Back to Journals » Clinical Optometry » Volume 14
Evaluation of Wear Experience with Soft Daily Disposable Lenses for Astigmatism over 16 Hours of Wear
Received 27 August 2022
Accepted for publication 18 October 2022
Published 28 October 2022 Volume 2022:14 Pages 207—214
DOI https://doi.org/10.2147/OPTO.S387740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Jennifer Swingle Fogt, Kimberly Patton
College of Optometry, The Ohio State University, Columbus, OH, USA
Correspondence: Jennifer Swingle Fogt, College of Optometry, The Ohio State University, 338 W 10th Ave, Columbus, OH, 43210, USA, Tel +1 614 292 0882, Email [email protected]
Objective: The purpose of this study was to assess the wear experience of participants while wearing a toric daily disposable contact lens with water surface technology over long days of lens wear.
Methods: Existing soft toric contact lens wearers were fit with the daily disposable study lenses. Participants assessed their initial comfort, vision, and satisfaction with the lenses by visual analog scale (VAS) survey. After a successful 1-week follow-up visit, participants were scheduled for 5 survey days, in which surveys were deployed to their smartphones for immediate assessments of comfort and quality of vision on a 1– 10 scale at 10, 12, 14, and 16 hours of lens wear on 5 subsequent weeknights. The final study visit assessed visual acuity, and overall lens wear experience surveys were completed with VAS surveys. The overall median and interquartile (IQR) range of all surveys were calculated.
Results: Thirty bilateral toric lens wearers completed the study. Median (IQR) initial impression VAS scores were 97(12) for quality of vision, 100(9) for comfort, and 96(10) for satisfaction. Median evening surveys resulted in comfort scores of 10(1) at 10 hours, 9(2) at 12 hours, 9(2) at 14 hours, and 8(2) at 16 hours of wear. Median evening surveys resulted in quality of vision scores of 10(1) at 10 hours, 10(2) at 12 hours, 9(2) at 14 hours, and 9(3) at 16 hours of wear. VAS scores for overall experience were 97(9) for comfort, 95(13) for vision, and 8(31) for dryness. End-of-day VAS scores were 93(21) for comfort, 90(15) for vision, and 21(38) for dryness. Mean (±standard deviation) OU LogMAR visual acuity with the study lenses was − 0.19(0.06).
Conclusion: Surveys of wear experience resulted in high scores for comfort and vision over the course of a long day of wear with the daily disposable study lenses in this population of patients with astigmatism.
Keywords: soft contact lenses, daily disposable, end-of-day, comfort, vision
Background
Successful wear of contact lenses requires satisfactory vision and comfort.1 Studies have shown that discomfort is the primary reason for discontinuation of lens wear,2–4 however poor vision has also been shown to play a role in contact lens dropout, particularly among patients with astigmatism.5 A recent study has reported that comfort with soft contact lenses for astigmatism, commonly known as toric lenses, has been shown to be associated with subjective vision quality.6 For this reason, it is important to maximize both vision and comfort since symptoms of discomfort may be exacerbated if a patient feels their vision is compromised.
Because a patient with astigmatism has a complex prescription, the rotation and stability of a toric lens can play a role in visual outcome.7 In order to minimize rotation of soft contact lenses for astigmatism, additional lens characteristics are added to the design of the lens which varies by manufacturer, and typically includes areas of differential edge thickness that prevents a lens from rotating on the eye.8 As a result, toric lenses may feel different on-eye than spherical lenses, leading many toric contact lens wearers to suffer from increased symptoms of ocular dryness or discomfort.9 While toric lens designs are generally stable, some residual rotation may occur due to the variation in corneal curvature or eyelid anatomy of individual patients. Practitioners must carefully assess the rotation of a toric lens when determining the prescription power of the lens, as a rotated lens may require a different axis to compensate for rotational shifts in the lens.
Additional lens characteristics to consider when optimizing comfort for patients include the lens material and the frequency of lens replacement.10 Daily disposable contact lenses do not require daily cleaning and overnight storage, which is believed to improve comfort compared to re-wearable lenses which require lens care systems.11 In addition, daily disposable contact lenses are associated with less lens deposits, which decreases associated comfort issues in lens wearers, including decreasing the risk of triggering giant papillary conjunctivitis (GPC) and/or ocular allergic responses in patients.12 Additionally, a recent study found that less superficial punctate staining and symptoms of dryness occurred with daily disposable contact lens wear when compared to planned replacement lens wear.13 Daily disposable contact lenses provide ocular health benefits and ease of care for patients.14
For patients with astigmatism, an ideal soft contact lens would maximize both comfort and vision,6 and would be able to maintain these qualities for long hours of wear.2 A soft contact lens for astigmatism must orient itself properly after insertion in order to provide the correct prescription, and must remain rotationally stable during wear in order to achieve and maintain clear vision. The daily disposable lens used in this study is designed with a modified prism-ballast design that stabilizes the lens by making the thickest points of the lens at 8 o’clock and 4 o’clock to create two anchor points during wear.15 Additionally, the study lens has a silicone hydrogel core that is surrounded by a water surface treatment that provides greater than 80% water content at the lens surface, which is believed to contribute to both comfort and vision.16 Given the known benefits of daily disposable lenses, including the accompanying improvement in comfort,17 it is likely that these water surface technology lenses would provide long-lasting comfort and vision throughout the day. Previous studies have found high subjective comfort and vision scores with spherical lenses of this lens material,18 but no studies have been conducted to evaluate the comfort and vision of these lenses for patients with astigmatism. The purpose of this study was to assess the subjective comfort and quality of vision of astigmatic wearers of the study contact lenses over a long day of lens wear.
Methods
This open-label, prospective study was conducted under the approval of the Institutional Review Board at The Ohio State University and is registered on ClinicalTrials.gov (#NCT04844281). This study complied with the Declaration of Helsinki and all participants completed electronic written informed consent prior to screening. A diagram of the study design is presented in Figure 1.
 |
Figure 1 Study design. |
Habitual wearers of soft toric contact lenses aged 18–40 were recruited to participate in the study. After completing the informed consent process, participants completed a vision and ocular health assessment to determine eligibility before being fit with the study lenses. To be eligible, participants were required to wear soft lenses for astigmatism in both eyes, have 20/25 or better vision with their current lens correction and be able to complete all study visits, including 5 long study days with at least 16 hours of lens wear. Patients who were pregnant, had active ocular or systemic inflammation, or had a prescription beyond the range available for the study lenses were ineligible. Eligible participants were fit with the study lens (PRECISION1® for Astigmatism; Alcon Inc, Fort Worth, TX, USA). The fitting process included an evaluation of the centration and movement of the lens, rotation after at least 10 minutes of lens settling, and an over-refraction. After successful fitting of the study contact lenses by the investigator, a visual analog scale (VAS) survey of initial lens impressions with the lenses was deployed to the participant’s own smart device using REDCap (Research Electronic Data Capture), a secure, web-based software platform hosted at The Ohio State University, that is utilized to capture data for research studies.19,20 Each VAS survey was completed by moving a slider along a line to correspond with their impression of each quality on a scale from 0 to 100. The initial quality of vision VAS was anchored with “POOR Quality” at 0 and “EXCELLENT Quality” at 100. The initial comfort VAS was anchored with “POOR Comfort” at 0 and “EXCELLENT Comfort” at 100. The initial satisfaction VAS was anchored with “NOT Satisfied” at 0 and “EXTREMELY Satisfied” at 100. Additional lenses were dispensed to eligible participants, so that they could wear lenses each day until Visit 2, which followed in 1 week (±3 days).
At Visit 2, visual acuity, slit-lamp assessments of ocular health and contact lens fit, and an over-refraction were completed. No subjects required any changes in prescription, so no additional follow-up visits were needed. Subjects were dispensed additional lenses to wear until Visit 3 and the 5 evening survey days were scheduled for weekdays between visits 2 and 3. On the morning of each survey study day, subjects received a “Morning Survey” asking for the time of contact lens insertion that day. Later that evening, an “Evening Survey” was automatically deployed via REDCap at 10, 12, 14 and 16 hours of lens wear. The surveys were deployed on 5 weekdays between Visit 2 and Visit 3 to maintain consistency. Evening surveys included 1–10 forced-choice grading of comfort and quality of vision, with 1 anchored as “Poor comfort” or “Poor vision” and 10 anchored as “Excellent comfort” or “Excellent vision.” The forced-choice selection was used based upon a previous study that explored comfort and vision during evening wear with a spherical contact lens.21 At Visit 3, after approximately 2 weeks of study contact lens wear, participants completed additional VAS assessments of their overall contact lens wear experience while wearing the study lenses. Overall and end-of-day quality of vision VAS surveys were anchored with 0 as “POOR Quality” and 100 as “EXCELLENT Quality”. Overall comfort and end-of-day comfort were each anchored with “POOR Comfort” at 0 and “EXCELLENT Comfort” at 100. Overall dryness and end-of-day dryness were anchored with “No Dryness” at 0 and “MAXIMUM Dryness” at 100. Overall VAS assessments consisted of overall quality of vision, overall comfort and overall dryness. End-of-day VAS surveys included end-of-day quality of vision, end-of-day comfort, and end-of-day dryness. Participants also completed the eight-question Contact Lens Dry Eye Questionnaire (CLDEQ-8) survey, which specifically asks patients to answer the questions based upon their experiences over the past 2 weeks of lens wear.22,23 Additionally, participants completed a final survey which included questions regarding the participants’ experiences with daily disposable lenses and with the study lenses. The scales for convenience, ease of use, and preference for daily disposable contact lenses were 0 to 10, where a score of 0 was not convenient, easy, or preferred; 5 was marked as neutral; and 10 was labelled as very convenient, easy, or preferred.
Statistical Analysis
This sample size of 30 was chosen based upon a previous contact lens study which assessed spherical lens comfort and vision over a long evening of wear.21 A paired t-test sample size calculation based on the difference in comfort from 10 to 14 hours of wear from that study found that a minimum of 12 participants should be enrolled to find a difference in comfort at that timepoint. Two-factor analysis of variance (ANOVA) was used to evaluate the effect of the days and timepoints of the forced-choice evening surveys. Comparisons for each time point of the evening surveys were made using Tukey pairwise analysis. The Anderson–Darling test for normality was completed on the survey data, and non-parametric statistical analysis was used due to non-normality. Median and interquartile range were calculated for the VAS and forced-choice surveys. Responses to all surveys given at the end of the study, including overall and end-of-day comfort, vision and dryness, CLDEQ-8, convenience, ease of use, and satisfaction were analyzed further using a Mann–Whitney analysis to compare responses of habitual reusable lens wearers to habitual daily disposable lens wearers. A Spearman correlation coefficient test was completed to look at the relationship between comfort and vision using both the overall comfort and vision scores and the end-of-day comfort and vision scores. Statistical analysis was conducted using MiniTab (Version 18.1, State College, PA, USA).
Results
Forty-one soft contact lens participants enrolled in the study and completed the consent process. Eleven of these participants were screen failures who did not meet inclusion/exclusion criteria or only required a toric lens in one eye. Thirty bilateral toric wearers, 19 female and 11 male participants completed the study. The (average ± standard deviation) age of the participants with bilateral astigmatism who completed the study was 28.4 ± 6.0 years (Range 19–40 years). The races represented in the participant population included 5 Asian, 21 Caucasian, 1 Black/African American, 2 who reported more than one race, and 1 unknown/not reported participant. Two participants identified their ethnicity as Hispanic or Latino.
Twenty of the participants habitually wore planned replacement lenses and 10 participants habitually wore daily disposable lenses. Two of the daily disposable lens wearers were wearers of the study lens before enrolling in the study.
Visual Acuity
Visual acuity was measured at every visit either with habitual lens or test lens. Vision while wearing the daily disposable contact lenses in this study was measured with LogMAR ETDRS charts, and participants had exceptional vision monocularly and binocularly. Visual acuity with the study lenses recorded at Visit 3 is reported in Table 1. The mean LogMAR binocular acuity of −0.19 is equivalent to 20/12.5−1 Snellen visual acuity.
 |
Table 1 Visual Acuity Data with Study Contact Lenses at Visit 3 |
Rotation of Lenses
Lens fit and rotation was assessed after lenses had settled on the eyes for at least 10 minutes. Of the 54 toric lenses evaluated for rotation, 36 eyes (66.7%) had zero rotation, 49 (90.7%) had rotation 5 degrees or less, and 51 eyes (94.4%) had rotation less than 10 degrees. One eye (1.9%) had 15 degrees of rotation. While the protocol required any trial lens with an over-refraction or rotation that did not maximize visual acuity to be refit, none of the eyes in the study required a second trial lens due to rotation.
Initial Impressions Assessment
Median values (IQR) for the initial impression surveys completed during Visit 1 were 97.0 (11.8) for quality of vision, 100.0 (9.0) for comfort, and 96.0 (10.0) for satisfaction.
Subjective Assessment of Comfort and Vision at Evening Time Points
All 30 subjects were scheduled to complete 4 surveys each night for 5 nights between Visit 2 and Visit 3 for a total of 600 surveys deployed. One participant claimed to have completed the surveys, but no data was found in the data capture system for any of the 5 nights. For the remaining 29 participants, 2 participants were missing 1 night of survey deployment and 1 participant did not have the surveys sent on two evenings.
Median (IQR) for vision and comfort were calculated using data for all 5 days for each time point. At 10 hours of wear, the median (IQR) score for comfort was 10 (1), with a mild decrease over the next 6 hours, with a score of 9 (2) at 12 hours; 9 (2) at 14 hours; and 8 (2) at 16 hours of wear. Median (IQR) quality of vision scores were 10 (1) at 10 hours; 10 (2) at 12 hours; 9 (2) at 14 hours; and 9 (3) at 16 hours of wear. All statistics on the evening surveys can be found in Table 2.
 |
Table 2 Results of Evening Surveys on a 1–10 Scale at Time Points 10, 12, 14, and 16 Hours After Lenses Were Inserted Using All Data Collected Over 5 Days of Surveys (n=29) |
A two-factor repeated analysis of variance (ANOVA) on the means was performed for comfort with evening time points (10, 12, 14 and 16 hours of wear) and day (1–5) as factors, and a interaction term between time and day.24 A P-value less than 0.05 was considered significant. The day of the surveys and the interaction term were not significant. The time point was significant (P<0.001), and Tukey pairwise comparison found no significant differences in comfort at 10 and 12 hours, and a significant difference in the 14- and 16-hour timepoints compared to all other timepoints. A two-factor repeated ANOVA was also completed for vision results, using timepoint and day as factors. An interaction term for time and day was also included. The interaction term was not significant, while day (P=0.04) and timepoint were significant (P<0.001). Tukey pairwise comparisons of the days showed a significant difference only between days 3 and 4. Overall, this suggests that there was no linear trend for the vision results across the days. Tukey analysis of the vision at each timepoint found a significant difference between all time point pair comparisons. Tukey analysis of the vision at each timepoint found a significant difference between all timepoints.
End-of-Study Surveys
End-of-day median (IQR) scores were 93.0 (21.0) for quality of vision and 89.5 (15.0) for comfort. The median end-of-day dryness score was 21.0 (37.8). Median (IQR) scores were 96.5 (8.5) for overall quality of vision and 95.0 (13.3) for overall comfort. The overall dryness median score was 8.0 (24.9). All values calculated for end-of-day and overall surveys are reported in Table 3.
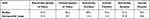 |
Table 3 Visual Analog Scale Assessments of Overall Quality of Vision, Comfort, and Dryness |
The Median (IQR) CLDEQ-8 Score Was 8.0 (7.0)
Data for the final lens wear experience survey was missing data for one participant and is based upon 29 subjects. The median (IQR) score for both convenience and ease of use was 10 (0). The median score for satisfaction with the study lens was 10 (2). No adverse events occurred in this study.
The VAS surveys of initial comfort and vision were compared to the overall comfort and vision surveys using Mann–Whitney analysis, with no significant differences found. Similarly, there were no significant differences when overall comfort and vision were compared to end-of-day comfort and vision.
To determine if the replacement mode of the participants’ habitual contact lenses played a role in the subjective findings of the study lenses, Mann–Whitney was used to analyze the results of all surveys completed at the end of the study. Survey responses of participants who habitually wore reusable lenses to those of participants who habitually wore daily disposable lenses before enrolling in the study. The median scores of the two groups were not significantly different for CLDEQ, convenience, ease of use or satisfaction. There were no significant differences in the responses of the two groups when comparing the end-of-day surveys, or the overall surveys of vision and dryness. The only significant difference was found was between the median overall comfort score for the study lenses when comparing the habitual reusable lens group (96.5) to the habitual daily disposable wearer (88.0) group (P=0.04).
Relationship of Comfort and Vision
The Spearman correlation coefficient test was used to examine the relationship between comfort and vision found in this study. Assessment of overall comfort and overall vision revealed a strong positive correlation (ρ=0.63; P<0.001). Evaluation of end-of-day comfort and end-of-day vision revealed a moderate positive correlation (ρ=0.58; P=0.001).
Discussion
Comfort and vision are both critical to successful contact lens wear. A decline in comfort with soft contact lens wear is a well-known phenomena,25–27 and previous studies have explored comfort assessments during the evening using different survey techniques, including asking patients to recall their end-of-day comfort levels,28 and completion of home surveys before lens removal.29 The ability to quantify vision and comfort in real time via smartphone surveys in the current study gives insight into when changes in symptoms occur during lens wear, and a previous study used this method for capturing subjective impressions of soft sphere contact lenses.21 Results from the current study found that the expected decline in lens comfort and vision over time was gradual over the course of the evening, with median scores of 8(2) for comfort and 9(3) for vision at 16 hours of wear. This maintenance of comfort is important with soft lens wear, as discomfort with lenses in general has been targeted as the most common cause for contact lens dropout.25 It is likely that the water surface treatment of the study lenses are playing a role in these findings, as surface treatment of lens materials can improve lubricity of a soft contact lens, and therefore improve comfort.30 The results of the CLDEQ-8 survey results in this study further confirm the overall comfort findings with the lenses. The median CLDEQ-8 score of 8.0(7.0) is lower than the cutoff point of 12 that is associated with frequent symptoms of dry eye.31
Despite the increased challenges of correcting vision for patients with astigmatism, compared to spherical lens wearers, the vision scores found in this study remained high over a long evening, with a median score of 9 (3) at 16 hours of wear. In this study, it is likely that the high vision scores were a result of the low rotation found with the lenses. Stability of the rotation of the lenses was not assessed in this study, but the high vision ratings at all surveys throughout the study may imply that vision was not blurring intermittently as can occur with unstable soft toric contact lenses. The subjective scores are further validated objectively by the binocular LogMAR visual acuity score of −0.19 (20/12.5−1 Snellen). Comfort and vision were positively correlated with this study lens, which further validates the findings in a previous study of soft toric contact lenses, which found that ocular discomfort may increase if subjective visual quality declines.6
The results of this study reveal that long hours of wear with the study lens yielded reports of high comfort and quality of vision up to 16 hours of wear. It should be noted that the open-label nature of this study could have introduced some potential bias for the participants. This was a non-comparative study, but comparison of the comfort and vision scores of those study participants who were habitual wearers of reusable lenses to those who wore daily disposable lenses habitually did reveal a statistically significant difference when scoring overall comfort of the study lenses. This difference may imply that previous lens wear experience can play a role in subjective assessments of new wear. While this study only examined symptoms using one soft contact lens, the methodology used in this study to assess comfort and vision in real time was effective, and future comparative studies with different lens materials are possible.
Conclusion
In this study, participants responded positively to initial wear, overall wear and end-of-day wear with the study lenses. When surveyed on their comfort and vision over the course of long days in this study, the participants assigned high ratings for both comfort and vision for up to 16 hours of wear with the study lenses.
Data Sharing Statement
Data reported in this manuscript are available within the article. Study-level data including the study protocol are available. To request access to the data, the researcher must sign a data use agreement. All proposals should be directed to [email protected] for up to 36 months following article publication.
Acknowledgments
Funding for this investigator initiated trial was provided by Alcon, Inc., Fort Worth, TX, USA. The project described was supported in part by Award Number Grant UL1TR002733 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Disclosure
Dr Jennifer Swingle Fogt reports grants, personal fees from Alcon, Inc, during the conduct of the study; grants from Bausch + Lomb and Interojo; personal fees from Contamac, outside the submitted work. Dr Jennifer Swingle Fogt also received research funding from Eyenovia and Nevakar for ocular pharmaceutical studies. The authors report no other conflicts of interest in this work.
References
1. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact Lens Anterio. 2017;40:15–24. doi:10.1016/j.clae.2016.10.002
2. Nichols JJ, Willcox MD, Bron AJ, et al. The tfos international workshop on contact lens discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54:TFOS7–TFOS13. doi:10.1167/iovs.13-13212
3. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39:93–99. doi:10.1097/ICL.0b013e318271caf4
4. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26:168–174. doi:10.1097/01.ico.0000248382.32143.86
5. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002;22:516–527. doi:10.1046/j.1475-1313.2002.00066.x
6. Maldonado-Codina C, Navascues Cornago M, Read ML, et al. The association of comfort and vision in soft toric contact lens wear. Cont Lens Anterior Eye. 2021;44:101387. doi:10.1016/j.clae.2020.11.007
7. Chamberlain P, Morgan PB, Moody KJ, Maldonado-Codina C. Fluctuation in visual acuity during soft toric contact lens wear. Optom Vis Sci. 2011;88:E534–E538. doi:10.1097/OPX.0b013e31820ea1ea
8. Eghbali F, Hsui EH, Eghbali K, Weissman BA. Oxygen transmissibility at various locations in hydrogel toric prism-ballasted contact lenses. Optom Vis Sci. 1996;73:164–168. doi:10.1097/00006324-199603000-00007
9. Young G, Chalmers RL, Napier L, et al. Characterizing contact lens-related dryness symptoms in a cross-section of UK soft lens wearers. Cont Lens Anterior Eye. 2011;34:64–70. doi:10.1016/j.clae.2010.08.005
10. Stapleton F, Tan J. Impact of Contact lens material, design, and fitting on discomfort. Eye Contact Lens. 2017;43:32–39. doi:10.1097/ICL.0000000000000318
11. Lira M, Silva R. Effect of Lens care systems on silicone hydrogel contact lens hydrophobicity. Eye Contact Lens. 2017;43:89–94. doi:10.1097/ICL.0000000000000247
12. Hickson-Curran S, Spyridon M, Hunt C, Young G. The use of daily disposable lenses in problematic reusable contact lens wearers. Cont Lens Anterior Eye. 2014;37:285–291. doi:10.1016/j.clae.2014.03.002
13. Ichijima H, Karino S, Sakata H, Cavanagh HD. Improvement of subjective symptoms and eye complications when changing from 2-week frequent replacement to daily disposable contact lenses in a subscriber membership system. Eye Contact Lens. 2016;42:190–195. doi:10.1097/ICL.0000000000000167
14. Chalmers RL, Hickson-Curran SB, Keay L, et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the tempo registry. Invest Ophthalmol Vis Sci. 2015;56:654–663. doi:10.1167/iovs.14-15582
15. Mathew J. Importance of rotational stability in toric contact lens wearers. Available from: https://us.alconscience.com/sites/g/files/rbvwei1736/files/pdf//Importance-of-Rotational-Stability-and-Tear-Film-Stability-in-Toric-Contact-Lens-Wearers-Updated.pdf.
16. Cummings S, Giedd B, Pearson C. Clinical performance of a novel daily disposable soft contact lens. J Cont Lens Res Sci. 2020;4:e23–e30. doi:10.22374/jclrs.v4i1.39
17. Fahmy M, Long B, Giles T, Wang CH. Comfort-enhanced daily disposable contact lens reduces symptoms among weekly/monthly wear patients. Eye Contact Lens. 2010;36:215–219. doi:10.1097/ICL.0b013e3181e5859f
18. Rutschilling R, Fogt JS. Wear experience of a water surface daily disposable contact lens in existing silicone hydrogel planned replacement lens wearers. Clin Optom. 2022;14:27–34. doi:10.2147/OPTO.S353666
19. Harris PA, Taylor R, Minor BL, et al. The redcap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
20. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (redcap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi:10.1016/j.jbi.2008.08.010
21. Fogt JS, Patton K. Long day wear experience with water surface daily disposable contact lenses. Clin Optom. 2022;14:93–99. doi:10.2147/OPTO.S367891
22. Caffery B, Begley C, Simpson T, et al. Contact lens dry eye questionnaire (CLDEQ). Invest Ophth Vis Sci. 1999;40:S909–S910.
23. Chalmers RL, Begley CG, Moody K, Hickson-Curran SB. Contact lens dry eye questionnaire-8 (Cldeq-8) and opinion of contact lens performance. Optometry Vision Sci. 2012;89:1435–1442. doi:10.1097/OPX.0b013e318269c90d
24. Robitzsch A. Why Ordinal variables can (almost) always be treated as continuous variables: clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. Front Educ. 2020;5. doi:10.3389/feduc.2020.589965
25. Fonn D. Targeting contact lens induced dryness and discomfort: what properties will make lenses more comfortable. Optom Vis Sci. 2007;84:279–285. doi:10.1097/OPX.0b013e31804636af
26. Begley CG, Caffery B, Nichols KK, Chalmers R. Responses of contact lens wearers to a dry eye survey. Optom Vis Sci. 2000;77:40–46. doi:10.1097/00006324-200001000-00012
27. Martin-Montanez V, Lopez-de la Rosa A, Lopez-Miguel A, et al. End-of-day dryness, corneal sensitivity and blink rate in contact lens wearers. Cont Lens Anterior Eye. 2015;38:148–151. doi:10.1016/j.clae.2015.01.003
28. Grant T, Tang A. A survey of contact lens wearers and eye care professionals on satisfaction with a new smart-surface silicone hydrogel daily disposable contact lens. Clin Optom. 2020;12:9–15. doi:10.2147/OPTO.S233328
29. Dumbleton KA, Guillon M, Theodoratos P, Patel T. Diurnal variation in comfort in contact lens and non-contact lens wearers. Optom Vis Sci. 2016;93:820–827. doi:10.1097/OPX.0000000000000920
30. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The Tfos international workshop on contact lens discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS37–TFOS70.
31. Chalmers RL, Keay L, Hickson-Curran SB, Gleason WJ. Cutoff score and responsiveness of the 8-item contact lens dry eye questionnaire (CLDEQ-8) in a large daily disposable contact lens registry. Contact Lens Anterio. 2016;39:342–352. doi:10.1016/j.clae.2016.04.005
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Evaluating the Performance of Verofilcon A Daily Disposable Contact Lenses in a Group of Heavy Digital Device Users
Schulze MM, Fadel D, Luensmann D, Ng A, Guthrie S, Woods J, Jones L
Clinical Ophthalmology 2023, 17:3165-3175
Published Date: 24 October 2023
