Back to Journals » Infection and Drug Resistance » Volume 17
Evolution of Peritoneal Dialysis-Associated Peritonitis: Pathogen, Antibiotic Resistance, and the Impact of Lymphocyte Count on Treatment Outcomes
Authors He Y , Yang G , Wang P, Wang X, Xiong Z, He Y, Xiong Z
Received 30 September 2023
Accepted for publication 7 February 2024
Published 19 February 2024 Volume 2024:17 Pages 685—696
DOI https://doi.org/10.2147/IDR.S442641
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
YuJian He,1,2,* Guang Yang,1,* Pengpeng Wang,1,3 Xu Wang,1,3 Zuying Xiong,1 Yan He,1,* Zibo Xiong1,*
1Renal Division, Peking University Shenzhen Hospital, Shenzhen, People’s Republic of China; 2Renal Division, PKU-Shenzhen Clinical Institute of Shantou University Medical College, Shenzhen, People’s Republic of China; 3Renal Division, PKU-Shenzhen Clinical Institute of Shenzhen University Medical College, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zibo Xiong, Renal Division, Peking University Shenzhen Hospital, Shenzhen, People’s Republic of China, Tel +86-13510880599, Email [email protected]
Purpose: Antibiotic administration leads to alterations in pathogenic organisms and antibiotic resistance, posing a significant risk to peritoneal dialysis patients’ health. This study aimed to investigate changes in the cause-specific peritonitis, pathogen profiles, antibiotic resistance, and the prognostic factors among patients with peritoneal dialysis-associated peritonitis (PDAP) at our center.
Patients and Methods: We included 463 PDAP patients who attended Peking University Shenzhen Hospital between 2002 and 2023. We analyzed the effects of empirical treatment regimens with cefazolin and ceftazidime or gentamicin.
Results: From 2002 to 2023, we observed that gram-positive staphylococci emerged as the primary causative agents, while the proportion of gram-negative bacillary, enteric peritonitis, and catheter-associated peritonitis decreased significantly. However, the overall cure rate for PDAP and gram-negative bacillary peritonitis declined significantly from 2014 to 2023. Notably, we observed no increase in antibiotic resistance associated with antibiotic drugs use. In addition, reduced lymphocyte counts due to the prevalence of 2019 coronavirus disease (COVID-19) emerged as an independent risk factor for treatment failure in cases of gram-negative bacillary peritonitis.
Conclusion: We did not observe elevated antibiotic resistance in our center when employing empirical dosing strategies involving cefazolin, ceftazidime, or gentamicin. Additionally, we found that a decrease in lymphocyte count due to the COVID-19 epidemic was a significant risk factor for treatment failure in cases of gram-negative bacillary peritonitis at our center. This study provides a foundation for developing clinical treatment strategies for PDAP.
Keywords: antibiotic resistance, COVID-19, lymphocyte count, peritoneal dialysis, peritonitis, pathogen spectrum
Introduction
Peritoneal dialysis (PD) utilizes the peritoneum as a semi-permeable membrane to introduce dialysis solution into the peritoneal cavity by gravity. This process eliminates metabolites and toxic substances while balancing internal environment homeostasis through osmosis.1,2 PD is commonly used for acute kidney injury (AKI), chronic kidney disease (CKD), kidney failure, and acute toxicity.3 However, the presence of a catheter increases the risk of infection, with peritoneal dialysis-associated peritonitis (PDAP) being the most common complication.4–7 Despite advancements in technology, patient education, and management, the incidence of PDAP persists.8 Moreover, prolonged exposure to antibiotics has escalated pathogen resistance, complicating PDAP treatment. The evolving antimicrobial spectrum of pathogens poses a challenge for empirical dosing in PDAP.
The International Society of Peritoneal Dialysis (ISPD) guidelines have put forward a revised definition of cause-specific peritonitis, along with management criteria for pathogenic peritonitis, culture-negative peritonitis, enteric peritonitis, and catheter-associated peritonitis, with the aim of improving the treatment of peritonitis.9 Nonetheless, the pathogenic spectrum and antibiotic susceptibility of PDAP evolve continually, due to the widespread use of antibiotics, leading to inconsistent outcomes among different centers.10 Zeng and Hwang et al revealed an annual increase in the proportion of gram-negative bacteria peritonitis cases relative to total peritonitis.11,12 Kitterer et al reported that strains of gram-negative bacteria were increasingly less susceptible to ceftazidime and gentamicin.13 As a result, adapting ISPD guideline regimens to real-world situations may be necessary, placing greater emphasis on empirical dosing.
The long-term effects of our empirical dosing strategy (cefazolin and ceftazidime or gentamicin) in treating PDAP remains uncertain. Therefore, we conducted a retrospective study to investigate the impact of this empirical dosing strategy on cause-specific peritonitis, antimicrobial spectrum, and antibiotic resistance at our center and the presence of other factors influencing the prognosis of peritonitis.
Materials and Methods
Ethics
The study received approval from the Ethics Committee of Peking University Shenzhen Hospital (NO. 2022050). Informed consent was waived due to the retrospective nature of the study. All patient information was treated confidentially, and the study adhered to the Declaration of Helsinki.
Patients
We included 463 PDAP patients in this study from February 2002 to February 2023. To facilitate data comparison, we divided the patients into two groups based on a nine-year interval before and after 2011, with a three-year isolation period in between. The 2002–2011 group consisted of 169 episodes of peritonitis, while the 2014–2023 group comprised 294 episodes. We collected patient demographic information, including gender, age, age on dialysis, primary renal disease, microbiology, antimicrobial sensitivity results, and clinical outcomes.
Peritonitis
Catheter-related peritonitis was defined as peritonitis occurring within three months of a catheter infection with the same organism at the exit site or from a tunnel collection, and in the effluent or one sterile site in the context of antibiotic exposure. Enteric peritonitis was defined as peritonitis originating from an intestinal source, involving processes such as inflammation, perforation, or ischemia of intraabdominal organs. Medical cure was defined as the complete resolution of peritonitis, along with the absence of complications such as relapse/recurrent peritonitis, catheter removal, transfer to hemodialysis for ≥30 days, or death. Relapsing peritonitis was defined as an episode of peritonitis occurring within four weeks of completing therapy for a prior episode with the same organism or one sterile (culture-negative) episode (specific organism followed by the same organism, culture-negative followed by a specific organism, or specific organism followed by culture-negative), and was counted as a single episode. In contrast, recurrent and repeat infections were considered separate episodes. PDAP death referred to death with peritonitis occurring within 30 days. Treatment failure included PD catheter removal and PDAP-related death.
Inclusion Criteria
We included all PDAP patients who met the 2022 diagnostic criteria recommended by the ISPD, which required the presence of at least two of the following criteria: (i) clinical features suggestive of peritonitis, such as abdominal pain and/or cloudy dialysis effluent; (ii) dialysis effluent white blood cell (WBC) count >100/μL or >0.1× 109 /L after a dwell time of at least 2 hours, with >50% polymorphonuclear leukocytes; and (iii) positive dialysis effluent culture. We excluded patients who did not have a dialysis effluent culture or who withdrew from active treatment. These inclusion and exclusion criteria ensured that the study population was consistent with current standards for PDAP diagnosis and minimized potential bias due to misclassification or incomplete data.
Therapeutic Schedule
All patients received initial treatment with intraperitoneal first-generation cephalosporin to cover gram-positive organisms, combined with third-generation cephalosporin or aminoglycoside which based on the patient’s residual renal function, to gram-negative organisms. The choice of antibiotics was adjusted promptly after the results of dialysis effluent cultures and antibiotic susceptibility testing became available to ensure optimal coverage and minimize the risk of antibiotic resistance or toxicity. The duration of antibiotic treatment was determined based on the severity and resolution of peritonitis symptoms, as well as the results of subsequent follow-up cultures. The term “most sensitive antibiotic” pertains to the antibiotic exhibiting the utmost susceptibility to the causative agent. Antibiotics demonstrating a sensitivity of ≥ 90% are delineated as highly sensitive antibiotics.
Statistics
Statistical analysis was performed using SPSS version 26.0. Normally distributed continuous variables were presented as mean ± standard deviation (SD) and compared between groups using the two sample Student’s t-test. Non-normally distributed continuous variables were presented as median and interquartile range (IQR) and compared between groups using the Mann–Whitney rank sum test. Categorical variables were reported as frequencies or percentages and compared between groups using the Chi-square or Fisher’s exact test as appropriate.
To identify independent protective factors and risk factors for treatment failure, logistic regression analysis was employed. In the initial univariate analyses, variables with a p-value ≤ 0.10 and demonstrated prognostic relevance in clinical practice were selected for inclusion in the subsequent multivariate analyses. In sensitivity analyses, we excluded data from patients treated after December 2019. This step aimed to clarify whether prognostic risk factors for gram-negative bacillary peritonitis were associated with the 2019 coronavirus disease (COVID-19) epidemic. Odds ratios (OR) and their corresponding 95% confidence intervals (CI) were calculated to determine the relationship between the factors of interest and treatment outcome. A P-value ≤ 0.05 was considered statistically significant.
Results
Peritonitis Rates
To understand the incidence of peritonitis in our centre over the last 22 years, we calculated the overall incidence of peritonitis. From February 2002 to February 2023, 463 episodes of peritonitis occurred in 306 PD patients, including 161 (52.61%) male and 145 (47.39%) female patients. Among of them, 209 (68.30%) experienced just one episode of peritonitis, and 97 (31.70%) had two or more episodes. The incidence of peritonitis was 0.12 episodes per patient-year.
Population Characteristics
To explore any changes in patient population characteristics, we compared the characteristics of PDAP patients in the 2002–2011 and 2014–2023 groups (Table 1). Compared to the 2002–2011 group, patients in the 2014–2023 group tended to be younger and had a longer dialysis age. Additionally, the proportion of patients with chronic nephritis as their primary disease increased from 28.4% to 34.7% and replaced diabetic nephropathy as the most frequently occurring source of the condition.
 |
Table 1 The Characteristics of the Peritoneal Dialysis-Associated Peritonitis Patients Between the 2002–2011 and 2014–2023 Groups |
Changes in Bacterial Spectrum and Cause-Specific Peritonitis
To analyze changes in bacterial composition and cause-specific peritonitis, we compared relevant data between the 2002–2011 and 2014–2023 groups (Table 2). In the past two decades, peritonitis caused by gram-positive cocci, mainly Staphylococcus, has consistently been the primary causative organism of peritonitis in our center. Compared to the 2002–2011 group, the 2014–2023 group had reduced proportions of gram-negative bacillary, enteric peritonitis, and catheter-associated peritonitis, with E. coli peritonitis showing a particularly significant decrease. Moreover, in the 2014–2023 group, culture-negative peritonitis decreased, although this difference was not statistically significant. Additionally, the incidence of gram-negative cocci, gram-positive rods, fungi, and polymicrobial peritonitis in the 2014–2023 group were similar to those in the 2002–2011 group.
 |
Table 2 The Compositions of the Cause-Special Peritonitis Between the 2002–2011 and 2014–2023 Groups |
Antimicrobial Sensitivity and Resistance of Pathogenic Bacteria
To investigate the effect of long-term antibiotic use on antibiotic susceptibility, we compared data related to pathogens from 2002–2011 and 2014–2023 for both groups (Figure 1). The results showed no significant change in antimicrobial susceptibility for all pathogens. Vancomycin and rifampicin remain the most sensitive antibiotics against gram-positive cocci, while amikacin, imipenem and piperacillin/tazobactam were highly sensitive against gram-negative bacillary. Ampicillin and ampicillin/sulbactam remained the most resistant antibiotics. In addition, antibiotic susceptibility of gram-negative bacillary to gentamicin and ceftazidime increased in the 2014–2023 group, suggesting that empirical treatment at our center did not increase antibiotic resistance. Moreover, the susceptibility of all pathogens to cefepime may remain at a high level.
 |
Figure 1 The change of antimicrobial sensitivity in gram-positive cocci and gram-negative bacillary peritonitis between the 2002–2011 and 2014–2023 groups. |
PDAP Outcomes
From 2002 to 2023, 391 (84.45%) out of 463 PDAP patients were cured, while the remaining 72 cases were classified as treatment failures, with 59 patients requiring catheter removal and 13 patients succumbing to the disease. To investigate the changes in the prognosis of peritonitis caused by specific pathogens, we compared the cure rates of two patient groups from 2002 to 2011 and 2014 to 2023 (Table 3). Compared with the 2002–2011 group, the overall cure rates for PDAP and gram-negative bacillary peritonitis were significantly lower in the 2014–2023 group. Notably, the cure rate for gram-positive coccus peritonitis remained above 90%, while the failure rate for fungal peritonitis was 100%. Moreover, there were no significant changes in the cure rates for catheter-associated peritonitis, culture-negative peritonitis, enteric peritonitis, or other bacterial peritonitis.
 |
Table 3 Comparison of Prognosis Between the 2002–2011 and the 2014–2023 Groups |
Association Between Risk Factors and Gram-Negative Bacillary Peritonitis Treatment Failure
To investigate potential factors beyond causative agent resistance that may contribute to the decline in cure rates for gram-negative bacillary peritonitis, we conducted a risk factor analysis of the patient cohort spanning from 2014 to 2023. Our findings indicate that lymphocyte count emerged as an independent risk factor influencing the failure of gram-negative bacillary treatment (OR: 0.054, 95% CI: 0.005–0.598, P = 0.017). These results are summarized in Table 4.
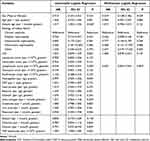 |
Table 4 Significant Risk Factors for the Gram-Negative Bacillary Peritonitis Prognosis During 2014–2023 |
Sensitivity Analysis
To investigate the association between lymphocyte counts and the occurrence of COVID-19, we conducted additional sensitivity analyses. These analyses were rigorously validated by restricting our patient selection to those recorded between February 2014 and November 2019, with patients from the period following the COVID-19 outbreak being excluded. Our multifactorial analysis yielded the result that lymphocyte counts were not identified as a risk factor for treatment failure in patients with gram-negative bacillus infections during the period from February 2014 to November 2019 (OR: 0.014, 95% CI: 0.001–1.421, P = 0.070), as detailed in Table 5.
 |
Table 5 Significant Risk Factors for the Gram-Negative Bacillary Peritonitis Prognosis During 2014–2019 |
Discussion
PDAP remains a common and serious complication of PD therapy, often leading to treatment failure and mortality. Given the single-center specificity of PDAP, it is crucial to regularly summarize the pathogenic spectrum and antibiotic resistance patterns. In this study, we analyzed the prevalence of various types of cause-specific peritonitis, antibiotic resistance, and patient prognosis under empirical treatment with cefazolin and ceftazidime or gentamicin-based drugs over a 22-year period at our center. Our findings provide valuable guidance for the management of PDAP treated empirically with similar drug regimens. Furthermore, the methods employed in this study are applicable to single-center investigations of other drug-resistant pathogens.
A key finding of our study is the increasing proportion of younger PDAP patients, accompanied by a rise in dialysis age. This trend can be partially attributed to the expansion of our dialysis center since 2002, leading to the recruitment of more patients over time. Like many others around the world,14–16 our center has observed an increasing incidence of kidney disease in younger individuals. Consequently, younger patients are more likely to receive PD and experience PDAP. This trend has significant implications for PD and PDAP management, as younger patients may present different comorbidities, lifestyles, and treatment preferences that must be considered for optimal care. Furthermore, chronic nephritis has gradually become the main cause of PD patients in our center, which is consistent with the etiology of younger CKD patients of developing nations.17–19
According to ISPD guidelines, the overall peritonitis rate should be no more than 0.40 episodes per year at risk and the positive bacterial culture rate for peritonitis should be over 85%.9 Our study discovered an incidence of peritonitis at our center was 0.12 episodes/patient/year, demonstrating that our incidence rates are well below the ISPD-recommended threshold. Thus, our findings align with the ISPD recommendations for peritonitis incidence in a single center. However, our center’s data indicates that the positive rate during 2014–2023 was only 73.47%, albeit an increase from 68.64% in 2002–2011. Notably, this trend is not exclusive to our center, as other centers have also reported sub-optimal rates.20–23 This may result from antibiotics use before collecting peritoneal fluid, potentially killing or suppressing bacteria. To overcome this challenge, many molecular diagnostic techniques, such as polymerase chain reaction (PCR) and high-throughput sequencing,24,25 are being developed and applied to identify the microbial flora in peritonitis.26 By offering rapid and accurate diagnosis, these techniques may enhance peritonitis management and compliance with ISPD guidelines. Moreover, our study discerned a decline in the occurrence of enteric peritonitis and catheter-related peritonitis within our center during 2014–2023. This decline primarily stems from the center’s concerted efforts to ameliorate risk factors, including gastrointestinal dysfunction and hypokalemia among PD patients, coupled with the implementation of standardized education and training in PD procedures in recent years.
The choice of antibiotics for PDAP is critical to patient outcomes.27 Because dosing regimens may vary among different centers, it is essential to develop an empirical treatment protocol tailored to the local situation.9,28 According to ISPD guidelines, first-generation cephalosporins or vancomycin are recommended as empirical treatment for gram-positive cocci. Patients on long-term use of certain antibiotics or receiving dialysis are at increased risk of colonization and infection with vancomycin-resistant enterococci.29–31 Consequently, our center opts for cefazolin to treat gram-positive cocci, switching to vancomycin only if cefazolin proves ineffective. This is probably the main reason why we can maintain a sensitivity rate of 100% for vancomycin at our center. Recent studies have suggested that the susceptibility of gram-positive bacteria to first-generation cephalosporins may be decreasing.9,13 However, we have not yet analyzed the resistance patterns of gram-positive cocci to first-generation cephalosporins. Further investigation is required to ascertain the efficacy of first-generation cephalosporins against gram-positive bacteria in our setting and to develop alternative treatment strategies, if necessary.
The ISPD guidelines for gram-negative bacillary peritonitis recommend employing third-generation cephalosporins or aminoglycoside antibiotics as empirical treatment. However, the use of these antibiotics has been associated with the emergence of extended-spectrum β-lactamase (ESBL) mutations in some organisms, leading to resistance to cephalosporins.11,13,32 In this study, we did not observe an increase in resistance to ceftazidime or gentamicin in gram-negative bacteria. Furthermore, the susceptibility of gram-negative bacteria to ceftazidime tended to rise. This finding may reflect our center’s preference for narrow-spectrum antibiotics as the initial choice for empirical treatment in recent years, which may have helped to limit the development of antibiotic resistance.
Regarding aminoglycoside antibiotics, our center observed consistently high susceptibility of gram-negative bacillary to amikacin, with slightly increased susceptibility to gentamicin. Related studies have similar results.8 Thus, aminoglycosides can be considered a viable option for treating gram-negative bacillary at the center.
Moreover, gram-negative bacillary have consistently demonstrated sensitivity to carbapenems, with imipenem exhibiting greater than 90% sensitivity. Previous studies have indicated that the effectiveness of carbapenems is comparable to that of cefazolin or ceftazidime combined with netilmicin for the treatment of PDAP.33 However, the use of carbapenems has been associated with the disruption of normal flora and an increased risk of infection. Consequently, carbapenems are not recommended as a first-line option for the initial treatment of PDAP.
According to the ISPD guideline, using cefepime as a single agent to cover both gram-positive cocci and gram-negative bacillary is an effective strategy for empiric treatment. This study showed that cefepime has high susceptibility against both gram-positive cocci and gram-negative bacillary. In particular, cefepime demonstrated a sensitivity rate of up to 100% against gram-positive cocci. Therefore, cefepime can be used alone as a suitable empirical treatment option for peritoneal dialysis-associated peritonitis at out center.
The present study also evaluated the medical cure and failure rates of PDAP at our center during the period of 2002–2023. The findings indicated that the cure rate for gram-positive cocci consistently remained above 90%. However, a significant decline in the cure rate of gram-negative bacillary peritonitis was observed in recent years, which was the primary cause of the overall decrease in cure rate. Similar issues have been reported in other studies, and the high risk of treatment failure and mortality in patients with gram-negative bacterial peritonitis has been associated with multiple factors. Firstly, it may be linked to exposure to contamination, exit infections, and intestinal infections.11,34 Secondly, ESBL mutant gram-negative bacillary can hydrolyze the β-lactam ring, resulting in resistance to penicillin, cephalosporins, and monocyclic antibiotics. Thirdly, their plasmids typically carry genes that confer resistance to other antibiotics, such as aminoglycosides, leading to ineffective treatment with multiple antibiotics.35,36 However, despite the fact that several of the aforementioned studies have found that the cause of treatment failure in gram-negative bacillary is associated with antibiotic resistance, however, the present study did not find an increase in resistance to antibiotics (eg, third-generation cephalosporins and gentamicin) among gram-negative bacillary along with a decrease in the gram-negative bacillary cure rate, which seems to suggest the existence of other factors that influence prognosis in gram-negative bacillary peritonitis in addition to antibiotic resistance.
To explore these other prognostic factors for gram-negative bacillary peritonitis, we conducted risk factor analysis and sensitivity analysis. We discovered that decreased lymphocyte counts during the COVID-19 pandemic period were an independent risk factor for poor prognosis in gram-negative bacillary peritonitis. This finding suggests that the decreased cure rate of gram-negative bacillary peritonitis at our center may be associated with immune system abnormalities in patients due to COVID-19.
Recent studies have identified several factors contributing to COVID-19-associated lymphocytopenia. Lymphocytes express ACE2 receptors on their surfaces, making them susceptible to direct infection by SARS-CoV-2, leading to their lysis.37 Additionally, the cytokine storm observed in COVID-19 patients, characterized by significantly elevated levels of interleukins (mainly IL-6, IL-2, IL-7), granulocyte colony-stimulating factor, interferon-gamma-inducible protein 10, MCP-1, MIP1-a, and tumor necrosis factor (TNF)-α, may promote lymphocyte apoptosits.38–40 This cytokine activation can also lead to atrophy of lymphoid organs, including the spleen, further impairing lymphocyte urnover.41 Lymphocytes play a pivotal role in both cellular and humoral immunity against invading pathogens.42 A decrease in lymphocyte counts can compromise the immune response, potentially delaying the control and elimination of infecting pathogens. Prolonged infection duration may contribute to the progression of peritonitis and eventual treatment failure. It has been demonstrated that the adaptive immune response, involving CD4+ T cells and cytokine release, is crucial in protecting the intestinal barrier and inhibiting bacterial translocation.43–45 Lymphopenia may compromise this barrier and promote bacterial translocation from the intestine to the peritoneal cavity, increasing susceptibility to gram-negative bacteria like E. coli and affecting peritonitis prognosis.
Several limitations should be acknowledged in our study. First, this is a retrospective study conducted at a single center, which may limit the generalizability of our results to other institutions. The antibiotic sensitivity patterns observed in our center could be influenced by the local use of certain antibiotics or the prevalence of specific bacterial strains, which may not be representative of other regions. Further multicenter studies are needed to confirm our findings. Second, our analysis did not include the results of antibiotic resistance testing for gram-positive cocci against first-generation cephalosporins. Therefore, we could not fully evaluate the resistance patterns of all organisms implicated in PDAP. We plan to update our analysis as more data become available. Finally, due to a change in hospital system, we were unable to collect data on patients with peritonitis in the period of 2012–2013. To facilitate comparison, we categorized patients into two groups based on a nine-year interval before and after the system update. Nonetheless, the impact of this time gap on our findings is expected to be minimal. Additionally, for patients included in the 2002–2011 period of our study, we were unable to collect laboratory data due to the older timeframe. Consequently, we could not assess variations in lymphocyte counts between patients in the 2002–2011 and 2014–2023 groups.
Conclusion
In conclusion, this single-center retrospective study summarizes the effect of empirical treatment with cefazolin and ceftazidime or gentamicin as the main agents on PDAP. Gram-positive cocci remained the predominant causative organisms at our center, with a significant decrease in the rates of gram-negative rods, enteric peritonitis and catheter-associated peritonitis. Importantly, there was no significant increase in drug resistance with our empirical treatment. Vancomycin, third-generation cephalosporins, aminoglycosides, and cefepime monotherapy remain available as empiric treatment options for PDAP at our center. Moreover, the cure rate of gram-negative bacillary and overall peritonitis decreased significantly, which appeared to be associated with a decrease in lymphocytes due to the COVID-19 epidemic. Our study provides a foundation for developing clinical treatment strategies for PDAP. In addition to regular monitoring of antimicrobial susceptibility patterns, we should also pay attention to the impact of patients’ immune function status on the prognosis of PDAP.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, Zibo Xiong, upon reasonable request.
Ethical Disclosure
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of the Ethics Committee of Peking University Shenzhen Hospital approved this study.
Patient Consent Statement
Informed consent was waived because it was a retrospective study.
Acknowledgments
We are grateful to all our colleagues in the clinical departments and laboratories.
Funding
This work was supported by Shenzhen San-Ming Project of Medicine (SZSM201812097), Shenzhen Postdoctoral Research Grant (50820191286), Shenzhen Science and Technology Innovation Commission (JCYJ20220530150412026), and the General Program for Clinical Research at Peking University Shenzhen Hospital (LCYJ2021004).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Xia Y, Fan Q, Zhang J, et al. Risk factors and prognosis for latent tuberculosis infection in dialysis patients: a retrospective cohort study at a single tertiary care center. Semin Dial. 2023;37(1):59–64. doi:10.1111/sdi.13150
2. Yang Y, Liao Y, Yuan Z, Xiong Z, Xiong Z. Use of catheterography to diagnose a peritoneal dialysis catheter misplaced in the rectus sheath following percutaneous insertion. Perit Dial Int. 2020;40(5):518–519. doi:10.1177/0896860820918127
3. Liao JL, Zhang YH, Xiong ZB, et al. The Association of Cognitive Impairment with Peritoneal Dialysis-Related Peritonitis. Perit Dial Int. 2019;39(3):229–235. doi:10.3747/pdi.2018.00180
4. Hsieh YP, Chang CC, Wen YK, Chiu PF, Yang Y. Predictors of peritonitis and the impact of peritonitis on clinical outcomes of continuous ambulatory peritoneal dialysis patients in Taiwan--10 years’ experience in a single center. Perit Dial Int. 2014;34(1):85–94. doi:10.3747/pdi.2012.00075
5. Boudville N, Kemp A, Clayton P, et al. Recent peritonitis associates with mortality among patients treated with peritoneal dialysis. JASN is J Am Soc Nephrol. 2012;23(8):1398–1405. doi:10.1681/ASN.2011121135
6. Fan Q, Huang X, Zhang J, Sun Y, Xiong Z, Xiong Z. Value of gamma interferon enzyme-linked immunospot assay in the diagnosis of peritoneal dialysis-associated tuberculous peritonitis. Int Urol Nephrol. 2022;54(4):843–849. doi:10.1007/s11255-021-02960-1
7. Yang G, Tan L, Yao H, Xiong Z, Wu J, Huang X. Long-Term Effects of Severe Burns on the Kidneys: research Advances and Potential Therapeutic Approaches. J Inflamm Res. 2023;16:1905–1921. doi:10.2147/JIR.S404983
8. McGuire AL, Carson CF, Inglis TJ, Chakera A. Effects of a Statewide Protocol for the Management of Peritoneal Dialysis-Related Peritonitis on Microbial Profiles and Antimicrobial Susceptibilities: a Retrospective Five-Year Review. Perit Dial Int. 2015;35(7):722–728. doi:10.3747/pdi.2014.00117
9. Li PK, Chow KM, Cho Y, et al. ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment. Perit Dial Int. 2022;42(2):110–153. doi:10.1177/08968608221080586
10. Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: a global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017;57(13):2857–2876. doi:10.1080/10408398.2015.1077192
11. Zeng Y, Jiang L, Lu Y, et al. Peritoneal dialysis-related peritonitis caused by gram-negative organisms: ten-years experience in a single center. Renal Failure. 2021;43(1):993–1003. doi:10.1080/0886022X.2021.1939050
12. Hwang TY, Kim MG, Oh SW, Jo SK, Cho WY, Yang J. Pathogens of peritoneal dialysis peritonitis: trends from a single-center experience over 15 years. Kidney Res Clin Pract. 2020;39(2):221–227. doi:10.23876/j.krcp.19.035
13. Kitterer D, Latus J, Pöhlmann C, Alscher MD, Kimmel M. Microbiological Surveillance of Peritoneal Dialysis Associated Peritonitis: antimicrobial Susceptibility Profiles of a Referral Center in Germany over 32 Years. PLoS One. 2015;10(9):e0135969. doi:10.1371/journal.pone.0135969
14. Yoon SY, Park HW, Kim HJ, et al. National trends in the prevalence of chronic kidney disease among Korean adults, 2007-2020. Sci Rep. 2023;13(1):5831. doi:10.1038/s41598-023-33122-1
15. Ademola AD, Asinobi AO, Alao MA, Olowu WA. Childhood Nephrotic Syndrome in Africa: epidemiology, Treatment Trends, and Outcomes. Semin Nephrol. 2023;42(5):151311. doi:10.1016/j.semnephrol.2023.151311
16. Wei YQ, Li XJ, Gao CL, Xia ZK. Research progress in growth of chronic kidney disease in children. Zhonghua Er Ke Za Zhi. 2023;61(5):474–477. doi:10.3760/cma.j.cn112140-20221104-00936
17. Yang Y, Da J, Jiang Y, Yuan J, Zha Y. Low serum parathyroid hormone is a risk factor for peritonitis episodes in incident peritoneal dialysis patients: a retrospective study. BMC Nephrol. 2021;22(1):44. doi:10.1186/s12882-021-02241-0
18. Wu H, Ye H, Huang R, et al. Incidence and risk factors of peritoneal dialysis-related peritonitis in elderly patients: a retrospective clinical study. Perit Dial Int. 2020;40(1):26–33. doi:10.1177/0896860819879868
19. Cao Y, Li W, Yang G, Liu Y, Li X. Diabetes and hypertension have become leading causes of CKD in Chinese elderly patients: a comparison between 1990-1991 and 2009-2010. Int Urol Nephrol. 2012;44(4):1269–1276. doi:10.1007/s11255-012-0194-0
20. Camargo CH, Cunha Mde L, Caramori JC, Mondelli AL, Montelli AC, Barretti P. Peritoneal dialysis-related peritonitis due to coagulase-negative Staphylococcus: a review of 115 cases in a Brazilian center. Clin J Am Soc Nephrol. 2014;9(6):1074–1081. doi:10.2215/CJN.09280913
21. Persy B, Ieven M. Four-year analysis of microbial aetiology and antimicrobial sensitivity patterns of peritoneal-dialysis related peritonitis in a tertiary care facility. Acta clinica Belgica. 2013;68(1):48–53. doi:10.2143/ACB.68.1.2062720
22. Szeto CC, Leung CB, Chow KM, et al. Change in bacterial aetiology of peritoneal dialysis-related peritonitis over 10 years: experience from a centre in South-East Asia. Clin Microbiol Infect. 2005;11(10):837–839. doi:10.1111/j.1469-0691.2005.01222.x
23. Wang HH, Huang CH, Kuo MC, et al. Microbiology of peritoneal dialysis-related infection and factors of refractory peritoneal dialysis related peritonitis: a ten-year single-center study in Taiwan. J. Microbiol Immunol Infect. 2019;52(5):752–759. doi:10.1016/j.jmii.2018.10.013
24. Yang G, Chen H, Chen Q, et al. Injury-induced interleukin-1 alpha promotes Lgr5 hair follicle stem cells de novo regeneration and proliferation via regulating regenerative microenvironment in mice. Inflamm Regen. 2023;43(1):14. doi:10.1186/s41232-023-00265-7
25. Yang G, Waheed S, Wang C, Shekh M, Li Z, Wu J. Exosomes and Their Bioengineering Strategies in the Cutaneous Wound Healing and Related Complications: current Knowledge and Future Perspectives. Int J Bio Sci. 2023;19(5):1430–1454. doi:10.7150/ijbs.80430
26. Ye P, Xie C, Wu C, et al. The application of metagenomic next-generation sequencing for detection of pathogens from dialysis effluent in peritoneal dialysis-associated peritonitis. Perit Dial Int. 2022;42(6):585–590. doi:10.1177/08968608221117315
27. Htay H, Cho Y, Pascoe EM, et al. Center Effects and Peritoneal Dialysis Peritonitis Outcomes: analysis of a National Registry. Am. J. Kidney Dis. 2018;71(6):814–821. doi:10.1053/j.ajkd.2017.10.017
28. Li PK, Szeto CC, Piraino B, et al. ISPD Peritonitis Recommendations: 2016 Update on Prevention and Treatment. Perit Dial Int. 2016;36(5):481–508. doi:10.3747/pdi.2016.00078
29. Saengsuwan P, Singkhamanan K, Madla S, Ingviya N, Romyasamit C. Molecular epidemiology of vancomycin-resistant Enterococcus faecium clinical isolates in a tertiary care hospital in southern Thailand: a retrospective study. PeerJ. 2021;9:e11478.
30. Zacharioudakis IM, Zervou FN, Ziakas PD, Rice LB, Mylonakis E. Vancomycin-resistant enterococci colonization among dialysis patients: a meta-analysis of prevalence, risk factors, and significance. Am J Kidney Dis. 2015;65(1):88–97. doi:10.1053/j.ajkd.2014.05.016
31. Moso MA, Macesic N. Peritoneal Dialysis-Related Peritonitis With Carbapenem-Resistant Klebsiella pneumoniae and Vancomycin-Resistant Enterococcus faecium. Open Forum Infect Dis. 2021;8(1). doi:10.1093/ofid/ofaa525
32. Jacoby GA, Munoz-Price LS. The new beta-lactamases. New Engl J Med. 2005;352(4):380–391. doi:10.1056/NEJMra041359
33. Leung CB, Szeto CC, Chow KM, et al. Cefazolin plus ceftazidime versus imipenem/cilastatin monotherapy for treatment of CAPD peritonitis--a randomized controlled trial. Perit Dial Int. 2004;24(5):440–446. doi:10.1177/089686080402400508
34. Wu H, Yi C, Zhang D, et al. Changes of antibiotic resistance over time among Escherichia coli peritonitis in Southern China. Perit Dial Int. 2022;42(2):218–222. doi:10.1177/08968608211045272
35. Malloy AM, Campos JM. Extended-spectrum beta-lactamases: a brief clinical update. Pediatr Infect Dis J. 2011;30(12):1092–1093. doi:10.1097/INF.0b013e31823c0e9d
36. Yip T, Tse KC, Lam MF, et al. Risk factors and outcomes of extended-spectrum beta-lactamase-producing E. coli peritonitis in CAPD patients. Perit Dial Int. 2006;26(2):191–197. doi:10.1177/089686080602600213
37. Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. doi:10.1038/s41368-020-0074-x
38. Singh S, Sharma A, Arora SK. High producer haplotype (CAG) of −863C/A, −308G/A and −238G/A polymorphisms in the promoter region of TNF-α gene associate with enhanced apoptosis of lymphocytes in HIV-1 subtype C infected individuals from North India. PLoS One. 2014;9(5):56.
39. Liao YC, Liang WG, Chen FW, Hsu JH, Yang JJ, Chang MS. IL-19 induces production of IL-6 and TNF-alpha and results in cell apoptosis through TNF-alpha. J Iimmunol. 2002;169(8):4288–4297. doi:10.4049/jimmunol.169.8.4288
40. Aggarwal S, Gollapudi S, Gupta S. Increased TNF-alpha-induced apoptosis in lymphocytes from aged humans: changes in TNF-alpha receptor expression and activation of caspases. J Iimmunol. 1999;162(4):2154–2161. doi:10.4049/jimmunol.162.4.2154
41. Chan JF, Zhang AJ, Yuan S, et al. Simulation of the Clinical and Pathological Manifestations of Coronavirus Disease 2019 (COVID-19) in a Golden Syrian Hamster Model: implications for Disease Pathogenesis and Transmissibility. Clin Infect Dis. 2020;71(9):2428–2446. doi:10.1093/cid/ciaa644
42. Cronkite DA, Strutt TM. The Regulation of Inflammation by Innate and Adaptive Lymphocytes. J Immunol Res. 2018;2018(2018):1467538. doi:10.1155/2018/1467538
43. Hu J, Kang H, Liu C, Hu P, Yang M, Zhou F. Regulatory T Cells Could Improve Intestinal Barrier Dysfunction in Heatstroke. Inflammation. 2019;42(4):1228–1238. doi:10.1007/s10753-019-00983-6
44. Powell N, MacDonald TT. Recent advances in gut immunology. Parasite Immunol. 2017;39(6). doi:10.1111/pim.12430
45. Park A, Lee Y, Kim MS, et al. Prostaglandin E2 Secreted by Thyroid Cancer Cells Contributes to Immune Escape Through the Suppression of Natural Killer (NK) Cell Cytotoxicity and NK Cell Differentiation. Front Immunol. 2018;9:1859. doi:10.3389/fimmu.2018.01859
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
