Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Experiences and Perceptions of Post-Stroke Fatigue Among Stroke Survivors in Saudi Arabia: A Qualitative Interview Study
Authors Alahmari WS, Shalabi KM , Basuodan RM , Alhowimel AS , Alotaibi M
Received 6 September 2023
Accepted for publication 27 November 2023
Published 4 December 2023 Volume 2023:16 Pages 3761—3776
DOI https://doi.org/10.2147/JMDH.S434312
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wafa Saeed Alahmari,1,2 Kholood Matouq Shalabi,1 Reem M Basuodan,1 Ahmed Saad Alhowimel,3 Mazyad Alotaibi3
1Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 2Centre for Rehabilitation and Ageing Research, School of Medicine, University of Nottingham, Nottingham, UK; 3Physical Therapy and Rehabilitation Department, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia
Correspondence: Kholood Matouq Shalabi, Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, PO Box 84428, Riyadh, Saudi Arabia, Email [email protected]
Purpose: Post-stroke fatigue (PSF) is a debilitating condition that negatively impacts the quality of life of stroke survivors. The rehabilitation of stroke survivors is important for their quality of life, and rehabilitation programs that cater to the needs of these patients are required. However, there is very little published information on their needs, especially in the Middle East. Therefore, this study aimed to explore stroke survivors’ perceptions and experiences of PSF and its causes, its impact on their daily life, their coping strategies, and support from physicians and caregivers in the context of Saudi Arabia.
Patients and Methods: This qualitative interview study was conducted with eight post-stroke survivors from two tertiary stroke centers in Saudi Arabia.
Results: The responses in the interviews showed high heterogeneity. From the responses, five main themes and several subthemes were generated: (1) description of PSF as both a physical and psychological experience; (2) perceived causes of PSF (physical causes, psychological causes, and stroke-related causes); (3) impact of PSF on daily life (activities of daily living and social interactions); (4) coping strategies for PSF (pacing, self-motivation, and social participation); and (5) perspectives about support from caregivers and healthcare practitioners (lack of support, provision of information about PSF and its management, physiotherapy interventions, encouragement, and overprotectiveness).
Conclusion: Stroke survivors have variable physical and psychological experiences of PSF and variable perceptions of its causes and impact. High heterogeneity was also noted in the perception of support provided by healthcare providers and families or caregivers—ranging from lack of support to overprotection. Similarly, patients’ perceptions of the role of physiotherapy and their attitude towards physiotherapy were also variable. Despite this, the findings do highlight the need for more individualized understanding of PSF and the development of treatment strategies that consider biological, psychological, and social factors.
Keywords: cerebrovascular stroke, fatigue, inductive thematic analysis, patient perspective, Saudi Arabia, semi-structured interview
Introduction
Post-stroke fatigue (PSF) is a debilitating condition that affects 25% to 85% of patients with cerebrovascular stroke worldwide.1 Although it is a common condition, there are scarce data about its diagnosis and management.2–4 Further, there is no clear definition for PSF on account of its heterogeneous clinical presentations, inherent subjectivity, and complex biopsychosocial elements.5,6 It is commonly defined as a feeling of early exhaustion that develops during physical or mental activity, results in interference with usual and desired activities, and does not improve with rest.5,7 PSF can occur in patients with all types of stroke, even in those with minor strokes and little disability.8 Several factors have been reported to increase the risk for PSF, including sociodemographic factors (eg, older age, female sex, and smoking status), stroke-related factors (eg, stroke type, stroke location, and associated leukoaraiosis), comorbidities (particularly diabetes mellitus), and psychological factors (eg, depression, anxiety, and sleep disturbances). However, these risk factors are not well-established.8 With regard to the effects of PSF, it has been reported that PSF affects stroke survivors’ quality of life through its negative effects on cognition and ability to participate in social activities and rehabilitation programs.9–11 Given the variable presentation of PSF, it is important to understand the perspective of post-stroke survivors to develop appropriate management strategies. However, very few qualitative studies have attempted to explore the perspectives of stroke survivors on PSF.12 For example, in a meta-synthesis of 12 qualitative studies investigating stroke survivors’ experiences of fatigue,13 only four studies explicitly mentioned PSF in their aims.9–11,14 Further, a previous review on PSF interventions reported that there was insufficient evidence to demonstrate the efficacy of any intervention for treating or preventing fatigue after a stroke.15,16 Thus, there is a clearly a need for more studies from the perspectives of stroke survivors in order to better understand the patterns of presentation, risk factors, and appropriate treatment strategies.
The majority of the studies on PSF have been conducted in Western countries, and the available literature on PSF in the Middle East is still rudimentary. As the healthcare context and sociocultural perspectives in this region are distinct from those of Western countries, this is likely to be reflected in the characteristics, perceptions, and expectations of stroke survivors. Therefore, the present study sought to address this gap by exploring how post-stroke survivors in Saudi Arabia, a country in the Middle East, experience and perceive PSF and its causes, how it impacts their daily life, their coping strategies, support from caregivers and doctors, and the management strategies. To the best of our knowledge, this is the first such qualitative study to be conducted in the Middle East region, specifically Saudi Arabia, and therefore, the findings would have high clinical value in the treatment of stroke patients in this region.
Materials and Methods
Study Design and Setting
This is a qualitative descriptive study that uses a semi-structured interview approach and was conducted at two major rehabilitation centers in Saudi Arabia, namely, King Fahad Medical City Hospital (KFMC) and Sultan Bin Abdelaziz Humanitarian City Hospital (SNAHC).
Recruitment and Sampling Method
The participants were selected using purposive sampling, and the maximum variation technique was utilized to optimize the spectrum of participants’ perspectives studied.17
Hospital registry records of the stroke units at KFMC and SNAHC were used to identify potential participants, who were invited to face-to-face interviews. The primary researcher (WA) informed each patient individually about the details and the purpose of the research in a 30-minute session. Then, WA handed them an informed written consent form to read and ensured that they had adequate time to read it. Those who agreed to participate in the research and signed the written informed consent form were recruited to the study.
Participants
Adult patients (≥18 years old) diagnosed with cerebrovascular stroke for at least one month prior to recruitment with moderate to severe fatigue (based on a fatigue severity scale [FSS] score of at least 4) and enrolled in a physiotherapy treatment were invited to participate. Patients with other central nervous system disorders (eg, multiple sclerosis and Parkinson disease) or medical conditions that can exacerbate fatigue (eg, cardiac, renal, or hepatic diseases) were excluded. The patients’ medical files were reviewed to exclude those with chronic illness prior to the recruitment process. Patients who were unable to communicate due to dementia, aphasia, or cognitive impairment were also excluded because the research was dependent on patients’ ability to communicate their own perceptions and experiences.
Procedure and Data Collection
Face-to-face semi-structured interviews with open-ended questions were used to collect the data. An interview guide (Table 1) was developed based on a literature review and based on the aims of this study, which was to explore patients’ perception of PSF, its causes, its impact on their daily life, coping strategies, support received from caregivers and doctors, and the role of physiotherapy and other interventions in its management. A pilot study was conducted with two participants (who were not included in the final sample), and based on the results, some words in the interview guide were changed or simplified. All interviews were conducted by the same researcher (WA) in a private meeting room at the hospitals, and the interviews lasted for 30 to 40 min. The interviews were carried out in the Arabic language (the native language of the researcher and the patients) and were recorded with a digital audio recorder.
 |
Table 1 Interview Guide |
Before the interview, data on the patients’ sociodemographic characteristics (ie, age, gender, educational level, and occupation), medical history, FSS score, functional activity levels, and physiotherapy interventions received were recorded.
To reduce bias, the researcher explained the details of the interview and its purpose to the participants and ensured that they understood it before conducting the study. Moreover, the researcher was not previously acquainted with any of the participants and, therefore, did not influence their responses. The researcher maintained a reflective diary that documented the experiences, including the strengths and weaknesses, of the interviews conducted.
Ethical Considerations and Informed Consent
The study was approved by the Faculty of Medicine and Health Sciences ethics committee at the University of Nottingham (the primary host institution) (ethical approval number 2631603) and by the local ethical governance committees of KMFC (institutional review board approval number 00010471) and SBAHC. All participants were given an information sheet to read and an informed consent form to sign in which they were assured that they were free to withdraw at any point and that their responses could be published in an anonymized fashion. Study complies with the Declaration of Helsinki.
Data Analysis
The interviews were recorded using a digital audio recorder and transcribed into Arabic by WA, after which they were translated into English by the primary researcher (WA). The accuracy of the translated text was checked by two researchers proficient in Arabic and English (MA and MH). Any discrepancies that arose were discussed, and suitable English terms were selected. To further validate the translation, the transcripts were given to two other researchers (AH and KH) who were proficient in both English and Arabic. The researchers who verified the translated text, that is, MA, and AH, were not involved in the research. The final English draft was agreed upon by all researchers, translated into Arabic, and compared to the original transcripts in Arabic to further validate the data and translation process.
The final transcripts were anonymized and analyzed with inductive thematic analysis.18 WA thoroughly reviewed the interview transcripts and began coding and mapping them according to appropriate subthemes and themes. This mapping exercise involved the entire research team, and the researchers collectively agreed on the grouping of codes into themes.
Results
Sociodemographic and Clinical Characteristics
The study included eight participants (four males and four females) (mean age = 52.4 ± 14 years; range, 27–65 years). All the participants were married. With regard to their level of education, six had a Bachelor’s degree and two had a higher degree. With regard to occupational status, three participants had retired, 2 had stopped working due to stroke, two had a part-time job, and one had a full-time job. Out of the 8 participants, 5 were from the outpatient department and 3 were from the inpatient department.
The duration of time since stroke onset ranged from 2 to 24 months (mean ± SD = 6.8 ± 7.8 months). Four patients (50%) had left hemiparesis/hemiplegia, and four (50%) had right hemiparesis/hemiplegia. With regard to comorbidities, six patients (75%) had hypertension; five (62.5%), diabetes; and two (25%), dyslipidemia. Only two patients had no medical comorbidities other than stroke. The FSS scores ranged from 4.5 to 6.11 (mean = 5.31 ± 0.5). Their functional levels ranged from independent to “modified independent”, which referred to… (Table 2). Table 3 presents the physiotherapy interventions, which comprised stretching exercises, strengthening exercises, endurance and gait training, and education and home exercise programs.
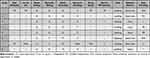 |
Table 2 Functional Levels of the Participants |
 |
Table 3 Physiotherapy Interventions Being Received by the Participants |
Themes and Subthemes
Five main themes were identified from the interview transcripts: (1) experience of PSF, (2) perceived causes of PSF, (3) impact of PSF on daily life activities, (4) strategies for coping with PSF, and (5) perceptions about support from caregivers and healthcare practitioners. The themes are detailed in this section and summarized in Table 4.
 |
Table 4 Summary of the Themes and Subthemes Generated from the Interviews |
Theme 1: Experience of PSF
This theme aimed at capturing the patients’ experience and description of PSF. Patients were asked to freely describe the symptoms of fatigue they experienced following stroke, in terms of both physical symptoms and their psychological state. It was noted that most participants found it challenging to describe PSF. In general, they used terms such as “being tired and sluggish”, “lacking energy”, and “feeling sleepy and exhausted” to explain their understanding of PSF.
Tired. I have no energy and I don’t like doing anything even when I can…I feel sluggish all day at home. [Participant 7, male]
I feel tiredness in my whole body. [Participant 3, female]
Some more specific descriptions of PSF symptoms were also reported by participants, and these included physical symptoms (such as pain, weakness, sleepiness, loss of balance, lack of energy, headache, and tachycardia) and psychological symptoms (such as poor concentration and emotional/mood disturbance).
Here is an example of a quote describing physical symptoms:
I feel heartache with a rapid pulse, and tiredness and sluggishness. [Participant 1, female]
Here are examples of quotes describing psychological symptoms:
Sometimes tiredness affects my understanding, and my concentration is low even during conversations. [Participant 1, female]
Sluggishness causes me to have low concentration and to become distracted. [Participant 3, female]
Sluggishness makes me feel disappointed and causes me to cry for no reason. [Participant 6, male]
The responses under this theme were, thus, varied and ranged from physical to psychological symptoms.
Theme 2: Perceived Causes of PSF
In general, it appeared that participants found it difficult to understand the causes of PSF and were hesitant about their answers. Most participants reported psychological or physical factors such as weakness and emotional exhaustion, but a few participants felt that PSF is an expected sequel of stroke that results from biological factors associated with stroke. Their responses can be categorized into the three subthemes: psychological factors, physical factors and “it is normal”.
Psychological factors: Most participants considered psychological factors to be a direct cause of PSF. More specifically, they felt that sluggishness and tiredness were the main causes of PSF.
I feel tired and exhausted as a psychological result of the condition. [Participant 8, male]
It’s psychological more than physical. [Participant 8, male]
Sluggishness may be due to the psychological condition. [Participant 2, female]
The responses indicated that the participants felt that the stress and strain caused by the negative experience of their recent stroke might have resulted in mental and emotional exhaustion.
Physical factors: Some participants attributed PSF to physical factors such as immobility and weakness, which were sequelae of their stroke. They also believed that their energy levels were altered as a result of chronic immobility.
I think this tiredness is because my body has adapted to my condition. I have spent 6 months lying on my bed, so my muscles have relaxed and weakened even though I have gained more weight. [Participant 3, female]
Only one participant thought that PSF was caused by biological factors, such as vitamin deficiency.
It may be because the vitamin D and hemoglobin levels in my body are low. [Participant 2, female]
“It is normal”: A few participants did not attribute PSF to any cause. They felt that one should expect to experience fatigue following a stroke and that it is a “normal” part of having a stroke.
I think tiredness is a normal result of the stroke. [Participant 5, male]
I feel like laziness comes without a reason; I feel it all day. [Participant 2, female]
Thus, it appears that the perceived causes were varied and ranged from psychological and physical factors to biological factors directly associated with stroke.
Theme 3: Impact of PSF on Daily Life Activities
Under this theme, most participants reported that fatigue had a notable negative impact on their life.
This feeling of tiredness completely changed my life. After the stroke, the feeling has gone up 90%. [Participant 2, female]
The stroke survivors mainly described how PSF affected their activities of daily living (ADLs) and their social interactions. Thus, two subthemes were observed: impact on ADLs and impact on social interactions.
Impact on ADLs: All the participants had busy and active lifestyles prior to stroke, and they had not experienced such fatigue previously. From the quotes below, it can be deduced that the fatigue was the reason why they could not be as active, busy, or athletic as they were before the stroke.
I didn’t feel any tiredness before the stroke. I used to be active and athletic. [Participant 6, male]
I didn’t feel any fatigue before the stroke. I used to have a busy life. [Participant 3, female]
The participants reported experiencing sudden onset of fatigue after their stroke that impacted their ability to carry out their usual activities. The patients expressed disappointment about the new difficulties in their life imposed by their perceived fatigue, and they frequently compared their active pre-stroke lifestyle to their sedentary post-stroke lifestyle. When asked to describe the impact of PSF on their everyday activities, they emphasized that PSF made every day self-care activities, such as eating, bathing, dressing, and showering, more challenging and tiring.
Sometimes, I feel too tired even just to eat my meal or go to the toilet. [Participant 4, female]
Some participants also reported that PSF had an impact on their basic ADLs, such as doing housework, managing their finances, and engaging in social activities. They reported having to perform tasks based on their energy levels and discussed the importance of pacing in enabling them to function.
Before I developed this condition, I would tidy the whole house, but now, with this tiredness, I do one task at a time. [Participant 3, female]
I want to tidy my bedroom, but I don’t want to move. [Participant 2, female]
I need a lot of time to finish one task. [Participant 2, female]
The participants also spoke about how PSF had affected their ability to learn and apply new knowledge. Some participants described the challenges they faced with reading.
Tiredness is linked to concentration, such as when I’m talking to you or reading something. [Participant 3, female]
I used to love reading, but now I avoid it. [Participant 3, female]
My concentration goes down when I’m reading, and even reading makes me tired. [Participant 4, female]
I can’t read now because I easily get tired. The same goes for watching TV. [Participant 5, male]
The participants also reported that some activities that they previously found enjoyable and easy to do had become less pleasurable, and that they had started to avoid these.
Some participants reported that fatigue had limited their mobility and ability to access the wider community. Activities, such as walking, driving, and using public transport, that they had previously found easy, had become more challenging.
Due to this feeling [tiredness], I limit my driving to nearby areas. [Participant 8, male]
I feel tired, dizzy and fatigued when driving. [Participant 6, male]
Some participants described the negative impact of fatigue on their mobility, including their ability to climb stairs or travel.
Travelling makes me tired. I can travel only a short distance. [Participant 3, female]
I also feel tired and lazy climbing the stairs. I need more time than before to go up the stairs. [Participant 1, female]
Impact on social interactions: Some participants stated that PSF had affected their work and participation in social activities, as it limited interpersonal interactions, such as informal meetings with friends and relatives and social events.
This tiredness prevented me from attending meetings and social gatherings. [Participant 3, female]
At work, I can’t complete my task because I’m tired. I usually ask my friend to help me. [Participant 8, male]
Participants also described how PSF limited their community, social, and civic life. Recreational and leisure activities, such as watching TV, going to the gym, and walking, which they had found enjoyable and accessible before their stroke, had become more challenging.
I liked going to the gym before the stroke and the exhaustion, but there’s no way I could do that now. [Participant 3, female]
Before [the stroke], I used to walk outdoors for 3 hours, but now I can no longer do that because I feel tired. [Participant 3, female]
Overall, the participants felt that the everyday activities that they had taken for granted before their stroke, such as work meetings, social gatherings, and leisurely activities, had become limited due to their PSF.
Theme 4: Strategies for Coping with PSF
This theme depicts the strategies used to cope with fatigue in the patients’ daily lives. Their responses were categorized as pacing, self-motivation, and social participation.
Pacing: Almost all participants reported that sleeping, resting, having breaks, and pacing their activities (either physical or mental) improved their PSF symptoms. This helped them cope with their fatigue and enabled them to finish tasks.
I rest and sleep when I feel tired. After that, I feel like I can move. [Participant 7, male]
The tiredness decreases after I sleep. [Participant 3, female]
They reported that the onset of fatigue during activities occurred faster than it did prior to the stroke and that they had to train themselves to respond to their increased demands for rest and sleep. The onset of fatigue also prevented them from continuing their task, and they needed to rest in order to resume their activity later.
When I feel tired, I take a break and sleep. After that, I feel better. [Participant 8, male]
Thus, slowing down and taking multiple breaks improved their ability to handle fatigue.
Self-motivation: Some participants found that trying to stay active through physical exercise provided them with the physical stimulation they needed to cope with fatigue. For instance, some participants noted that they got up whenever they felt tired and that they felt more motivated after getting up.
Sometimes, if I get tired, I try to get up and say to myself “Don’t give up”. [Participant 1, female]
Self-motivation and pushing themselves within limits worked for some of the participants. Such participants spoke of always pushing themselves slightly beyond their limit to build their stamina and overcome the disabling fatigue.
I noticed that the tiredness started when I walked for a while but tried to force myself to keep walking. It’s important to pay attention to my walking and not the fatigue. [Participant 3, female]
They felt that fatigue was a roadblock that they had to overcome by working through it and fighting it until they ultimately overcame it, by gradually pushing themselves physically and mentally.
Social participation: The participants also revealed that taking part in social activities that were engaging helped them physically deal with fatigue. A few participants found that social activities (such as spending time with friends and attending social gatherings) were helpful in reducing their fatigue symptoms.
When I go out with my family, the boredom and tiredness improve, and I feel more active. Staying at the hospital makes the time pass so slowly. [Participant 4, female]
I try to bring the groceries from the supermarket. Whenever I do this, I feel better and more energetic. Social gatherings also make me feel the same way. [Participant 2, female]
Some participants felt that social interactions involving physical and mental activities helped them shift their focus away from their fatigue and improved their stamina. They also felt that gradually trying to get back to their social tasks could speed up their recovery.
Thus, under this themes, the reported coping strategies varied from resting and taking breaks when required to pushing oneself to move and participate in social and other activities.
Theme 5: Perspectives About Support from Caregivers and Healthcare Practitioners
The responses under this theme were varied: some participants stated that they had received good support from healthcare practitioners (HCPs) and caregivers, while others said that they had not. These responses are described under the subthemes perceptions of support from HCPs and perceptions of support from caregivers.
Perceptions of support from HCPs: The responses under this subtheme were categorized as “lack of support”, “education and support”, and “support from physiotherapists”.
With regard to the category lack of support, most participants reported that they had not received any kind of support from HCPs to help them manage PSF. They explained that during their interactions with HCPs, PSF had never been discussed as an issue associated with post-stroke survival, and they had not received any education about PSF. The participants also mentioned that they had received inaccurate information about PSF from HCPs.
I have not received any education about fatigue from my doctor. I thought it was a normal feeling. If there were something [I could do] about it, they should have let me know. [Participant 8, male]
One participant reported feeling reluctant to discuss his symptoms of fatigue with his doctors, as they did not perceive it as part of his stroke recovery.
I have not discussed this issue [of tiredness] with my doctors or my physiotherapist. [Participant 6, male]
With regard to the category education and support, a few participants reported that they had received clear guidance, support, and information about management strategies during clinical consultations with their HCPs.
They told me in physiotherapy not to go beyond my tolerance [level] and to take frequent breaks. They also told me to walk as much as I could to be active. [Participant 8, male]
The doctors and the therapist said I have low endurance and my muscles are relaxed so we need to strengthen them. [Participant 3, female]
With regard to the category support from physiotherapists, some participants said that they did not see immediate benefits of the physiotherapy program. One participant mentioned that she felt bored and unmotivated during the physiotherapy sessions and that physiotherapy was not beneficial in terms of reducing her fatigue symptoms. Some patients reported that they were initially nervous about how they would cope with their fatigue during the rehabilitation sessions, but there was a strongly held belief among the participants that more physiotherapy sessions would improve their PSF. Other participants expressed that longer and more frequent physiotherapy sessions had helped reduce their fatigue-related symptoms. In contrast, other participants experienced deterioration in their fatigue following physiotherapy sessions. Several participants expressed dissatisfaction with the frequency and intensity of their physiotherapy sessions. One participant explained that she was receiving only one session per week, which she perceived as suboptimal.
Physical exercise reduces the tiredness and makes me feel much better [after my physiotherapy sessions]. [Participant 7, male]
At some points, it feels boring and tiring. It [physiotherapy] has been going on for a long time but with no improvement. [Participant 2, female]
Perceptions of support from families or caregivers: Two categories were generated here, namely, “encouragement” and “overprotectiveness”.
With regard to encouragement, some participants discussed how their families and relatives offered support and encouraged them to be active and independent and to complete their exercises so that they could improve their well-being and functioning.
My brothers, sister and especially my husband support me. They say, ‘You can do it. It’s easy. Look at that person.’ They show me examples. They also drive me to centers where I can do exercises. They tell me to walk as much as I can. Sometimes I sleep and they say, “No, get up and move”. [Participant 3, female]
With regard to overprotectiveness, some participants explained how their family encouraged them to avoid activities that could lead to physical exhaustion instead, in the belief that they were providing good support.
My family doesn’t want me to become tired, so they give me whatever I want. [Participant 8, male]
My daughter spoils me and doesn’t let me do anything all day. [Participant 1, female]
Thus, under this theme, the responses of the participants were varied, with some reporting a lack of support from caregivers or HCPs and other reporting that they had received support and information from HCPs and encouragement from family members.
Discussion
This study explores the perceptions and experiences of the various aspects of PSF among stroke survivors in Saudi Arabia and is the first such study to be conducted in this region. The data revealed a range of different perceptions and experiences of PSF that included physiological and psychological symptoms, as well as different beliefs about the causes of PSF, in terms of both physiological and psychological causes. Despite these variations, a consistent view expressed by the participants was that PSF had a negative impact on their daily life activities and social participation. The reported coping strategies for managing the symptoms of PSF included pacing, self-motivation, and social participation. A key finding that could have important clinical implications was that the participants generally felt that they had not received enough support from their physicians or caregivers. Moreover, the participants considered their healthcare providers and caregivers to be under-prepared for managing PSF. Further, the participants thought that their physiotherapists could have been more motivating, as receiving encouragement from their physiotherapists would have impacted their ability to engage in the exercise program.
The stoke survivors’ perception of PSF observed in this study was in line with the core features of PSF reported in a meta-analysis of twelve qualitative studies, which included easy fatiguability, lack of energy for ADLs, increased sensitivity to stress, and disturbed sleep.13 In contrast, a web-based thematic analysis6 found that stroke survivors’ perceptions of PSF were limited to physical tiredness and lack of energy. Despite this, it appears that most previous studies reported a range of physical and psychological symptoms, and the present findings confirm previous notions that PSF has a varied and complex presentation.
The perceived etiologies of PSF among our stroke survivors were different from those of similar qualitative studies in the literature. For instance, post-stroke survivors interviewed in Barbour and Mead’s qualitative study attributed PSF to stroke-related factors (eg, the stroke lesion) and hospital admission interventions, with poor sleep and boredom perceived as exacerbating factors.9 In another qualitative interview study,19 PSF was attributed to factors such as old age, medication, and poor health. In our study, the reported etiologies were varied and ranged from physiological and stroke-related factors to psychological factors, with some participants even indicating the PSF was an expected sequela of stroke. Although the exact mechanisms of PSF remain elusive, the main proposed predisposing factors and triggers include pre-existing brain lesions, neuroendocrine disorders, reduced physical activity, and passive coping strategies.20,21 The present patients also reported that reduced physical activity over their long treatment course may have contributed to PSF. However, the study did not consider the potential influence of pre-existing brain lesions or neuroendocrine. In the future, it might be beneficial to determine whether these factors affect PSF in post-stroke patients in Saudi Arabia, as this could help screen out patients who are likely to develop PSF and provide them with relevant information and coping strategies.
The patients’ reported impact of PFS on their ADLs was consistent with that of similar studies which reported how PSF affected patients’ abilities to engage in normal ADLs and social activities.11,14,22,23 Additionally, the impact of PSF on the ADLs of stroke survivors is compounded by massive loss of time, as they take time to complete physical activities.19 In our study, too, participants reported that they required a longer amount of time to complete tasks as compared to the pre-stroke phase. Thus, reducing the impact of PSF on ADLs should be the focus of interventions for stroke survivors to get back to their normal lives. The reported fatigue coping strategies by our participants were also similar to the self-management strategies reported in the literature, such as rest, flexibility and pacing of activities, adjusting priorities, self-motivation, and accepting help from others.9,11,19 To date, however, evidence-based data about effective self-management or interventional strategies for PSF are insufficient.
Our study revealed several interesting findings about stroke survivors’ perception of support from HCPs and families or caregivers. While some caregivers encouraged patients to increase their activity levels and become independent, others tended to overprotect their patients by discouraging physical activity, with the belief that it might harm the patients. This finding reflects a significant lack of knowledge among families and caregivers about how to deal with PSF. Moreover, it points to the need to provide stroke survivors and their caregivers with educational materials on PSF, especially information about aspects that can be worked into their daily routine such as exercise, sleep patterns, and avoiding drugs and excessive alcohol.5,24 Additionally, according to a scoping review of adaptation to PSF in stroke survivors and their care partners, HCPs need to train survivors and care partners about meeting their needs and provide information about adaptive therapies.25
With regard to support from HCPs, many participants reported that they had shared their physical and psychological experiences of PSF with their HCPs but had received no response, inaccurate data, inadequate answers, or only guidance about their physical symptoms. This finding is corroborated by previous qualitative studies.9–11,14 Importantly, according to the responses of our participants, psychological support was not considered a vital part of their PSF management by their healthcare providers. This trend has also been observed by other researchers, who reported that patients with PSF continued to have psychological and mental disturbances even after recovery from their physical symptoms.26–28 Thus, interventions for managing PSF need to prioritize patients’ psychological symptoms. For example, therapeutic cognitive behavioral interventions have been found to improve PFS,15,27 help patients engage in physical activities, and increase their ADLs. These findings point to the need for HCPs to recognize their roles and responsibilities in ensuring that patients with PSF receive the support and care that they need by paying attention to their complaints, communicating effectively, and helping patients understand the rationale behind PSF therapies. The participants in this study also expressed concern over the frequency of physiotherapy sessions and believed that more frequent sessions were likely to improve their symptoms. Accordingly, Zedlitz et al reported that gradual increments in exercise had a significant effect in reducing PSF.29 However, although various guidelines5,30,31 highlight the importance of engaging in physical activities and avoiding a sedentary lifestyle in improving PSF, there are no data about the type of exercises or frequency of physiotherapy sessions recommended for improving PSF. Some participants in this study mentioned that they did not feel motivated during the sessions. This observation has important implications, as patient motivation is important in shaping the outcomes of any treatment.32,33 Thus, the element of motivation is essential when designing interventions for managing PSF, and physiotherapists and caregivers must exert efforts to motivate their patients.32 Overall, given the observed interactions between biological, social (eg, family and caregivers care), and psychological factors in the present study, it might be useful to apply the biopsychosocial model for the management of PSF. This model was created in 1977 by George Engel, who believed that psychological and social factors contribute as much to a person’s medical condition as biological factors do.34 Based on this model, the experiences of PSF patients can be examined in three major contexts: biological (ie, pathophysiology), psychological (ie, fear, depression, anxiety, and behaviors such as coping mechanisms) and social environment contexts.34,35 To summarize, the results suggest that the treatment of PSF should be in alignment with the biopsychosocial model and needs to include multi-dimensional physiotherapy, occupational therapy, and psychotherapy.
The main strength of this study is the robust methodical and systematic approach that meets the criteria for the four indicators of trustworthiness, namely, credibility, transferability, dependability, and confirmability. To increase the credibility of this study, the primary researcher sought to engage participants and establish a rapport with them by informally interacting with them before the interviews. She also ensured that the participants completely understood the purpose and objectives of the study and the interview procedures by explaining these to each of the participants individually before the interviews. Transferability is the ability to generalize a researcher’s findings to the broader population on which it is based or to transfer the findings to another context, and reliability refers to the consistency of results over repeated assessments or in different contexts. To enhance the reliability of this study and the transferability of its findings, the research was planned and carried out after extensive discussions on its design, participant recruitment strategy, and data analysis with the researcher’s supervisory team. During the discussions, the suitability and practicality of all the available methods/strategies for participant recruitment and data analysis were examined, and the methods that were considered the best by the primary researcher on the basis of the aforementioned criteria were chosen for use in the study. The methods used to conduct this study make it easier to link this study’s findings to research on other populations. This enhances the external validity of this study. Further, the methods adopted in this study are easily transferable to research among communities that share similar socio-religious and healthcare attributes to those of Saudi Arabia. The confirmability of a research is established when a researcher’s interpretations and findings are derived only from the collected data and not from her own beliefs or any previous understanding of the subject matter. In this study, at every decision-making point, the reasons and arguments behind a decision were documented to justify it. In addition, the decisions made were based only on the findings to make sure that confirmability was ensured and the research was of high quality.
A significant limitation is that this study was carried out at only two rehabilitation centers in Saudi Arabia. However, the selected institutions are tertiary care centers that treat patients from all over the country, so the findings can be considered as representative of the nationwide population. Another major limitation was the small sample size. Further, a selection bias could not be completely avoided, as patients with aphasia and cognitive impairment were excluded, the interviews were conducted at the treating hospitals, and duration since stroke onset was similar in all the participants. Another potential limitation is that we did not screen the patients for depression, even though some patients exhibited symptoms of depression such as anhedonia and sleep disturbance. In addition, fatigue is considered as a sign of depression according to most scales. In fact, a couple of reviews on the topic have reported a significant association between PSF and emotional disturbances such as depression and anxiety.36,37 Despite depression and fatigue share some common features, they are not the same. Fatigue can increase the risk of developing depression, and it can also be a symptom of depression.38 However, a randomized controlled trial39 (RCT) by Choi-Kwon et al found that fluoxetine, a selective serotonin reuptake inhibitor (SSRI) antidepressant, effectively treats depression but not fatigue. This suggests that these two conditions are distinct entities. In the future, we could explore the potential association between PSF and depression and corresponding treatment strategies in this population.
Conclusion
Stroke survivors in Saudi Arabia have heterogeneous physical and psychological experiences of PSF and variable perceptions of its causes and its impact on their lives. Pacing activities, sleep, taking breaks, social support, and self-motivation are the main coping strategies reported. An important finding that emerged was that there was wide heterogeneity in the perceived support provided by HCPs and families or caregivers—ranging from lack of support to overprotectiveness. The patients’ perception of the role of physiotherapy and their attitudes towards physiotherapy sessions were also variable. Despite this, the general perception was that there were gaps in the provision of information about PSF and support for its management. Moreover, there is possibly excessive focus on the physical aspect of PSF and not enough consideration of the psychological component of PSF among HCPs. Considering the complex interactions of biological, social, and psychological factors in the onset and experience of PSF, there is a need for awareness and coping strategies that based on a biopsychosocial model of treatment management.
What the Study Has Added
Stroke survivors in Saudi Arabia have varied perceptions of post-stroke fatigue and were generally of the opinion that the support provided by caregivers and healthcare practitioners is inadequate. The findings imply that better educational and management tools that consider both the physical and psychological components of PSF are required. From this perspective, the biopsychosocial model would provide a suitable framework for devising strategies for the management of PSF.
Ethics Approval and Informed Consent
This study was approved by the Faculty of Medicine and Health Sciences Ethics Committee of the University of Nottingham (Ethics No. 2631603). Ethical approval was also obtained from King Fahad Medical City (IRB No. 00010471). The lead researcher received permission from the stroke unit directors at KFMC and SNAHC to access hospital registry records, select eligible participants, and obtain their contact information in order to invite them to face-to-face interviews. Written informed consent was obtained from all participants. All participants were given an information sheet to read and an informed consent form to sign in which they were assured that they were free to withdraw at any point and that their responses could be published in an anonymized fashion. Study complies with the Declaration of Helsinki.
Acknowledgments
We want to thank everyone who took part for their contributions. We also want to thank King Fahad Medical City Hospital and Sultan Bin Abdelaziz Humanitarian City Hospital for permitting us to conduct the research at their facilities. This work was supported by the Princess Nourah bint Abdulrahman University Researchers Supporting Project (grant number PNURSP2023R267), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Princess Nourah bint Abdulrahman University Researchers Supporting Project (grant number PNURSP2023R267), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia. This study is also part of the PhD scholarship fund from Princess Norah University at the University of Nottingham.
Disclosure
There are no conflicts of interest to declare.
References
1. Alghamdi I, Ariti C, Williams A, Wood E, Hewitt J. Prevalence of fatigue after stroke: a systematic review and meta-analysis. Eur Stroke J. 2021;6(4):319–332. doi:10.1177/23969873211047681
2. Al-Senani F, Al-Johani M, Salawati M, et al. An epidemiological model for first stroke in Saudi Arabia. J Stroke Cerebrovasc Dis. 2020;29(1):104465. doi:10.1016/j.jstrokecerebrovasdis.2019.104465
3. McKevitt C, Redfern J, Mold F, Wolfe C. Qualitative studies of stroke: a systematic review. Stroke. 2004;35(6):1499–1505. doi:10.1161/01.STR.0000127532.64840.36
4. Salter K, Hellings C, Foley N, Teasell R. The experience of living with stroke: a qualitative meta-synthesis. J Rehab Med. 2008;40(8):595–602. doi:10.2340/16501977-0238
5. Hinkle JL, Becker KJ, Kim JS, et al. Poststroke fatigue: emerging evidence and approaches to management: a scientific statement for healthcare professionals from the American Heart Association. Stroke. 2017;48(7):e159–e170. doi:10.1161/STR.0000000000000132
6. Thomas K, Gamlin C, de Simoni A, Mullis R, Mant J. How is poststroke fatigue understood by stroke survivors and carers? A thematic analysis of an online discussion forum. BMJ Open. 2019;9(7):e028958. doi:10.1136/BMJOPEN-2019-028958
7. Aali G, Drummond A, Das Nair R, Shokraneh F. Post-stroke fatigue: a scoping review. F1000Res. 2020;9:242. doi:10.12688/F1000RESEARCH.22880.2/DOI
8. Zhang S, Cheng S, Zhang Z, Wang C, Wang A, Zhu W. Related risk factors associated with post-stroke fatigue: a systematic review and meta-analysis. Neurol Sci. 2021;42(4):1463–1471. doi:10.1007/S10072-020-04633-W
9. Barbour VL, Mead GE. Fatigue after stroke: the patient’s perspective. Stroke Res Treat. 2012;2012:1–6. doi:10.1155/2012/863031
10. Kirkevold M, Christensen D, Andersen G, Johansen SP, Harder I. Fatigue after stroke: manifestations and strategies. Disabil Rehab. 2012;34(8):665–670. doi:10.3109/09638288.2011.615373
11. White JH, Gray KR, Magin P, et al. Exploring the experience of post-stroke fatigue in community dwelling stroke survivors: a prospective qualitative study. Disabil Rehab. 2012;34(16):1376–1384. doi:10.3109/09638288.2011.645111
12. Tremayne EJ, Freeman J, Coppola A. Stroke survivors’ experiences and perceptions of post-stroke fatigue education in the subacute phase of stroke. The FASE qualitative study. Br J Occup Ther. 2020;84(2):111–121. doi:10.1177/0308022620963741
13. Eilertsen G, Ormstad H, Kirkevold M. Experiences of poststroke fatigue: qualitative meta-synthesis. J Adv Nurs. 2013;69(3):514–525. doi:10.1111/JAN.12002
14. Flinn NA, Stube JE. Post-stroke fatigue: qualitative study of three focus groups. Occup Ther Int. 2010;17(2):81–91. doi:10.1002/OTI.286
15. Wu S, Mead G, Macleod M, Chalder T. Model of understanding fatigue after stroke. Stroke. 2015;46(3):893–898. doi:10.1161/STROKEAHA.114.006647
16. Su Y, Yuki M, Otsuki M. Non-pharmacological interventions for post-stroke fatigue: systematic review and network meta-analysis. J Clin Med. 2020;9(3):621. doi:10.3390/jcm9030621
17. Creswell JW, Poth CN. Qualitative inquiry and research design: choosing among five approaches. Available from: https://books.google.com.eg/books?hl=en&lr=&id=DLbBDQAAQBAJ&oi=fnd&pg=PP1&dq=+Creswell+JW.+Qualitative+inquiry+and+research+design:+choosing+among+five+approaches.+2nd+ed.+London:+Sage%3B+2007.&ots=-hn83gMRSw&sig=YZHny59H_F3xBhotuYkqwk6Pf8&redir_esc=y#v=onepage&q=Creswell%20JW.%20Qualitative%20inquiry%20and%20research%20design%3A%20choosing%20among%20five%20approaches.%202nd%20ed.%20London%3A%20Sage%3B%202007.&f=false.
18. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706QP063OA
19. Worthington E, Hawkins L, Lincoln N, Drummond A. The day-to-day experiences of people with fatigue after stroke: results from the Nottingham Fatigue After Stroke study. Int J Ther Rehabil. 2017;24(10):449–455. doi:10.12968/IJTR.2017.24.10.449
20. de Doncker W, Dantzer R, Ormstad H, Kuppuswamy A. Mechanisms of poststroke fatigue. J Neurol Neurosurg Psychiatry. 2018;89(3):287–293. doi:10.1136/JNNP-2017-316007
21. Paciaroni M, Acciarresi M. Poststroke Fatigue. Stroke. 2019;50(7):1927–1933. doi:10.1161/STROKEAHA.119.023552
22. Lerdal A, Bakken LN, Kouwenhoven SE, et al. Poststroke fatigue--a review. J Pain Symptom Manage. 2009;38(6):928–949. doi:10.1016/J.JPAINSYMMAN.2009.04.028
23. van de Port IGL, Wevers L, Roelse H, van Kats L, Lindeman E, Kwakkel G. Cost-effectiveness of a structured progressive task-oriented circuit class training programme to enhance walking competency after stroke: the protocol of the FIT-Stroke trial. BMC Neurol. 2009;9(1). doi:10.1186/1471-2377-9-43
24. Boddice G, Brauer S, Gustafsson L, Kenardy J, Hoffmann T. Clinical guidelines for stroke management 2010. National Stroke Foundation; 2010. Available from: https://espace.library.uq.edu.au/view/UQ:266895.
25. Teng CH, Phonyiam R, Davis LL, Anderson RA. Adaptation to poststroke fatigue in stroke survivors and their care partners: a scoping review. Disabil Rehab. 2023;45(13):2233–2247. doi:10.1080/09638288.2022.2084775
26. Cumming TB, Packer M, Kramer SF, English C. The prevalence of fatigue after stroke: a systematic review and meta-analysis. Int J Stroke. 2016;11(9):968–977. doi:10.1177/1747493016669861
27. Wu S, Chalder T, Anderson KE, Gillespie D, Macleod MR, Mead GE. Development of a psychological intervention for fatigue after stroke. PLoS One. 2017;12(8). doi:10.1371/JOURNAL.PONE.0183286
28. Wu S, Kutlubaev MA, Chun HYY, et al. Interventions for post-stroke fatigue. Cochrane Database Syst Rev. 2015;7(6). doi:10.1002/14651858.CD007030.PUB3
29. Zedlitz AMEE, Rietveld TCM, Geurts AC, Fasotti L. Cognitive and graded activity training can alleviate persistent fatigue after stroke: a randomized, controlled trial. Stroke. 2012;43(4):1046–1051. doi:10.1161/STROKEAHA.111.632117
30. Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(8):2532–2553. doi:10.1161/STR.0000000000000022
31. Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–e169. doi:10.1161/STR.0000000000000098
32. Maclean N, Pound P, Wolfe C, Rudd A. Qualitative analysis of stroke patients’ motivation for rehabilitation. BMJ. 2000;321(7268):1051–1054. doi:10.1136/BMJ.321.7268.1051
33. McNair R, Griffiths L, Reid K, Sloan H. Medical students developing confidence and patient centredness in diverse clinical settings: a longitudinal survey study. BMC Med Educ. 2016;16(1). doi:10.1186/S12909-016-0689-Y
34. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. doi:10.1037/0033-2909.133.4.581
35. Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehab. 2017;31(8):995–1004. doi:10.1177/0269215517709890
36. Ponchel A, Bombois S, Bordet R, Hénon H. Factors associated with poststroke fatigue: a systematic review. Stroke Res Treat. 2015;2015:347920. doi:10.1155/2015/347920
37. Acciarresi M, Bogousslavsky J, Paciaroni M. Post-stroke fatigue: epidemiology, clinical characteristics and treatment. Eur Neurol. 2014;72(5–6):255–261. doi:10.1159/000363763
38. Choi-Kwon S, Choi J, Kwon SU, Kang D-W, Kim JS. Fluoxetine is not effective in the treatment of poststroke fatigue: a double-blind, placebo-controlled study. Cerebrovasc Dis. 2007;23(2–3):103–108. doi:10.1159/000097045
39. English C, Simpson DB, Billinger SA, et al. A roadmap for research in post-stroke fatigue: consensus-based core recommendations from the third Stroke Recovery and Rehabilitation Roundtable. Neurorehabilit Neural Repair. 2023;15459683231209170. doi:10.1177/15459683231209170
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
