Back to Journals » Infection and Drug Resistance » Volume 13
Evaluation of Modified Rapid Carbapenem Inactivation Method (mrCIM) Combined with Rapid EDTA-Modified Carbapenem Inactivation Method (reCIM) to Detect Carbapenemase and Distinguish Metallo-Carbapenemase in Enterobacteriaceae Within Four Hours
Authors Wei Q, Sun J, Wang Z, Yan L, Zhang C, Xu X
Received 13 February 2020
Accepted for publication 1 June 2020
Published 23 June 2020 Volume 2020:13 Pages 1919—1927
DOI https://doi.org/10.2147/IDR.S249570
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Qiang Wei, Jide Sun, Zhu Wang, Li Yan, Chuanming Zhang, Xiuyu Xu
Department of Laboratory Medicine, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China
Correspondence: Xiuyu Xu
Department of Laboratory Medicine, The First Affiliated Hospital of Chongqing Medical University, No. 1 Youyi Road, Yuzhong District, Chongqing 400016, People’s Republic of China
Tel/ Fax +86-23-89012513
Email [email protected]
Purpose: To develop a rapid EDTA-modified carbapenem inactivation method (reCIM) combined with modified rapid carbapenem inactivation method (mrCIM) to detect carbapenemase and distinguish metallo-β-lactamases from carbapenemases in Enterobacteriaceae in 4 hrs.
Materials and Methods: The sensitivities and specificities of mrCIM and reCIM were retrospectively evaluated in 247 carbapenem-resistant Enterobacteriaceae of which 107 were carbapenemase producers confirmed by PCR and sequencing. In addition, mrCIM and reCIM were prospectively evaluated with 47 carbapenem-resistant enterobacterial isolates.
Results: The sensitivity and specificity of mrCIM were 96.3% and 97.1% at 2.5 hrs post incubation, and the specificity increased to 98.6% at 3 hrs. The combined mrCIM and reCIM showed a sensitivity of 95.4% and a specificity of 100% at 2.5 hrs post incubation in identifying metallo-β-lactamases, and the sensitivity increased to 97.0% at 3 hrs. These performance characteristics are comparable to mCIM and eCIM; however, compared with mCIM and reCIM tests which need at least 24 hrs to detect results, the mrCIM and reCIM required less than 4 hrs of total work time.
Conclusion: The combined mrCIM and reCIM can be used to accurately and quickly detect carbapenemase and metallo-β-lactamases in Enterobacteriaceae in 4 hrs and are suitable for routine use in most clinical microbiology laboratories.
Keywords: modified rapid carbapenem inactivation method, rapid EDTA-modified carbapenem inactivation method, metallo-carbapenemase, Enterobacteriaceae, detection
Introduction
Infections due to carbapenem-resistant Enterobacteriaceae (CRE) are increasingly reported worldwide, associating with alarming mortality rates and increased health-care costs.1,2 Resistance to carbapenems can be attributed to the production of carbapenemases or other mechanisms including decreased permeability, overproduction of ESBLs or cephalosporinases, efflux pumps or combinations of these mechanisms.3 Distinguishing carbapenem-producing Enterobacteriaceae (CPE) from CRE due to non-carbapenemase-mediated mechanisms is important, as CPE strains disseminate between patients more readily than non-CPE isolates caused by the quick and easy horizontal transmission of carbapenemase genes such as blaKPC and warrant implementation of more intensive infection control measures than would be employed in the absence of carbapenemase production, making the importance of rapid diagnosis of carbapenemase-producing microorganism and the importance of utilization of the next-generation sequencing to evaluate the circulating strains.4,5 Carbapenemases are categorized in different classes that define their hydrolytic profile: Ambler class A serine β-lactamases including KPC and GES, VIM, NDM and IMP belonging to the Ambler class B metallo-β-lactamases (MBLs), and OXA-48 or OXA-48-like belonging to the class D.6,7
Currently, characterization of the underlying mechanism of carbapenem resistance is not undertaken by most clinical microbiology laboratories for therapeutic purpose. However, understanding if an organism is carbapenemase carrier and, if so, the class of carbapenemase produced has treatment implications, especially for the novel β-lactam and β-lactamase inhibitor compounds such as ceftazidime-avibactam or meropenem-vaborbactam which have activity against some carbapenemases including Ambler class A carbapenemases as well as some Ambler class C enzymes but not Amber class B enzymes,8,9 making rapid and accurate detection to identify MBLs from carbapenemases is essential.
Molecular assays are regarded as gold standard methods for detecting antibiotic-resistant genes, however phenotypic detection is convenient, manageable and a cost-effective method and plays a vital role in screening carbapenemases in clinical microbiology laboratories. Over the last decade, various phenotypic carbapenemase detection tests have been developed, including growth-based assays which measure resistance based on growth in the presence of an antibiotic such as modified carbapenem inactivation method (mCIM), hydrolysis methods which detect the product of hydrolysis that is catalyzed by carbapenemase enzymes (eg, Carba NP and derivatives and MALDI-TOF MS methods).10–12 These tests can detect the presence of carbapenemase and some modifications to these assays can provide more information on the specific carbapenemase groups being produced such as EDTA-mCIM (eCIM) and multiplex lateral flow immunoassays.10,13-15 In 2017 Muntean et al reported a rapid carbapenem inactivation method (rCIM) which was a rapid (less than 3 hrs), cheap and accurate screen test for carbapenemase-producing Enterobacteriaceae.16 However, this assay cannot discriminate between Ambler class A and Ambler class B carbapenemase. In the present study, we modify the rCIM (mrCIM) and develop a rapid EDTA-modified carbapenem inactivation method (reCIM) which could detect carbapenemase and distinguish MBLs from carbapenemases in Enterobacteriaceae in 4 hrs. The performance of mrCIM and reCIM were compared with mCIM, eCIM and molecular assay.
Materials and Methods
Bacterial Isolates
A total of 247 non-repetitive CRE isolates recovered from clinical specimens between 2015 and 2018 in the first affiliated hospital of Chongqing medical university were used to retrospectively evaluate mrCIM and reCIM. These isolates include Klebsiella spp. (94), Escherichia coli (43), Enterobacter cloacae complex (82), Enterobacter spp. (13) and Citrobacter spp. (15). For the prospective study, the 47 non-repetitive CRE isolates (32 K. pneumoniae, 9 E. coli, 4 E. cloacae complex and 2 Citrobacter freundii) recovered from clinical specimens over a period of 3 months were included. These strains were identified as CRE in routine antimicrobial susceptibility tests. All the clinical samples involved in this research were part of the routine hospital laboratory procedure.
All the isolates were identified by VITEK MS (bioMerieux, Hazelwood, MO, USA). The MIC values of ertapenem, imipenem and meropenem were determined by the VITEK2 compact (bioMerieux). Antimicrobial susceptibilities were interpreted by the recommendation of CLSI-M100 S29.17 For phenotypic tests described below, K. pneumoniae strain ATCC BAA-1705 was used as positive control for mCIM and mrCIM, and K. pneumoniae ATCC BAA-2146 was used as positive control for eCIM and reCIM, whereas K. pneumoniae ATCC BAA-1706 as the negative control.
mCIM and eCIM
The mCIM and eCIM were performed following the protocol recommended by CLSI-M100 S29. And the results of mCIM and eCIM were interpreted with CLSI-M100 S29 guideline.17
mrCIM and reCIM
The mrCIM was developed based on rCIM previously described by Muntean et al16 with some modifications. Firstly, isolates were incubated with meropenem for 45 min. Secondly, the indicator E. coli ATCC 25922 was incubated for 2.5 h in the next incubation step. Thirdly, growth of indicator E. coli with OD > 2.0 is highly indicative of carbapenemase production, and OD < 1.0 can be considered as carbapenemase negative. For indicator E. coli growth between 1.0 and 2.0, 30 min of additional incubation was beneficial (Figure 1). In the reCIM, a second 1-mL sterile water tube with final concentration of 5 mM EDTA was needed, and the following procedures were the same as those in mCIM (Figure 1). When the turbidity of indicator E. coli with and without EDTA both reach more than 2.0, it can be considered as reCIM-negative, indicating that the test strains producing a serine carbapenemase. On the contrary, if the test strain is mrCIM positive and the turbidity of indicator E. coli is less than 1.0 in the presence of EDTA, then the reCIM is positive (Figure 1). The cut-offs in mrCIM and reCIM were defined using control strains ATCC BAA-1705 (KPC positive), ATCC BAA-1706 (carbapenemase negative) and ATCC BAA-2146 (NDM positive) in 10 times repetition of mrCIM and reCIM tests.
Molecular Detection of the β-Lactamase Genes
An in-house PCR was performed as previously described and primers targeting carbapenemase genes including blaKPC, blaNDM, blaOXA-48-like, blaVIM, and blaIMP, other β-lactamase genes encoding ESBLs and AmpC, and genes encoding porins such as OmpK, OmpF were used.18,19 DNA template for the isolates was prepared as follows. Five colonies were inoculated in 100 μL of distilled water, followed by heating at 95°C for 10 min. Subsequently, the suspensions were centrifuged at 15,000 rpm for 2 min and the supernatant was used as PCR template. PCR was performed as: a volume of 14.5 μL of PCR Master Mix was mixed with 2 μL of forward and reverse primers in a 25-μL reaction. Then, 1 μL of sample from each test isolate was added to the mixture. The PCR program consisted of an initial denaturation step at 95°C for 5 mins, followed by 35 cycles of denaturation at 95°C for 30 s, annealing at 60°C for 30 s, elongation at 72°C for 30 s, and a final extension at 72°C for 10 mins. Molecular detection by PCR and sequencing was considered as the gold standard for β-lactamase characterization.
Statistical Analysis
All statistical analyses were performed with the SPSS software version 24.0 (Chicago, IL, USA). The sensitivity and specificity were calculated, with their respective 95% CI. Test sensitivities and specificities were compared using the McNemar’s v2 test from the base R package.
Results
Carbapenemase Genes Expressed by Tested Strains
Of the 247 CRE isolates used in the retrospective study, 107 isolates were carbapenemase gene carriers. As shown in Table 1, the carbapenemase genes identified were blaKPC-2 (31/107, 29.0%), blaNDM-1 (44/107, 41.1%), blaNDM-5 (13/107, 12.1%), blaIMP-4 (5/107, 4.7%), blaIMP-8 (1/107, 0.9%). Two strains (2.0%) were found to carry blaNDM-1 and blaIMP-8, and one strain carrying blaNDM-1 and blaIMP-4. In addition, blaKPC-2 and blaNDM-1 were simultaneously detected in 8 isolates (7.5%), blaKPC-2 and blaIMP-4 in one isolate (0.9%). There was also one isolate (0.9%) harboring blaKPC-2, blaNDM-1 and blaIMP-4 at the same time. In a prospective study, the 47 CRE strains were identified to be blaKPC-like carriers (33/47, 70.2%), blaNDM-like carriers (8/47, 17.0%) and blaIMP-like carriers (1/47, 2.1%) (Table 2).
 |
Table 2 Results from the Prospective Study, Showing Agreements and Differences Between the mrCIM, reCIM and Molecular Results. Results for 2.5 h Growth Time of the Indicator Strain |
Sensitivity and Specificity of mrCIM and reCIM in Retrospective Analysis
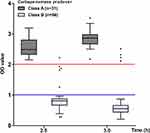
A total of 247 CRE isolates were firstly screened for carbapenemase genes, followed by tests with mCIM and mrCIM to evaluate the sensitivity and specificity of mrCIM due to the changes in conditions compared with the original rCIM. The isolates included 107 carbapenemase producers and 140 non-carbapenemase producers. At 2.5 h of incubation, the indicator strain, when challenged with inactivated antibiotic, grew to a median of OD value 3.13 (range 1.61–4.00, IQR 2.85–3.42) (Figure 2). In contrast, when challenged with active antibiotic, the median growth was of 0.73 (range 0.15–2.21, IQR 0.54–0.88) (Figure 2). As shown in Table 1, at 2.5 h post incubation, the mrCIM correctly identified 96.3% of carbapenemase producers (103/107) and 98.6% of non-carbapenemase producers (138/140), respectively. Two Enterobacter cloacae complex isolates which produced growth around 1.5 McFarland units at 2.5 h were further incubated for 30 mins, and growth declined to less than 1.0 McFarland units. Consequently, the accuracy of mrCIM of examining non-carbapenemase producers increased to 100% (140/140). Thus, the sensitivity of mrCIM was 96.3% (95% CI 90.1–98.8%) and the specificity was 100% (95% CI 96.7%%-100%) at 3 hrs. Among the undetected strains, there were one Escherichia coli carrying blaNDM-5, one Enterobacter cloacae complex carrying blaIMP-4, one Enterobacter cloacae complex carrying blaNDM-1 and blaIMP-8, one Citrobacter freundii carrying blaKPC-2 and blaIMP-4 (Table 1).
The 107 carbapenemase carriers were further screened by eCIM and reCIM to evaluate the ability to detect metallo-β-lactamases. As shown in Table 1, both eCIM and reCIM correctly identified all the 31 class A carbapenemase carriers. 63/66 (95.5%) class B carbapenemase carriers were detected definitely by eCIM, while 61 isolates were positive by reCIM (92.4%). Detailedly, two Escherichia coli strains with blaNDM, one Enterobacter cloacae complex with blaIMP-4 and two Enterobacter cloacae complex isolates expressing blaNDM-1 and blaIMP-8 got false-negative results in reCIM. At 2.5 h of incubation, the indicator strain in class A carbapenemase positive strains grew to a median of OD value 2.49 (range 2.15–3.19, IQR 2.33–2.78), while the median growth declined to 0.81 (range 0.29–2.22, IQR 0.67–0.88) in class B carbapenemase positive strains (Figure 3). When further incubated to 3 h, the OD value of the blaNDM-1-carrying Escherichia coli with false-negative reCIM result reduced from 1.26 to 0.87 (Figure 3). As a result, the sensitivity of reCIM was 93.9% (95% CI 84.4–98.0%) and the specificity was 100% (95% CI 86.3%%-100%) at 3 h. Since the eCIM-derived carbapenemase phenotype detection methods can not differentiate serine carbapenemase from metallo-β-lactamase in isolated producing multiple-carbapenemases,10 the 10 isolates carrying both class A carbapenemase and class B carbapenemase were not included in the retrospective evaluation of reCIM.
Prospective Evaluation of mrCIM and reCIM
The 47 CRE isolates of prospective study were identified as carbapenem resistant with resistance to ertapenem, imipenem or meropenem in routine antimicrobial susceptibility tests and then tested by mrCIM. Using the cut-off defined in the retrospective study, 41 strains (87.2%, 41/47) got positive results at 2.5 hrs post incubation. With further incubation for 30 mins, another one strain with OD value around 1.8 also got a positive result (Figure 4). The 5 isolates with negative mrCIM results were identified to produce hyperproduced cephalosporinase, ESBL, or hyperproduced cephalosporinases and ESBLs simultaneously. Thus, the specificity of mrCIM in the prospective study was 100% (95% CI 46.3–100%), and the sensitivities were 97.6% (95% CI 85.9–99.9%) and 100% (95% CI 89.6–100%) at 2.5 h and 3 h post incubation, respectively. In a prospective study of reCIM, 8 positive results were observed in strains carrying blaNDM-like genes and 33 negative results seen in isolates expressing blaKPC-like genes at 2.5 h post incubation. Unfortunately, there was no significant decrease in OD value in the blaIMP-like positive strain co-cultured with EDTA (Table 2, Figure 5), even with further incubation. Therefore, the specificity and sensitivity of reCIM in prospective study were 100% (95% CI 87.0–100%) and 88.9% (95% CI 50.7–99.4%), respectively.
Taking together the results of retrospective analysis and prospective analysis, mrCIM had a sensitivity of 96.3% (95% CI 90.1–98.8%) and a specificity of 97.1% (95% CI 92.4–99.1%) at 2.5 h post incubation, and the specificity increased to 98.6% (95% CI 94.4–99.8%) at 3 h. In addition, reCIM showed a sensitivity of 95.4% (95% CI 85.4–98.8%) and a specificity of 100% (95% CI 86.3–100%) at 2.5 h post incubation, and the sensitivity increased to 97.0% (95% CI 88.5–99.5%) at 3 h. These performance characteristics are comparable to the mCIM and eCIM; however, compared with mrCIM and reCIM which need at least 24 hrs to detect results, the mrCIM and reCIM required less than 4 hrs of total work time, which is compatible with the daily practice of a clinical microbiology laboratory.
Discussion
The quick spread of CPE remains a significant clinical and public health concern, making reliable phenotypic detection of carbapenemase production an essential first step in combating this problem. In this work, we present and evaluate the performance of mrCIM test and reCIM. We can conclude that mrCIM has high sensitivity and specificity in the detection of CPE, comparable to the original rCIM14 and the CLSI approved mCIM test.10 Also, reCIM has comparative performance characteristics with eCIM in distinguishing MBLs from carbapenemases. The combined mrCIM and reCIM could not only detect carbapenemase activity in Enterobacteriaceae isolates but also identify Amber B carbapenemases simultaneously.
In this research, the rCIM was modified (mrCIM) to adjust reCIM. To achieve maximum inhibition of MBLs by EDTA without non-specific inhibition of non-class B carbapenemases, 45 min incubation was needed in the pre-incubation step, and 2.5 h to 3 h incubation of indicator E. coli required in the next step. Also, the cut-offs were changed to 2.0 for positives and 1.0 for negatives. Accordingly, these conditions were applied to the combined mrCIM, leading to the difference compared with rCIM. In rCIM, 30 min incubation is needed in the pre-incubation step, and 1.5 h to 2 h incubation of indicator E. coli is required. Cut-off of 1.0 is used to differ between positives and negatives.
In a retrospective study, the mrCIM showed 97.6% of accuracy which was comparable with the original rCIM,16 with 2 false-positive and 4 false-negative results at 2.5 h post sub-incubation. The false-positive results were seen in strains carrying blaCTX-M-1 and blaCTX-M-15 genes, and we hypothesized this result is due to a low carbapenemase activity of ESBL enzymes as previously described.20 Besides, four mrCIM false-negative results were randomly found in isolates harboring blaNDM-5 or blaIMP-4, which were probably caused by partial hydrolysis and low level of some specific carbapenemases or the delay for the ATCC25922 to grow in the presence of meropenem. Therefore, mrCIM may not be suitable for the detection of strains with low carbapenemase activity. However, based on our experimental results, the sensitivity and specificity of detecting carbapenemase in Enterobacteriaceae for mrCIM is comparable with that for the original rCIM, and this was also verified in the prospective analysis.16 What’s more, combined with reCIM we developed in this research, distinction of carbapenemase types could be quickly performed simultaneously.
In both retrospective and prospective analysis, the combined mrCIM and reCIM showed satisfactory detection and identification of class A carbapenemase; however with respective 92% and 95.5% accuracy of identifying class B carbapenemase for reCIM and eCIM, there seem some problems in the identification of MLBs for the EDTA-inhibition-based methods. To achieve complete inhibition of MBLs by EDTA in the retrospective evaluation of reCIM, when the EDTA concentration was increased to twofold or even higher folds, growth inhibition of indicator E. coli were observed in all MBLs strains (data not shown), confirming that these enzymes could be totally inhibited when using a high concentration of EDTA. However, non-specific inhibitions were also detected for non-class B carbapenemases at higher EDTA concentrations.
Compared with other carbapenemase phenotype detection methods described these years,21–24 the combined mrCIM and reCIM have several distinct advantages. Firstly, the detection time is less than 4 hrs, 1 day shorter than the mCIM and eCIM or other reported methods. Secondly, the tests are simple to perform and the results are easy to assess. Thirdly, no special equipment or reagents other than meropenem disks, TSB medium and the EDTA. The former two reagents are common in clinical microbiology lab and the EDTA is stable at ambient temperature and can therefore be kept for several years. Moreover, the tests are accessible to any laboratory throughout the world as it requires only basic laboratory materials.
The mrCIM and reCIM we evaluated in this study also has some limitations. We tested the major carbapenemase types only (NDM, IMP, KPC) as VIM, GES, and OXA-48 carbapenemase-producing Enterobacteriaceae are scarce in Chongqing,18,25 and the performances should be evaluated using other different carbapenemase enzymes. Using PCR and sequencing, several isolates were confirmed to produce multiple different enzymes, including both blaKPC and blaNDM or blaVIM, and reCIM failed to detect MBLs in multi-carbapenemase. This issue has been raised for other phenotypical-based characterization test,8,25 however, the incidence rate of Enterobacteriaceae isolates co-harboring different carbapenemases is relatively low in China, especially in Chongqing.26–28 Some researchers have developed in-house phenotypical methods using EDTA combined boric acid to inhibit MBLs and serine enzymes, respectively.29 Indeed, here the majority of carbapenemase positive strains can be correctly identified at 2.5 hrs post sub-incubation, however the results of isolates with OD. value around 1.5–2.0 are uncertain and prolonged 30 mins incubation are necessary.
Conclusion
Overall, compared to CLSI recommended mCIM and eCIM, the high sensitivity and specificity, the simplicity and convenience, and the low cost of combined mrCIM and reCIM, as well as the significantly decreased turnaround time, make it a useful tool for routine detecting CPE and MBLs in clinical microbiology laboratories. These combined tests not only resolve the main limitation of the original rCIM as they can identify MBLs but also provide same-day results compared with CLSI recommended mCIM and eCIM.
In conclusion, the combined mrCIM and reCIM bring important improvement to phenotypic detection methods of carbapenemase-producing Enterobacteriaceae in clinical microbiology laboratories, guiding the appropriate treatment and efficient implementation of infection control measures of CPE infections.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grants No: 81803110). The funder had no role in study design, experiments, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017;215(suppl1):S28–S36. doi:10.1093/infdis/jiw282
2. Coppi M, Antonelli A, Giani T, et al. Multicenter evaluation of the RAPIDEC® CARBA NP test for rapid screening of carbapenemase-producing Enterobacteriaceae and Gram-negative nonfermenters from clinical specimens. Diagn Microbiol Infect Dis. 2017;88(3):207–213. doi:10.1016/j.diagmicrobio.2017.04.009
3. Bush K, Fisher J. Epidemiological expansion, structural studies, and clinical challenges of new β-lactamases from gram-negative bacteria. Annu Rev Microbiol. 2011;65:455–478. doi:10.1146/annurev-micro-090110-102911
4. Goodman KE, Simner PJ, Tamma PD, Milstone AM. Infection control implications of heterogeneous resistance mechanisms in carbapenem-resistant Enterobacteriaceae (CRE). Expert Rev Anti Infect Ther. 2016;14(1):95–108. doi:10.1586/14787210.2016.1106940
5. Ambler RP. The structure of beta-lactamases. Philos Trans R Soc Lond B Biol Sci. 1980;289(1036):321–331. doi:10.1098/rstb.1980.0049
6. Fasciana T, Gentile B, Aquilina M, et al. Co-existence of virulence factors and antibiotic resistance in new Klebsiella pneumoniae clones emerging in south of Italy. BMC Infect Dis. 2019;19(1):928. doi:10.1186/s12879-019-4565-3
7. Di Tella D, Tamburro M, Guerrizio G, et al. Molecular epidemiological insights into colistin-resistant and carbapenemases-producing clinical Klebsiella pneumoniae isolates. Infect Drug Resist. 2019;12:3783–3795. doi:10.2147/IDR.S226416
8. Tamma PD, Simner PJ. Phenotypic detection of carbapenemase-producing organisms from clinical isolates. J Clin Microbiol. 2018;56(11):e01140–18. doi:10.1128/JCM.01140-18
9. Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Machuca I, Pascual A. Treatment of infections caused by extended-spectrum-beta-lactamase-, ampC-, and carbapenemase-producing Enterobacteriaceae. Clin Microbiol Rev. 2018;31(2):e00079–17. doi:10.1128/CMR.00079-17
10. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing.
11. Lupo A, Papp-Wallace KM, Sendi P, Bonomo RA, Endimiani A. Non-phenotypic tests to detect and characterize antibiotic resistance mechanisms in Enterobacteriaceae. Diagn Microbiol Infect Dis. 2013;77(3):179–194. doi:10.1016/j.diagmicrobio.2013.06.001
12. Rood IGH, Li Q. Review: molecular detection of extended spectrum-β-lactamase- and carbapenemase-producing Enterobacteriaceae in a clinical setting. Diagn Microbiol Infect Dis. 2017;89(3):245–250. doi:10.1016/j.diagmicrobio.2017.07.013
13. Boutal H, Vogel A, Bernabeu S, et al. A multiplex lateral flow immunoassay for the rapid identification of NDM-, KPC-, IMP- and VIM-type and OXA-48-like carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73(4):909–915. doi:10.1093/jac/dkx521
14. Rösner S, Kamalanabhaiah S, Küsters U, Kolbert M, Pfennigwerth N, Mack D. Evaluation of a novel immunochromatographic lateral flow assay for rapid detection of OXA-48, NDM, KPC and VIM carbapenemases in multidrug-resistant Enterobacteriaceae. J Med Microbiol. 2019;68(3):379–381. doi:10.1099/jmm.0.000925
15. Song W, Park MJ, Jeong S, et al. Rapid identification of OXA-48-like, KPC, NDM, and VIM carbapenemase-producing Enterobacteriaceae from culture: evaluation of the RESIST-4 O.K.N.V. multiplex lateral flow assay. Ann Lab Med. 2020;40(3):259–263. doi:10.3343/alm.2020.40.3.259
16. Muntean MM, Muntean AA, Gauthier L, et al. Evaluation of the rapid carbapenem inactivation method (rCIM): a phenotypic screening test for carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73(4):900–908. doi:10.1093/jac/dkx519
17. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing.
18. Sun K, Xu X, Yan J, Zhang L. Evaluation of six phenotypic methods for the detection of carbapenemases in gram-negative bacteria with characterized resistance mechanisms. Ann Lab Med. 2017;37(4):305–312. doi:10.3343/alm.2017.37.4.305
19. Doyle D, Peirano G, Lascols C, Lloyd T, Church DL, Pitout JD. Laboratory detection of Enterobacteriaceae that produce carbapenemases. J Clin Microbiol. 2012;50(12):3877–3880. doi:10.1128/JCM.02117-12
20. Dupont H, Gaillot O, Goetgheluck AS, et al. Molecular characterization of carbapenem-nonsusceptible enterobacterial isolates collected during a prospective interregional survey in France and susceptibility to the novel ceftazidime-avibactam and aztreonam-avibactam combinations. Antimicrob Agents Chemother. 2016;60(1):215–221. doi:10.1128/AAC.01559-15
21. Jing X, Zhou H, Min X, et al. The simplified carbapenem inactivation method (sCIM) for simple and accurate detection of carbapenemase-producing gram-negative bacilli. Front Microbiol. 2018;9:2391. doi:10.3389/fmicb.2018.02391
22. Jing X, Min X, Zhang X, et al. The rapid carbapenemase detection method (rCDM) for rapid and accurate detection of carbapenemase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Front Cell Infect Microbiol. 2019;9:371. doi:10.3389/fcimb.2019.00371
23. Liao Q, Xie Y, Wang C, et al. Development and evaluation of the method for detecting metallo-carbapenemases among carbapenemase-producing Enterobacteriaceae. J Microbiol Methods. 2019;163:105652. doi:10.1016/j.mimet.2019.105652
24. Byun JH, Seo Y, Kim D, et al. An agar plate-based modified carbapenem inactivation method (p-mCIM) for detection of carbapenemase-producing Enterobacteriaceae. J Microbiol Methods. 2020;168:105781. doi:10.1016/j.mimet.2019
25. Zhou M, Wang D, Kudinha T, Yang Q, Yu S, Xu YC. Comparative evaluation of four phenotypic methods for detection of class A and B carbapenemase-producing Enterobacteriaceae in China. J Clin Microbiol. 2018;56(8):e00395–18. doi:10.1128/JCM.00395-18
26. Zhang R, Liu L, Zhou H, et al. Nationwide surveillance of clinical carbapenem-resistant Enterobacteriaceae (CRE) strains in China. EBioMedicine. 2017;19:98–106. doi:10.1016/j.ebiom.2017.04.032
27. Zhang Y, Wang Q, Yin Y, et al. Epidemiology of carbapenem-resistant Enterobacteriaceae infections: report from the China CRE network. Antimicrob Agents Chemother. 2018;62(2):e01882–17. doi:10.1128/AAC.01882-17
28. Wang Q, Wang X, Wang J, et al. Phenotypic and genotypic characterization of carbapenem-resistant Enterobacteriaceae: data from a longitudinal large-scale CRE study in China (2012–2016). Clin Infect Dis. 2018;67(suppl_2):S196–S205. doi:10.1093/cid/ciy660
29. Caméléna F, Cointe A, Mathy V, et al. Within-a-day detection and rapid characterization of carbapenemase by use of a new carbapenem inactivation method-based test, CIMplus. J Clin Microbiol. 2018;56(9):e00137–18. doi:10.1128/JCM.00137-18
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.