Back to Journals » International Journal of General Medicine » Volume 16
Evaluation of Proton Pump Inhibitors Prescribing Among Hospitalized Patients: A Cross-Sectional Study
Authors Abukhalil AD , Ali O, Saad A, Falana H , Al-Shami N , Naseef HA , Rabba A
Received 4 November 2022
Accepted for publication 4 January 2023
Published 11 January 2023 Volume 2023:16 Pages 141—150
DOI https://doi.org/10.2147/IJGM.S396202
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdallah Damin Abukhalil, Ola Ali,* Asmaa Saad,* Hiba Falana, Ni’meh Al-Shami, Hani A Naseef, Abdullah Rabba
Pharmacy Department, Faculty of Pharmacy, Nursing and Health Professions, Birzeit University, Birzeit, West Bank, Palestine
*These authors contributed equally to this work
Correspondence: Abdallah Damin Abukhalil; Hiba Falana, Pharmacy Department, Faculty of Pharmacy, Nursing and Health Professions, Birzeit University, Birzeit, West Bank, Palestine, Tel +970-5-98204036 ; +970-5-9519486, Fax +970-2-2982017, Email [email protected]; [email protected]
Background: Proton pump inhibitors (PPIs) are the most effective agents for managing acid-related disorders. However, inappropriate prescribing of PPIs is becoming an issue of concern.
Objective: This study aimed to assess the appropriate utilization of PPIs in terms of indication, dose, frequency, and route of administration during admission and discharge. Furthermore, direct costs associated with inappropriate PPI use were calculated.
Methods: A descriptive cross-sectional study was conducted at the internal medicine department of a tertiary hospital in Palestine from January 1, 2021, to June 30, 2021. The medical records of patients aged 18 years or older, hospitalized for 48 hours or more, and receiving oral or intravenous (IV) PPIs during their stay were collected and evaluated for the appropriateness of PPIs prescribed according to clinical guidelines.
Results: Of 262 patients, 80.2% had an appropriate indication for prophylaxis (67.6%) or treatment (12.6%). A total of 230 patients were prescribed IV pantoprazole.182 (79.1%) had an appropriate indication, whereas 122/182 (67%) received IV PPI instead of oral without an appropriate indication. Of the 32 patients who received 20 mg of oral omeprazole, 28 (87.5%) had an appropriate indication, dose, and route of administration, whereas 16/28 (57.1%) had an inappropriate frequency. At discharge, 32.5% of patients were discharged with unnecessary PPI prescriptions. The total direct cost of inappropriate PPI Indications and route of administration in 188 patients over six months was $1518.
Conclusion: This study showed that most patients received a PPI for an appropriate indication with the correct dose. However, a high prevalence of inappropriate IV pantoprazole administration was observed, resulting in the highest costs, demonstrating the importance of correctly ordering IV medications. Adherence to clinical guidelines, such as those of the American College of Gastroenterology (ACG), will improve the appropriateness of PPI prescribing, prevent complications, and reduce healthcare costs.
Keywords: PPIs, proton pump inhibitors, indication, IV-PO switch, cost-saving, pantoprazole, omeprazole, Palestine
Introduction
Proton pump inhibitors (PPIs) are the most commonly prescribed antisecretory agents worldwide because of their high efficacy and safety. PPIs suppress gastric acid secretion by inhibiting the H+/K+ ATPase pump in gastric parietal cells, thereby increasing gastric pH.1,2 PPIs are indicated for the treatment of gastrointestinal disorders, including gastroesophageal reflux disease (GERD) and peptic ulcers, stress ulcer prophylaxis (SUP), prevention of NSAID-induced gastric ulcers, and antiplatelet-induced gastrointestinal bleeding in high-risk patients.3–6 IV PPIs are also indicated in medical conditions such as before endoscopy for acute upper gastrointestinal bleeding (UGIB), post-endoscopic gastric and duodenal ulcer bleeding for 72 hours, and critically ill patients with nothing by mouth status (NPO).7,8
The inappropriate use of PPIs is becoming an issue of concern because of adverse events and increased healthcare costs. Several side effects are associated with inappropriate or chronic PPI use. Complications include hypomagnesemia, rebound hyperacidity, vitamin B12 deficiency, increased risk of enteric Clostridium difficile infection, community-acquired pneumonia, acute interstitial nephritis, and osteoporosis-induced bone fractures.9 Drug-drug interactions have been reported in many studies.10 In addition, PPI overuse is associated with increased healthcare costs. PPIs come after statin medications in terms of global expenditure, estimated at over $11 billion annually in the US At the same time, UK data indicate that approximately 100 million pounds and 2 billion pounds are spent uselessly nationally and worldwide, respectively.11,12
Studies have shown that many PPI prescriptions are initiated in hospitals without a valid indication, with 22–79% of prescriptions continued on discharge.13–16 A regional study that examined the inappropriate prescribing of PPIs among hospitalized patients in Jordan showed poor adherence to current practice guidelines, and 70% of patients received a PPI with no valid indications.17 Furthermore, in a study in Saudi Arabia, the estimated yearly cost of inappropriate IV PPI at an academic medical center was $156,044.18
Studies assessing the appropriateness of PPI prescriptions for hospitalized patients in Palestine are lacking. Therefore, this study aimed to evaluate the appropriate use of PPIs regarding indication, dose, frequency, and route of administration during admission and discharge and to assess the direct cost associated with inappropriate PPI therapy.
Methodology
Type and Sample of the Study
This descriptive, retrospective, cross-sectional study was conducted at a tertiary hospital in Palestine. The study included patients aged ≥ 18 who were admitted or transferred to the Department of Internal Medicine between January 1, 2021, and June 30, 2021, and received oral or IV PPIs during their stay in the Department of Internal Medicine. (Figure 1) Patients with less than 48 hours of hospital stay, diagnosed with septic shock, transferred to other departments, died, did not receive a PPI, and patients with incomplete medical information were excluded from the study.
 |
Figure 1 Patients flowchart. |
Data Collection
Data were obtained from the electronic medical records of the hospital. Data included age, sex, length of stay, medical history, medication history, the reason for admission, PPI regimen (dose, frequency, route of administration, and duration of use), and G.I. risk medications during hospitalization and discharge. G.I. risk medications include anticoagulants, antiplatelets, glucocorticoids, and NSAIDs.
Assessment of Appropriateness of PPI Therapy
Two clinical pharmacists and two senior Pharm-D students assessed the appropriateness of PPI prescriptions based on the American College of Gastroenterology (ACG) clinical guidelines.3,8,19 All PPI orders, either for treatment or prophylaxis, were evaluated in terms of dose, frequency, and route of administration.20–23
Patients on PPIs were categorized into three groups: on PPIs indicated for G.I. treatment, PPIs indicated for prophylaxis, and others with no valid indication. Indications for PPI treatment include UGIB, NSAID-induced ulcers, and PUD. Indications for prophylaxis with a PPI include patients prescribed PPIs for NSAIDs-induced ulcer prevention, SUP, patients taking ≥2 antithrombotic, concomitant use of NSAID and steroids, and prior history of gastrointestinal bleeding. Patients prescribed PPIs for a valid indication and/or in an appropriate dosage form for at least one day where deemed appropriate. Indications for IV PPIs were considered appropriate if the patient had UGIB symptoms, nausea, vomiting, and NPO. Simultaneously, the IV dosage form was considered unjustified for patients who can tolerate oral medications without a clear indication for an IV route of administration.
Cost Analysis
The cost avoidance calculations associated with the inappropriate use of PPIs were performed manually based on the number of days of inappropriate PPI use, including inappropriate indications and missed opportunities to switch from IV to oral formulations. The frequency of PPI use was multiplied by the cost and the number of inappropriate PPI use days. The cost avoidance calculations were based on the actual cost of the product and did not include administration or nursing time.
Statistical Analysis
The data collected from the records were entered into the SPSS statistical package for social science (version 22.0.0.0) and then identified, categorized, recoded, and analyzed.
Descriptive analysis was performed for categorical data, expressed as frequencies and percentages, and continuous data expressed as means and standard deviations. In addition, chi-square and fisher’s exact tests were used to assess the association between the appropriateness of PPI prescription during admission and discharge with the patient’s age, gender, comorbidities, and the number of past and discharged G.I. risk medications. P-values less than 5% were considered statistically significant.
Ethical Considerations
This study was approved by the Ethical Committee of Birzeit University (reference number BZUPNH2104). Moreover, the requirement to obtain written patient consent was waived because this was a retrospective study and patient information was anonymous. The study complied with the ethical guidelines of the Declaration of Helsinki and patient data.
Results
Patient Characteristics
Of the 1827 patients, 262 who received PPIs during hospital admission had complete health records and met the inclusion criteria (Figure 1). The average age of the participants was (60.91±17.438), 139 (53.1%) were less than 65 years, and 144 (55%) were male. More than 50% of the participants had more than three comorbidities. One hundred (38.2%) patients were on antiplatelet therapy before hospital admission, whereas 181 (69.1%) patients took oral anticoagulants during admission. (Table 1).
 |
Table 1 Characteristics of Patients Prescribed PPI (N=262) |
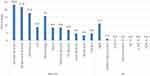
Figure 2 shows the participants’ medical histories: 53.4% of the sample had three or more comorbidities, half of the patients had a history of HTN, 40% had diabetes, and 42.7% had CVD.
 |
Figure 2 Past Medical History (N=262). *Others: benign prostatic hyperplasia, malignant tumors, infections, retinopathy, constipation, liver disorders, and hernia. |
Figure 3 shows the reasons for hospital admission; 85.9% of the participants presented with non-GI complications, such as renal, respiratory, and CNS disorders (23.3%, 21.8%, and 17.9%, respectively). Regarding G.I. disorders, 14.1% had G.I. complications, and 11.1% presented with UGIB.
PPI Regimen During Admission
Of 262 admitted patients, 230 (87.8%) received 40 mg intravenous pantoprazole, and 32 (12.2%) received 20 mg oral omeprazole either once or twice a day. Of the 230 patients who received IV PPIs, 182 (79.1%) had an appropriate PPI indication, dosage, and frequency. In contrast, 122/182 (67%) patients had an inappropriate route of administration. For patients receiving oral PPIs, 28/32 (87.5%) were prescribed PPI for an appropriate indication with the correct dosage and route of administration. However, 16/28 of (57.1%) patients had an inappropriate frequency (Figure 4).
 |
Figure 4 Evaluation of the PPI regimen for patients who received PPI for appropriate indications during the hospital stay. |
Association Between Patients’ Characteristics and Appropriateness of PPI
Indication During Admission and Discharge
As shown in Table 2, of 262 admissions, 177 (67.6%) patients were prescribed PPI for prophylaxis indication, 33 (12.6%) patients were prescribed PPIs for treatment indication, and 52 (19.8%) were prescribed PPIs with no indications. Bivariate analysis revealed that patients aged < 65 years were significantly more likely to take PPI with no indication (26.6%) than those aged ≥ 65 years (12.2%) during admission (p = 0.007). Furthermore, patients not receiving high-risk G.I. medication before admission were significantly more likely to have PPI with no appropriate indication (27.4%) than those receiving two or three medications (8.8% and 0.0%, respectively (p = 0.016).
 |
Table 2 Association Between Patient Characteristics and Appropriateness of PPI Indications During Admission and Discharge |
Regarding PPI prescription at discharge, 203 (77.5%) patients were given a PPI. Of these, 137 (67.5%) patients had an appropriate indication, with only 15 patients discharged with a PPI for a specific duration of treatment, and 188 were discharged on a PPI for a non-specific duration of therapy. Chi-square results showed that patients aged < 65 years (50.5%) were significantly associated with a prescription of PPIs for no indication compared to patients aged 65 years and older (16.7%) (p < 0.001), in addition, patients with no comorbidities were at a higher risk of being discharged on PPIs inappropriately (60%) compared to patients with three or more comorbidities (25.2%) (p = 0.044). A total of 55.1% of patients discharged with no G.I. risk medications were more likely to be prescribed a PPI with inappropriate indications than those discharged with two or three medications (2.1% and 0.0%, respectively; p < 0.001) (Table 2).
Cost Analysis
The mean hospitalization days was 5.52±2.537, with a median of 5, IQR (4 and 7) days, a maximum length of 20 days, and a minimum of 2 days. As shown in Table 3, 1515.91 USD is the total cost avoidance for the study period. Most cost avoidance opportunities (65%) are associated with IV oral switching. For cost evaluation based on days of inappropriateness, the total number of days for inappropriate IV indication was 299, the number of inappropriate oral indications was 41 days, and 593 days for inappropriate IV route of administration required switching to oral administration.
 |
Table 3 Cost Effect of Inappropriate PPIs Indications and Route of Administration |
Discussion
This retrospective cross-sectional study is the first to address prescribing PPIs during hospitalization and at discharge at a tertiary hospital in Palestine. The two main PPIs on the hospital formulary were IV pantoprazole and oral omeprazole. The PPIs were assessed for indication, dose, frequency, and route of administration. Furthermore, the cost associated with inappropriate use was assessed and calculated.
The prescription of PPI with no valid indication for use was more prevalent among patients aged less than 65 years and patients not taking G.I. risk medication. Participants with these characteristics are less prone to G.I. complications and do not fulfill the criteria for using PPIs for treatment or prophylaxis indications. This finding was supported by a study that assessed factors associated with the inappropriate use of acid-suppressive inhibitors and stated that patients with no past G.I. risk medications had higher odds of being prescribed AST inappropriately.24 This finding reflects the practitioner’s behavior in prescribing PPIs to most patients upon admission and discharge rather than not prescribing them because PPIs are well-known drugs with reasonable safety profiles and few complications, making prescribers less hesitant to order and prescribe them. Many reports have shown that PPIs are associated with long-term complications such as osteoporosis, which increases the risk of C. difficile infection. In a recent study in Palestine, PPI use was associated with an increased risk of CDI among hospitalized patients.25 Furthermore, the appropriateness of PPI therapy was noted as related to the patient gender and the number of comorbidities.
Most patients in the study were prescribed PPIs for an appropriate indication, with only 20% being prescribed PPIs without a clear indication. The most appropriate indication was for G.I. bleeding prevention owing to the combined use of antiplatelet agents and anticoagulants in patients older than 65 years, followed by SUP-and NSAIDs NSAID-induced ulcer prevention which is similar to the findings of a similar study that was conducted in a tertiary hospital in Malaysia, where PPI use was inappropriate in 19% of 153 patients.26 Other studies conducted in Saudi Arabia, Portugal, and Shanghai found higher rates of inappropriate use; 76.4%, 61.5%, and 47%, respectively.24,27,28
In this study, antiplatelet and anticoagulants were prescribed in 46.2% and 69.1% of the cases, respectively. The use of these drugs, alone or combined with other G.I. risk factors, contributed to a high percentage of PPI orders for ulcer prophylaxis. However, although beyond the scope of this study, the appropriate indication of antithrombotic drug use should be assessed for appropriate indications because of the finding of a recent study that assessed venous thromboembolism (VTE) prophylaxis among medical patients in Palestine. The study reported overuse of anticoagulants without proper indication. Hence, prescribing PPIs might have resulted from a prescribing cascade in these patients.29
Regarding the dose of the PPIs prescribed to the participant, of the 182 patients who received IV 40 mg pantoprazole, all patients were given the correct dose, except for one with an inappropriate frequency. For prophylaxis indications, all patients received a correct dose of pantoprazole 40 mg once daily. For omeprazole, of the 28 patients who received it, all were prescribed a higher dose of 20 mg twice daily for gastric prophylaxis, where 20 mg daily was more appropriate.21 This result is higher than that of a similar regional study conducted in Saudi Arabia, where the appropriate dose of acid-suppressive therapy (AST) was only 12.7% of patients (n= 256).24
The high trend of inappropriate IV pantoprazole use was evident in this study. Of 182 patients with appropriate indications for pantoprazole use, 67% had an inappropriate IV route of administration. Some Patients were administered IV PPIs without a valid indication, such as suspected UGIB, NPO, and severe nausea and vomiting. In these situations, oral PPI is preferred to reduce complications, cost, nursing time, and effort in administering intravenous medications. Furthermore, some patients who were appropriately initiated on IV PPI therapy were not switched when they became candidates for oral PP leading to an increased risk of infections, adverse effects, and financial burden on the hospital. A similar finding in regional studies was seen in a study conducted in Saudi Arabia, where IV pantoprazole was inappropriately prescribed in 62.2% (n=74) and 68.3% (n= 100) of cases.18,23 Furthermore, 52 patients with no valid indication for PPI therapy were 92.3% inappropriately administered intravenous pantoprazole. This finding is similar to studies in Brazil and Labuan, which reported that 76.6% of 333 patients received IV omeprazole and 85% of 117 patients received IV pantoprazole and esomeprazole, with no indication.30 Inappropriate prescribing of IV medication where patients qualify for oral drug administration continues to be an opportunity for healthcare cost saving. Hospitals need to develop clear protocols for ordering IV medications and Where physicians and clinical pharmacists assess the appropriateness of oral versus IV dosage forms.
The most drug-related problems associated with prescribing PPIs on discharge were indication and duration of treatment. Most patients (77.5%) were discharged on a PPI, with only 32.5% having a valid indication. This finding is lower than a study conducted in Portugal, which reported that 62.3% of patients (n=171) were discharged on PPIs with no indication.27 Furthermore, 92.6% of patients were discharged on PPIs without a specific duration of treatment. Not specifying the treatment duration can cause patients to continue taking the medication for an extended period, masking major GI complications or causing long-term side effects associated with PPI use. The long-term consumption of PPIs leads to health complications, including Clostridium difficile and peritonitis infection, hypomagnesemia, B12 deficiency, pneumonia, bone fracture, dementia, and chronic kidney disease. Furthermore, it is associated with an increased financial burden on the healthcare systems and patients.
The cost associated with inappropriate PPI use during hospital admission were calculated. A total cost of 1515.91 USD would have been saved in 6 months if PPIs were appropriately prescribed to 188 patients in terms of indication and route of administration. Most of the cost burden (65%) was attributed to the incorrect use of the IV route when oral PPIs were more appropriate. For example, an oral Pantoprazole tablet costs $0.04 compared to $1.70 for an IV vial. Therefore, using the correct route will decrease costs and highlight the importance of appropriate PPI prescription.
Similar studies have the cost burden of improper use of PPIs. For example, a study performed in Brazil showed that the cost of inadequate prescription of IV PPIs was $1696 in six months.30 Also, a study conducted in Saudi Arabia indicated that the total annual cost of an inadequate prescription of IV PPI was 585,167 Saudi Riyal (SAR) (156,044 USD).18 A Lebanese study found that the semi annual cost of inappropriate use of PPIs is $17,732.5 in terms of indication and $14,571 in the appropriate route of administration.31 This cost was calculated from the actual drug cost, reflecting direct cost savings. At the same time, indirect cost savings, including nurse time for drug preparation and administration, were not measured but would also be affected if PPIs were correctly prescribed.
The inappropriateness of PPI prescriptions can be minimized by implementing stewardship programs necessary to reduce inappropriate prescribing, prevent complications, and save time and money. In addition, providing continuing education and evaluating the healthcare staff’s level of knowledge is also essential to increase awareness about the criteria for appropriate prescribing of PPIs, improve staff practice and behavior, and decrease the inappropriate utilization of PPIs.
Limitations and Strengths
This study had several strengths, including the sample size over a reasonable period of six months, which is comparable with other similar studies and considered sufficient to reflect the trends of PPIs use in clinical practice. In addition, patients were not randomly selected; all patients admitted during the study period were examined case by case, and those who fulfilled the inclusion criteria were included in the study.
However, this study has some limitations. First, the study was conducted in a single tertiary hospital in Palestine; therefore, the results cannot be generalized to other clinical settings. Second, the number of patients with a short hospital stay of less than 48h was significant; they were not included in this study, which may have underestimated the appropriateness of PPIs. Third, it is noteworthy that the study was conducted only on PPIs and did not consider other acid suppression medications, such as H2 antagonists. Furthermore, patient information on over-The-counter PPI and PPI prescribed by primary care providers is unavailable. Finally, we did not examine the specialty of PPI prescribers.
Conclusion
This study showed that most patients were prescribed a proper dose for an appropriate indication, with a high prevalence of inappropriate IV PPIs, increasing healthcare costs and demonstrating the importance of adequately ordering IV medications. In addition, most patients were discharged on PPIs without a specific duration, leading to unnecessary use. Commitment to clinical guidelines, such as the American College of Gastroenterology (ACG) guidelines, will improve the appropriateness of PPIs prescription regimens, prevent complications, and reduce healthcare costs.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Strand DS, Kim D, Peura DA. 25 years of proton pump inhibitors: a comprehensive review. Gut Liver. 2017;11(1):27–37. doi:10.5009/gnl15502
2. Sachs G, Shin JM, Howden CW. Review article: the clinical pharmacology of proton pump inhibitors. Aliment Pharmacol Ther. 2006;23(Suppl s2):2–8. doi:10.1111/j.1365-2036.2006.02943.x
3. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):27–56. doi:10.14309/ajg.0000000000001538
4. Fallone CA, Chiba N, van Zanten SV, et al. The Toronto consensus for the treatment of helicobacter pylori infection in adults. Gastroenterology. 2016;151(1):51–69.e14. doi:10.1053/j.gastro.2016.04.006
5. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of helicobacter pylori infection. Am J Gastroenterol. 2017;112(2):212–239. doi:10.1038/ajg.2016.563
6. Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728–738. doi:10.1038/ajg.2009.115
7. Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2021. Endoscopy. 2021;53(3):300–332. doi:10.1055/a-1369-5274
8. Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI. ACG clinical guideline: upper gastrointestinal and ulcer bleeding. ACG. 2021;116(5):899–917.
9. Boghossian TA, Rashid FJ, Thompson W, et al. Deprescribing versus continuation of chronic proton pump inhibitor use in adults. Cochrane Database Syst Rev. 2017;3(3):Cd011969. doi:10.1002/14651858.CD011969.pub2
10. Yibirin M, De Oliveira D, Valera R, Plitt AE, Lutgen S. Adverse effects associated with proton pump inhibitor use. Cureus. 2021;13(1):e12759. doi:10.7759/cureus.12759
11. Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol. 2012;5(4):219–232. doi:10.1177/1756283X12437358
12. Forgacs I, Loganayagam A. Overprescribing proton pump inhibitors. BMJ. 2008;336(7634):2–3. doi:10.1136/bmj.39406.449456.BE
13. Zink DA, Pohlman M, Barnes M, Cannon ME. Long-term use of acid suppression started inappropriately during hospitalization. Aliment Pharmacol Ther. 2005;21(10):1203–1209. doi:10.1111/j.1365-2036.2005.02454.x
14. Yap MH, Yip G, Edwards A, D’Intini V, Tong E. Appropriateness of proton pump inhibitor use in patients admitted under the general medical unit. J Pharm Pract Res. 2019;49(5):447–453. doi:10.1002/jppr.1548
15. Souaid CK, Maalouf RG, Hallit S, Akiki B, Dagher E. Relevance of proton pump inhibitors prescriptions in a tertiary care hospital in Lebanon. Arab J Gastroenterol. 2020;21(3):194–198. doi:10.1016/j.ajg.2020.07.008
16. Nachnani JS, Bulchandani D, Moormeier J, Foxworth J. Patient and physician predictors of inappropriate acid-suppressive therapy (AST) use in hospitalized patients. J Hosp Med. 2009;4(8):E10–E14. doi:10.1002/jhm.492
17. Zalloum N, Farha RA, Awwad O, Samara N. Inappropriate prescribing of proton pump inhibitors among patients in two Jordanian tertiary health facilities. Trop J Pharm Res. 2016;15(11):2489. doi:10.4314/tjpr.v15i11.26
18. Mohzari YA, Alsaegh A, Basheeruddin Asdaq SM, Al Shanawani SN, Albraiki AA, Bagalb A. The pattern of intravenous proton-pump inhibitor utilization at an academic medical center in Riyadh, Saudi Arabia. J Res Pharm Pract. 2020;9(3):151–154. doi:10.4103/jrpp.JRPP_20_62
19. Gastroenterology ACo. Guidelines - American College of Gastroenterology; 2022. Available from: https://gi.org/guidelines/.
20. Graham DY, Tansel A. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16(6):800–808.e807. doi:10.1016/j.cgh.2017.09.033
21. UpToDate. Omeprazole: drug information; 2022. Available from: https://uptodatefree.ir/topic.htm?path=omeprazole-drug-information#F203562.
22. UpToDate. Pantoprazole: drug information; 2022. Available from: https://uptodatefree.ir/topic.htm?path=pantoprazole-drug-information.
23. Grube RR, May DB. Stress ulcer prophylaxis in hospitalized patients not in intensive care units. Am J Health Syst Pharm. 2007;64(13):1396–1400. doi:10.2146/ajhp060393
24. Korayem GB, Alkanhal R, Almass R, et al. Patients, prescribers, and institutional factors associated with inappropriate use of acid suppressive therapy in medical wards: an experience of a single-center in Saudi Arabia. Int J Gen Med. 2021;14:5079–5089. doi:10.2147/IJGM.S328914
25. Abukhalil AD, AbuKhdeir L, Hamed M, et al. Characteristics, risk factors, and prevalence of clostridioides difficile among hospitalized patients in a Tertiary Care Hospital in Palestine. Infect Drug Resist. 2021;14:4681–4688. doi:10.2147/IDR.S333985
26. Elnaem MH, Mohamed MH, Bin Nazar AH. Evaluation of proton pump inhibitors prescribing among non-critically ill hospitalized patients in a Malaysian Tertiary Hospital. J Appl Pharm Sci. 2017;7:83.
27. Gamelas V, Salvado V, Dias L. Prescription Pattern of Proton Pump Inhibitors at Hospital Admission and Discharge. GE Port J Gastroenterol. 2019;26(2):114–120. doi:10.1159/000488506
28. Liu Y, Zhu X, Li R, Zhang J, Zhang F. Proton pump inhibitor utilisation and potentially inappropriate prescribing analysis: insights from a single-centred retrospective study. BMJ Open. 2020;10(11):e040473. doi:10.1136/bmjopen-2020-040473
29. Abukhalil AD, Nasser A, Khader H, et al. VTE prophylaxis therapy: clinical practice vs clinical guidelines. Vasc Health Risk Manag. 2022;18:701–710. doi:10.2147/VHRM.S382050
30. Marcon Bischoff L, Faraco L, Machado L, Bialecki A, Almeida G, Becker S. Inappropriate usage of intravenous proton pump inhibitors and associated factors in a high complexity hospital in Brazil. Arq Gastroenterol. 2021;58:32–38. doi:10.1590/s0004-2803.202100000-07
31. Nasser SC, Nassif JG, Dimassi HI. Clinical and cost impact of intravenous proton pump inhibitor use in non-ICU patients. World J Gastroenterol. 2010;16(8):982–986. doi:10.3748/wjg.v16.i8.982
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.