Back to Journals » Infection and Drug Resistance » Volume 16
Evaluation of the Antibacterial Activity of Quinoxaline Derivative Compound Against Methicillin-Resistant Staphylococcus aureus
Authors Elfadil A , Alzahrani AM, Abdullah H , Alsamhan H , Abujamel TS, Ahmed HE, Jiman-Fatani A
Received 15 December 2022
Accepted for publication 7 April 2023
Published 18 April 2023 Volume 2023:16 Pages 2291—2296
DOI https://doi.org/10.2147/IDR.S401371
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Abdelbagi Elfadil,1,2 Ahmad Mandeel Alzahrani,1 Hani Abdullah,1 Hamoud Alsamhan,3– 5 Turki S Abujamel,6,7 Hafsa Elawd Ahmed,8 Asif Jiman-Fatani1
1Department of Clinical Microbiology and Immunology, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 2Center of Research Excellence for Drug Research and Pharmaceutical Industries, King Abdulaziz University, Jeddah, Saudi Arabia; 3Department of Pharmaceutical Care, Ministry of National Guard-Health Affairs, Riyadh, Saudi Arabia; 4Department of Infectious Disease Research, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia; 5Department of Pharmacy Practice, College of Pharmacy, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 6Vaccines and Immunotherapy Unit, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia; 7Department of Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia; 8Department of Medicine, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
Correspondence: Ahmad Mandeel Alzahrani, Department of Clinical Microbiology and Immunology, Faculty of Medicine, King Abdulaziz University, P.O. Box 80205, Jeddah, 21589, Saudi Arabia, Tel +966 54 095 9911, Email [email protected]
Background: While the frequency of methicillin-resistant Staphylococcus aureus (MRSA) continues to rise globally, there is a fear regarding an increase in vancomycin resistance among S. aureus strains. As far back as the 1960s, MRSA was one of the world’s most prevalent antibiotic-resistant bacteria. Among hospitalized patients and community members, MRSA is the cause of a significant number of infections. As a result of its resistance to classical beta-lactam and, in some cases, vancomycin antibiotics, efforts must be made as soon as feasible to find a new approach to fighting MRSA.
Purpose: This study is designed to evaluate the antibacterial activity of quinoxaline derivative compound against MRSA in comparison with vancomycin as a reference drug.
Methods: Sixty MRSA isolates were subjected to susceptibility testing by broth microdilution method for quinoxaline derivative compound and vancomycin. Each drug’s minimal inhibitory concentration (MIC) was determined and compared.
Results: Among the sixty MRSA isolates, most of the quinoxaline derivative compound MIC findings (56.7%) were 4 μg/mL compared to vancomycin MIC values (63.3%) of 4 μg/mL. In comparison, 20% of quinoxaline derivative compound MIC readings were 2 μg/mL, while the vancomycin MIC results were 6.7%. However, the overall proportion of MIC readings at ≤ 2 μg/mL for both antibacterial agents was equal (23.3%). None of the isolates were resistant to vancomycin.
Conclusion: This experiment revealed that most MRSA isolates were associated with low MICs (1– 4 μg/mL) for quinoxaline derivative compound. Overall, the susceptibility of the quinoxaline derivative compound signifies a promising efficacy against MRSA and may set a novel treatment approach.
Keywords: antibiotic resistance, drug discovery, methicillin-resistant Staphylococcus aureus, minimum inhibitory concentration, quinoxaline, vancomycin
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is a contagious bacterium that is resistant to nearly all ß-lactam antibiotics, including penicillin, amoxicillin, methicillin, and oxacillin.1,2 MRSA develop resistance via hydrolysis of the ß-lactam ring renders it incapable of binding to the penicillin-binding protein (PBP)3 or via mecA gene encodes an alternative PBP2a with a low affinity for ß-lactam antibiotics.4
Hospital-acquired MRSA (HA-MRSA) has been documented since the 1960s and is rising steadily over time in the healthcare facilities.5–7 Community-acquired MRSA (CA-MRSA)8 emerged in the 1990s from long care facilities and individuals sharing objects settings9 as a simple skin infection but can quickly progress into life-threatening illnesses.10 MRSA have a capsule that protects their outermost layer and produces a slime layer that helps them bind to catheters, prosthetic valves, and prosthetic joints. MRSA also produces numerous toxins and enzymes that help them trigger the immune response and destroy healthy tissues.11–13
When penicillin was first used to treat Staphylococcus aureus infections in 1941, over 90% of Staphylococcal isolates were susceptible to penicillin.14 Nevertheless, penicillin resistance emerged swiftly, partially owing to natural bacterial evolution but exacerbated by humans’ misuse of these drugs.15,16 The incidence of disease caused by MRSA has increased drastically worldwide, and the bacteria continue to evolve and take on new molecular traits.17 There are growing public health concerns related to emerging of resistant to the last-resort of antibiotic therapy against MRSA. Researchers discovered the vancomycin-resistant Staphylococcus aureus (VRSA) strain in 2002, which is rising steadily over time in the healthcare facilities.18–20
Compound screening constitutes a viable source of lead molecules that might assist fill the drug discovery pipeline against MRSA.21 The current study aimed and designed to investigate whether a promising quinoxaline derivative compound is as good as vancomycin for inhibiting the growth of selected MRSA isolates using the broth microdilution method, determining the drug’s minimum inhibitory concentration (MIC), and establishing the levels of susceptibility following the Clinical and Laboratory Standards Institute (CLSI) guidelines.
Materials and Methods
Sample Collection
Sixty isolates of MRSA were evaluated in this study. They are obtained from the Department of Medical Laboratory Technology, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia. Isolates were preserved in glycerol and stored at −80°C. Prior to testing, all isolates were thawed and cultured on Mannitol salt agar (HiMedia, India) and incubated overnight at 37°C in an aerobic environment. By routine methods, colonies were previously identified for their catalase and tube coagulase tests. Sample collection was performed in agreement with the ethics and research committee of the Faculty of Applied Medical Sciences at King Abdulaziz University (No. 38-712-456) and complied with the Declaration of Helsinki. As the clinical isolates in this study were a part of the hospital’s routine laboratory procedure, the ethics committee exempted this research from informed consent.
Antibacterial Agents
Tested drugs against MRSA include quinoxaline derivative compound, obtained by (Fluorochem Ltd, UK) and Tostaf® 500 Vancomycin powder 500 mg/vial, obtained by (MediS, Tunisia).
Stock Solution Preparations
Quinoxaline derivative compound stock solution was prepared by dissolving 0.0048 g in 3 mL Dimethyl sulfoxide (DMSO) solvent. The final concentration of the stock solution at 1:100 is equal to 16 µg/mL.
Vancomycin stock solution was prepared by dissolving 0.0051 g in 8 mL sterile distilled water. The final concentration of the stock solution at 1:10 is equal to 64 µg/mL.
Inoculum Preparation
All samples (n=60) were cultured on Mannitol salt agar for 18±24 h before testing. Three to five well-isolated colonies of each sample were suspended in 2 mL saline and shaken vigorously on a vortex mixer. Inoculum suspension density was adjusted to 0.5 McFarland using a suspension turbidity detector (Biosan Densitometers - DEN-1B). All inoculum suspensions are diluted 1:150 in cation-adjusted Mueller–Hinton broth (CAMHB) - No.2 Control Cations (HiMedia, India). CAMHB was prepared according to the manufacturer’s instructions.
Broth Microdilution Method
The procedure for performing broth microdilution method is done as described by CLSI (M07-A9) protocol.22
CAMHB is dispensed in a sterile, plastic 96-well plate with round bottom wells. Each antibacterial drug in the experiment was conducted on a separate plate. Using a multichannel pipette, 100 µL of CAMHB were filled in columns 2–12. Column 1 was filled with 200 µL of antibacterial agents stock solution diluted to 1:100 with a final concentration equal to 16 µg/mL. Two-fold serial dilutions (log2 dilution ranges) were performed by transferring 100 µL from the first well to the 10th with the following consecutive concentrations (16, 8, 4, 2, 1, 0.5, 0.25, 0.12, 0.06, 0.03). Each column – from 1 to 11 – was filled with 100 µL of 1:150 0.5 McFarland bacterial suspension. Growth control wells (column 11) are drug-free wells that contain 100 µL of bacterial suspension and 100 µL of CAMHB. Column 12 (blank) contained 100 µL of CAMHB and 100 µL distilled water.
The plate is covered in a tight-fitting plastic bag and incubated at 35±2°C in an ambient air incubator for 24 hours without agitation.
Determination of Minimum Inhibitory Concentration
Minimum inhibitory concentration (MIC) is defined as the lowest concentration of a drug that will inhibit the visible growth of a microorganism. MIC results of the two antibacterial using the broth microdilution method were interpreted following the CLSI guidelines.22,23
Results
The susceptibility of MRSA isolates to vancomycin and quinoxaline derivative compound is determined using MIC test. Two-fold serial (log2 dilution ranges) concentrations were used for testing the quinoxaline derivative compound at 16 to 0.03 µg/mL. Results obtained for the MIC of both antibacterial drugs were between 8 and 1 µg/mL. The quinoxaline derivative compound’s results were compared with vancomycin as a reference drug.
As presented in Table 1, out of the sixty MRSA isolates included in this study, the majority of the quinoxaline derivative MIC results (56.7%) were 4 µg/mL, whereas the vancomycin MIC results represent (63.3%). In contrast, 20% of quinoxaline derivative MIC results were 2 µg/mL compared with vancomycin MIC results, which showed only 6.7%. However, the total percentage of MIC results of both drugs at ≤2 µg/mL were identical (23.3%).
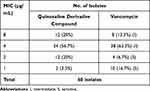 |
Table 1 Comparison of MIC Results of MRSA Isolates Between Quinoxaline Derivative Compound and Vancomycin |
Results also revealed that 20% of isolates tested for quinoxaline derivative were 8 µg/mL compared to 13.3% for vancomycin. Only 3.3% of isolates showed a remarkable 1 µg/mL MIC for quinoxaline derivative compared to 16.7% of isolates tested for vancomycin. The MIC results of 4 µg/mL for both drugs were similar in 35% of total isolates.
According to CLSI, vancomycin-intermediate Staphylococcus aureus (VISA) are those isolates with MIC between 4 and 8 µg/mL, whereas the MIC results ≥16 µg/mL is vancomycin-resistant.22 Accordingly, 76.7% of total isolates are found to be intermediate against vancomycin, while 23.3% are vancomycin-sensitive Staphylococcus aureus (VSSA). None of the isolates were found to be resistant to vancomycin, ie, MIC ≥16 μg/mL.
Discussion
The establishment and spread of vancomycin resistance make the treatment of MRSA more difficult.24 To our knowledge, research to assess the efficacy of this quinoxaline derivative compound in treating MRSA infections has not yet been utilized. Therefore, the results from this study indicate that quinoxaline derivative compound might offer a new therapeutic method for MRSA infections as an alternative to vancomycin. No appreciable differences in the MICs between the quinoxaline derivative compound and vancomycin were found in this investigation.
The MIC and vancomycin exposure, as assessed by the area underneath the concentration curve, are the most important pharmacokinetic–pharmacodynamic indices for optimizing bacterial lysis and patient outcomes with vancomycin treatment. For modern vancomycin administration, an area under the concentration curve/MIC index goal of 400 mg/L hour is advised. Midway through the twenty-first century, CLSI lowered the S. aureus vancomycin MIC susceptibility breakpoint to 2 µg/mL. Since then, however, a number of separate investigations have established relationships between isolates with vancomycin MICs within the resistant range with patient outcomes.25 The results from this study indicate that no sensitivity findings for either drugs were related to high MICs. The Centers for Disease Control and Prevention (CDC) guidelines, on the other hand, are to view these strains as possibly intermediate. They advise additional testing as well as research into the condition of the patient for vancomycin treatment, including probable reaction to vancomycin therapy. Additionally, to completely comprehend the epidemiology, microbiology, and pathophysiology of MRSA infections and to choose the effective preventive and treatment measures, more information from well-designed research is required.26
The current study is considered as an introduction to future studies aimed to investigating the effect of quinoxaline derivatives compound at the cellular and molecular levels and the possibility of emergence of MRSA resistance to this compound. Cell wall thickening as well as, presumably, the movement of genetic material, are considered to explain the growth of vancomycin resistance. Vancomycin functions by binding permanently to the terminal d-alanyl-d-alanine of bacterial cell wall substrates, limiting cell wall biosynthesis by targeting the regions important for cell wall synthesis. Resistance in VISA strains is considered to develop due to variations in peptidoglycan biosynthesis. VISA strains synthesis additional peptidoglycan with higher levels of D-alanyl-D-alanine residues. Because these residues attach to vancomycin molecules, they can efficiently sequester the antibiotic, thus preventing it from accessing the bacteria it was designed to kill. Moreover, the newly changed cell walls containing attached vancomycin further restrict the movement of drug molecules. Those genes that code for the graRS two-component regulatory structure were among the genes reported to be elevated in VISA strains. This regulatory system was given its name for its link with glycopeptide susceptibility. A further two-component regulatory system known as graRS is responsible for regulating the expression of the ABC transporter permease that is encoded by the vraG gene. This transporter is a constituent of an ATP-binding sequence. It was discovered that graRS is a significant factor in the VISA-type susceptibility that is present in some cellular strains of Staphylococcus aureus. The deletion of the vraG gene produced this hypersensitivity to vancomycin in the VISA strain Mu50. The isolate was sequenced, and the results showed that it had a shortened YycH protein and an amino acid alteration in the vraG gene.27
As we search for a new drug to treat MRSA, preventing and controlling infection caused by MRSA is one of the most important problems to solve. Colonization, exposure to infected skin or fomites, impaired host defenses, and other factors may all play a role in the spread of the infection. The degree to which various techniques have been successful in controlling MRSA has varied significantly. MRSA has been kept at a low incidence in many European nations due to active surveillance cultures and contact restrictions; this has been accomplished by these nations with or without decolonization (such as Finland, Netherlands, and France). Other nations have also had difficulty bringing their MRSA outbreaks under control, although they have made progress (such as Canada and Germany). The United States and Japan are two of the nations that have the highest rates of MRSA infection.28
Conclusion
The spread of multidrug-resistant Staphylococcus aureus in hospitals and community is a public health threat and a major hurdle in the treatment of MRSA infection. Because of the promising antibacterial activity against MRSA compared to vancomycin, further drug discovery research and development for this quinoxaline derivative compound is warranted.
Abbreviations
MRSA, methicillin-resistant Staphylococcus aureus; MIC, minimum inhibitory concentrations; CLSI, Clinical and Laboratory Standards Institute; VRSA, vancomycin-resistant Staphylococcus aureus; VISA, vancomycin-intermediate Staphylococcus aureus; VSSA, vancomycin-sensitive Staphylococcus aureus; PBP, penicillin-binding protein; HA-MRSA, hospital-acquired MRSA; CA-MRSA, community-acquired MRSA; DCD, Centers for Disease Control and Prevention; CAMHB, cation-adjusted Mueller–Hinton broth (CAMHB); DMSO, dimethyl sulfoxide; ATP, adenosine triphosphate.
Funding
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, under grant no. (G: 304-140-1441). The authors, therefore, acknowledge with thanks DSR for technical and financial support.
Disclosure
The authors report no conflict of interest in this work.
References
1. Bartels MD, Worning P, Andersen LP, et al. Repeated introduction and spread of the MRSA clone t304/ST6 in Northern Europe. Clin Microbiol Infect. 2021;27(2):284.e1–284.e5. doi:10.1016/j.cmi.2020.05.004
2. Masimen MAA, Harun NA, Maulidiani M, Ismail WIW. Overcoming methicillin-resistance Staphylococcus aureus (MRSA) using antimicrobial peptides-silver nanoparticles. Antibiotics. 2022;11(7). doi:10.3390/antibiotics11070951
3. Umar Zango U, Ibrahim M, Abdurrahman Abubakar Shawai S, Muhammad Shamsuddin I. A review on β-lactam antibiotic drug resistance. MOJ Drug Des Develop Ther. 2019. doi:10.15406/mojddt.2019.03.00080
4. Ba X, Harrison EM, Edwards GF, et al. Novel mutations in penicillin-binding protein genes in clinical Staphylococcus aureus isolates that are methicillin resistant on susceptibility testing, but lack the mec gene. J Antimicrob Chemother. 2014;69(3):594–597. doi:10.1093/jac/dkt418
5. Figueiredo AMS. What is behind the epidemiological difference between community-acquired and health-care associated methicillin-resistant Staphylococcus aureus? Virulence. 2017;8(6):640–642. doi:10.1080/21505594.2017.1335847
6. Safdari H, Aryan E, Sadeghian H, Shams SF, Aganj M. Frequency of methicillin-resistant Staphylococcus aureus (MRSA) in nose and cellular phone of medical and non-medical personnel of emergency departments of Ghaem hospital in Mashhad city. Clin Epidemiol Glob Health. 2020;8(4):1043–1046. doi:10.1016/j.cegh.2020.03.017
7. Henderson A, Nimmo GR. Control of healthcare- and community-associated MRSA: recent progress and persisting challenges. Br Med Bull. 2018;125(1):25–41. doi:10.1093/bmb/ldx046
8. Rodríguez F, Salinas C, Fernández S, et al. Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) clones from Paraguayan children. J Infect Dev Ctries. 2020;14(3):290–297. doi:10.3855/jidc.12108
9. Weber K. Community-associated methicillin-resistant Staphylococcus aureus infections in the athlete. Sports Health. 2009;1(5):405–410. doi:10.1177/1941738109343653
10. Mahmoud ERA, Ahmed HAH, Abo-senna ASM, Riad OKM, Abo-Shadi MM. Isolation and characterization of six gamma-irradiated bacteriophages specific for MRSA and VRSA isolated from skin infections. J Radiat Res Appl Sci. 2021;14(1):34–43. doi:10.1080/16878507.2020.1795564
11. Mirani ZA, Naz S, Khan F, et al. Antibacterial fatty acids destabilize hydrophobic and multicellular aggregates of biofilm in S. aureus. J Antibio. 2017;70(2):115–121. doi:10.1038/ja.2016.76
12. Cheung GYC, Bae JS, Otto M. Pathogenicity and virulence of Staphylococcus aureus. Virulence. 2021;12(1):547–569. doi:10.1080/21505594.2021.1878688
13. Chen J, Zhou H, Huang J, Zhang R, Rao X. Virulence alterations in Staphylococcus aureus upon treatment with the sub-inhibitory concentrations of antibiotics. J Adv Res. 2021;31:165–175. doi:10.1016/j.jare.2021.01.008
14. Livermore DM. Antibiotic resistance in staphylococci. Int J Antimicrob Agents. 2000;16:3–10. doi:10.1016/S0924-8579(00)00299-5
15. Mancuso G, Midiri A, Gerace E, Biondo C. Bacterial antibiotic resistance: the most critical pathogens. Pathogens. 2021;10:10. doi:10.3390/pathogens10101310
16. Samreen AI, Malak HA, Abulreesh HH, Abulreesh HH. Environmental antimicrobial resistance and its drivers: a potential threat to public health. J Glob Antimicrob Resist. 2021;27:101–111. doi:10.1016/j.jgar.2021.08.001
17. Guo Y, Song G, Sun M, Wang J, Wang Y. Prevalence and therapies of antibiotic-resistance in Staphylococcus aureus. Front Cell Infect Microbiol. 2020;10:10. doi:10.3389/fcimb.2020.00107
18. Wu Q, Sabokroo N, Wang Y, Hashemian M, Karamollahi S, Kouhsari E. Systematic review and meta-analysis of the epidemiology of vancomycin-resistance Staphylococcus aureus isolates. Antimicrob Resist Infect Control. 2021;10(1). doi:10.1186/s13756-021-00967-y
19. Liu WT, Chen EZ, Yang L, et al. Emerging resistance mechanisms for 4 types of common anti-MRSA antibiotics in Staphylococcus aureus: a comprehensive review. Microb Pathog. 2021;156:104915. doi:10.1016/j.micpath.2021.104915
20. Finks J, Wells E, Dyke TL, et al. Vancomycin-resistant Staphylococcus aureus, Michigan, USA, 2007. Emerg Infect Dis. 2009;15(6):943–945. doi:10.3201/eid1506.081312
21. Porras G, Chassagne F, Lyles JT, et al. Ethnobotany and the role of plant natural products in antibiotic drug discovery. Chem Rev. 2021;121(6):3495–3560. doi:10.1021/acs.chemrev.0c00922
22. Clinical and Laboratory Standards Institute (CLSI). M07-A9: methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—Ninth edition. Available from: www.clsi.org.
23. Clinical and Laboratory Standards Institute (CLSI). M100-S22: performance standards for antimicrobial susceptibility tests; susceptibility breakpoints for antimicrobial susceptibility testing—Twenty Eighth edition; 2018. Available from: www.clsi.org.
24. Guthridge I, Smith S, Law M, Binotto E, Hanson J. Efficacy and safety of intravenous lincosamide therapy in methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2021;65(9). doi:10.1128/AAC.00343-21
25. Phillips C, Wells N, Martinello M, Smith S, Woodman R, Gordon D. Optimizing the detection of methicillin-resistant Staphylococcus aureus with elevated vancomycin minimum inhibitory concentrations within the susceptible range. Infect Drug Resist. 2016;87. doi:10.2147/IDR.S107961
26. Gorwitz RJ, Jernigan DB, Powers JH, Jernigan JA. Strategies for Clinical Management of MRSA in the Community: summary of an experts’ meeting convened by the centers for disease control and prevention participants in the Centers for Disease Control and Prevention-Convened Experts’ Meeting on Management of MRSA in the Community; 2006. Available from: http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.html.
27. Howden BP, Davies JK, Johnson PDR, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010;23(1):99–139. doi:10.1128/CMR.00042-09
28. Harris A. Methicillin-resistant Staphylococcus aureus (MRSA) in adults: prevention and control. Available from: https://www.uptodate.com/contents/methicillin-resistant-staphylococcus-aureus-mrsa-in-adults-prevention-and-control.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
