Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Evaluation of Policy Governing Herbal Medicines Regulation and Its Implementation in Ethiopia
Authors Demeke H, Hasen G , Sosengo T , Siraj J , Tatiparthi R , Suleman S
Received 4 April 2022
Accepted for publication 13 June 2022
Published 22 June 2022 Volume 2022:15 Pages 1383—1394
DOI https://doi.org/10.2147/JMDH.S366166
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Henok Demeke,1 Gemmechu Hasen,2 Teshome Sosengo,1 Jafer Siraj,3 Ramanjireddy Tatiparthi,2 Sultan Suleman2
1Pharmacy Department, College of Health and Medical College, Haramaya University, Haramaya, Oromia, Ethiopia; 2School of Pharmacy, Institute of Health, Jimma University, Jimma, Oromia, Ethiopia; 3School of Pharmacy, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman, Ethiopia
Correspondence: Gemmechu Hasen, Email [email protected]
Background: Ethiopia is one of the world’s oldest countries, with a fascinating history of herbal medicine. However, there is a lack of evidence for the regulatory framework for herbal medicines and its implementation. Thus, the aim of this study was to evaluate the policy governing herbal medicines regulation and its implementation in Ethiopia.
Methods and Materials: An archival review, a semi-structured interview with key informants, a cross-sectional study involving traditional healers, and an institution-based cross-sectional survey were conducted from June 15, 2020 to December 25, 2020. The qualitative data was transcribed using Microsoft Word 10, whereas the quantitative data was recorded and analyzed using SPSS 20 computer statistical software. The study’s findings are summarized using descriptive statistics. In addition, multiple logistic regressions were performed to identify factors affecting regulation of herbal medicine (HM) in Ethiopia. Variables with p< 0.05 were considered potential predictors.
Results: According to all key informants, Ethiopia has yet to adopt distinct policies and laws on herbal medicine that may provide an independent regulatory framework. Similarly, the majority of respondents in an institution-based survey indicated that there were no defined policies (n=52, 57.3%), laws (n=53, 59.6%), or registration systems (n=67, 75.3%) for herbal medicine. However, traditional healers claimed that they are licensed by either the Woreda Health Bureau (n=21, 95.5%) or the Regional Health Bureau (n=1, 4.5%) to legally practise traditional herbal medicine. Besides, no traditional healer is licensed by Ethiopian Food and Drug Administration (EFDA) or Ministry of Health.
Conclusion: Ethiopia has yet to adopt distinctive herbal medicine policies and laws to provide an independent herbal regulatory system. Despite the fact that the EFDA has a mandate for herbal medicine regulation, traditional healers are licensed by the woreda and regional health bureaus, thus more investigation is needed.
Keywords: herbal medicine, regulation, policy, legal framework, Ethiopia
Introduction
Herbal medicines have a long tradition of use outside of allopathic medicines around the globe.1 It is estimated that around 80% of the world’s population uses herbal medicines, either for maintaining general wellbeing or as part of their primary source of health care.2 As such, herbal medicines can save many lives, particularly in the developing countries.3 Despite herbal medicines with an extended history of popular use being normally safe when used appropriately at common therapeutic doses, the absence of evidence of toxicity or adverse drug events can not be taken as confirmation of the lack of toxicity or safety of herbal medicines.4
Scientifically, it has been proven that herbal medicines and their practices can cause harmful, adverse reactions if the product or therapy is of poor quality or it is taken inappropriately, even though there is a common belief that herbal medicine is safe since they are natural.5 For instance, data from 260 Asian patented herbal medicines show that 25% of products contain high levels of heavy metal, and 7% contain unspecified drugs which are added intentionally to bring a desired effect.6 As a result, national health authorities have enacted policies and laws to ensure that all herbal medicines are safe and of good quality, as herbal medicines have a high demand and market value for public health.7
In a global survey conducted by the World Health Organization (WHO), around 124 member states (64%) responded that they had laws or regulations on herbal medicines whereas around 125 member states or almost 65% of member states responded that they have a registration system for herbal medicines.6 For instance, regulatory harmonization of European Union member states established legislation (Directive 2001/83/European Commission & Directive 2004/24/European Commission) that has been approved to direct herbal medicine marketing in the European Union member states.8
In Africa, however, there are a large number of traditional herbal medicines, and a lot of public knowledge about them, but there is no legal basis for establishing these traditional herbal medicines as part of the drug legislation. In most parts of Africa, herbal remedies are sold in open markets, shops, and even at traditional healers without giving any scientific proof of their safety, efficacy, or quality.9
In sub-Saharan Africa, although most studies have come from a few countries (including Nigeria, South Africa, Ghana, and Uganda), many gaps have been identified in policy design and practice.10 In Kenya, there is no registration system for herbal medicines and they are sold without restriction.3,11 In Ethiopia, the majority of populations rely on traditional medicine for basic health services, most of which are derived from herbs.12 Herbal medicines were detailed in National Health Medicine policy, as well as Science and Technology policies in 1993, and have been translated into legislation and regulation (recently as Regulation no. 1112/2019).13 Nevertheless, herbal medicines with a long history of traditional use in the country are sold without any restrictions in the open market without proven safety, efficacy and quality.14,15 Thus, the aim of this study was to evaluate the policy governing herbal medicines regulation and its implementation in Ethiopia.
Methodology
Study Design and Location
The study was conducted to critically evaluate the policy governing herbal medicines regulation and its implementation in Ethiopia.
An archival review and in-depth key informant interviews were done to evaluate the policy governing herbal medicines regulation and to identify challenges to regulation of herbal medicines. Institution-based cross-sectional survey was performed to determine factors that affect regulation of herbal medicines and its implementation in Ethiopia.
In the case of institution-based cross-sectional surveys and in-depth key informant interviews, various institutions have been used encompassing: Ethiopian Food and Drug Authority [Medicine Registration & Licensing directorate, Product Safety directorate], Federal Ministry of Health [Medical Equipment & Supplies directorate], Armour Hanson Research Institute [clinical research and development division], Ethiopia Public Health Institute [Traditional & Modern Medicine Research directorate], Pharmaceutical industries [Research and Development Division], and Food, Beverage and Pharmaceutical Development Institute [Herbal and Traditional Medicine Development Directorate]. For the cross-sectional study involving only traditional healers, all traditional healers found in Addis Ababa were included to measure the legality of traditional herbal medicines and to identify associated factors that affect the legal practice of herbal medicines. This study was conducted in Addis Ababa from June 15, 2020 to December 25, 2020 where the majority of institutions are found. Addis Ababa is the capital city of Ethiopia with an area of 540 km2 and population of 3.43 million (1.81 million female and 1.62 million male) according to 2017 projections.16
Sample Population, Size, and Sampling Technique
In in-depth key informant interviews, 15 participants were chosen relying on purposive sampling technique. It was used to select participants who had direct or indirect involvement in the regulation and possessed profoundly discerning knowledge of herbal medicines. In institution-based cross-sectional survey, 89 study participants were selected from respective directorates/teams by using a convenience sampling technique. Any willing professional experts were included in this study design. In the cross-sectional study involving traditional healers, study participants were chosen by purposive and snowball sampling techniques. Twenty-two study participants were chosen from Addis Ababa (AA) City. Two traditional healers were selected from each of the following: Bole sub city, Nifas Silk sub city, Kolfe Keranio sub city, Kerkos sub city, Arada sub city, Akaki Kaliti sub city, Addis sub city, Yeka sub city, Lemi Kura sub city, Gulele sub city and Lideta sub city.
Data Collection Procedure
For archival review, a structured checklist was prepared depending on WHO guidelines for registration of TM in Africa region to show assessment on definition, policy and requirements for registrations of HMs in Ethiopia, Nigeria, EU and India. A point of checklist includes safety, efficacy, and quality, labeling and packing requirements in registration of HM among comparative countries. In in-depth interviews of key informants, a semi-structured interview was prepared depending on the research questions to generate qualitative data. Face-to-face semi-structured interviews with key informants (KIs) were conducted. The content of the interview tool was prepared depending on research questions of this study. In institution-based cross-sectional survey, structured questionnaires were prepared depending on WHO’s global report on traditional and complementary medicine.6 A questionnaire was pretested on eight non-healthcare workers to assess its clearness and simplicity, and validated by three experts in two rounds before the beginning of the study. Points of the questionnaire were organised in different sections: socio-demographic data of study participants, policy governing herbal medicines, law and regulation of herbal medicines in Ethiopia, and main difficulties in regulations of herbal medicines in Ethiopia. Similarly, for cross-sectional study involving traditional healers, a structured questionnaire was prepared mainly depending on WHO’s global report on traditional and complementary medicine. A questionnaire was pretested on three non-traditional healer individuals to assess its clarity and validated by two experts in two rounds in terms of face and content before commencement of the study. Points of the questionnaire were incorporated in different sections: demographic data of traditional healers, legality of herbal medicines and pattern of practice. In both cases, the questionnaires were prepared in English and translated into Amharic and reverse-translated back to English to check the reliability of the instrument. Written informed consent was obtained from each participant and the questionnaires were distributed to the participants in the respective institutions. All steps in data collection and recording were closely monitored by the principal investigator and data was collected daily, recorded, and compiled for the next day.
Statistical Analysis
In archival review, the selection of data was started by searching through each country’s DRA website to inform the definition, regulatory pathways and requirements for registration of herbal medicines. Data selected were extracted into Microsoft Word 10, analyzed for similarities and differences across the countries, and presented in a comparison table. For in-depth interview of key informants, the qualitative data was analysed using a content (thematic) analysis approach. All written notes were transcribed verbatim using Microsoft Word 2010. Then, all responses were subjected to thematic framework analysis, involving a five-step process: familiarization, coding, identifying a thematic framework, charting data into a matrix and interpreting the data. Two major themes related to policy of traditional medicines in Ethiopia were developed from the content analysis. One major theme and three sub-themes were generated related to challenges affecting HM registration in Ethiopia from the content analysis. All the filled questionnaires were checked to ensure their completeness before they were manually entered into Statistical Package for Social Sciences (SPSS) Version 20.0, based on appropriate coding and scoring formats for analysis. The results were summarized using descriptive statistics. In institution-based cross-sectional survey multiple logistic regression analysis was used to test for the level of significance. Odds ratios and p-values were used to check the significance factors. Variables with p<0.05 were considered potential factors for the presence of weak implementation and control mechanism for HM in Ethiopia. Binary logistic regression test was performed to identify eligible output variables for multiple logistic regressions.
Results
Archival Review
An overview of definition, regulatory pathways, regulatory bodies as well as minimum requirements for registration of herbal medicines in EU, India, Nigeria and Ethiopia are presented in Tables 1 and 2, respectively. Accordingly, from the archival review, it was revealed that despite the fact that proclamations no. 661/2009 and 1112/2018 were adopted in response to the 1993 health policy, TM is still not regulated as it should have been.
 |
Table 1 Summary of Definition, Classification of HMs and Responsible DRAs in Respective Countries |
 |
Table 2 Comparison of Requirements for Registration of Herbal Medicine Practices Ethiopia, India, EU, and Nigeria DRAs |
An in-Depth Key Informant Interview
According to all key informants, Ethiopia has not developed specific policies and laws on HM so far, which may convey a separate framework in its regulation. Some of the key informants indicated that TM was governed with series health policy of 1993. However, all participants indicated that new policy governing traditional medicine (TM) encompassing HM has been drafted in Health Sector Transformation Plan (HSTP) with powerful strategic plans, once it passes through the ministers’ council and is ratified by the House of Representatives. “Basically, HSTP has four core objectives and fourteen directives. TM is a component among those 14 directives which indicate the level of concern provided to indigenous medicinal knowledge in the country” (key informant 4).
Most of the key informants elaborated problems on regulation of HMs with its overall quality, safety, and efficacy from various points of view: knowledge-related, laws-related, and budget-related problems.
Most key informants believe that traditional Ethiopian herbal remedies (ETHMs) have not been adequately conducted in Ethiopia because they are tedious, often time-consuming (at least 10 to 15 years), and possibly fruitless. In addition, most participants felt that there was a huge gap in maintaining TM knowledge in Ethiopia.
Some of the key informants believed that Ethiopia has no specific legislation on protection of indigenous medicinal knowledge. As a result, intellectual property rights (IPR) have not been properly settled by laws, which creates mistrust among intellectual property owners and ultimately obscures secrets. They also say that the nature of TM is a shared heritage that can influence the core values of creativity. Almost all key informants thought that there is no sufficient budget for HMs from governmental and non-governmental bodies, which subsequently brought lack of expertise, lack of education, and lack of well-organized laboratories with modern instruments. “Even funders or donors do not provide any support for the pharmaceutical sectors unlike that of beverage and food industrial sector” (key informant 9).
Institution-Based Cross-Sectional Study
Demographic Data
Among 89 participants, 60 (67.4%) were males and the remaining 29 (32.6%) were females. The age of study participants ranged from 26 to 48, with mean age of 35.56 years (SD = ±6.30 years). Among all study participants, 64 (71.9%) of them hold Bachelor of Science degree and the remaining 23 (25.8%) hold Master of Science (Figure 1).
 |
Figure 1 Demographic characteristics of study participants for cross-sectional survey (N=89). |
Regulation of Herbal Medicines in Ethiopia
Among all study participants, 38 (42.7%) of them were affirmatives on availability of national policies while majority 51 (57.3%) of respondents were not positive toward its existence. Only 36 (40.4%) respondents had agreed on the presence of national laws related to HM whereas 53 (59.6%) of them is agreed. Among those participants who responded positively, 8 (9%), 15 (17%) and 13 (14%) of them considered national laws to be the same as the law for modern medicines, as separate law for HM, and as partly the same as for modern medicines, respectively (Figure 2). Multiple logistic regression analysis showed that the shortage of financial support for HM (p=0.014) and absence of mechanism to monitor HM safety (p=0.013) were contributing factors for inadequately implemented control mechanisms for HM in the market (Table 3).
 |
Table 3 Contributing Factors for Weak Implementation of TM Regulation (N=89) |
 |
Figure 2 Opinion of expert on regulation of TM in Ethiopia. |
Cross-Sectional Study Involving Only Traditional Healers
Characteristics of Study Participants
All of the study participants were male. All of the study participants also lived in the city of Addis Ababa. The age of respondents ranged from 31 to 74, with the mean age of 50.1 years (SD = ±11.5 years). The respondents have experience that ranged from 10 years to 55 years, with a mean of 24.4 years (SD = ±13.1 years) (Table 4).
 |
Table 4 Demographic Data for Cross-Sectional Study Comprising Healers |
Legality and Pattern of Practice
All of the study participants were licensed to legally practice TM. Out of 22 study participants, for the majority (17, 77.3%), it was a family influence which fascinated them to inaugurate TM business while 4 (18.2%) respondents joined TM business due to the impact of well-reputed traditional healers in their entire career. Only one respondent (4.5%) launched TM business through research over time due to the nature of his/her educational background. The majority of study participants (13, 59.1%) inferred that HM was not a profitable business in terms of money as sold at affordable price for end users whereas the remaining 6 (17.3%) and 3 (13.6%) labelled it as profitable or very profitable, respectively, relying on their profit margin. Meanwhile, 13 (59.1%) respondents believed that currently operating intellectual property policy regime (IPR) could be labelled as very low in terms of its potential to safeguard practitioners’ IPR in Ethiopia. Majority of respondents (14, 63.7%) chose patent certificates as the best IPR tool in terms of its capability in ensuring practitioners’ maximum reputability and profitability (Table 5).
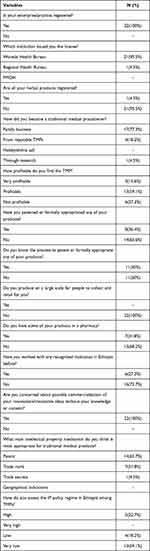 |
Table 5 Healers’ Responses on Legality and Patterns of Practice in HMs in AA (N=22) |
Discussion
The National Traditional Medicine Policy is a critical source of control over the quality, safety, and effectiveness of herbal medicines, and it was realized successfully through the implementation of an effective regulatory framework. According to our study, the traditional medicine regulatory system in Ethiopia is not legally sufficient in terms of scope or function; yet, as compared to orthodox medicines, herbal medicine regulation has received little attention from the Ethiopian government.17
The Ethiopian Food and Drug Authority prepare the regulatory standards and specifications for medicines and implement them upon its approval from appropriate organization organ. However, no official herbal remedy has yet been officially confirmed to ensure the overall quality of herbal medicines. Thus, the experience from the European Union countries could be used as a base ine in Ethiopia to establish a stringent regulatory platform in order to ensure the safety, efficacy and quality of traditional herbal medicines. In the European Union, European Medicine Agency has a well-organized legislative framework for registration of HM different pathways through directive 2004/24/EC and directive 2001/83/EC depending on traditional use of medicine and available scientific evidence.18
In an in-depth key informant interview, most participants described the major challenges facing effective herbal medicine control in Ethiopia. Currently, there is no adequately recognized scientific knowledge for traditional herbal medicine to safeguard the well-being of users. This drawback may exist as a result of poor documentation or lack of a database for traditional herbal medicines to generate flawless demarcation of well-researched herbal medicines from unknown herbal medicines. There are also no sufficient experts, budget, policies or strategies which are directly related to traditional herbal medicine development and regulation.19 Similarly, in institution-based cross-sectional survey study, an absence of mechanisms to monitor safety of HM and shortage of financial support for scientific researches were found to be strong contributing factors for the inadequately implemented control mechanism for HM in Ethiopia. But, all of these challenges fundamentally ascend from the government as it has poor concern for and commitment to traditional medicine knowledge. In Ethiopia, according to Proclamation No. 100/1948, it is mandatory for TMPs to hold a license to carry on the profession. The latest proclamation, No.218/2000, was ratified to deter the medical practitioners’ registration, proclamation No. 100/1948. Its introduction says that it is found indispensable to revoke the medical practitioners’ registration proclamation.20 According to all traditional healers, it is mandatory to receive license from woreda health bureaus of respective sub city after fulfilling required criterias to officially practice traditional medicine in Addis Ababa region. In Ethiopia, traditional medicine practice is very secretive. As a result, most of the time traditional medicine practice is passed from generation to generation along family lines that hold the knowledge. The majority of respondents were also dissatisfied with recently operating intellectual property policy regime from the perspective of its potential to safeguard practitioners’ intellectual property rights. It has mainly originated due to the lack of specific legislation to protect the intellectual property rights system. These critical drawbacks essentially emerged from the lack of a strong traditional medicine practitioners’ association (TMPs), and lack of motivation from the Ethiopian government for traditional medicine practitioners, and traditional medicine practices themself.
In Ethiopia, a utility model certificate is applied to certify HM innovators. Though it is simple, it cannot give the maximum profit and reputability for innovator (usually TMPs) as it stays for short period of time (maximum of ten years). The majority of study participants (TMPs) chose patent rights as the best tool to possess intellectual property rights (IPR), which would maximally protect the right of innovators to own newly innovated herbal medicines. Similarly, India has patented industrially applicable AYRUVEDA knowledge even with its complex interims of ownership as it is practiced through time in the public domain.18
Conclusion
Ethiopia has yet to adopt distinctive herbal medicine policies and laws to provide an independent herbal regulatory system. Despite the fact that the EFDA has a mandate for herbal medicine regulation, traditional healers are licensed by the woreda and regional health bureaus, thus more investigation is needed. In addition, one of the key challenges affecting the effective regulation of herbal products in Ethiopia is a lack of financial support for scientific research on herbal medicines, as well as a lack of methods to monitor the safety of herbal medicines.
Data Sharing Statement
The documents supporting this study will be available upon request from corresponding author.
Ethical Approval and Consent to Participate
The Helsinki Declarations was followed for undertaking this study. It was approved by institutional review board of Jimma University (Reference no. IRB 000245/2012). Study participants provided written informed consent prior to interviews for collection of data. The withdrawal right of study participants from involvement in the study at any time was assured.
Acknowledgment
The authors would like to express their sincere gratitude to all the respondents for accepting the invitation to participate in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sharad S, Manish P, Mayank B, Mitul C, Sanjay S. Regulatory status of traditional medicines in Africa Region. IJRAP. 2011;2(1):103–110.
2. Alostad Azhar H, Steinke douglas T, Schafheutle Ellen I. A qualitative exploration of Bahrain and Kuwait herbal medicine registration systems: policy implementation and readiness to change. J Pharm Policy Pract. 2019;12(1):1–20. doi:10.1186/s40545-018-0159-5
3. World Health Organization. National policy on traditional medicine and regulation of herbal medicines; Report of a global survey; 2005:1–168.
4. Alostad Azhar H, Steinke Douglas T, Schafheutle Ellen I. International comparison of five herbal medicine registration systems to inform regulation development: United Kingdom, Germany, United States of America, United Arab Emirates and Kingdom of Bahrain. Pharmaceut Med. 2018;32(1):39–49.
5. Verma N. Herbal medicines: regulation and practice in Europe, United States and India. Int J Herb Med. 2013;1(4):1–5.
6. World Health Organization(WHO). Global report on traditional and complementary medicine; 2019:1–225.
7. Martins E. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Neurol. 2014;4:1–10.
8. Salmon JW, Liu FX. Herbal medicine regulation in China, Germany and the United States. Res Gate. 2017;9(6):42–49.
9. Sharad S, Manish P, Mayank B, Mitul C, A Sanjay. Regulatory status of Traditional Medicines in Africa region. Phytomedicine. 2011;2(1):103–110.
10. James PB, Wardle J, Steel A, Adams J. Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. Br Med J Glob Heal. 2018;3:e000895.
11. Onyambu.Mo. A review of trends in herbal drugs standardization, regulation and integration to the national healthcare systems in Kenya and the Globe. Int J Pharmacogn Chin Med. 2019;3:3.
12. Debella A. Overview on the status of traditional medicine in Ethiopia and prospects for its development. Altern Integr Med. 2017;62(2):5162.
13. Ethiopian Food & Drug Authority(EFDA). Food and medicine administration proclamation; 2019:11099–11172.
14. Deribe KK, Alemayehu A, Binyam G, Yunis M. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Heal Dev. 2000;20(2):127–134.
15. Herbal Medicines: Challenges. Pharmacotherapy Group, University of Benin. Trop J Pharm Res. 2002;1:53–54.
16. Getnet S. Assessment of concomitant use of herbal and conventional medicines among patients with diabetes in public hospitals of Addis Ababa, Ethiopia. J ResGate. 2017;1:1–54.
17. Food, Medicine and HealthCareAdministration and Control Authority(FMHACA). Expediting Medicine Market Authorization Strategy. Addis Ababa, Ethiopia; 2017:1–39.
18. European Medicine Agency(EMA). Guideline on non-clinical documentation in applications for marketing authorisation/registration of well- established and traditional herbal medicinal products; 2019.
19. Fantaw D. Explore the challenge in medicines registration process in Ethiopia: qualitative phenomenological study. Acta Sci Pharm Sci. 2020;4(1):44–51.
20. G Mersa Y. The legal protection of Ethiopia traditional medicines and patent system. St Marry’s Univ Institutional Repos; 2005:1–12.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
