Back to Journals » Drug Design, Development and Therapy » Volume 16
Expanding the Clinical Use of CDK4/6 Inhibitors in the Treatment of Hormone Receptor-Positive, HER2-Negative Breast Cancer from Metastatic Setting to Adjuvant Setting
Authors Abdel-Razeq H , Sharaf B
Received 1 January 2022
Accepted for publication 4 March 2022
Published 16 March 2022 Volume 2022:16 Pages 727—735
DOI https://doi.org/10.2147/DDDT.S356757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Hikmat Abdel-Razeq,1,2 Baha’ Sharaf1
1Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan; 2School of Medicine, The University of Jordan, Amman, Jordan
Correspondence: Hikmat Abdel-Razeq, Department of Internal Medicine, King Hussein Cancer Center, Queen Rania Al Abdullah Street, P.O. Box: 1269, Amman, 11941, Jordan, Tel +962-6 5300460, Ext: 1000, Email [email protected]
Abstract: More than two-thirds of patients with breast cancer present with hormone receptor (HR)-positive, human epidermal growth factor receptor-2 (HER2)-negative disease at their initial diagnosis. HR-positive breast cancer’s growth depends on Cyclin D1, a direct transcriptional target of estrogen receptors (ER). The recent introduction of cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitors (palbociclib, ribociclib, and abemaciclib) has revolutionized the treatment of metastatic HR-positive, HER2-negative breast cancer in both endocrine-sensitive and endocrine-resistant settings and in both pre-and post-menopausal women. Multiple large randomized clinical trials had demonstrated improvement in progression-free survival (PFS) and, more recently, in overall survival (OS). Adjuvant endocrine therapy (ET) significantly reduces the risk of recurrence and death among patients with HR-positive early-stage breast cancer (EBC). However, up to 20% of these patients will experience local, regional or distal recurrences in the first ten years. Such resistance to ET motivated researchers to try CDK4/6 inhibitors in EBC, both in adjuvant and neoadjuvant settings. While many clinical trials are still ongoing, at least one study and two meta-analyses had shown beneficial results, based on which the US Food and Drug Administration had recently approved the use of one of these agents, abemaciclib, in combination with ET for the adjuvant therapy of patients with high-risk EBC. In this paper, we review the recently published and ongoing landmark clinical trials attempting to expand the use of CDK4/6 inhibitors, in combination with ET, in the adjuvant setting of EBC.
Keywords: CDK4/6 inhibitors, ribociclib, palbociclib, abemaciclib, early-stage breast cancer, adjuvant
Introduction
Globally, breast cancer is the most commonly diagnosed cancer among females.1–3 Despite successful efforts in early detection and the recent advances in therapeutic interventions, it remains a leading cause of cancer-related mortality in females.4 In 2020, an estimated 2.26 million new breast cancer cases were diagnosed, with over 675,000 related deaths worldwide.4
Seventy percent of all breast cancer patients present with hormone receptor (HR)-positive, human epidermal growth factor receptor-2 (HER2)-negative disease at their initial diagnosis.5–7 The HR-positive breast cancer growth depends on Cyclin D1, a direct transcriptional target of estrogen receptors (ER).8 Cyclin D1 activates Cyclin-Dependent Kinase (CDK) 4/6, resulting in G1-S phase transition and entry to the cell cycle.9,10 Resistance to ET is associated with continued dependence on Cyclin D1 and CDK 4/6.11
CDK4/6 inhibitors (palbociclib, ribociclib, and abemaciclib) have revolutionized the treatment of metastatic HR-positive, HER2-negative breast cancer, in both endocrine sensitive12–15 and endocrine-resistant settings,16–20 with nearly doubling of progression-free survival (PFS). Recently published data have shown significant improvement in overall survival (OS), too.21,22 Such dramatic improvements in treatment outcomes were seen in both premenopausal,23,24 and post-menopausal settings, and they appear to be independent of the ET partner.25 More recent studies have shown that the benefit of CDK4/6 inhibitors may extend to include patients with HER2-positive disease as well.26,27
Although adjuvant ET significantly reduces the risk of recurrence and death among patients with HR-positive early-stage breast cancer (EBC), some patients may experience recurrence; either locally or as metastatic disease.28 These concerns encourage clinicians and scientists to search for ways to improve treatment outcomes in the adjuvant setting, especially in high-risk patients.
This paper reviews the recently published and ongoing clinical trials attempting to introduce CDK4/6 inhibitors in treating HR-positive, HER2-negative EBC in the adjuvant setting.
CDK4/6 in Advanced Breast Cancer
The very first CDK4/6 inhibitor, palbociclib, was granted accelerated approval in 2015 for women with untreated metastatic hormone receptor positive, HER2 negative breast cancer, based on the results of a randomized Phase 2 study conducted in front line setting (PALOMA-1 trial).29
Palbociclib, ribociclib, and abemaciclib, the three available CDK4/6 inhibitors, were tried initially as a second line,16,17,30 then in the upfront treatment of metastatic breast cancer (mBC).13,23,30,31 Recently, the US Food and Drug Administration (FDA) performed a pooled analysis of seven phase-3 clinical trials that enrolled a total of 4200 patients using CDK4/6 inhibitors in the first-line setting with aromatase inhibitors (AI) or with fulvestrant in any setting. Among participants who received the CDK4/6 inhibitors in the frontline setting combined with an AI, median PFS improved by 13.1 months (HR, 0.55).32 The difference in median PFS was 7.4 months (HR, 0.56) for those who received a CDK4/6 inhibitor with fulvestrant, irrespective of the line of therapy. A PFS benefit is consistent irrespective of progesterone receptor (PR) status, the disease-free interval from adjuvant therapy (either more or less than 12 months), de novo metastatic disease, lobular histology, or bone-only metastases.32
Adverse Event Profile of CDK4/6 Inhibitors
Since the introduction of CDK4/6 inhibitors, clinicians have had to deal with many predictable adverse events (AEs); none impacted the wider adoption of these agents, even in heavily pretreated patients.
A recently published systematic review and meta-analysis of randomized controlled trials with 3685 patients addressed common AEs.33 This review showed a higher incidence of hematological toxicity (neutropenia, leukopenia, thrombocytopenia, and anemia), along with fatigue, diarrhea, nausea, and transaminitis, Table 1.
 |
Table 1 Common Adverse Events* |
Neutropenia is a class side effect of CDK4/6 inhibitors, and grade 3–4 neutropenia were very common in the PALOMA, MONALEESA, and MONARCH clinical trials, with an incidence of 65% in palbociclib, 58% with ribociclib and lowest with abemaciclib (22–27%). However, the rate of febrile neutropenia did not exceed 2% with any of the three agents, which is extremely low when compared with chemotherapy.34,35 The huge difference between chemotherapy and CDK4/6 inhibitors-associated neutropenia can be attributed to the difference in their mechanisms of action; CDK4/6 inhibitors induce cell cycle arrest without DNA damage or apoptosis of proliferating neutrophil precursor cells, as in chemotherapy, making neutrophil count recovery much quicker with CDK4/6 inhibitors, compared to chemotherapy.36 For the same reason, neutropenia with CDK4/6 inhibitors is managed by dose interruption and reduction, with no role for granulocyte colony-stimulating factor (G-CSF).
Diarrhea may occur with all three CDK4/6 inhibitors, but more frequently with abemaciclib, which is considered the most potent CDK4/6 inhibitor and is approximately five times more potent against CDK4 than CDK6, which may also explain the less hematological toxicity exerted by abemaciclib.37 In the MONARCH-2 trial, 13.4% of the patients on abemaciclib had Grade-3 diarrhea, which can be managed by increasing fluid intake and antimotility agents.18
Prolongation of the QTc interval, seen mainly with ribociclib, may lead to a type of ventricular tachycardia, known as torsades de pointes, resulting in ventricular fibrillation.38 In randomized ribociclib trials, QTc interval prolongation experienced by patients was reversible and managed by dose interruption and reduction, without any clinical consequences. Treatment with ribociclib is recommended only in patients with QTc < 450 msec. The use of ribociclib in patients at high risk for developing QTc prolongation and uncontrolled cardiac diseases must be avoided. Additionally, the concomitant use of ribociclib with medications known to prolong the QTc interval is strongly discouraged.39
Stomatitis, though not frequently encountered, it can be disturbing. In one meta-analysis study that involved a total of 2980 patients enrolled in 6 studies, the pooled relative risk (RR) of any-grade stomatitis was 2.02 (95% CI: 1.65–2.48). Higher RRs were observed among patients receiving letrozole (8.50, 95% CI: 2.22–32.57) or palbociclib-containing regimens (2.44, 95% CI: 1.88–3.18).40
CDK4/6 Inhibitors in Adjuvant Setting
The efficacy of CDK4/6 inhibitors in the adjuvant setting had been tested in 5 major clinical trials; 3 were recently published, one ribociclib trial (EarlEE-2) was held,41 while the fifth (NATALEE) remains ongoing.42
These trials evaluated the efficacy of CDK4/6 inhibitors in an almost similar setup, assessing the improvement in invasive disease-free survival (iDFS) in both pre- and post-menopausal women. However, the duration of therapy varied; ribociclib was given for 3 years in NATALEE,42 abemaciclib for 2 years in monarchE,43 palbociclib for 2 years in PALLAS, and 1 year in PENELOPE-B, Table 2.44,45
 |
Table 2 Summary of Adjuvant Clinical Trials |
Palbociclib Adjuvant Clinical Trials
Palbociclib had been tested in two clinical trials in two different settings. The first, the PALLAS trial, used palbociclib as an addition to the routinely used ET in regular adjuvant settings, while in the other trial, the PENELOPE-B, palbociclib was given following neoadjuvant chemotherapy and surgery to minimize the chance of recurrence in patients with residual disease.
The PALLAS was a Phase III open-label clinical trial designed to evaluate the potential efficacy of the CDK4/6 inhibitor, palbociclib, in the adjuvant setting of EBC. In this study, 5761 patients with HR-positive, HER2-negative stage II–III breast cancer were randomized, within one year from the diagnosis, and within 6 months of receiving adjuvant ET, to palbociclib 125 mg daily, 3 weeks on/1 week off for two years, in combination with adjuvant ET versus ET alone. The primary endpoint was iDFS in an intention to treat (ITT) analysis. After a median follow-up of 31 months, iDFS was not improved by adding palbociclib. The 4-year iDFS was 84.2% for palbociclib-containing arm versus 84.5% for ET alone arm (HR, 0.96, 95% confidence interval (CI) 0.81–1.14; P=0.65), crossing a pre-specified futility boundary.
The distant relapse-free survival (dRFS) was not different, either; 86.2% in patients who received ET plus palbociclib and 87.8% in patients treated with ET alone (HR, 1.05 (95% CI, 0.87 to 1.28). No specific subgroup seemed to benefit from the addition of palbociclib to ET.44 At an earlier interim analysis, the independent data monitoring committee recommended discontinuing palbociclib in patients still receiving it. The AEs within the palbociclib arm were a major issue, with two-thirds of patients developing grade-3 or 4 AEs. Compared to less than 10% in the control arm, early discontinuation of palbociclib was encountered in 44.9% of patients; majority were because of AEs.44,45
The PENELOPE-B trial was a double-blinded, randomized, phase-3 trial in which 1250 patients with HR-positive, HER2-negative early breast cancer with a residual invasive disease after taxanes-based neoadjuvant chemotherapy, and at high-risk of relapse were randomized to 1 year of palbociclib 125 mg daily, 3 weeks on/1 week off, plus standard ET versus standard ET with placebo for 1 year.
After a median follow-up of 42.8 months, the longest follow-up among all reported adjuvant and neoadjuvant CDK4/6 inhibitors trials, the palbociclib did not result in any improvement in iDFS over the placebo arm (HR, 0.93; 95% CI, 0.74–1.17; P=0.525), a finding that was consistent among all subgroups. One of the interesting observations in this trial was the early separation of iDFS curves at the 2 years and 3 years’ time points. Palbociclib seemed to add some benefit; however, these benefits disappeared by longer follow up, and the curves converged again. Similarly, the OS, one of the secondary endpoints, was not different between the two groups (HR, 0.87; 95% CI 0.61–1.22; P =0.420). There was no difference between both arms in the incidence of grade 3 or 4 non-hematological AEs; 19.9% versus 19.0%. In other serious AEs, 8 fatal cases were reported; 6 in the control arm and 2 in the experimental arm. As with other CDK4/6 inhibitors trials, palbociclib showed a lower incidence of menopausal symptoms, namely hot flushes and arthralgia, than ET alone. Only 20% discontinued palbociclib prematurely and did not complete the 13 cycles of treatment, while 42% did not complete 2 years of adjuvant palbociclib in the PALLAS trial.46
Abemaciclib Adjuvant Clinical Trials
Abemaciclib was also tried in the adjuvant therapy of patients with EBC. The monarchE trial was an open-label, Phase 3 study, in which 5637 patients with HR-positive, HER2-negative high-risk, and EBC were enrolled after they received the standard lines of treatment as indicated. Patients were randomized to receive abemaciclib 150 mg twice daily for 2 years plus standard adjuvant ET, or ET alone. The trial had 2 cohorts; cohort 1 included patients with 4 or more lymph nodes, or those with 1–3 lymph nodes and either tumor size ≥ 5 cm, or grade-3. The second cohort included patients with 1–3 lymph nodes, grade 1–2, and tumor size < 5 cm, but with Ki-67 ≥ 20%. The eligibility criteria came from the phase-3 GEICAM/ 990647 and GEICAM 2003–10 trials,48 which showed that patients with these features had the highest risk of early recurrence with adjuvant chemotherapy and AI. The primary endpoint was iDFS, and the secondary endpoints were dRFS, OS, and safety. Adding abemaciclib to standard ET resulted in significant improvement in iDFS (HR, 0.713; 95% CI 0.583–0.871; P=0.0009), with 2-year iDFS absolute difference 3.0% (92.3% and 89.3%). The abemaciclib-containing arm also showed superior dRFS with 3.0% absolute increment at 2 years; 93.8% vs 90.8% compared to ET alone. Higher rates of gastrointestinal and hematological AEs were encountered in the abemaciclib-containing arm, with dose reduction required in 41.2%, and 463 patients (16.6%) discontinued abemaciclib because of AEs.43
Additional follow-up analysis from monarchE was presented at the 2021 European Society of Medical Oncology (ESMO) annual meeting and was published recently. With a median follow-up of 27 months, and 90% of patients were off treatment, both iDFS (HR, 0.70, 95% CI 0.59–0.82; P<0.0001) and dRFS (HR, 0.69, 95% CI 0.57–0.83; P < 0.0001) benefits were maintained. Additionally, the absolute improvements in 3-year iDFS and dRFS rates were 5.4% and 4.2%, respectively. Abemaciclib benefit was observed regardless of the Ki-67 index.49 These results suggest that Ki-67 ≥ 20% could be utilized, together with other features such as nodal involvement, tumor size, and grade, to identify HR-positive, HER2-negative, EBC patients at higher risk of recurrence.
Ribociclib Adjuvant Clinical Trials
The ribociclib trial (NATALEE, NCT03701334) is a phase 3 multi-Center, randomized, open-label trial, using a lower dose of ribociclib (400 mg daily, 3 weeks on/1 week off), but for a longer duration (3 years). An estimated 4000 patients, both pre- and post-menopausal women and men aged ≥ 18 years, will be enrolled. Eligibility criteria include patients with anatomic stage III or stage II (with N1 or N0, with grade 2–3 and/or Ki67 ≥ 20%). The primary endpoint is iDFS while secondary endpoints include recurrence-free survival, dDFS, OS, patient-reported outcomes, and pharmacokinetics.42
Discussion
More than 80% of breast cancers are diagnosed with an early-stage disease, and most of these tumors are HR-positive and HER2-negative. So, the current treatment options under discussion involve most breast cancer patients.
Recent advances in adjuvant ET, including the use of AI; alone or in sequential following tamoxifen,28 extending the duration of ET beyond the 5 years,50–52 and ovarian function suppression,53,54 had clearly improved treatment outcomes of patients with EBC. However, despite these measures, around 20% of treated patients will have a recurrence, mostly in the form of an incurable metastatic disease.55 CDK4/6 inhibitors have changed the landscape of ET in patients with metastatic breast cancer. The clinical efficacy of the CDK4/6 inhibitors in the metastatic setting was almost the same, and the decision to use one drug or another depends largely on the toxicity profile, dosing schedule, physicians’ preference, or availability. However, as we illustrated, things might not be the same in EBC. The difference and the discordant results between the PALLAS and monarchE trials were surprising but can be explained. First, the monarchE trial used, in addition to the anatomic stage, biological characteristics of the tumor to define and enroll biologically higher-risk patients, including those with 4 or more lymph nodes or a mix of high anatomic and biologic risk (1–3 positive lymph nodes with grade-3 tumors, or with centrally assessed Ki-67 immunohistochemistry staining in ≥ 20% of tumor cells). Only 11.5% of patients in the monarchE trial were with stage IIa, while the majority (74.1%) had a stage-III disease, compared to 17.5% and 48.6%, respectively, in the PALLAS trial, Figure 1. Second, the treatment discontinuation rate was significantly higher in the PALLAS trial (44.9%) than in the monarchE trial (27.7%), and so was the dose reduction, Table 2. Third, though both the PALLAS and monarchE trials had almost the same number of study participants and the exact duration of treatment (2 years), follow-up was longer in the PALLAS trial, compared with monarchE; 23.7 months versus 19 months, respectively. More follow-up is needed to see if the benefit of abemaciclib will persist.
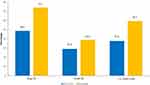 |
Figure 1 The PALLAS versus the MonarachE trial. More patients in the MonarachE trial had higher risk features including Stage-III, Grade-III and positive lymph nodes. |
The PENELOPE-B trial, which also tested palbociclib in the adjuvant setting, was negative, but it had two major differences; palbociclib was given for one year only, and eligibility criteria defined high-risk patients as those who had residual disease after standard neoadjuvant chemotherapy and had to have other high-risk clinical and pathologic features. This trial had the longest follow up ever for trials using CDK4/6 inhibitors in the adjuvant setting (42.8 months), and its negative results turn the focus again toward monarchE, whether the positive finding will vanish with longer follow up, as seen in the two palbociclib trials, or there may be something special in abemaciclib; being a more potent inhibitor, its continuous administration without a week off, or its known unique single-agent efficacy.19 However, looking at the Kaplan-Meier curves, it is interesting to note the early separation of curves such that, at the 2-year and 3-year time points, palbociclib seems to add some benefit similar to what has been seen in the monarchE trial. However, this apparent early separation of the curves disappeared with longer follow-up.
The fourth adjuvant trial, the NATALEE trial, tested ribociclib for a longer duration (3 years), but the patient enrolled in this trial, based on eligibility criteria, were considered intermediate risk compared to both the PALLAS and monarchE trials. Hopefully, the trial result will give us a clear idea of whether there is a difference between the 3 CDK4/6 inhibitors and whether the longer duration of treatment is beneficial.
To further address the role of CDK4/6 inhibitors in the adjuvant setting of HR-positive, HER2-negative early breast cancer, a recently published systematic review and meta-analysis included the three published studies that enrolled 12,647 patients, showed that the addition of CDK4/6 inhibitors to ET resulted in a trend for a benefit in iDFS (HR, 0.85, 95% CI 0.71–1.01; P=0.071). However, the analysis showed no significant improvement in dRFS (HR, 0.83, 95% CI 0.58–1.19; P=0.311). As expected, discontinuation of treatment and the risk of all-grade toxicities were significantly higher in the combination arm (OR 22.11, 95% CI 9.45–51.69, P < 0.001) and (OR 9.36, 95% CI 3.46–25.33, P < 0.001), respectively.56
Another, more recently-published meta-analysis of the three published trials by Gao et al showed that the combination of CDK4/6 inhibitors and ET in the adjuvant setting prolonged iDFS in patients with HR-positive, HER2-negative early breast cancer (HR 0.87, 95% CI, 0.76=0.98, P=0.03). The advantage was more evident in patients with N2/N3 nodal status (HR 0.83, 95% CI 0.71–0.97, P=0.02), while menopausal status and prior adjuvant or neoadjuvant chemotherapy had no impact on treatment outcomes. Additionally, rates of grade 3/4 AEs were significantly higher with the combination therapy (RR 4.14, 95% CI 3.33–5.15, p<0.00001) with significantly higher treatment discontinuation rate due to AEs (RR 19.16, 95% CI 9.27–39.61, p < 0.00001).57
Based on the above data, the US FDA granted, in October 2021, the first approval for a CDK4/6 inhibitor (abemaciclib) in combination with ET for the adjuvant treatment of HR-positive, HER2-negative EBC. The approval, however, was restricted for patients at higher risk for recurrence; those with node-positive and those with a Ki-67 score ≥ 20%.58
Conclusions
CDK4/6 inhibitors have revolutionized the treatment of HR-positive, HER-negative metastatic breast cancer. However, their introduction for EBC in combination with ET in the adjuvant setting was not as smooth, as clinical trials reached conflicting results. At least one CDK4/6 inhibitor, abemaciclib, was recently approved by the US FDA for higher-risk patients. Further studies examining inherited differences among available CDK4/6 inhibitors, longer follow-up, and selecting higher risk patients based on anatomical and biological criteria may clarify their potential benefit.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, took part in drafting, revising and critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel R, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Lei S, Zheng R, Zhang S, et al. Global patterns of breast cancer incidence and mortality: a population‐based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021;41(11):1183–1194. doi:10.1002/cac2.12207
3. Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer. 2021;149(4):778–789. doi:10.1002/ijc.33588
4. Luo C, Li N, Lu B, et al. Global and regional trends in incidence and mortality of female breast cancer and associated factors at national level in 2000 to 2019. Chin Med J. 2021;135(1):42–51. doi:10.1097/cm9.0000000000001814
5. Howlader N, Altekruse S, Li C, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5):dju055. doi:10.1093/jnci/dju055
6. Ayyagari R, Tang D, Patterson-Lomba O, et al. Progression-free survival with endocrine-based therapies following progression on non-steroidal aromatase inhibitor among post-menopausal women with hormone receptor positive, human epidermal growth factor receptor-2 negative metastatic breast cancer: a network meta-analysis. Curr Med Res Opin. 2018;34(9):1645–1652. doi:10.1080/03007995.2018.1479246
7. Messina C, Cattrini C, Buzzatti G, et al. CDK4/6 inhibitors in advanced hormone receptor-positive/HER2-negative breast cancer: a systematic review and meta-analysis of randomized trials. Breast Cancer Res Treat. 2018;172(1):9–21. doi:10.1007/s10549-018-4901-0
8. Altucci L, Addeo R, Cicatiello L, et al. 17 beta-Estradiol induces cyclin D1 gene transcription, p36D1-p34cdk4 complex activation and p105Rb phosphorylation during mitogenic stimulation of G (1)-arrested human breast cancer cells. Oncogene. 1996;12(11):2315–2324.
9. Oki T, Nishimura K, Kitaura J, et al. A novel cell-cycle-indicator, mVenus-p27K−, identifies quiescent cells and visualizes G0–G1 transition. Sci Rep. 2014;4:4012. doi:10.1038/srep04012
10. Schwartz G, Shah M. Targeting the cell cycle: a new approach to cancer therapy. J Clin Oncol. 2005;23(36):9408–9421. doi:10.1200/jco.2005.01.5594
11. Guo Q, Lin X, Ye L, et al. Comparative efficacy of CDK4/6 inhibitors plus aromatase inhibitors versus fulvestrant for the first-line treatment of hormone receptor-positive advanced breast cancer: a network meta-analysis. Target Oncol. 2019;14(2):139–148. doi:10.1007/s11523-019-00633-9
12. Finn RS, Martin M, Rugo HS, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–1936. doi:10.1056/NEJMoa1607303
13. Goetz M, Toi M, Campone M, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–3646. doi:10.1200/jco.2017.75.6155
14. Hortobagyi G, Stemmer S, Burris H, et al. Breast cancer, locally advanced and metastatic first-line ribociclib + letrozole for post-menopausal women with hormone receptor-positive (HR+), HER2-negative (HER2–), advanced breast cancer (ABC). Ann Oncol. 2016;27:vi553. doi:10.1093/annonc/mdw435.03
15. Rugo H, Finn R, Diéras V, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res Treat. 2019;174(3):719–729. doi:10.1007/s10549-018-05125-4
16. Cristofanilli M, Turner N, Bondarenko I, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–439. doi:10.1016/s1470-2045(15)00613-0
17. Turner N, Slamon D, Ro J, et al. Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med. 2018;379(20):1926–1936. doi:10.1056/nejmoa1810527
18. Sledge G, Toi M, Neven P, et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875–2884. doi:10.1200/jco.2017.73.7585
19. Dickler M, Tolaney S, Rugo H, et al. MONARCH 1, A Phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR+/HER2− metastatic breast cancer. Clin Cancer Re. 2017;23(17):5218–5224. doi:10.1158/1078-0432.ccr-17-0754
20. Slamon D, Neven P, Chia S, et al. Overall survival with ribociclib plus fulvestrant in advanced breast cancer. N Engl J Med. 2020;382(6):514–524. doi:10.1056/nejmoa1911149
21. Im S, Lu Y, Bardia A, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381(4):307–316. doi:10.1056/nejmoa1903765
22. Sledge G, Toi M, Neven P, et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor–positive, ERBB2-negative breast cancer that progressed on endocrine therapy—MONARCH 2. JAMA Oncol. 2020;6(1):116. doi:10.1001/jamaoncol.2019.4782
23. Tripathy D, Im S, Colleoni M, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. Lancet Oncol. 2018;19(7):904–915. doi:10.1016/s1470-2045(18)30292-4
24. Neven P, Rugo H, Tolaney S, et al. Abemaciclib plus fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer in premenopausal women: subgroup analysis from the MONARCH 2 trial. Breast Cancer Res. 2021;23(1). doi:10.1186/s13058-021-01463-2
25. Llombart-Cussac A, Pérez-García J, Bellet M, et al. PARSIFAL: a randomized, multi-center, open-label, phase II trial to evaluate palbociclib in combination with fulvestrant or letrozole in endocrine-sensitive patients with estrogen receptor (ER)[+]/HER2[-] metastatic breast cancer. J Clin Oncol. 2020;38(15_suppl):1007. doi:10.1200/jco.2020.38.15_suppl.1007
26. Tolaney S, Wardley A, Zambelli S, et al. Abemaciclib plus trastuzumab with or without fulvestrant versus trastuzumab plus standard-of-care chemotherapy in women with hormone receptor-positive, HER2-positive advanced breast cancer (monarcHER): a randomised, open-label, phase 2 trial. Lancet Oncol. 2020;21(6):763–775. doi:10.1016/s1470-2045(20)30112-1
27. O’Sullivan C, Suman V, Goetz M. The emerging role of CDK4/6i in HER2-positive breast cancer. Ther Adv Med Oncol. 2019;11:175883591988766. doi:10.1177/1758835919887665
28. Early Breast Cancer Trialists’ Collaborative Group. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386(10001):1341–1352. doi:10.1016/S0140-6736(15)61074-1
29. Finn RS, Crown JP, Lang I, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16(1):25–35. doi:10.1016/S1470-2045(14)71159-3
30. Slamon D, Neven P, Chia S, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor–positive, human epidermal growth factor receptor 2–negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018;36(24):2465–2472. doi:10.1200/jco.2018.78.9909
31. Im S, Mukai H, Park I, et al. Palbociclib plus letrozole as first-line therapy in post-menopausal Asian women with metastatic breast cancer: results from the Phase III, randomized PALOMA-2 study. J Glob Oncol. 2019;5(5):1–19. doi:10.1200/jgo.18.00173
32. Gao J, Cheng J, Bloomquist E, et al. CDK4/6 inhibitor treatment for patients with hormone receptor-positive, HER2-negative, advanced or metastatic breast cancer: a US Food and Drug Administration pooled analysis. Lancet Oncol. 2020;21(2):250–260. doi:10.1016/s1470-2045(19)30804-6
33. Yang L, Xue J, Yang Z, et al. Side effects of CDK4/6 inhibitors in the treatment of HR+/HER2− advanced breast cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med. 2021;10(5):5590–5599. doi:10.21037/apm-21-1096
34. Andersson M, Lidbrink E, Bjerre K, et al. Phase III randomized study comparing docetaxel plus trastuzumab with vinorelbine plus trastuzumab as first-line therapy of metastatic or locally advanced human epidermal growth factor receptor 2–positive breast cancer: the HERNATA study. J Clin Oncol. 2011;29(3):264–271. doi:10.1200/jco.2010.30.8213
35. Sammons S, Topping D, Blackwell K. HR+, HER2– advanced breast cancer and CDK4/6 inhibitors: mode of action, clinical activity, and safety profiles. Curr Cancer Drug Targets. 2017;17(7):637–649. doi:10.2174/1568009617666170330120452
36. Hu W, Sung T, Jessen B, et al. Mechanistic investigation of bone marrow suppression associated with palbociclib and its differentiation from cytotoxic chemotherapies. Clin Cancer Res. 2015;22(8):2000–2008. doi:10.1158/1078-0432.ccr-15-1421
37. Braal CL, Jongbloed EM, Wilting SM, Mathijssen RHJ, Koolen SLW, Jager A. Inhibiting CDK4/6 in breast cancer with palbociclib, ribociclib, and abemaciclib: similarities and differences. Drugs. 2021;81(3):317–331. doi:10.1007/s40265-020-01461-2
38. Chandrasekhar S, Fradley M. QT Interval prolongation associated with cytotoxic and targeted cancer therapeutics. Curr Treat Options Oncol. 2019;20(7). doi:10.1007/s11864-019-0657-y
39. Coppola C, Rienzo A, Piscopo G, Barbieri A, Arra C, Maurea N. Management of QT prolongation induced by anti-cancer drugs: target therapy and old agents. Different algorithms for different drugs. Cancer Treat Rev. 2018;63:135–143. doi:10.1016/j.ctrv.2017.11.009
40. Long Q, Li X, Wu G, Zhang J, Li H. Oral adverse effects of CDK4/6 inhibitors among breast cancer patients: a systematic review and meta-analysis. Ann Palliat Med. 2021;10(6):6556–6563. doi:10.21037/apm-21-1156
41. O’Shaughnessy J, Alba E, Bardia A, et al. EarLEE-2: a phase 3 study of ribociclib + endocrine therapy (ET) for adjuvant treatment of patients with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–), intermediate-risk, early breast cancer (EBC) [abstract]. Cancer Res. 2018;78(4Suppl):
42. A Phase III multi-center, randomized, open-label trial to evaluate efficacy and safety of ribociclib with endocrine therapy as an adjuvant treatment in patients with hormone receptor-positive, HER2-negative early breast cancer (new adjuvant trial with ribociclib [LEE011]: NATALEE). Available from: https://clinicaltrials.gov/ct2/show/NCT03701334.
43. Johnston S, Harbeck N, Hegg R, et al. Abemaciclib combined with endocrine therapy for the adjuvant treatment of HR+, HER2−, node-positive, high-risk, early breast cancer (monarchE). J Clin Oncol. 2020;38(34):3987–3998. doi:10.1200/jco.20.02514
44. Gnant M, Dueck AC, Frantal S, et al. Adjuvant palbociclib for early breast cancer: the PALLAS trial results (ABCSG-42/AFT-05/BIG-14-03). J Clin Oncol. 2021–2022;40(3):282–293. doi:10.1200/JCO.21.02554
45. Mayer E, Demichele A, Pfeiler G, et al. PALLAS: PALbociclib CoLlaborative adjuvant study: a randomized phase 3 trial of palbociclib with standard adjuvant endocrine therapy versus standard adjuvant endocrine therapy alone for HR+/HER2- early breast cancer. Ann Oncol. 2017;28:v66. doi:10.1093/annonc/mdx362.064
46. Loibl S, Marmé F, Martin M, et al. Palbociclib for residual high-risk invasive HR-positive and HER2-negative early breast cancer-the Penelope-B trial. J Clin Oncol. 2021;39(14):1518–1530. doi:10.1200/jco.20.03639
47. Martin M, Brase J, Ruiz A, et al. Prognostic ability of EndoPredict compared to research-based versions of the PAM50 risk of recurrence (ROR) scores in node-positive, estrogen receptor-positive, and HER2-negative breast cancer. A GEICAM/9906 sub-study. Breast Cancer Res Treat. 2016;156(1):81–89. doi:10.1007/s10549-016-3725-z
48. Martín M, Ruiz Simón A, Ruiz Borrego M, et al. Epirubicin plus cyclophosphamide followed by docetaxel versus epirubicin plus docetaxel followed by capecitabine as adjuvant therapy for node-positive early breast cancer: results from the GEICAM/2003-10 study. J Clin Oncol. 2015;33(32):3788–3795. doi:10.1200/jco.2015.61.9510
49. Harbeck N, Rastogi P, Martin M, et al. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: updated efficacy and Ki-67 analysis from the monarchE study. Ann Oncol. 2021;32(12):1571–1581. doi:10.1016/j.annonc.2021.09.015
50. van Hellemond I, Geurts S, Tjan-Heijnen V. Current status of extended adjuvant endocrine therapy in early-stage breast cancer. Curr Treat Options Oncol. 2018;19(5):26. doi:10.1007/s11864-018-0541-1
51. Blok E, Kroep J, Meershoek-Klein Kranenbarg E, et al. Optimal duration of extended adjuvant endocrine therapy for early breast cancer; results of the IDEAL trial (BOOG 2006-05). J Natl Cancer Inst. 2017;110(1):40–48. doi:10.1093/jnci/djx134
52. Tjan-Heijnen V, van Hellemond I, Peer P, et al. Extended adjuvant aromatase inhibition after sequential endocrine therapy (DATA): a randomised, phase 3 trial. Lancet Oncol. 2017;18(11):1502–1511. doi:10.1016/S1470-2045(17)30600-9
53. Perrone F, De Laurentiis M, De Placido S, et al. Adjuvant zoledronic acid and letrozole plus ovarian function suppression in premenopausal breast cancer: HOBOE phase 3 randomised trial. Eur J Cancer. 2019;118:178–186. doi:10.1016/j.ejca.2019.05.004
54. Pagani O, Francis P, Fleming G, et al. Absolute improvements in freedom from distant recurrence to tailor adjuvant endocrine therapies for premenopausal women: results from TEXT and SOFT. J Clin Oncol. 2020;38(12):1293–1303. doi:10.1200/jco.18.01967
55. Colleoni M, Sun Z, Price K, et al. Annual hazard rates of recurrence for breast cancer during 24 years of follow-up: results from the International Breast Cancer Study Group trials I to V. J Clin Oncol. 2016;34(9):927–935. doi:10.1200/jco.2015.62.3504
56. Agostinetto E, Vian L, Caparica R, et al. CDK4/6 inhibitors as adjuvant treatment for hormone receptor-positive, HER2-negative early breast cancer: a systematic review and meta-analysis. ESMO Open. 2021;6(2):100091. doi:10.1016/j.esmoop.2021.100091
57. Gao H, Lin Y, Zhu T, et al. Adjuvant CDK4/6 inhibitors combined with endocrine therapy in HR-positive, HER2-negative early breast cancer: a meta-analysis of randomized clinical trials. Breast. 2021;59:165–175. doi:10.1016/j.breast.2021.07.002
58. US Food and Drug Administration. FDA approves abemaciclib with endocrine therapy for early breast cancer; 2021. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-abemaciclib-endocrine-therapy-early-breast-cancer.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
