Back to Journals » Journal of Pain Research » Volume 12
Evaluation of patients’ needs to design and assess a patient education program in cancer pain
Authors Prevost V , Delorme C, Heutte N , Leconte A, Bechet C, Licaj I, Bignon R, Bisson C, Cauchin S, Gicquère M, Grach MC, Guillaumé C, Le Garrec J, Ropartz MC, Roux N, Sep Hieng V, Le Chevalier A, Clarisse B
Received 17 December 2018
Accepted for publication 10 April 2019
Published 6 June 2019 Volume 2019:12 Pages 1813—1823
DOI https://doi.org/10.2147/JPR.S197920
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
V Prevost,1 C Delorme,2,3 N Heutte,4 A Leconte,4 C Bechet,5 I Licaj,4 R Bignon,3,6 C Bisson,2,3 S Cauchin,3,7 M Gicquère,3,8 MC Grach,3,8 C Guillaumé,3,9 J Le Garrec,3,7 MC Ropartz,3,10 N Roux,3,9 V Sep Hieng,3,6 A Le Chevalier,3,10 B Clarisse4
1UMR 1086 Inserm ANTICIPE (Interdisciplinary Research Unit for Cancer Treatment and Prevention) and University of Normandy, Caen, France; 2Pain Assessment and Treatment Centre, Bayeux Hospital, Bayeux, France; 3Regional Pain Network for Lower Normandy, Bayeux, France; 4Clinical Research Unit, Centre François Baclesse, Caen, France; 5Pharmacie de la Croix d’Or, Paris, France; 6Pain and Palliative Care Unit, Lisieux Hospital, Lisieux, France; 7Pain Assessment and Treatment Consultation, Alençon-Mamers Intercommunal Hospital, Alençon, France; 8Pain and Palliative Care Unit, Centre François Baclesse, Caen, France; 9Pain and Palliative Care Unit, University Hospital, Caen, France; 10Pain Assessment and Treatment Centre, Avranches-Granville Hospital, Avranches, France
Purpose: Patient education constitutes a relevant strategy to improve pain management. In the field of therapeutic patient education (TPE), we aimed 1) to assess pain impact in cancer patients, 2) to identify patients’ educative needs in pain management, and 3) to refine research criteria for its future evaluation.
Patients and methods: Pain intensity, relief and interference were assessed in 75 cancer patients with unbalanced background pain. Self-assessment questionnaire evaluated i) patients’ pain management and ii) their knowledge and needs in TPE.
Results: Most patients experienced pain for more than 6 months and 41.6% reported adequate pain relief. Understanding pain and pain management were major patients’ preferences (>58%). Most patients declared they knew their pain treatments, but fewer than half of them were able to name them. However, education concerning pain treatment was considered as essential in <30% of patients. Almost all patients (97.1%) stated pain education as beneficial, with a preference for individualized sessions (41.2%). In addition, the assessment criteria for its future evaluation were refined.
Conclusion: Targeted population mainly concerned patients with persistent pain. Only half of patients reported pain relief despite antalgics. Patient education was declared as beneficial for almost all participants.
Practice implications: Tailoring a pain TPE on patients’ needs has the potential to help them to optimally manage their pain daily.
Keywords: cancer pain, pain management, pain assessment, patient education, educative needs, questionnaire
Plain language summary
- Almost one-third of cancer patients thought that suffering was normal
- Only half patients being treated with analgesics reported adequate pain relief
- Most patients stated they knew their pain treatments but fewer than half of them were able to name them
- For most patients, an education program would focus on managing pain in daily life
- Most patients preferred individual than collective sessions
Introduction
Pain remains one of the most feared symptoms in cancer patients and leads to impaired quality of life.1 Even if numerous guidelines and recommendations have improved the quality of cancer pain management, 55% of patients still experience pain during their treatment.2 Suboptimal management of pain is amply documented, and approximately one-third of patients do not receive pain medication proportional to their pain intensity.3 Undertreatment of cancer pain has been in particular associated to patient-related barriers.4,5 In response to this issue, therapeutic patient education (TPE), as defined by the World Health Organization,6 enables people with chronic disease to manage their illness and is considered of high importance in achieving optimal pain control.7
The number of published studies evaluating Pain Education Programs (PEP) for patients with cancer has increased in recent years.8 As highlighted by the analysis of eight systematic reviews in the field of cancer pain covering nearly 40 years,9 including three meta-analyses,10–12 PEP improve patients’ knowledge about cancer pain and achieve reductions in self-reported pain intensity measurements. However, heterogeneity of publications (in terms of study design, intervention content, and pain outcome assessments) complicates the comparison across studies and hinders the identification of a gold standard procedure.
In this context, our team has undertaken an extensive five-step research program (Figure 1): 1) training in TPE of 10 nurse–physician pairs (finalized); 2) identification of educative needs of patients and relatives in cancer pain; 3) development and optimization of a PEP for patients with cancer (which must be authorized by the French Regional Health Agency); 4) regional pilot study aiming to assess the quality and transferability of the program; 5) program evaluation using a comparative interventional randomized study.13 The originality and strengths of this 5-step research are that it provides access to the PEP to all individuals across the community and is based on close collaboration between health care professionals and researchers.
In order to improve PEP effectiveness, the administration of programs should be optimized. There is a critical need to specifically train health providers in TPE according to the WHO model.6 This training must be realized by dedicated authorized organisms and is a prerequisite to allow caregivers to be integrated in French TPE programs. In the first step of our research program, 10 nurse–physician pairs benefited from TPE training in order to facilitate harmonization and appropriation of the educational practice. The training involved the entire care staff in order to reach a consensus on modalities for the PEP construction and development as well as for the project implementation.
The present manuscript presents step 2 which aimed to identify the educative needs of patients in the setting of cancer pain so that they could be taken into account in the final PEP (step 3). Likewise, we aimed to assess pain and its impact on daily life in cancer patients. We further aimed to refine our research criteria to optimize research steps 4 and 5.
Patients and methods
Study design and ethics
We conducted a multicenter prospective noninterventional trial. The local ethics committee approved the study protocol. This study has received ethical approval from the Comité de Protection des Personnes de Nord-Ouest III (April 2014), from the Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé (July 2014) and from the Commission nationale de l’informatique et des libertés (February 2015). The trial was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent. The trial is registered as ID-RCB 2014-A00239-38, clinical trial NCT02391740.
Participants
Eligible patients with cancer met the pain criteria based on the definition of unbalanced background pain (meeting at least one of the 4 criteria described below), according to the Standards, Options and Recommendations.14 Inclusion criteria were, therefore, as follows: pain related to one’s disease or its treatments; meeting at least one of the following criteria: 1) average pain intensity amounting at least 4 on a scale of 10 or 2) pain preventing sleep in the previous 2 weeks, or 3) more than 4 daily episodes of breakthrough cancer pain, or 4) an impact on daily activities; pain treatment since at least 1 month; cancer diagnosis confirmed at least one month ago; life expectancy more than 6 months; health compatible with PEP requirements (WHO performance scale ≤2); 18 years or older, able to understand, speak and read French; without cognitive dysfunction.
Participants were recruited by 10 nurse–doctor pairs from the 10 centers involved in the Regional Pain Network (RRDBN) previously trained in TPE (step 1 of the project). Enrolment was performed in both university and local hospitals based on the representativeness of the file active of each center to best identify the educational characteristics of the various populations in the catchment area. In order to ensure this representativeness, we have imposed patient recruitment to be relatively balanced between the 2 kinds of reference structures either in the university town or in the 8 peripheral sites.
Instruments
Identification of patients’ educative needs regarding cancer pain
Educative needs were assessed using a 3-part form based on a questionnaire developed in patients with cancer from the Cancer Center Léon Bérard (Lyon, France) and adapted by our group to the field of pain. The original questionnaire was constructed on surveys conducted in 40 patients using a face-to-face structured interview and proofread by methodologists, health-professionals, patients, and social scientists. The 10-min questionnaire was pilot-tested with patients to ensure the clarity of the questions prior to the implementation of the trial.
The first section gathered general data on the patients, their lifestyle, disease, pain and its treatment, general and sociodemographic information, degree of autonomy, presence of caregivers, type of hospitalization, geographic accessibility, cancer type and stage, treatment and the intensity, and type and treatment of their pain.
The second part with 9 items addressed patient-reported pain management. It assessed how patients experienced their pain and its impact on daily life, their understanding of it, how they coped with it, and how they discussed it with medical staff and relatives. Each of these items was scored using a visual analogic scale (continuous scale comprised of a horizontal line of 10 cm in length, between two extremes which allows the health professional to score the intensity of the answer between 0 [not at all] and 10 [completely]).
The third part, given only to patients interested in the educative approach, assessed their knowledge about TPE and need of it. It focused on patients’ beliefs about TPE and their willingness to participate in the program. Patients were also asked to indicate and order their needs and expectations concerning the program and its modalities (individual, collective, or a mixture of individual and group sessions). Finally, they were asked whether they would have accepted to follow the program.
Overall, the questionnaire included 36 questions in total for the three parts, to be completed by the patient (Figure S1). Only patients who answered that they were interested in the educative approach on the last question of the second part completed the 9 items of the third part since our purpose was to build a PEP answering to the needs of this patient subset.
 | Figure S1 The evaluation regarding cancer pain and patients’ educative needs (3 parts, 36 questions in total of the self-reported questionnaire). |
Brief Pain Inventory (BPI)
Pain was assessed using the “Questionnaire Concis sur les Douleurs”, a validated French version of the BPI,15 commonly used in research protocols.8 The short version has been validated in French,16 and the French Authority for Health recommends the use of subscale 9 to assess quality of life in patients suffering from pain.17 Pain intensity scores were rated using a 0 (no pain) to 10 (worst imaginable pain) numeric rating scale. Categories of pain severity18 were determined from the worst pain intensity scores (ie, 1–4= mild pain, 5–6= moderate pain, and 7–10= severe pain). In addition to assessing pain intensity, location, and relief, the BPI allows a rapid self-assessment of the impact of pain on daily activities, considering two subdimensions (affect and activity) using 7 items (general activity, mood, walking ability, normal work, relations with other people, sleep, and enjoyment of life). Response choices were rated on a 11-point numeric summated rating scale (0–10), with higher scores indicating greater pain intensity or impact on daily life.
The BPI also allows calculating the pain management index (PMI), which, by combining pain intensity and analgesic treatment, assesses the proper use of analgesics.19 The PMI is explained to patients as being a way to quantify how well their pain is managed pharmacologically (0= no analgesia, 1= nonopioid analgesia, 2= a mild opioid, 3= a strong opioid). It is calculated by subtracting the maximum pain level reported by the patient from the type of analgesic treatment,20 the score ranging from −3 (nonanalgesia therapy patient with severe pain) to +3 (opioid therapy patients without pain).
Statistical analyses
The main judgment criterion was the mean of the 10-point scores of the 9 items from the second part of the questionnaire developed to identify patients’ educative needs dealing with “How the patient feels his/her pain and pain impact on daily life”. For each of these 9 items, 0 represents “not at all” and 10 represents “completely”. For the statistical power computation, assuming a standard deviation (sd) of 2, we found that 62 assessable patients were required to estimate the 95% CI with a precision of 0.5 points. We planned to enroll 75 consecutive patients to anticipate potential nonassessable patients.
Statistical analyses were performed with a bilateral α risk of 5%. Exploratory data analysis provided frequencies and their 95% CI for qualitative variables and mean and SD for quantitative variables. Proportions were compared using the Chi-square test if applicable, otherwise using the Fisher’s exact test. Means were compared using the Student’s test if applicable; otherwise, the Mann–Whitney test was used.
Results
Patient characteristics
Study population
From March 2015 to February 2016, 75 patients were enrolled, of whom 72 were assessable. Inclusions were conducted in a way that participating patients were representative of the regional oncological activity. 44.5% were recruited equitably from the 2 major centers of the university town and 55.5% came from the 8 smaller centers in satellite cities.
Demographics
The population was almost gender balanced (female 57.0%). Mean age was 59.9 (SD, 12.7), ranging from 25 to 85 years. Around half of the patients were retired (54.2%), while a minority (5.6%) were jobseekers. 72% of the participants lived with a spouse and mainly benefited from the assistance of relatives (88.9%).
Cancer type and WHO performance status
Patients had been diagnosed with cancer in the past 2.3 years on average. Lung (29.2%) and breast (20.8%) cancers were the most frequent cancers. Most participants (61.1%) had locally advanced cancer and almost half suffered from metastases (48.6%). 20.8% were fully active and able to carry on with all pre-disease activities unrestrictedly (performance status, PS 0), 41.7% were restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature (PS 1), and 36.1% were ambulatory and capable of all self-care but unable to carry out any work activities (<50% in bed during the day, PS 2).
General medical data on pain and its treatment
Patients were asked about their pain in general (Table 1). Most patients had experienced pain for more than 6 months (74.3%) and reported to know the cause(s) of their pain (73.2%). The main cause identified was cancer (75.0%), followed by treatment (25.0%) and mood (8.3%). About 30% of patients thought that experiencing pain was “normal” in their setting and 79.1% stated that there were solutions to relieve pain.
 | Table 1 Patients’ pain and treatment (n=72)a |
Concerning pain treatment, 91.6% declared knowing which pain treatment they were taking and 84.7% declared taking it in full. Yet, when patients were asked to list their pain treatment, only 30.6% responded as prescribed by the doctor. To avoid any ambiguity due to the prescription of paracetamol “as needed”, we further compared listed and prescribed pain treatment. Here again, more than half of the patients (51.4%) did not know exactly what their pain treatment was, ie, 48.6% were able to name correctly the drugs they were receiving. Strong opioids were received by 62.5% of patients.
Pain characteristics obtained with the BPI
Back pain was the most common pain experienced by 52.8% of the patients. Participants’ pain intensity, interference, and relief are summarized in Table 2. Moderate-to-severe pain was noted for 83.3% of the patients. On a scale of 0–10, patients rated their worst pain at 6.5 (SD, 1.9), with the average pain rated at 4.9 (SD, 1.9). Pain was relieved for 51.9% of patients. The mean pain interference score was 4.6 (SD, 1.1). Daily life and normal work, mean scores 6.0 (SD, 2.2 and 2.8, respectively) were strongly impacted by pain. In contrast, pain was less likely to impact relations with other people, mean score 3.4 (SD, 2.8). 23.6% of the patients had a negative PMI score, indicating inadequate pain management.
 | Table 2 Pain characteristics of patients according to Brief Pain Inventory (n=72)a |
Patient-reported pain management
Table 3 presents patients’ feelings concerning the management of their pain. As the main objective, the mean score for the 9 assessed items on this feeling on pain was 6.9 (SD, 1.3) of 10. More precisely, a good understanding and management of pain treatment were reported with a mean score of 7.8. The exploration of potential associations between patients’ feeling about pain management and their feeling about pain highlighted that better understanding of treatment was positively statistically significantly related to 1) the feeling that there are solutions to relieve pain (p=0.005), 2) less sleep discomfort (p=0.03), and 3) better relief obtained with pain treatment (p=0.02). The mean score concerning pain management was 6.6 (SD 2.7). Patients sought aid very moderately from their relatives (4.6, SD 3.6) and no relationship was noted between support from patients’ relatives and ability to manage their pain. In addition, participants declared speaking about their pain, thinking that their relatives understood their pain and believed that their pain was at a level around 6 out of 10. Concerning their relations with health care professionals, patients felt quite able to speak about their pain (8.4, sd 1.6) and to tell them if they recognized worsening signs of pain (8.7, SD 1.5).
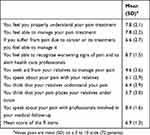 | Table 3 Patient-reported pain management (n=72) |
Patients’ knowledge and need of TPE
Most patients (83.3%) and especially males had never heard about TPE. After a brief explanation of TPE as defined by the WHO (1998), about half of the patients believed that such an approach could help them (54.4%) and declared that they would be willing to participate (47.2%) in a TPE program. Those who thought that it could be helpful were mostly women (70.3%, p=0.02), those who experienced pain for more than 6 months (86.5%, p=0.05), and those who felt less able to manage their pain (respective score of 5.9, SD 3.0 vs 7.3, SD 2.3, for patients who thought TPE could be helpful versus others, p=0.05).
Patients interested in TPE were then asked about their needs regarding their pain. A section of the educative questionnaire dealt with 12 issues among which patient had to select 4 to be addressed in a PEP (Figure 2). Priority was given to subjects concerning pain understanding (67.6%), pain management alone (67.6%), and coping with pain in daily life (58.9%). Topics involving relatives were less retained (communication about pain with their environment: 17.6% and participation in pain management: 5.9%). No issues other than those proposed were suggested by the patients. They were also asked about their preference concerning the format of the training. The preferred choice was individual workshop (41.2%). 11.8% preferred collective sessions, 29.4% preferred alternating individual and collective sessions, and 17.7% had no specific preference. Regarding their willingness to join a PEP, most patients were ready to participate in a PEP close to home (97.1%) and ready to return to hospital for a PEP outside scheduled visiting hours (97.1%).
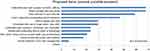 | Figure 2 Identification of patients’ educative needs, ranked in decreasing order (n=34). |
Patients’ characteristics among participating hospitals
When comparing patients’ data obtained from the 2 major hospitals with those from peripheral centers, no significant differences were found in patient profile (sociodemographics, disease characteristics, pain interference with daily life, pain treatments, and educative knowledge).
Discussion
Most patients experienced pain for more than 6 months, suffered from locally advanced cancer, and had metastases. These three aspects of the disease frequently lead to severe pain and complicate cancer management.21 Furthermore, only 1 in 2 patients treated with analgesics reported adequate pain relief, which is consistent with the literature.1,22 Undertreatment often results from a lack of knowledge about cancer pain and is largely linked to patient barriers and representations.7 Thus, one-third of our patients still believed that suffering from pain was normal, even though pain is considered unacceptable and can now be relieved in 70–90% of cases.21
To overcome these hurdles, active patient involvement is necessary and self-management education appears to be a relevant approach.23,24 Over 80% of our patients had never heard about TPE and only about 50% were interested in receiving it after hearing the definition. This poor rate endorses the need for further study to explore how their needs might be met if TPE does not suit them or how perhaps their lack of interest could be changed. Another explanation could be that some patients do not accept the new patient role of active partners in their disease management and can refuse to take part actively in management of their pain, as already documented in the literature.25 This testifies to the importance of creating clear communication between health care providers and patients, a distinctive feature of the TPE approach that has become commonplace in the field of diabetes, for example.
Nevertheless, among patients interested in TPE, almost all were clearly in favor of joining a PEP close to home, thanks to pain regional network, even outside scheduled hospital visiting hours.
With regard to patients’ preferences, understanding and managing pain and coping in daily life are of prime importance in a PEP, as reported by more than 55% of our patients. By contrast, fewer than 30% attached value to the use and understanding of pain treatment. Nevertheless, most of them declared to understand their pain and to know how it was treated (7.8 on a 0–10 scale for both items). Even so, fewer than half of them were able to name their prescribed drugs correctly, which indicates that they need to develop knowledge and skills in this field. This highlights the discrepancy between patients’ expectations and needs. From an ethical point of view, the aim of the first step of a PEP, which is called the educational diagnosis or, more relevantly, the “shared educational assessment”,26 is precisely to bring the patient’s needs to light. The same applied to the role of relatives in the management of their pain. Issues involving relatives were less retained (ie, participation in pain management for 5.9%) and few patients sought aid from relatives for pain management (4.6/10). However, involvement in the patient’s environment has been demonstrated to be very important for pain management.27 In this context, we plan to propose to patients to ask their relatives to participate in the further steps of our program, if they wish. Concerning the format of the educational sessions, 41.2% of the patients preferred the individual workshops, even though collective sessions (chosen by 11.8%), are known to be successful. Peer learning is indeed more productive in terms of sharing experiences, giving “tips and tricks”, and promoting dialogue.28 The patients’ reluctance could be attributable to the taboo still associated with cancer and pain. Our program will, therefore, be offered in a flexible format allowing collective and/or individual sessions, if needed. Small homogeneous patient groups could also be organized.
These preliminary findings and the limitations observed will, in turn, benefit the two evaluation steps and allow the program to be improved. The inclusion and recruitment criteria will be refined. The inclusion criteria require clarification because the version used in the present study, which is based on the notion of unbalanced pain, could lead to confusion among nurses with little experience in clinical research. Patients were sometimes considered as noneligible because the criteria focused on a pain intensity rating of 4 of 10, whereas patients with less pain but with insomnia-related pain were in fact eligible. Moreover, eligibility criteria did not mention the possibility to enroll patients experiencing pain after anticancer treatment. This will be made clearer in the following steps. Inclusion criteria concerning cancer pain will be clarified as follows: pain related to one’s disease or its treatments and/or sequelae of the disease and its treatment (current or not); meeting at least one of the following criteria: 1) average pain intensity amounting at least 4 on a scale of 10, OR 2) pain preventing sleep in the previous 2 weeks, OR 3) more than 4 daily episodes of breakthrough cancer pain, OR 4) an impact on daily activities; pain treatment since at least 1 month. These insufficiently defined eligibility criteria were time-consuming, slowed down recruitment and led to selecting a population with rather intensive pain and a quite severe stage of disease. However, this category of patients might not be the most inclined to join a PEP as they are already preoccupied with health care and are perhaps less receptive to participating in collective sessions, because they are likely to be in greater pain. Conversely, patients with pain after anticancer treatment would certainly be more willing to participate.
The geographical recruitment of our patients was representative of the file active of the participating hospitals since there were more inclusions in the major teaching hospitals, yet all the outlying centers participated. As patients’ features were similar whatever the site where they were managed for cancer pain, we plan to include patients in steps 4 and 5 without imposing any proportional representativeness.
For this preliminary study, we make the decision to use the validated BPI, frequently used in trials.15 This choice reinforces the interest of our approach. Assessing the impact of pain on daily activities would indeed seem to be more appropriate, as it is less fluctuant, more realistic and more relevant than evaluating pain intensity in the context of TPE, which mainly aims to improve quality of life.6 In our patients, pain was reported to mainly impact daily life and normal work, areas on which educative programs are focused. Appropriate management of pain should ensure that it has a limited impact on daily life, thereby underlining the value of the educative approach. In the next stages of our research, the questionnaire will be used as the main assessment criterion. The benefit of TPE on the impact of pain will be defined as a 2-point decrease on a scale of 10 between the mean values of the seven items measured before and at the end of the program, which is considered to correspond to a clinically significant improvement.29 The BPI was also used to calculate the PMI, which allows the proper use of analgesics to be assessed.19 As almost one-quarter of our patients had a negative PMI score, inadequate pain management may be suspected. Unrelieved pain may also be related to patients not taking their medications as prescribed, for reasons highlighted in our study. Even though misconceptions about opioids remain common,30 TPE could allow them to better understand and manage pain treatment and to communicate appropriately with health care providers, despite the fact that this item was not identified as a priority by our patients. Medicine-taking is a complex human behavior and non-adherence is common,31 including in the field of pain.32 TPE aims at improving the understanding of pain, its treatment, and side effects. Above all, its objective is to allow patients to acquire the skills needed to make them active agents in their pain management and in their coping with cancer pain.
Conclusion
This study demonstrates the current situation concerning cancer-related pain and its perception at a French regional level. Targeted population concerned a majority (around three-quarters) of patients who experienced persistent pain since more than 6 months. Despite all patients being under analgesic treatments, only half of them reported adequate pain relief. We further observed that almost all patients declared pain education as beneficial, with a preference for individualized sessions. These findings reinforce the need to pursue this extensive joint project involving clinical staff and researchers through the evaluation of the benefits of a PEP using a robust method.
In a context of access to care for all enhanced by health network and not solely limited to large hospitals, implementation of a PEP tailored to the patients’ needs has the potential to give them skills and confidence to optimally manage their pain daily and ultimately improve their quality of life.
Data sharing statement
Data from this study are not publicly available. The authors will allow sharing of participant data, such as pain characteristics, patients’ feelings about pain and its management, and patients’ educative needs. If you have any questions or would like to request data please get in touch via the following e-mail address: [email protected].
Acknowledgments
The authors would like to thank the teams of Argentan (C. Le Gal, C. Van Delook), Cherbourg (I. Lepleux), Flers (F. Lecaer, A.L. Millet), and Saint -Lô (M. Feuillet, S. Gehanne) for their participation in the study. They also thank the TAKEDA Company for its Grant that allowed the implementation of this study (Step 2). They are also grateful for the financial support of the Apicil Foundation and the ARDCOM (Step 1), the “Ligue contre le Cancer” (Step 4) and the French National Cancer Institute INCa (Invitation to tender RISP15-007_FP, Step 5). We wish to thank the patients and their relatives who participated in this study and the teams in the participating centers. We acknowledge the ARS (French Regional Health Agency) and ERET (Regional Area for Therapeutic Education) for their support during the development of the PEP and its validation. We also thank Magalie Hureau at the Cancer Center Léon Bérard for providing the original questionnaire on cancer patients’ needs. Finally, we acknowledge Ray Cooke for language review and copyediting the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kroenke K, Theobald D, Wu J, Loza JK, Carpenter JS, Tu W. The association of depression and pain with health-related quality of life, disability, and health care use in cancer patients. J Pain Symptom Manage. 2010;40:327–341. doi:10.1016/j.jpainsymman.2009.12.023
2. Van den Beuken-van Everdingen MHJ, Hochstenbach LMJ, Joosten EAJ, Tjan-Heijnen VCG, Janssen DJA. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51:1070–1090.
3. Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32:4149–4154. doi:10.1200/JCO.2014.56.0383
4. Ward SE, Goldberg N, Miller-McCauley V, et al. Patient-related barriers to management of cancer pain. Pain. 1993;52:319–324.
5. Brant JM. The global experience of cancer pain. Asian Pac J Cancer Prev. 2010;11(Suppl 1):7–12.
6.
7. Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol. 2014;32:1727–1733. Erratum in: J Clin Oncol. 2014;322:117. doi:10.1200/JCO.2013.52.4827
8. Prevost V, Delorme C, Grach MC, Chvetzoff G, Hureau M. Therapeutic education in improving cancer pain management: a synthesis of available studies. Am J Hosp Palliat Care. 2016;33:599–612. doi:10.1177/1049909115586394
9. Adam R, Bond C, Murchie P. Educational interventions for cancer pain. A systematic review of systematic reviews with nested narrative review of randomized controlled trials. Patient Educ Couns. 2015;98:269–282. doi:10.1016/j.pec.2014.11.003
10. Bennett MI, Bagnall AM, José Closs S. How effective are patient-based educational interventions in the management of cancer pain? Pain. 2009;143:192–199. doi:10.1016/j.pain.2009.01.016
11. Cummings GG, Olivo SA, Biondo PD, et al. Effectiveness of knowledge translation interventions to improve cancer pain management. J Pain Symptom Manage. 2011;41:915–939. doi:10.1016/j.jpainsymman.2010.07.017
12. Jho HJ, Myung SK, Chang YJ, Kim DH, Ko DH. Efficacy of pain education in cancer patients: a meta-analysis of randomized controlled trials. Support Care Cancer. 2013;21:1963–1971. doi:10.1007/s00520-013-1756-0
13. Prevost V, Clarisse B, Heutte N, et al. Therapeutic patient education in cancer pain management: from practice to research: proposals and strategy of the French EFFADOL Program. J Cancer Educ. 2018;33:1355–1361. doi:10.1007/s13187-017-1258-8
14. Poulain P, Michenot N, Ammar D, et al. Mise au point sur l’utilisation du fentanyl transmuqueux chez le patient présentant des douleurs d’origine cancéreuse (version longue) [Update knowledge on the use of transmucosal Fentanyl in patients suffering from cancer pain]. Doul Et Analg. 2012;25:102–117. doi:10.1007/s11724-012-0287-7
15. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;13:129–138.
16. Larue F, Colleau SM, Brasseur L, Cleeland CS. Multicentre study of cancer pain and its treatment in France. BMJ. 1995;310:1034–1037.
17.
18.
19. Zelman DC, Cleeland CS, Howland EW. Factors in appropriate pharmacological management of cancer pain: a cross-institutional investigation. Pain (Suppl). 1987;30:S136. doi:10.1016/0304-3959(87)91344-3
20. Deandrea S, Montanari M, Moja L, Apolone G Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19:1985–1991. doi:10.1093/annonc/mdn419
21. Van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18:1437–1449. doi:10.1093/annonc/mdm056
22.
23. Howell D, Harth T, Brown J, Bennett C, Boyko S. Self-management education interventions for patients with cancer: a systematic review. Support Care Cancer. 2017;25:1323–1355. doi:10.1007/s00520-016-3500-z
24. Oldenmenger WH, Gearing JI, Mostovaya I, et al. A systematic review of the effectiveness of patient-based educational interventions to improve cancer-related pain. Cancer Treat Rev. 2018;63:96–103. doi:10.1016/j.ctrv.2017.12.005
25. Longtin Y, Sax H, Leape LL, Sheridan SE, Donaldson L, Pittet D. Patient participation: current knowledge and applicability to patient safety. Mayo Clin Proc. 2010;85:53–62. doi:10.4065/mcp.2009.0248
26. Sandrin-Berthon B. Diagnostic éducatif ou bilan éducatif partagé? [Educational diagnosis or shared educational assessment?]. Med Mal Metab. 2010;4:38–43.
27. Valeberg BT, Miaskowski C, Paul SM, Rustøen T. Comparison of oncology patients’ and their family caregivers’ attitudes and concerns toward pain and pain management. Cancer Nurs. 2016;39:328–334. doi:10.1097/NCC.0000000000000319
28. Mosnier-Pudar H, Hochberg-Parer G. Éducation thérapeutique, de groupe ou en individuel: que choisir? [Therapeutic education, within groups or individually, what to choose?]. Med Mal Metab. 2008;2:425–431.
29. Cleeland CS, Body JJ, Stopeck A, et al. Pain outcomes in patients with advanced breast cancer and bone metastases: results from a randomized, double-blind study of denosumab and zoledronic acid. Cancer. 2013;119:832–838. doi:10.1002/cncr.27789
30. Gunnarsdottir S, Sigurdardottir V, Kloke M, et al. A multicenter study of attitudinal barriers to cancer pain management. Support Care Cancer. 2017;25:3595–3602. doi:10.1007/s00520-017-3791-8
31. Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization; 2003. Available from:
32. Timmerman L, Stronks DL, Groeneweg JG, Huygen FJ. Prevalence and determinants of medication non-adherence in chronic pain patients: a systematic review. Acta Anaesthesiol Scand. 2016;60:416–431. doi:10.1111/aas.12697
Supplementary material
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

