Back to Journals » Patient Preference and Adherence » Volume 17
Examining Influenza Vaccination Patterns Among Young Adults with Asthma: Insights into Knowledge, Attitudes, and Practices
Authors Al-Qerem W , Alassi A, Jarab A, Al Bawab AQ, Hammad A , Alasmari F, Alazab B , Abu Husein D, AL Momani N, Eberhardt J
Received 14 September 2023
Accepted for publication 4 November 2023
Published 10 November 2023 Volume 2023:17 Pages 2899—2913
DOI https://doi.org/10.2147/PPA.S436622
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Johnny Chen
Walid Al-Qerem,1 Ameen Alassi,1 Anan Jarab,2,3 Abdel Qader Al Bawab,1 Alaa Hammad,1 Fawaz Alasmari,4 Badi’ah Alazab,1 Daoud Abu Husein,1 Nadeen AL Momani,3 Judith Eberhardt5
1Department of Pharmacy, Faculty of Pharmacy, Al-Zaytoonah University of Jordan, Amman, 11733, Jordan; 2College of Pharmacy, Al Ain University, Abu Dhabi, United Arab Emirates; 3Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 4Department of Pharmacology and Toxicology, College of Pharmacy, King Saud University, Riyadh, 12372, Saudi Arabia; 5School of Social Sciences, Humanities and Law, Department of Psychology, Teesside University, Middlesbrough, TS1 3BX, UK
Correspondence: Walid Al-Qerem, Department of Pharmacy, Faculty of Pharmacy, Al-Zaytoonah University of Jordan, Amman, 11733, Jordan, Tel +962777209601, Fax +96264291432, Email [email protected]
Purpose: Asthma is a major chronic disease of all ages, globally. Exacerbations are a significant problem for asthmatic patients. Despite advances in asthma management and efforts to identify asthma triggers, viral infections of the respiratory tract remain the most frequent triggers of asthma exacerbations. This study explored knowledge, attitudes, and practices (KAP) of asthmatic patients towards receiving the influenza vaccine.
Patients and Methods: This cross-sectional study enrolled 397 adult asthmatic patients visiting the outpatient respiratory clinics of three Jordanian medical facilities.
Results: The research included 66.4% females, with a median age of 32 years. The results showed that 42.4% of enrolled asthmatics had never received the flu vaccine and only 51.1% reported that they intended to take the vaccine in the current year. Most of those who had been vaccinated at least once in their lifetime reported that the side effects were mild (61.8%). Variables that decreased refusal/hesitancy towards receiving the flu vaccine in the current year included having well-controlled asthma (RRR = 0.193, 95% Cl (0.053– 0.698), p =0.012), and high knowledge about asthma and flu (RRR= 0.916, 95% Cl (0.847– 0.990), p =0.028, respectively).
Conclusion: A small number of the participants adhered to vaccinating against the flu which is due to lack of knowledge about the asthma, flu, and the vaccine. To address this challenge, we propose targeted health education campaigns, collaboration with healthcare providers, and utilization of digital platforms.
Keywords: asthma, exacerbation, influenza, influenza vaccine, morbidity
Introduction
Asthma is defined by Global Initiative for Asthma (GINA) as chronic airway inflammation that is accompanied by cough, wheezing, chest tightness, and breathlessness.1 Asthma is the most common chronic respiratory disease in people of all ages with number asthmatics is predicted to increase considerably as a result of several environmental risk factors.2 In Jordan, the prevalence of physician-diagnosed asthma ranges between 8.8% and 9.5%. In 2016, asthma prevalence was estimated to reach 12.3% among the Jordanian population in general.3
Exacerbation is a major component of asthma, which is defined by the most recent (2022) Global Initiative for Asthma (GINA) guidelines as “an acute or subacute worsening in symptoms and lung function from the patient’s usual status, occasionally it may be the initial presentation of asthma”.1
Upper respiratory tract viral infections are the most predominant triggers of acute severe asthma exacerbation. During the influenza pandemic of 2009, asthma was associated with an increased risk of hospitalization.4 Individuals who have asthma face an elevated likelihood of experiencing complications due to influenza. Infection with the influenza virus can potentially trigger asthma attacks, worsen asthma symptoms, and even result in pneumonia.5 Asthma imposes a significant economic burden on healthcare systems. In Jordan, the total cost of treatment-related problems due to asthma was estimated to be USD 1550 per patient.6 Another study conducted in the United States revealed that the annual direct medical costs were significantly associated with asthma severity ($3305 in mild, $7250 in moderate, and $9175 in severe asthma), while the indirect costs were $106 in mild, $321 in moderate, and $1000 in severe per person per year.7
According to the latest data published by WHO in 2020, influenza and pneumonia caused 3.59% of the total deaths in Jordan.8 Fortunately, influenza is a vaccine-preventable disease. The Centers for Disease Control and Prevention (CDC) recommends that all people aged six months and older be vaccinated against flu every year starting from September until the end of October, before the usual period of seasonal influenza in order to protect from influenza complications.5 In addition, GINA recommends that all people with asthma should be vaccinated against influenza annually.1 Although vaccination against influenza may have serious complications such as myocarditis and pericarditis,9 the benefit of receiving the vaccine outweigh the risks, particularly among high-risk populations including those with asthma,9 the benefit/risk ratio remains in favor of vaccination, particularly among high-risk populations.
Several factors place asthmatic patients in the high-risk group for developing complications from influenza infection including chronic airway inflammation, and weakened responses of innate immune cells including T-helper 1 cell and interferon-β, which play a critical role in inhibiting viral infections in the respiratory tract, leading to severe influenza infection, worsening of asthma symptoms and increased risk of developing pneumonia.4,10 As asthma increases the risk of severe influenza infection, vaccination of this group should be a priority. Nevertheless, the vaccination rate of asthmatics against influenza is only 40% and, unlike other high-risk groups, has failed to increase in recent years.11,12
Multiple studies have investigated the causes of low influenza vaccine coverage among high-risk groups. The lack of recommendations from physicians, prior adverse vaccine experiences, and misconceptions about the vaccine appear to be the most relevant factors associated with vaccine hesitancy.13 In general, studies examining predictors of influenza vaccine acceptance among both high-risk and at-risk populations underscore the importance of knowledge, beliefs, and attitudes.13,14
Numerous studies have explored perceptions of the flu vaccine among asthmatic children in Saudi Arabia,15 Jordan,16 and the UK.17 However, to the best of our knowledge, no prior research has been conducted among asthmatic adults in the Middle East. The current study represents a pioneering effort to examine the knowledge of adults with asthma regarding asthma, influenza and its vaccine, their adherence to practices that improve asthma control and their attitudes and practices towards vaccinating against influenza, and evaluate the variables associated with their intention to receive the influenza vaccine in the current year. Findings may help healthcare providers develop health campaigns to increase vaccination against influenza among asthmatics and thereby improve asthma control.
Materials and Methods
Methodology
This is a multicentered study that enrolled asthmatic adults who were attending outpatient respiratory clinics at two large Jordanian hospitals and one polyclinic; AlBashir Hospital which is located in the capital Amman and serves huge numbers of patients from different areas, King Abdullah University Hospital which is located in northern city of Irbid and serves patients from the north governorates of Jordan, and the First Health Center of Petra which is located in the outskirts of Zarqa the second most populated city in Jordan, in the period between December 2022 and May 2023. Inclusion criteria included adults 18 years or older who had been diagnosed with asthma based on the GINA guidelines and were willing to take part in the study.1 The participants were approached by the research pharmacist and provided with a brief description of the aims of the study. Asthma patients were informed about confidentiality, anonymity of the obtained data and voluntary participation, and an informed consent form was signed by all participants. The study was conducted according to the ethical principles of the Declaration of Helsinki. Ethical approval was obtained from Al-Zaytoonah University of Jordan (Ref#22/23/2020–2021), Jordan University of Science and Technology (Ref#2021/07) and Ministry of Health in Jordan (Ref#MOH/REC/2023/119).
Tool Validation
Content validity was assessed by an expert panel that included an infectious disease professional, a pulmonologist, and a clinical pharmacist. The questionnaire was originally written in English after an extensive literature review, and then translated-back translated from English to Arabic, since it is the mother language of Jordan. The translation was conducted by two linguistic experts and the two versions were comparable. A pilot study including 30 asthmatics was conducted to ensure the questionnaire’s clarity and intelligibility for the Jordanian participants. The data from the pilot study were excluded from the final analysis. To ensure the reliability of the results Cronbach’s alphas were calculated for each latent variable (knowledge about asthma, influenza and its vaccine, attitudes towards the influenza vaccine, and adherence to practices that improve asthma control).
Data Collection and Study Instruments
The data was collected using a custom-designed questionnaire using Google Forms. This questionnaire had been developed after an extensive literature review,18,19 translated into Arabic, and validated using a forward-back translation by two independent translators. The survey questionnaire was based on previously published studies by Al-Qerem et al that evaluated parental acceptance of the COVID-19 vaccine,20 after performing the necessary modifications for it to be suitable for the influenza vaccine among asthmatic adults. The questionnaire consisted of five parts. The first part included the demographic and medical profile of the patient including age, gender, educational level, marital status, socioeconomic status, smoking, exposure to passive smoking, asthma duration, and previous hospitalization due to asthma in the past year. The second part included the asthma symptom control (ASC)21 measure which consisted of four questions. One point was granted for each ‘yes’ answer, with a higher score indicating a lower score in asthma control. Participants were categorized as follows: well-controlled if they scored zero, partially controlled if they scored 1–2, and uncontrolled if their score exceeded two out of a maximum of four points. The third part assessed patients’ knowledge about asthma, influenza, and the influenza vaccine, with each correct answer in this section being granted one point and zero points being given for incorrect answers. The total score was determined by adding up all the points, with a maximum possible score of 27. A higher score denoted a greater level of knowledge.
The fourth part of the questionnaire evaluated patients’ attitudes toward vaccinating against influenza and included a Likert-style response scale (strongly agree, agree, neutral, disagree, or strongly disagree), ranging from five points for “strongly agree” to one point for “strongly disagree”. Reverse scoring was used for the negatively worded question. The total score for each item was calculated by summing the points, with a maximum possible score of 40. A higher score indicated a more favorable attitude towards the influenza vaccine. The fifth part assessed patients’ practices to control asthma in addition to any prior vaccine-related side effects, the severity of these side effects, and their intention to receive the flu vaccine in the current year. The asthma practices scale included a Likert-style response format ranging from 5 for “always” to 1 for “never”. The total score for each practice was computed by adding up the points, with a maximum achievable score of 55. A higher score reflected a greater commitment to asthma management practices. The final part addressed barriers encountered by respondents who stated that they did not receive the vaccine annually or that they had no intention to receive the influenza vaccine in the current year or were not sure about their vaccination plans. (See Appendix 1)
Sample Size Calculation
A convenience sampling technique was utilized based on a 50% population proportion, 95% significance level and a 5% margin of error to calculate the minimum required sample size, which was 385 participants. The current study included 397 patients.22
Statistical Analysis
SPSS version 28.0 was used to analyze the data. To assess the normality of the continuous variables, Q-Q plots and Kolmogorov–Smirnov test were applied. Therefore, continuous variables were presented as median and 95% CI, while categorical variables were presented as frequencies and percentages. To identify variable associations with the intention to receive the influenza vaccine in the current year, bivariate analyses using Chi-square and Kruskal–Wallis were performed, and a multinomial logistic regression model was built to conduct multivariate analysis. The independent variables included in the model were variables that had p values less than 0.2 in the bivariate analysis. The significance level was determined at p <0.05.
Results
Descriptive Statistics
The total enrolled sample in the present study consisted of 397 asthmatic adults (66.4% were females) with a median age of 32 (ranging from 30 to 34) years. The majority of the patients (72.9%) were married and 55.1% of the study sample fell into the high-income group, earning more than 1000 JDs/month (1400USD). Moreover, 52.6% of participants had a high school degree or lower. The median duration of asthma diagnosis in years was 10 (10–15), with 39.3% of the patients hospitalized in the past year due to asthma. In addition, (68.9%) of the patients were not smokers, while 19.4% were smokers and 11.6% were ex-smokers, respectively. 64% of participants had uncontrolled asthma and only 8.8% of the participants had well-controlled asthma symptoms (see Table 1).
 |
Table 1 Sociodemographic Characteristics of the Enrolled Participants (n=397) |
Knowledge About Asthma, Influenza, and the Influenza Vaccine
Asthmatics’ responses to the knowledge items regarding asthma, influenza, and the vaccine are presented in Table 2. The median for the total knowledge score was 17 (ranging from 15 to 20) out of a maximum possible score of 27 (Cronbach’s Alpha = 0.71). The highest percentage of correct answers on “asthma knowledge” was observed for the items “Do dust/air pollution trigger asthma symptoms?” and “Does smoking trigger asthma symptoms?” (95% and 93.5% respectively). On the other hand, the lowest scores were achieved on the items “Do you know how to properly use the peak flow meter?” and “Do NSAIDs (Brufen, Voltaren) worsen asthma symptoms?” (21.4% and 22.7%, respectively). Regarding “influenza knowledge”, 95% of asthmatics correctly answered the item “Influenza can spread from one person to another”, while only 20.7% of asthmatics correctly answered the item “Antibiotics can be used to treat flu”. Lastly, the item with the highest score in the influenza vaccine knowledge’ section was “Is there a vaccine against the flu?” (74.8%), while the item with the lowest percentage of correct responses was “Do you know the difference between triple and quadruple influenza vaccines?” with only 12.4% indicating that they knew the difference.
 |
Table 2 Patients’ Responses to Asthma, Flu, and Vaccine Knowledge Items (n=397) |
Attitudes Toward the Influenza Vaccine
Asthmatics’ responses to the influenza vaccine attitude items are provided in Table 3. The median for the flu vaccine attitude score was 28 (25–32) out of a maximum possible score of 40 (Cronbach’s Alpha = 0.768). In the reversed-coded statements, most of the asthmatics’ strongly disagreed/disagreed’ with the statement “Catching the flu is not a problem for me” with a total percentage of (62.6%), while only 40.5% “strongly disagreed/disagreed” with the statement “The flu vaccination may cause complications/troubles for me”. For the remaining statements, (76%) of the asthmatics “strongly agreed/agreed” with the item “It is easy to reach the pharmacy /hospital to receive the flu vaccination” while 46.5% “strongly agreed/agreed” with the statement “My physician believes that I should receive the flu vaccine”.
 |
Table 3 Participants’ Responses to Influenza Vaccine Attitude Items. (n=397) |
Practices Regarding Asthma and the Influenza Vaccine
Asthmatics’ responses to asthma practice items were assessed using 11 different statements as shown in Table 4. The median for the asthma practices score was 37 (ranging from 33 to 41) out of a maximum possible score of 55 (Cronbach’s alpha = 0.70). The most frequent practice among asthmatics was for the items “How often do you avoid exposure to dust/air pollution?” and “How often do you avoid exposure to pets?” with 81.6% and 76.1% of the asthmatics, respectively, reporting such practices as “always/usually”. On the contrary, the least-frequently reported practices among asthmatics were “How often do you use an air dehumidifier?” and “How often do you use a flow meter at home?” (10.6% and 11.6%, respectively).
 |
Table 4 Patients’ Responses to Different Asthma Practice Items. (n=397) |
Asthmatics’ responses to influenza vaccine practice items are provided in Table 5. The analysis showed that 42.4% of respondents had never received the influenza vaccine. Most of those who had received the vaccine (71.4%) could not identify which type of vaccine they had received. The most-reported side effect was redness, while the least-reported side effect was nausea (55.5% and 9.6%, respectively). In addition, 61.8% of the vaccinated asthmatics reported having mild side effects after receiving the vaccine. When patients were asked about their intention to take the influenza vaccine in the current year, 51.1% confirmed that they intended to do so.
 |
Table 5 Patients’ Responses to Influenza Vaccine Practice Items (n=397) |
A Multinomial Logistic Regression Between Sociodemographic Variables and the Intention to Vaccinate Against Influenza in the Current Year
Bivariate analysis using Chi-square and Kruskal–Wallis tests assessed the association between the intention to receive influenza vaccine in the current year and several socio-demographic and medical variables. Gender (p =0.035), education (p <0.001), household monthly income level (p <0.001), age (p=0.008), and knowledge (p=0.001) were significantly associated with the intention to receive the influenza vaccine.
A multinomial logistic regression was performed to assess the association between sociodemographic variables and the intention to vaccinate against influenza in the current year. The analysis revealed that as age increased, rejection of receiving the influenza vaccine decreased (Relative Risk Ratio (RRR)= 0.978, 95% Cl [0.959–0.997], p = 0.0021). As the knowledge score increased, hesitancy and rejection of receiving the influenza vaccine decreased (RRR = 0.902, 95% Cl [0.839–0.970], p = 0.05 and RRR = 0.916, 95% Cl [0.847–0.990], p =0.028, respectively). Being in the low-income group increased the odds of being hesitant toward receiving the influenza vaccine compared to the high-income group (RRR = 1.989, 95% Cl [1.187–3.332], p = 0.009). Moreover, asthmatics who had well-controlled asthma had lower odds of being hesitant toward receiving the influenza vaccine, compared to those who had uncontrolled asthma (RRR = 0.193, 95% Cl [0.053–0.698], p =0.012). (See Table 6)
 |
Table 6 Multinomial Regression Model Between Different Sociodemographic Characteristics and the Intention to Vaccinate Against Flu This Year (n=397) |
Reasons for not wanting to receive the influenza vaccine or not receiving it annually are presented in Figure 1. The most commonly-reported reason for non-vaccination was “I don’t know the benefit of it” (41.6%) followed by “I don’t believe it is effective” (20.8%), while the least-reported reasons were “The physicians do not recommend it” (1.2%) and “It is expensive” (6.7%).
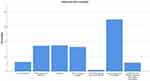 |
Figure 1 Reasons for non-vaccination. |
Discussion
The current study aimed to explore asthmatic patients’ knowledge about asthma, influenza and its vaccine, patients’ adherence to practices that improve asthma control, and their practices and attitudes towards vaccinating against influenza, and to determine the variables associated with asthmatics’ intention to receive the influenza vaccine in the current year. Our findings highlighted several socio-demographic and knowledge-related variables that significantly influenced vaccination intention among asthmatic patients. Gender, education, household monthly income level, age, and knowledge about asthma, influenza, and its vaccine were found to be associated with the intention to vaccinate against influenza. The results of the multinomial logistic regression provided further insights into the relationship between these variables and the intention to receive the influenza vaccine. As age increased, the rejection of the influenza vaccine decreased, indicating that older asthmatic patients were more inclined to get vaccinated. This result aligns with findings from a comprehensive review suggesting that older adults in the Middle East tend to have a more positive attitude towards influenza vaccination.23 A global systematic review has yielded similar findings.24 Age’s positive association with vaccination intention corresponds to the common understanding that older adults have a more positive attitude towards preventive measures like influenza vaccination.25 As age increases, awareness of disease risks and the importance of vaccination may similarly increase.
Although the present study did not find any significant association between vaccination intention and gender in the multivariate analysis, females had a significantly higher intention to receive the vaccine in the bivariable analysis. The association of gender with the intention to receive the influenza vaccine could be attributed to differing health-seeking behaviors and risk perceptions between men and women. Women often exhibit more proactive health-seeking tendencies,26 potentially leading to a greater intention to receive the influenza vaccine.
The present study also revealed that more knowledge about asthma, influenza and its vaccine was associated with reduced hesitancy towards and rejection of the influenza vaccine. A lack of knowledge has consistently been identified to act as a barrier towards influenza vaccination in high-risk groups as well as in the general public.24 This underscores the importance of health education and information dissemination to improve vaccine acceptance among asthmatic patients in Jordan.
Interestingly, being in the low-income group was associated with increased odds of vaccine hesitancy compared to the high-income group. This finding is in line with research on the effect of income disparities on influenza vaccination coverage in the United States, which showed decreased odds of receiving the influenza vaccine for individuals with a low income.27 Furthermore, the prevalence of high-risk indications for the influenza vaccine has been found to be higher in low-income groups.28 Financial concerns might act as a barrier to accessing healthcare services and vaccinations for some individuals. Addressing cost-related issues through subsidized vaccination programs (eg, free or low-cost influenza vaccines for asthmatic patients) or public health initiatives could be beneficial to promoting influenza vaccination equity in Jordan. Community-focused campaigns with culturally sensitive messaging, outreach programs, and mobile clinics can ensure equitable access to vaccination services, particularly in underserved areas. Collaborating with healthcare providers and leveraging their influence in patient education could foster trust and address cost-related concerns. Additionally, long-term educational efforts involving government agencies such as the Ministry of Health, local health departments, healthcare providers, and community organizations can combat misconceptions and emphasize vaccination’s importance for overall health.
One suggested approach is to enhance health education campaigns that are specifically tailored to the local culture, aiming to rectify prevailing misconceptions. Additionally, fostering a stronger collaboration between healthcare providers and public health practitioners is essential to ensure the accurate dissemination of information. Leveraging digital platforms and social media can serve as another avenue for sharing evidence-based content, contributing to the correction of misinformation. Digital interventions have been used successfully to increase influenza vaccine uptake in diabetic patients;29 their usefulness in relation to asthma patients’ vaccine uptake should be explored in future research. To encourage more interactive engagement, organizing workshops, town hall meetings, and support groups within communities could prove beneficial. Moreover, forming partnerships with local pharmacies and schools could play a significant role in ensuring that accurate information reaches a wider audience. Adopting these strategies would aid public health practitioners in effectively countering misinformation, elevating awareness, and contributing to bolstering influenza vaccination rates within the asthmatic patient population in Jordan.
Moreover, our study found that asthmatics with well-controlled asthma were less hesitant towards receiving the influenza vaccine compared to those with uncontrolled asthma. This finding contradicts prior research with parents of children in Jordan who had uncontrolled or partially controlled asthma showing lower odds of rejecting influenza vaccination than parents of those who had controlled asthma.16 Our findings suggest that adult patients who perceive their asthma to be under control may be more proactive in preventive measures such as vaccination. Healthcare providers should emphasize the importance of influenza vaccination, especially for asthmatic patients with suboptimal asthma control, as they may be at higher risk of severe complications from influenza infection.
The reasons reported by asthmatics for not wishing to get vaccinated against influenza shed light on potential barriers that need to be addressed in public health campaigns. The most cited reason was a lack of knowledge about the benefits of vaccination, emphasizing the need for targeted educational efforts to raise awareness about the importance of influenza vaccination for asthmatic patients. Pharmacist-initiated interventions to increase influenza vaccine uptake in patients with asthma or COPD have shown to be effective in prior research.30 Additionally, addressing forgetfulness and implementing strategies to remind asthma patients about the influenza vaccine’s availability could also help improve vaccination rates. Text message reminders, for example, have been shown to be an effective strategy for increasing influenza vaccine uptake.31 In light of the conflicting findings in the prior literature, a longitudinal study design could provide different insights and allow for the observation of changes over time.
The present findings can be interpreted in light of the COM-B model, which proposes that for behaviour change to occur, a person must have the capability, opportunity, and motivation to change the behaviour.32 Thus, our findings can be interpreted as follows: capability, as represented by knowledge about asthma, influenza, and its vaccine, was associated with reduced hesitancy towards and rejection of the influenza vaccine. Opportunity, reflected in socio-demographic factors such as gender, education, household monthly income level, and age, influenced the intention to vaccinate against influenza. For instance, being in the low-income group was associated with increased odds of vaccine hesitancy. Motivation, which can be influenced by age and gender among other factors,33 also played a role in vaccination intention. As age increased, the rejection of the influenza vaccine decreased, and females had a significantly higher intention to receive the vaccine in the bivariable analysis.
This underscores the importance of health education and information dissemination to improve influenza vaccine acceptance among asthmatic patients in Jordan. Future interventions aiming to increase influenza vaccination among asthmatic patients could benefit from considering these components of behavior change. The MRC framework34 could provide valuable guidance for future intervention development. This framework is a guide for developing and evaluating complex interventions and presents a process that includes development or identification of interventions, feasibility testing, evaluation and implementation. Using the MRC framework to guide intervention design could help identify key areas of focus based on our findings.
Study Strengths and Limitations
Several limitations of the current study need to be acknowledged. Convenience sampling was used to select participants, which may have led to selection bias; as participants self-selected into the study, their attitudes towards vaccination might differ from those who did not choose to take part, potentially impacting the generalizability of the findings. This bias could lead to the overrepresentation of proactive healthcare seekers and a potential overestimation of positive vaccination intentions. Conversely, those facing barriers might be underrepresented, affecting the diversity of our results. To enhance future research, adopting random sampling techniques could help mitigate self-selection bias and provide a more balanced representation, eliciting the views of those who may be less motivated to take part in such research. The cross-sectional design of the research is another limitation as this prevented us from establishing causal relationships between variables. Further research, using a longitudinal design, could offer more robust evidence of the factors influencing influenza vaccination behavior in asthmatic patients in Jordan over time. Furthermore, it is important to note that our study was partly conducted during a period when people were not actively taking the influenza vaccine, which could have influenced our findings. Future research should take the timing of data collection into consideration.
Yet it should be highlighted that a strength of this study lies in the use of multivariate logistic regression analysis to explore the association between sociodemographic variables and the intention to vaccinate against influenza. This allowed for the identification of independent predictors associated with vaccine acceptance, thereby providing a more nuanced understanding of the factors influencing vaccination behavior among asthmatic patients.
Apart from its analytic approach, another key strength of the present study lies in its novelty and contribution to the existing literature. By investigating the knowledge, attitudes, and practices of asthmatic patients towards receiving the influenza vaccine in Jordan, the study addresses a critical gap in research and provides valuable insights into an understudied area. Moreover, a large sample size was included by enrolling 397 asthmatic adults, thereby enhancing statistical power and allowing for more generalizable findings. These participants were recruited from outpatient respiratory clinics in various Jordanian hospitals, adding to the diversity of the sample and potentially increasing the external validity of the results.
Conclusion
This study provides a comprehensive examination of the factors influencing influenza vaccination intentions among asthmatic patients in Jordan. Our most impactful findings reveal that sociodemographic variables, particularly age and income, significantly influence vaccination intentions. As age increased, the rejection of the influenza vaccine decreased, indicating that older asthmatic patients were more inclined to get vaccinated. However, being in the low-income group was associated with increased odds of vaccine hesitancy. Moreover, we identified knowledge gaps and misconceptions about vaccination as major barriers to vaccine acceptance. These findings underscore the urgent need for targeted health education campaigns to address these misconceptions and improve vaccine acceptance.
We propose several strategies to increase influenza vaccination rates among this vulnerable population, including collaboration with healthcare providers, utilization of digital platforms, community engagement, and partnerships with pharmacies and schools. Further research is recommended, preferably using a longitudinal design, to monitor the effectiveness of these interventions and understand the dynamics of vaccine acceptance among asthmatic patients in Jordan over time.
By highlighting these key findings and recommendations, we aim to guide healthcare providers and policymakers in developing tailored interventions to improve asthma control and reduce the burden of exacerbations caused by respiratory viral infections.
Institutional Review Board Statement
Ethical approval was obtained from the Al-Zaytoonah ethical committee approval number (Ref#22/23/2020–2021), on 21 September 2021.
Funding
This work was supported by the Researchers supporting project number (RSP2023R235), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Anon. GINA main report - global initiative for asthma – GINA; 2022.
2. Al-Qerem WA, Ling J, Pullen R, McGarry K. Reported prevalence of allergy and asthma in children from urban and rural Egypt. Air Qual Atmos Health. 2016;9(6):613–620. doi:10.1007/s11869-015-0372-1
3. Al Hroob AM, Nawafleh H, Altaif KI, et al. Population Prevalence of Asthma in Ma’an Governorate, Jordan. Health Sci J. 2016;10:2.
4. Wark PAB. Why are people with asthma more susceptible to influenza? Eur Respir J. 2019;54(4):1901748. doi:10.1183/13993003.01748-2019
5. Centers for disease control vand prevention (CDC).
6. Tabaza H, Abu Farha R, Naser AY, Awwad O. Treatment-related problems and their cost among patients hospitalised with asthma exacerbation. J Pharm Health Serv Res. 2023;14(3):359–366. doi:10.1093/jphsr/rmad027
7. Song HJ, Blake KV, Wilson DL, Winterstein AG, Park H. Medical costs and productivity loss due to mild, moderate, and severe Asthma in the United States. J Asthma Allergy. 2020;13:545–555. doi:10.2147/JAA.S272681
8. World Health Organization (WHO).
9. Hajjo R, Sabbah DA, Bardaweel SK, Tropsha A. Shedding the light on post-vaccine myocarditis and pericarditis in covid-19 and non-covid-19 vaccine recipients. Vaccines. 2021;9(10):1186. doi:10.3390/vaccines9101186
10. Vasileiou E, Sheikh A, Butler C, et al. Effectiveness of influenza vaccines in asthma: a systematic review and meta-analysis. Clin Infect Dis. 2017;65(8):1388–1395. doi:10.1093/cid/cix524
11. Moitra S, Lacy P. Influenza vaccination and healthcare utilization in asthma: a Canadian experience. Lancet Reg Health. 2023;23:100526. doi:10.1016/j.lana.2023.100526
12. Keenan H, Campbell J, Evans PH. Influenza vaccination in patients with asthma: why is the uptake so low? Br J Gen Pract. 2007;57(538):359.
13. Knobler SL, Mack A, Mahmoud A, Lemon S. The Threat of Pandemic Influenza: Are We Ready? Workshop Summary. Washington, DC: National Academies Press; 2005.
14. Chapman GB, Coups EJ. Predictors of influenza vaccine acceptance among healthy adults. Prev Med. 1999;29(4):249–262. doi:10.1006/pmed.1999.0535
15. AlQurashi A, Aljishi H, Demyati E. Parental perception towards flu vaccination for asthmatic children in Saudi Arabia. Cureus. 2019. doi:10.7759/cureus.6460
16. Al-Qerem W, Jarab A, Hammad A, et al. Knowledge, attitudes, and practices of influenza vaccination among parents of children with asthma: a cross-sectional study. Vaccines. 2023;11(6): 1074.
17. Gnanasekaran SK, Finkelstein JA, Hohman K, O’Brien M, Kruskal B, Lieu TA. Parental perspectives on influenza vaccination among children with asthma. Public Health Rep. 2006;121(2):181–188. doi:10.1177/003335490612100213
18. Jiang B, Wang Z, Jia M, et al. Awareness, knowledge and attitude toward influenza vaccination in several population groups in China: a cross-sectional study. Front Public Health. 2022;10:950532. doi:10.3389/fpubh.2022.950532
19. Barry MA, Aljammaz KI, Alrashed AA. Knowledge, attitude, and barriers influencing seasonal influenza vaccination uptake. Can J Infect Dis Med Microbiol. 2020;2020. doi:10.1155/2020/7653745
20. Al-Qerem W, Al Bawab AQ, Hammad A, et al. Parents’ attitudes, knowledge and practice towards vaccinating their children against COVID-19: a cross-sectional study. Hum Vaccin Immunother. 2022;18. doi:10.1080/21645515.2022.2044257
21. Anon. GINA main report - global initiative for asthma – GINA; 2023.
22. Krejcie R, Morgan D. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–610. doi:10.1177/001316447003000308
23. Alalag ZA, Al-Jumaili AA, Al-Hamadani FY. A comprehensive review of drivers influencing flu vaccine acceptance in the middle east over the last six years: using health belief model. Int J Pharm Pract. 2022;30(1):5–16. doi:10.1093/ijpp/riab063
24. Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior – a systematic review of influenza vaccine hesitancy, 2005 – 2016. PLoS One. 2017;12(1):e0170550. doi:10.1371/journal.pone.0170550
25. Myers LB, Goodwin R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health. 2011;11(1):1–8. doi:10.1186/1471-2458-11-15
26. Ek S. Gender differences in health information behaviour: a Finnish population-based survey. Health Promot Int. 2015;30(3):736–745. doi:10.1093/heapro/dat063
27. Gaskin CM, Woods DR, Ghosh S, Watson S, Huber LR. The effect of income disparities on influenza vaccination coverage in the United States. Public Health Rep. 2023;138(1):85–90. doi:10.1177/00333549211069190
28. Zimmerman RK, Lauderdale DS, Tan SM, Wagener DK. Prevalence of high-risk indications for influenza vaccine varies by age, race, and income. Vaccine. 2010;28(39):6470–6477. doi:10.1016/j.vaccine.2010.07.037
29. Lee JL, Foschini L, Kumar S, et al. Digital intervention increases influenza vaccination rates for people with diabetes in a decentralized randomized trial. Npj Digital Med. 2021;4(1):138. doi:10.1038/s41746-021-00508-2
30. Klassing HM, Ruisinger JF, Prohaska ES, Melton BL. Evaluation of pharmacist-initiated interventions on vaccination rates in patients with asthma or COPD. J Community Health. 2018;43(2):297–303. doi:10.1007/s10900-017-0421-9
31. Jones Cooper SN, Walton-Moss B. Using reminder/recall systems to improve influenza immunization rates in children with asthma. J Pediatr Health Care. 2013;27(5):327–333. doi:10.1016/j.pedhc.2011.11.005
32. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. doi:10.1186/1748-5908-6-42
33. Klein SL, Morgan R. The impact of sex and gender on immunotherapy outcomes. Biol Sex Differ. 2020;11(1):1–10. doi:10.1186/s13293-020-00301-y
34. Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ. 2021;2021:374.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
