Back to Journals » Advances in Medical Education and Practice » Volume 11
Exploring Adult Learners’ Viewpoints and Motivation Regarding Distance Learning in Medical Education
Authors Bin Mubayrik HF
Received 19 September 2019
Accepted for publication 22 January 2020
Published 19 February 2020 Volume 2020:11 Pages 139—146
DOI https://doi.org/10.2147/AMEP.S231651
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Haifa Fahad Bin Mubayrik
Department of Educational Policies,College of Education, King Saud University, Riyadh, Saudi Arabia
Correspondence: Haifa Fahad Bin Mubayrik
Department of Educational Policies, College of Education, King Saud University, 3680 - King Saud University Unit No. 3, Riyadh 12372 – 7453, Saudi Arabia
Tel +966555368528
Email [email protected]
Introduction: Literature in education and training supports the notion that distance learning (DL) is the most effective mode of learning for health care workers to improve the quality of patient care. However, implementing DL requires pre-assessing learners’ perspectives and attitudes for providing better delivery, essential support, and facilities. This study aimed to identify the viewpoints and attitudes of dental graduates toward DL in medical education and their point views of the effectiveness and efficacy of DL tools.
Methods: A structured, self-administered questionnaire was distributed to registered adult graduates working in government- or private hospitals in a permanent position or for a long term (3 months or more). Data were collected and analyzed.
Results: Two-thirds (67.9%) of the participants had previously attended a DL course. The highest ranked items on the participants’ views on DL were ease of access, ability to take the course from any location, and be taught from anywhere in the world. Their perception of DL was analyzed in relation to gender and previous exposure to DL.
Conclusion: This investigation revealed a positive attitude among graduates on the effectiveness of DL. Most respondents appreciated DL’s convenience in terms of time flexibility and online attendance. Residents’ attitudes toward DL and DL characteristics are major factors to consider when instituting or planning for DL. Continuous medical education through DL will continue to generate considerable interest as an international movement.
Keywords: distance learning, healthcare, continuous education
Introduction
Despite their busy schedules, health care workers need to keep pace with the developments in their field and maintain and improve their professional knowledge and skills. Also, with the growing number of health care workers, the demand for health education and training services has grown as well. Health education is, therefore, facing an exceptional situation with the large numbers of health care workers and increasing demands and services. Distance learning (DL), in such cases, has played a significant role in the provision of education across the world. In 1996, Dutta Jena, and Panda1 observed that long-distance training in medical and health practice, particularly, can increase its cost-effectiveness and scope. Other studies have found distance education to improve time management, teamwork, communication skills, critical thinking, and knowledge application.2–6 Besides, it has been proven that a well-accepted strategy for higher education successfully engages participants in beyond physical classroom boundaries.2,7,8 Examining the first attempt at long-distance learning in the medical field, Blakeley and Curran-Smith3 reported some astounding outcomes. According to them, it was difficult for registered nurses to continue their health education because of work and home conflicts; however, after completing their first DL nursing course, they could gain and apply new knowledge. DL also served to impart knowledge and skills long distance; McDonald et al9 claimed that e-based learning per se is comparable to patient simulation.
Despite its advantages, DL also has its shortcomings. Bloomfield and Jones10 underscored the importance of supervision in technical procedures once training was completed. Others expressed concerns about DL limiting interactions and causing technical difficulties, and how its efficacy depends on the instructional design used.7–9 Thus, a combination of conventional teaching methods and DL may be an effective educational technique, particularly for undergraduates.9–11 Moreover, it would be difficult to implement DL in the medical corridors for specific clinical skills and procedures. Therefore, to effectively deliver these skills using a DL approach, adding video materials to the virtual program could help tackle the challenges of DL’s limitations as well as create a positive environment.12
DL in the medical field has thrived because of the problems and difficulties that have choked traditional learning. Most previous studies2–4,9–12 have measured DL’s effectiveness, usage, and design. However, learning attitudes and perceptions are also essential factors in successful learning.13 Therefore, this study aimed to identify the perceptions and attitudes of dental graduates toward DL in medical education and how effective and efficient they found the DL tools.
Methods
The Questionnaire
A structured, self-administered questionnaire was developed based on a literature review and pretested.8,12 A short introduction in the questionnaire explained the aim and the definition of distance- and face-to-face learning. There were 16 questions relating to distance- and face-to-face learning. The first part contained the introduction and asked participants whether they had attended a DL course. The second part had 16 questions that asked about the viewpoints of participants about DL, motivation, main characteristics of DL, advantages and disadvantages, as well as their opinion about face-to-face learning as compared to DL. The questionnaire was in random order. The responses were scored on a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.” The pilot study was conducted on 30 participants. No adjustments were necessary, and thus, the questionnaire was distributed to the study population.
Method and Participants
Ethical approval was granted by the local institutional Research Ethics Committee. Respondents were assured that their responses would remain confidential. The questionnaires were distributed and collected immediately after the survey by the researcher. Questionnaires were distributed to 106 dental graduates, and participation was voluntary. The purpose of the study was explained, and any uncertainties were resolved prior to participation. All participants were registered adult graduates working in government or private hospitals in a permanent position or for a long term (3 months or more).
Statistical Analysis
The collected data were analyzed using IBM SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, NY, USA). Frequencies, means, and exploratory factor analysis were used to analyze the prevalence of statistical differences.
Results
The Cronbach’s alpha value for the questionnaire was 0.863, which was above 0.70, indicating a good internal consistency. Women constituted 39.65% of the total respondents and men 60.4%. A total of 67.9% (24.5% women and 43.4% men) had previously attended a DL course. Of all the items, the ones most respondents valued and ranked the highest were convenient access to the online course (88.7%), followed by the ability to attend from any location (88.7%), and being taught from anywhere in the world (83.01%). The lowest-ranked item was DL workload (37.7% were not sure), followed by the need for IT support in DL (almost half the sample [49.1%] either did not agree or was not sure) (see Table 1, Figure 1).
 |
Table 1 Summary of Questionnaire Responses |
 |
Figure 1 Graphical representation of graduates’ responses to the questionnaire. |
 |
Figure 2 Scatter plot representation of the correlation between face-to-face benefits and advantages and disadvantages of distance learning. |
Perception of DL was analyzed in relation to gender and previous exposure to DL. Women suggested that it would be more useful if DL was based on daily clinical practice (p = 0.035) than did men. Responses from respondents who had attended a DL course and who found DL interesting, flexible in terms of time and location, global, self-paced, self-regulated, useful if accompanied by videos, and based on daily practice were statistically significant (p = 0.000). Respondents who had attended a DL course believed they would use the knowledge they learnt through DL in the future (p = 0.001). Significant responses also corresponded to enthusiasm in attending a DL course (p = 0.011) and considering DL cost-effective (p = 0.031) (Table 2).
 |
Table 2 T-Test Results of Questionnaire Responses According to Gender and Prior Attendance of Distance Learning Courses |
Factor analysis was also performed (Table 3). The correlation matrix showed the appropriateness of the data for factor analysis. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.810 (more than 0.6). Bartlett’s test of sphericity was significant (0.0001); thus, factor analysis with principal component analysis was performed. Using the rotated component matrix and the extraction method, with Varimax as the rotation method and Kaiser normalization, three factors were extracted. The names of the factors were created based on the meaning of the variables included in each factor. The three factors were attitude toward DL and characteristics, face-to-face (F2F) instruction benefits, and advantages and disadvantages of DL. The three factors were ranked based on students’ responses (Table 4).
 |
Table 3 Factor Loadings of Questionnaire Items |
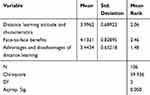 |
Table 4 Factors as Ranked by Students’ Responses |
Correlation
Spearman’s correlation indicated a significant moderate positive association between attending DL courses and attitude toward DL and characteristics (r(106) = 0.605, p = 0.000). It also indicated that there was a significant moderate positive association between appreciating F2F instruction benefits and valuing the advantages and disadvantages of DL (r(106) = 0.531, p < 0.000) (Figure 2).
Discussion
This investigation revealed a positive attitude toward DL among graduates, as two-thirds of the sample had attended DL at some point before taking the questionnaire. A majority of the respondents appreciated DL’s convenience in terms of time flexibility and online attendance. The results also revealed that residents’ attitudes toward DL and DL characteristics are major factors to consider when instituting or planning for DL and that understanding the advantages of traditional learning affects learners’ attitude toward DL. Thus, promoting DL’s benefits, convenience, and success may increase adult learners’ acceptance of DL as an alternative learning approach and lead to higher enrollment. Additionally, DL education in health care delivery is useful since it is applied at a learner’s own pace, which helps in reducing instructional time and complications for individual trainees. Indeed, long-distance training is effective provided it is adequate, appropriate, and soundly designed. It works well to address technical ability with its fixed assessment of performance.
As the results indicate, attending DL courses increases participants’ optimism toward and belief in DL. Factors related to this result include being taught by global experts and learning at one’s own pace and on one’s own time. Additionally, in the medical health field, there is often insufficiency of specialists and resources. A combination of these and other difficulties in medical health makes formation of DL centers of excellence a reasonable point of concern. Of importance is the complex nature and the vastness of the content of medical education courses. As health care education is critical for successful health outcomes, integration of DL should not be undertaken blindly. A successful integration should incorporate a well-choreographed plan that considers the most preliminary activities, which includes considering the varying attitudes toward and experiences of the DL participants before fully embracing this approach. First, a medical training institute must carry out a needs assessment to evaluate attitudes toward DL. If a need to implement distance education is determined, then a series of logical decisions are necessary to adopt DL.
Many global institutions have tested DL as a stand-alone solution in a bid to improve continuous medical education.6,14–19 The outcomes of these projects were successful, and hence, adoption of distance education in the field of medical health was advocated in these cases.6,14–19 In general, experts recommend initiating DL with an assimilation strategy that considers the pros and cons before implementation.17,18 Still, there is a need to widen the scope of DL training, particularly in new technical procedures and complex skills.20,21 Another limitation is the difficulty in measuring clinical skills obtained from DL and the difficultly and time needed to prepare its context.20,22 Strengthening medical skills with the help of videos and role-plays while simultaneously practicing on real patients immediately after completing a DL course can ensure a successful distance education.20,21 To measure learner’s attitudes, knowledge, and skills, it might be crucial to utilize adaptive learning that takes advantage of technology. This is applied at the beginning of the online training to determine which educational materials are the most appropriate for each learner.23,24
The Accreditation Council for Graduate Medical Education has instituted core competencies concerning the application of e-learning in graduate medical education.25 E-learning constituents that meet these requirements can be incorporated into the education of medical residents and fellows, substituting for lectures and other synchronous methods of instruction.26,27 As a result, an increase in the use of educational software programs in medical education has been reported.28
Asynchronous DL can be successfully utilized during demanding clinical care. Randomized trials of DL have been demonstrated to produce effects similar to those of traditional educational methods.22,29,30 The results of this investigation are encouraging. The positive attitudes toward DL found in this study show DL continuing education courses could be used for training in the workplace. The study outcomes are also helpful for policymakers and health care administrators to plan for continuing education, particularly because there is an increased global demand for medicine and medical facilities. This unprecedented growth in health care delivery has necessitated a quick turnaround in the medical world to match the supply with the demand. The changes that have triggered an increased demand for health care providers have simultaneously instigated increased demands on medical faculty, which can be met through DL.
Indeed, the future has a lot to offer regarding the transformation of pedagogical and instructional methods of DL, which is still in its inception stage, and with the current dynamic technological revolution, more sophisticated ways of delivering education are at hand. An important aspect of DL in continuous medical education is that in e-learning’s online environment, adaptive learning shows promise because it helps to identify the learner, personalize content, and individualize tracking, monitoring, support, and assessment. Similarly, collaborative learning has the potential to end learner isolation. The enormous advancements in synchronous distance education play a pivotal role in enhancing collaborative learning. Likewise, the continuous development of collaborative technologies, which include tools such as e-mail, teleconferencing, chats, message boards, and weblogs, contributes to collaborative learning’s success.
Despite the gains in medical education in using DL, its drawbacks should also be considered. In a systemic review31 of medical students involving 249 papers, it was revealed that technology may be a barrier for both tutors and students. Technology must be perceived as useful and easy for a successful course. They also found that interactivity and feedback between tutor and peer play a significant role in understanding, performance, and accepting the course. Course design and content are also crucial when using DL; for example, courses using virtual microscopy are highly valued when compared to virtual textbooks.31 Thus, previous limitations should be considered when planning for DL courses for adult health care learners.
Conclusion
Regarding continuous medical education around the world, DL offers a likely direction for the future. Indeed, distance education in health care has just begun, and this method of instruction has much potential. Earlier, distance education would have been considered inferior to traditional training in any field, but not anymore; distance education in all academic areas is in high demand, particularly by busy, in-service professionals. Although some biases may jeopardize the research on DL, there is enough evidence to show that health specialists effectively pass short courses associated with their present employment.
Ethical Considerations
Ethical approval was obtained from Research Ethics Committee, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia. (IRB#KSU-HE-19-235). Participation was voluntary, and both verbal and written consent were obtained prior to contribution.
Acknowledgments
The author would like to express deepest thanks to the Researchers Support and Services Unit at King Saud University for their editorial assistance.
Funding
This research project was supported by a grant from the Research Center for Humanities, Deanship of Scientific Research, King Saud University.
Disclosure
The author declares no conflict of interest.
References
1. Dutta PK, Jena TK, Panda SK. A plea for health manpower training through distance education. Med Educ Online. 1996;1(1):4285. doi:10.3402/meo.v1i.4285
2. Ahrens A, Zascerinska J, Ramar H, Andreeva N Educators’ opinion on webinars in higher education.
3. Blakeley JA, Curran-Smith J. Teaching community health nursing by distance methods: development, process, and evaluation. J Contin Educ Nurses. 1998;29(4):148–153.
4. McCutcheon LRM, Alzghari SK, Lee YR, Long WG, Marquez R. Interprofessional education and distance education: a review and appraisal of the current literature. Curr Pharm Teach Learn. 2017;9(4):729–736. doi:10.1016/j.cptl.2017.03.011
5. Lahti M, Kontio R, Pitkänen A, Välimäki M. Knowledge transfer from an e-learning course to clinical practice. Nurse Educ Today. 2014;34(5):842–847. doi:10.1016/j.nedt.2013.09.003
6. Sezer B. Faculty of medicine students’ attitudes towards electronic learning and their opinion for an example of distance learning application. Comput Hum Behav. 2016;55(PartB):932–939. doi:10.1016/j.chb.2015.10.018
7. Fadlelmola FM, Panji S, Ahmed AE, et al. Ten simple rules for organizing a webinar series. PLoS Comput Biol. 2019;15(4):e1006671. doi:10.1371/journal.pcbi.1006671
8. Knipfer C, Wagner F, Knipfer K, et al. Learners’ acceptance of a webinar for continuing medical education. Int J Oral Maxillofac Surg. 2019;48(6):841–846. doi:10.1016/j.ijom.2018.11.010
9. McDonald EW, Boulton JL, Davis JL. E-learning and nursing assessment skills and knowledge: an integrative review. Nurse Educ Today. 2018;66:166–174. doi:10.1016/j.nedt.2018.03.011
10. Bloomfield JG, Jones A. Using e-learning to support clinical skills acquisition: exploring the experiences and perceptions of graduate first-year pre-registration nursing students: a mixed method study. Nurse Educ Today. 2013;33(12):1605–1611. doi:10.1016/j.nedt.2013.01.024
11. Delf P. Designing effective eLearning for healthcare professionals. Radiography. 2013;19(4):315–320. doi:10.1016/j.radi.2013.06.002
12. Wagner F, Knipfer C, Holzinger D, Ploder O, Nkenke E. Webinars for continuing education in oral and maxillofacial surgery: the Austrian experience. J Cranio-Maxillofac Surg. 2019;47(4):537–541. doi:10.1016/j.jcms.2019.01.009
13. Sun P-C, Tsai RJ, Finger G, Chen -Y-Y, Yeh D. What drives a successful e-learning? An empirical investigation of the critical factors influencing learner satisfaction. Comput Educ. 2008;50(4):1183–1202. doi:10.1016/j.compedu.2006.11.007
14. Cabral VK, Valentini DF
15. Diniz KKS, Pagano AS, Fernandes APPC, Reis IA, Pinheiro Júnior LG, Torres H de C. Knowledge of professional healthcare providers about sickle cell disease: impact of a distance education course. Hematol Transfus Cell Ther. 2019;41(1):62–68. doi:10.1016/j.htct.2018.06.004
16. Blake H, Gartshore E. Workplace wellness using online learning tools in a healthcare setting. Nurse Educ Pract. 2016;20:70–75. doi:10.1016/j.nepr.2016.07.001
17. Al-Hadithy N, Ghosh S. Smartphones and the plastic surgeon. J Plast Reconstr Aesthet Surg. 2013;66(6):e155–e161. doi:10.1016/j.bjps.2013.02.014
18. Mazzoleni MC, Rognoni C, Finozzi E, et al. Usage and effectiveness of e-learning courses for continuous medical education. Stud Health Technol Inform. 2009;150:921–925.
19. Farrell B, Jennings B, Ward N, et al. Evaluation of a pilot e-learning primary health care skills training program for pharmacists. Curr Pharm Teach Learn. 2013;5(6):580–592. doi:10.1016/j.cptl.2013.07.005
20. Lejarraga H, Ageitos ML, Galli A, Castro C. A countrywide programme of continuing professional development in Argentina. Arch Dis Child. 1998;78(6):562–566. doi:10.1136/adc.78.6.562
21. Long P, Kiplinger N Making it happen: using distance learning to improve reproductive health provider performance. Available from: https://www.intrahealth.org/sites/ihweb/files/attachment-files/DL_high_res.pdf.
22. Mojtahedzadeh R, Mohammadi A, Emami AH, Rahmani S. Comparing live lecture, internet-based & computer-based instruction: a randomized controlled trial. Med J Islam Repub Iran. 2014;28:136.
23. Menon A, Gaglani S, Haynes MR, Tackett S. Using “big data” to guide implementation of a web and mobile adaptive learning platform for medical students. Med Teach. 2017;39(9):975–980. doi:10.1080/0142159X.2017.1324949
24. Sharma N, Doherty I, Dong C. Adaptive learning in medical education: the final piece of technology enhanced learning? Ulster Med J. 2017;86(3):198–200.
25. Accreditation Council for Graduate Medical Education. ACGME common program requirements; Section VI with background and intent. Available from: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_Section%20VI_with-Background-and-Intent_2017-01.pdf.
26. Zeiger RF. Toward continuous medical education. J Gen Intern Med. 2005;20(1):91–94. doi:10.1111/j.1525-1497.2004.30049.x
27. Ruiz JG, Mintzer MJ, Leipzig RM. The impact of e-learning in medical education. Acad Med. 2006;81(3):207–212. doi:10.1097/00001888-200603000-00002
28. Kim S. The future of e-learning in medical education: current trend and future opportunity. J Educ Eval Health Prof. 2006;3:3. doi:10.3352/jeehp.2006.3.3
29. Fordis M, King JE, Ballantyne CM, et al. Comparison of the instructional efficacy of Internet-based CME with live interactive CME workshops: a randomized controlled trial. JAMA. 2005;294(9):1043–1051. doi:10.1001/jama.294.9.1043
30. Moja L, Moschetti I, Cinquini M, et al. Clinical evidence continuous medical education: a randomised educational trial of an open access e-learning program for transferring evidence-based information - ICEKUBE (Italian clinical evidence knowledge utilization behaviour evaluation) - study protocol. Implement Sci. 2008;3(1):37.
31. Wong G, Greenhalgh T, Pawson R. Internet-based medical education: a realist review of what works, for whom and in what circumstances. BMC Med Educ. 2010;10:12. doi:10.1186/1472-6920-10-12
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
