research themes: stress is pervasive in all aspects of health care delivery; job satisfaction and retention are contingent on emotional health and wellness; health responsibility should be shared; and emotional health and physical health are connected.43 Specifically, this research sought to examine perceptions of current physical health status and the relationships between stress level and physical health and job satisfaction, in nurses, midwives, and paramedics in Australia.
Material and methods
Study aims
This study sought to explore: perceptions of physical health status; current stress levels; the relationship between health and job satisfaction; and the relationship between health and stress. The health participants were nurses, midwives, and paramedics.
Methods
This mixed-method research design utilized two methods: semistructured interviews and a self-rated stress survey questionnaire. The mixed-methods design was intentionally chosen for its possible transformative approach, in contrast with traditional studies, where the voices of the participants are highlighted as integral to the study findings. Therefore, the researchers focused on hearing, listening, and validating the participants’ perceptions and experiences. Examples of the interview questions on physical health are outlined in Table 1.
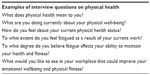  | Table 1 Interview questions |
The Stress assessment scale,44 first published in 2010, showed previous content validity and interrater reliability, when tested on a population of nurses. The questionnaire assessed physical, psychological, spiritual, and cognitive behavioral aspects, identifying an overall stress level. The 25-item questionnaire utilized a five-point Likert scale. The scale was scored as: 5= strongly agree; 4= agree; 3= unsure; 2= disagree; and 1= strongly disagree. The highest stress score was 125 and the lowest, 25. The questionnaire was mailed to each participant, with the option for completion before or immediately following the interview. Examples of the statements on physical health from this assessment are outlined in Table 2.
  | Table 2 Examples of stress assessment items |
Participant recruitment and selection
Participants were recruited by advertisements in health care and professional organizations, using a snowball selection technique.45 Health care professionals who were interested in participating made initial contact, with the chief investigator or the research assistant, by telephone or email. The inclusion criteria were:
- Registered nurse, midwife, or paramedic
- Currently practicing and employed in Australia.
There were 51 practitioners expressing an interest in the study, yet work demands prevented 27 practitioners from proceeding. Following institutional human ethics committee approval and informed consent, data was collected from 24 practitioners who were from several different health care organizations. While most participants did acknowledge that they were experiencing considerable stress, this was not known until each interview took place. Each practitioner was interviewed in a mutually agreeable location. The interview duration was 30–60 minutes. The study data were collected in 2012.
Analysis
The interviews were digitally recorded and uploaded as MP3 recordings. To maintain anonymity and confidentiality, pseudonyms were used to deidentify participants’ names and places of employment. While only one research team member collected the data, all research team members downloaded and listened to each recording. Members made notations against each question and identified recurring data and possible themes. The group then met to discuss commonalities and differences, as well as possible themes, and to confirm data quotes. Following a comprehensive discussion of the actual data and identifying there were no points of difference, the themes and subthemes were confirmed. In relation to the survey data, as a group of 24 participants, in statistical terms, is identified as a small group, each questionnaire was manually collated. The individual scores for each questionnaire were cross-checked and then compared with the rating scale: 25–50 (little or no stress); 51–75 (moderate stress); 76–100 (high stress); and 101–125 (extremely stressed).44 It was not intended that the survey results would be generalizable but rather, that the benefits of data triangulation would add to the richness of the interviews.46
Findings
Demographics
The participants comprised 15 nurses, five midwives, and four paramedics. The participants were currently employed in metropolitan and regional Australia. Their demographic details are outlined in Table 3.
  | Table 3 Descriptors for mean age and mean years of practice |
Research themes
Four themes arose from the data. The first theme revealed participants had different views on physical health in comparison with the Australian Government recommended guidelines. The second theme identified that physical and emotional health are important to job satisfaction. The two remaining themes identified the importance of increasing physical activity levels and a relationship between physical health and stress. Table 4 summarizes these findings.
  | Table 4 Key findings |
Theme 1: different perspectives on physical health to recommended government guidelines
Physical health was perceived as more than the physical capability to perform at work. Specifically, participants spoke of their health being impacted upon by their work responsibilities. Many were concerned about the quality of their diet because fast-paced work demands compromised their eating habits. This comment by one of the nurse participants typified this issue:
The biggest thing I have an issue with at the moment is food. I am always eating on the run.
Furthermore, it was evident that physical health was multifaceted. One senior nurse said:
Physical health, to me, is probably more about well-being [than] any particular ongoing health conditions, especially in regards to work, getting enough sleep, eating right, getting up in the morning with enough energy, feeling good as opposed to feeling run down all the time.
Some of the midwives spoke of physical as well as emotional demands in terms of their physical health:
Physical health is keeping yourself fit enough … midwifery is a very emotionally and physically demanding job … . I meditate every day, do mindfulness training … I walk every 3 days for an hour. I should walk every day … . You put your own needs on hold to look after other people … . I am exhausted as a result of my current work … . [Because of] fatigue I am less motivated to be bothered … to cook a meal. [Branca, midwife]
If you are upset or frightened [at work], that can have an effect on your body … not want to eat, irritable bowel syndrome etc … if you are getting negative feedback that can have a detrimental effect … . I have had a rollercoaster year … . I thought I could do it all … feels like I have been through fire … all the things I have been through … very rarely [I’ve] even had time to take a bath … . [Eliza, midwife]
Theme 2: physical health is important to job satisfaction
Participants identified a connection between physical health and job satisfaction to subsequent retention in their profession. Job satisfaction was a key determinant to workforce retention, and physical health was integral to job satisfaction. As Bailey, a paramedic, stated:
I am not the best I have been. I am not as fit as I used to be. Night shift does not help. Our night shift goes for 14 hours – the feeling of fatigue – it puts a lot of stress on the body. Sometimes you are out all night. I was fatigued 70%–80% of the time – want to sleep in [and], throughout the day I want[ed] to go back to bed. This was what constituted my days off. Work does impact. My back injury was due to CPR and then lifting the patient. Job satisfaction just went downhill.
Claudia, a senior nurse, acknowledged the importance of being injury-free and its relationships to job satisfaction:
There is nothing wrong with my back; fortunately I am in good health … . So many of the nurses of my age who have been lifting all the time and been doing so for 20–25 yrs, they are very tired, and their backs are sore, and they can’t do what I can do. I am very grateful … I can keep up with the younger ones.
Theme 3: desire to increase physical activity levels
Physical health was consistently acknowledged as important, albeit expected levels of physical activity were not within recommended guidelines. Responsibility for health was acknowledged as a personal matter; yet due to the effects of work demands, participants struggled to meet the minimum physical health standards. This comment by one of the nurses exemplified this issue:
I know it’s terrible … I prioritize physical health, right to the bottom of the page. If I have time, I have a massage, which is few and far between, but it would be lovely to exercise and be fit. To tell the honest truth, I don’t do anything. I’ve got five children, so I’ve got to look after the needs of those guys. Generally I come last.
Penny, a midwife provided further insight into this perspective.
My current emotional and physical health could be improved … don’t feel like I do enough walking, meditating etc … . I am not sufficiently disciplined … if I came to something regularly, it may motivate me.
While participants regarded the importance of physical health as their own responsibility, they believed support in the workplace was also needed. Bailey, a paramedic, discussed this in relation to other rescue professionals:
Physical health is not supported. Fire [personnel] get free gym membership but Ambulance [personnel] do not … . I would like to see gym at work, free running shoes … . Health and well-being programs to include fitness, anxiety, depression, impacts of smoking and drinking.
Furthermore, chronic musculoskeletal injuries were identified by most participants. The inability to maintain their physical health had resulted in ongoing chronic pain, thus limiting their ability and job performance. Lack of support, especially from managers, was continually identified:
A lot of patients you go to … you will feel worse or sicker than they are … there is no one helping you. [Polly, paramedic]
Theme 4: physical health and stress are related
The questionnaire demonstrated 23 of 24 participants had a moderate- to high-level of stress.43 Paramedics were the most stressed, the midwives had a similar level of stress, and the nurses were disproportionally lower, respectively scored at 75, 73.78, and 56. The total group stress level was identified to be in the moderate stress range, at 65.
The following comments from participants further exemplified the intensity of their stress at work. For Juliette, a newly graduated midwife, absences from work were attributed to stress, and she indicated that stressors will make her leave her position:
A lot of times when I try to pinpoint why I am not at work, it comes back to how I am feeling physically and emotionally … . I am very stressed out and very tired … . I sometimes feel the “stresses” … [are] going to be the chain breaker – make me leave … . I would prefer to be looked after more … it goes both ways – affecting my decision to stay or leave.
Physical health and the stress of the long working hours were intertwined for paramedics, with surfacing of subsequent health issues. Polly and Ethan explained this issue:
Exercise is difficult … I have a hyperstartle. My alcohol intake has increased. It has also affected my emotional support. I used to run and swim. To walk 1 km is even hard. I have put on 10 kg of weight. Before I was unwell, I would do a 2 km swim and then walk a couple [km] and run 3 [km]. [Polly]
I am becoming more and more fatigued … 14 hours is a long time, it is very draining, and essentially you don’t just work 14 hours, you’re awake you’re on your feet, and then you lose basically half the next day trying to recover from the night before. [Ethan]
Discussion and implications
The findings indicate the importance of physical health to health care professionals, and this extends beyond physical activity, nutrition, and recovery. Similarly, previous health studies and literature have identified factors such as physical inactivity, poor nutrition, and fatigue as impacting upon physical health.47,48 These factors increase the risk of poor health, including cardiovascular/metabolic diseases and musculoskeletal injuries, which consequently impact upon work performance. Our research has confirmed this finding.
Stress was revealed to be at the forefront of care delivery, and the effects of stress impacted on participants’ physical health. Stress also contributed to chronic fatigue and poor lifestyle. Overall stress levels were rated as moderate, and stress was not experienced as an isolated event. The results also confirmed the findings from previous research on the negative effects of workload and destructive interpersonal communication.23,49–51
These findings add to the existing literature on the insidious nature of the stress experienced by health professionals, where stress has been identified as integral in all workplace settings and associated with job dissatisfaction and intention to leave.35 While not specifically measuring for burnout in the questionnaire, the research participants used the term burnout in their interviews. Burnout was identified as a pervasive stress response, and it was also identified that unremitting fatigue, due to long working hours, shift work, staff shortage, and limited resources, impacted on participants’ ability to maintain an acceptable physical health status.
Our findings indicated that components of physical health, especially physical activity, were not well utilized to manage stress. Engagement in physical activity attenuates the effects of stress, job burnout, and dissatisfaction.52 It has been found that workers in high-stress, demanding occupations who were physically active and engaged in high-intensity activity were able to reduce stress levels and increase their levels of energy.53 Furthermore, it was shown that intervention programs that focused on physical activity behavior improved anxiety outcomes in nurses.54 While the complexity of factors impacting on individual’s stress level necessitates diverse stress interventions, increased levels of physical activity is a key consideration.
Two other important findings of the current study were that 1) health professionals’ perception of their physical health was more focused on a sense of well-being than on being able to have an optimal level of physical health for job performance; and 2) participants had a desire to increase their physical activity levels to improve their physical health. Both of these findings can provide reliable background information to develop further research. Specifically, research should be directed to improving workplace environments to, in turn, provide more opportunities for health professionals to achieve personalized health activities. Work pressure is an issue that results in health professionals’ inability to meet the minimum levels of physical activity that they desire; this, along with the high level of stress, results in suboptimal physical competency and lower levels of professional performance, increasing their risk of injury and disease.
Conclusion
This study is representative of the participants who were involved. This study was conducted in a large metropolitan city in Australia. It is not known what the results would have revealed had the study been conducted in a rural area or in another metropolitan city in Australia or beyond. The study may have revealed different results if the methodological approach had been different, for instance, as in an ethnographic, observational study.
As this was a small mixed-method study, it was not intended that the results be generalizable; however, the results may inform the development of subsequent research and future wellness programs for health care professionals. While, a small sample size may be considered a limitation of the study, most of the data were qualitative. It is evident that these results have demonstrated some health care professionals’ current lifestyle interventions need to be improved. Therefore, it is imperative that health-based organizations take responsibility to develop wellness programs that support health professionals’ healthy lifestyle management.
Acknowledgments
The authors thank Australian Catholic University, for the competitive funding to conduct this research, and the participants, for their willingness to share their experiences and their commitment to healthy workplaces.
Disclosure
The authors report no conflicts of interest in this work.
References
Glass N. An investigation of nurses’ and midwives’ academic/clinical workplaces: a healing model to improve and sustain hope, optimism, and resilience in professional practice. Holist Nurs Pract. 2009;23(3):158–170. | |
Lim J, Bogossian F, Ahern K. Stress and coping in Australian nurses: a systematic review. Int Nurs Rev. 2010;57(1):22–31. | |
who.int [homepage on the Internet]. WHO definition of health. World Health Organization; 1946. Available from: http://www.who.int/about/definition/en/print.html. Accessed February 13, 2014. | |
National Institutes of Health. Physical activity and cardiovascular health. NIH Consens Statement [online]. Dec 1995 [cited 2014 February 13];13(3):1–33. Available from: http://consensus.nih.gov/1995/1995ActivityCardivascularHealth101html.htm. Accessed February 13, 2014. | |
Brown WJ, Bauman AE, Bull FC, Burton NW. Development of Evidence-Based Physical Activity Recommendations for Adults (18–64 Years). Canberra: Department of Health and Ageing; 2012. | |
Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. | |
Tsismenakis AJ, Christophi CA, Burress JW, Kinney AM, Kim M, Kales SN. The obesity epidemic and future emergency responders. Obesity (Silver Spring). 2009;17(8):1648–1650. | |
Zapka JM, Lemon SC, Magner RP, Hale J. Lifestyle behaviours and weight among hospital-based nurses. J Nurs Manag. 2009;17(7):853–860. | |
Pietroiusti A, Neri A, Somma G, et al. Incidence of metabolic syndrome among night-shift healthcare workers. Occup Environ Med. 2010; 67(1):54–57. | |
Daraiseh NM, Cronin SN, Davis LS, Shell RL, Karwowski W. Low back symptoms among hospital nurses, associations to individual factors and pain in multiple body regions. Int J Ind Ergon. 2010;40(1):19–24. | |
Ngan K, Drebit S, Siow S, Yu S, Keen D, Alamgir H. Risks and causes of musculoskeletal injuries among health care workers. Occup Med (Lond). 2010;60(5):389–394. | |
Schluter PJ, Turner C, Huntington AD, Bain CJ, McClure RJ. Work/life balance and health: the Nurses and Midwives e-cohort Study. Int Nurs Rev. 2011;58(1):28–36. | |
Vasconcelos S, Marqueze E, Gonçalves L, et al. Morbidity among nursing personnel and its association with working conditions and work organization. Work. 2012;41 Suppl 1:S3732–S3737. | |
Rogers AE, Hwang WT, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff and patient safety. Health Aff (Millwood). 2004;23(4):202–212. | |
Chen J, Davis KG, Daraiseh NM, Pan W, Davis LS. Fatigue and recovery in 12-hour dayshift hospital nurses. J Nurs Manag. Epub April 23, 2013. | |
Gutwirth H, Williams B, Boyle M, Allen T. CPR compression depth and rate in relation to physical exertion in paramedic students. Journal of Paramedic Practice. 2012;4(2):90–95. | |
Gutwirth H, Williams B, Boyle M. Rescuer fatigue in cardiopulmonary resuscitation: a review of the literature. Journal of Emergency Primary Heath Care. 2009;7(4):1–9. | |
Pijl-Zieber EM, Hagan B, Armstrong EC, Hall B, Atkins L. Stingl M. Moral distress: an emerging problem for nurses in long-term care? Quality in Ageing and Older Adults. 2008;9(2):39–48. | |
Görgens-Ekermans G, Brand T. Emotional intelligence as a moderator in the stress-burnout relationship: a questionnaire study on nurses. J Clin Nurs. 2012;21(15–16):2275–2285. | |
Glass N. Investigating women nurse academics’ experiences in universities: the importance of hope, optimism and career resilience for workplace satisfaction. Annual Review of Nursing Education. 2007;5:111–136. | |
Ilhan MN, Durukan E, Taner E, Maral I, Bumin MA. Burnout and its correlates among nursing staff: questionnaire survey. J Adv Nurs. 2008;61(1):100–106. | |
Cowin LS, Johnson M, Craven RG, Marsh HW. Causal modeling of self-concept, job satisfaction, and retention of nurses. Int J Nurs Stud. 2008;45(10):1449–1459. | |
Pannowitz HK, Glass N, Davis K. Resisting gender-bias: insights from Western Australian middle-level women nurses. Contemp Nurse. 2009;33(2):103–119. | |
Jordan K, Fenwick J, Slavin V, Sidebotham M, Gamble J. Level of burnout in a small population of Australian midwives. Women Birth. 2013;26(2):125–132. | |
Mollart L, Skinner VM, Newing C, Foureur M. Factors that may influence midwives work-related stress and burnout. Women Birth. 2013;26(1):26–32. | |
Courtney JA, Francis AJP, Paxton SJ. Caring for the carers: fatigue, sleep, and mental health in Australian paramedic shiftworkers. Australian and New Zealand Journal of Organisational Psychology. 2010;3:32–41. | |
Brough P. Comparing the influence of traumatic and organizational stressors on the psychological health of police, fire, and ambulance officers. Int J Stress Manag. 2004;11(3):227–244. | |
worksafe.vic.gov.au [homepage on the Internet]. Injury hotspots: Ambulance service. WorkSafe Victoria; 2008. Available from: https://www4.worksafe.vic.gov.au/worksafe/hotspots/ambulance_hotspot.html. Accessed February 13, 2014. | |
Meadors P, Lamson A, Swanson M, White M, Sira N. Secondary traumatization in pediatric healthcare providers: compassion fatigue, burnout, and secondary traumatic stress. Omega (Westport). 2009–2010; 60(2):103–128. | |
Leinweber J, Rowe HJ. The costs of ‘being with the woman’: secondary traumatic stress in midwifery. Midwifery. 2010;26(1):76–87. | |
Regehr C, Goldberg G, Hughes J. Exposure to human tragedy, empathy, and trauma in ambulance paramedics. Am J Orthopsychiatry. 2002;72(4):505–513. | |
Courtney JA, Francis AJ, Paxton SJ. Caring for the country: fatigue, sleep and mental health in Australian rural paramedic shiftworkers. J Community Health. 2013;38(1):178–186. | |
Alexander DA, Klein S. First responders after disasters: a review of stress reactions, at-risk, vulnerability, and resilience factors. Prehosp Disaster Med. 2009;24(2):87–94. | |
Bentley MA, Crawford JM, Wilkins JR, Fernandez AR, Studnek JR. An assessment of depression, anxiety, and stress among nationally certified EMS professionals. Prehosp Emerg Care. 2013;17(3):330–338. | |
Lamontagne AD, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job-stress intervention evaluation literature, 1990–2005. Int J Occup Environ Health. 2007;13(3):268–280. | |
Ritter D. The relationship between healthy work environments and retention of nurses in a hospital setting. J Nurs Manag. 2011;19(1):27–32. | |
Cowin LS, Hengstberger-Sims C. New graduate nurse self-concept and retention: a longitudinal survey. Int J Nurs Stud. 2006;43(1):59–70. | |
Orrock M, Lawler J. Health care system reform and senior nurse managers: marginalization as a factor contributing to the nursing crisis. International Journal of Interdisciplinary Social Sciences. 2006;1(2):69–72. | |
Daehlen M. Job satisfaction and job values among beginning nurses: a questionnaire survey. Int J Nurs Stud. 2008;45(12):1789–1799. | |
Patterson PD, Moore CG, Sanddal ND, Wingrove G, LaCroix B. Characterizing job satisfaction and intent to leave among nationally registered emergency medical technicians: an analysis of the 2005 LEADS survey. J Allied Health. 2009;38(3):e84–e91. | |
Coomber B, Barriball KL. Impact of job satisfaction components on intent to leave and turnover for hospital-based nurses: a review of the research literature. Int J Nurs Stud. 2007;44(2):297–314. | |
McCarthy G, Almeida S, Ahrens J. Understanding employee well-being practices in Australian organizations. Int J Health Wellness Soc. 2011;1(1):182–198. | |
Glass N, Ogle KR, Webb H, Rice V, Yeboah C. Wellness for work: perspectives from nurses, midwives and paramedics in Australia. The International Journal of Health, Wellness and Society. 2014;3(1):23–39. | |
Glass N. Interpersonal Relating: Health Care Perspectives on Communication, Stress and Crisis. South Yarra: Palgrave Macmillan; 2010. | |
Sadler GR, Lee HC, Lim RS, Fullerton J. Recruitment of hard-to-reach population subgroups via adaptations of the snowball sampling strategy. Nurs Health Sci. 2010;12(3):369–374. | |
Borbasi S, Jackson D. Navigating the Maze of Research: Enhancing Nursing and Midwifery Practice. 3rd ed. Chatswood: Mosby Elsevier; 2012. | |
Baer HJ, Glynn RJ, Hu FB, et al. Risk factors for mortality in the nurses’ health study: a competing risks analysis. Am J Epidemiol. 2011; 173(3):319–329. | |
Hegg-Deloye S, Brassard P, Jauvin N, et al. Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emerg Med J. Epub January 12, 2013. | |
Tourangeau AE, Cranley LA. Nurse intention to remain employed: understanding and strengthening determinants. J Adv Nurs. 2006;55(4):497–509. | |
Vessey JA, Demarco R, DiFazio R. Bullying, harassment, and horizontal violence in the nursing workforce: the state of the science. Annu Rev Nurs Res. 2010;28:133–157. | |
Cox Dzurec L, Bromley GE. Speaking of workplace bullying. J Prof Nurs. 2012;28(4):247–254. | |
Toker S, Biron M. Job burnout and depression: unraveling their temporal relationship and considering the role of physical activity. J Appl Psychol. 2012;97(3):699–710. | |
Hansen AM, Blangsted AK, Hansen EA, Søgaard K, Sjøgaard G. Physical activity, job demand-control, perceived stress-energy, and salivary cortisol in white-collar workers. Int Arch Occup Environ Health. 2010;83(2):143–153. | |
Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224–231. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
