Back to Journals » OncoTargets and Therapy » Volume 12
Evaluation of MET T1010I and MET rs40239 single-nucleotide polymorphisms in triple-negative breast cancer: a case–control study
Authors Kalapanida D, Zagouri F, Gazouli M , Tsiakou A, Zografos E , Dimitrakakis C, Marinopoulos S , Giannos A, Sergentanis TN, Kastritis E , Terpos E , Dimopoulos MA
Received 2 October 2018
Accepted for publication 29 November 2018
Published 28 May 2019 Volume 2019:12 Pages 4195—4202
DOI https://doi.org/10.2147/OTT.S189329
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Federico Perche
Despoina Kalapanida,1 Flora Zagouri,1 Maria Gazouli,2 Andriani Tsiakou,3 Eleni Zografos,2 Constantine Dimitrakakis,4 Spyridon Marinopoulos,4 Aris Giannos,4 Theodoros N Sergentanis,1 Efstathios Kastritis,1 Evangelos Terpos,1 Meletios-Athanassios Dimopoulos1
1Department of Clinical Therapeutic, Alexandra Hospital, Medical School, University of Athens, Athens, Greece; 2Department of Basic Medical Sciences, Laboratory of Biology, University of Athens School of Medicine and Laboratory of Cell and Gene Therapy, Biomedical Research Foundation of the Academy of Athens, Athens, Greece; 3First Department of Dermatology, Syggros Hospital, University of Athens School of Medicine, Athens, Greece; 4Department of Obstetrics and Gynaecology, Alexandra Hospital, Medical School, University of Athens, Athens, Greece
Aim: The purpose of this study is to evaluate the role of MET T1010I and MET rs40239 as potential risk factor and/or prognostic markers in patients with triple-negative breast cancer (TNBC).
Methods: 114 samples of DNA from paraffin-embedded breast normal tissues of patients with TNBC and 124 samples of healthy controls were collected and analyzed for MET T1010I and MET rs40239 polymorphisms.
Results: MET T1010I CT genotype was associated with increased risk of TNBC in both univariate and multivariate analysis. The status of rs40239 was not associated with a higher risk for TNBC at either the univariate or the multivariate analysis. None of the examined polymorphisms was associated with overall survival at the univariate or multivariate Cox regression analysis (adjusted HR=1.35, 95% CI: 0.31–5.97 for MET T1010I CT/TT vs CC; adjusted HR=1.78, 95% CI: 0.73–4.35 for rs40239 AG/GG vs AA).
Conclusion: Our case–control study suggests that MET T1010I seems to be a risk factor for TNBC in the Caucasian Greek population, in contrast with MET rs40239, where no correlation was found.
Keywords: SNPS, MET T1010I, MET rs40239, triple-negative breast cancer, biomarker
Introduction
Triple-negative breast cancer (TNBC) constitutes 15–20% of all malignant breast tumors and is characterized by high levels of distal recurrence and a poor outcome.1,2 Single-nucleotide polymorphisms (SNPs) may be risk factors of breast cancer, and may also play a key role in the progress of the disease, the development of drug resistance and the overall survival of breast cancer patients, even though SNPs do not usually function individually but in concert with other factors.3 In recent years, numerous meta-analyses have emerged, showing an association between polymorphisms of functionally important genes, such as BRCA1, TGFβ1, ATG5, PARP1 and TNBC, with great variety across different races and geographic regions.4–7
C-Met is a transmembrane protein, member of the tyrosine kinase receptors family (RTKS) and is mainly expressed in the surface of epithelial and endothelial cells.8 The binding to its ligand, hepatocyte growth factor (HGF), leads to the onset of a cascade of multiple signaling pathways that regulate important biological activities, such as cell growth, proliferation, survival, motility and migration, leading to organogenesis and tissue repair.9,10 Dysregulation of C-Met activity has been associated with multiple processes in carcinogenesis, such as tumor initiation, progression, invasion, metastasis, angiogenesis and drug resistance in multiple malignancies (breast cancer, ovarian cancer, papillary renal cancer, gastric cancer and lung cancer).11–13 Furthermore, c-Met SNPs such as MET rs1621, MET rs11762213 and MET rs41736 have already been established as potential risk factors in a variety of solid tumors.14–16
MET T1010I (also known as T992I) constitutes a germline mutation in the Met gene, located in a non-kinase domain, in a region encoding the intracellular juxtamembrane domain. MET T1010I has been previously associated with non-small lung cancer, gastric cancer, colon cancer, hereditary papillary renal cancer and metastatic breast cancer.17–20 Especially in metastatic breast cancer, the presence of MET T1010I polymorphism resulted in markedly undifferentiated tumors with dense cellularity and a high mitotic index, both in vivo and in vitro, according to Liu et al. Moreover, in the same study, investigators observed that MET T1010I-induced colony formation in the absence of HGF in identical samples.21
MET rs40239 is located in the intron region of the c-Met gene and has been associated with locoregional gastric cancer. Specifically, the G allele of this polymorphism has been associated with a statistically significant improvement in progression-free survival and overall survival in a Japanese cohort.22
The aim of this study is to evaluate the role of Met T1010I and rs40239 as potential risk factors and/or prognostic markers in patients with TNBC who have received chemotherapy, via a case–control study of 114 patients with TNBC and 124 controls.
Methods
Subjects
Incident cases of 114 patients with histologically confirmed TNBC, during the period 2000 through 2014, were recruited. Operations were performed at the Department of Obstetrics and Gynecology, “Alexandra” Hospital, Medical School, University of Athens, Greece, and chemotherapy was administered at the Oncology Department of “Alexandra” Hospital, Medical School, University of Athens, Greece. The exclusion criteria were: no invasive disease, metastatic disease at diagnosis, family history of breast cancer (first-degree relative with breast cancer, known BRCA1 and BRCA2 mutations), history of prior malignancy and no signed informed consent form. Furthermore, additional information on histological characteristics, tumor size, lymph node infiltration, grade, histological stage expression levels of ki67 and p53, disease-free survival and overall survival were collected from patient files and were registered on an electronic database. Regarding controls, women with normal results on routine mammograms were recruited. Cases and controls were individually matched on age (±2 years); controls had no prior history of other malignancy. Both cases and controls were Caucasian and reside in the same geographical region (the greater metropolitan area of Athens, Attika). All participants in the study signed an informed consent form. This case–control study is in accordance with the Helsinki Declaration and has been approved by the Review Board of Alexandra General Hospital of Athens.
Genotyping of MET T1010I and MET rs40239
For TNBC patients, DNA from paraffin-embedded normal breast tissues was isolated with Nucleopsin Tissue kit (Macherey Nigel, Germany). DNA was extracted from the blood of healthy controls using the same kit. PCR was used to amplify the selected sequences, by means of specially designed promoters. Digestion products were collected through restriction fragment length polymorphism (RFLP) and were analyzed for the detection of differences between patients and controls. For T1010I, the primers F: 5ʹ GATCTGGGCAGTGAATTAGTT 3ʹ and R: 5ʹ GTTGTTTATTTTTGGTTTTGCA 3ʹ were used. The PCR product was 226 bp. The PCR produce was digested with the TasI (Tsp509I, Thermo Fisher Scientific) enzyme. In the presence of the C allele were generated two products 17 bp and 209 bp products and in the presence of the T allele were generated three products 17 bp, 70 bp and 139 bp.
For rs40239, the primers F: 5ʹ TTTTATGTCAGTTCCTATTGG 3ʹ and R: 5ʹ CTCTGGAAATGACTGAACTT 3ʹ were used. The PCR product was 285 bp. The PCR produce was digested with the TaiI (MaeII, Thermo Fisher Scientific, Waltham, MA, USA) enzyme. In the presence of the A allele were generated two products 23 bp and 262 bp products and in the presence of the G allele were generated three products 23 bp, 53 bp and 209 bp.
Additionally, the endogenous levels of the corresponding gene products were quantified by ELISA.
Statistical analysis
Descriptive statistics were estimated, separately for cases and controls. Mann–Whitney Wilcoxon test (MWW) and Chi-square test were appropriately implemented for the comparison of demographic, lifestyle and reproductive factors in cases and controls. To analyze the associations between the examined polymorphisms and risk of TNBC, three logistic regression models were estimated: heterozygous vs wild type (the most frequent homozygous genotype was considered “wild type”), homozygous vs wild type and dose–response allele model (0: wild type, 1: heterozygous, 2: homozygous subjects). Unconditional logistic regression analysis was performed to estimate univariate and multivariate ORs with 95% CIs. The multivariate ORs were adjusted for age, smoking, alcohol, body mass index, menopausal status, age at menarche and education; subanalyses for premenopausal and postmenopausal women were conducted. The deviation of allele frequencies in controls from the Hardy–Weinberg equilibrium (HWE) was examined with the appropriate goodness-of-fit Chi-square test, given that the deviation may denote bias.23 Regarding the associations between the examined polymorphisms and overall survival, univariate and multivariate Cox regression analysis were performed; the multivariate Cox regression model was adjusted for patient age, grade (increment by one in the low =1, intermediate =2, high =3 grouping) and stage (increment by one in the I–II–III TNM classification) of breast cancer. Kaplan–Meier survival curves were estimated for the graphic representation of the results.24 Censoring date was January 31, 2016. Statistical analysis was performed using STATA/SE version 13 statistical software (Stata Corporation, College Station, TX, USA).
Results
Demographic characteristics, lifestyle habits, anthropometric and reproductive parameters, in cases and controls, are summarized in Table 1. Case status was associated with younger age at menarche (p=0.023, MWW) and alcohol consumption (p=0.046, Chi-square test). Educational attainment, menopausal status and smoking rates did not differ between cases and controls. 61.4% of TNBC cases were T2, 63.2% were node negative and 86.9% were grade 3 carcinomas.
 | Table 1 Distribution of the 114 triple-negative breast cancer cases and the 124 age-matched controls by demographic, lifestyle and reproductive variables |
Genotype frequencies, unadjusted and adjusted ORs regarding the association between TNBC and the examined polymorphisms are presented in Table 2. MET T1010I CT genotype was associated with increased risk of TNBC (OR=3.88, 95% CI: 1.04–14.47); no homozygous carriers of the MET T1010I T allele were noted in the study sample. The finding persisted at the multivariate logistic regression analysis, adjusted for age, smoking, alcohol consumption, menopausal status, age at menarche and education (adjusted OR=6.07, 95% CI: 1.51–24.46). Despite the smaller numbers in subgroup analyses, the finding was replicated in postmenopausal women (adjusted OR=16.36, 95% CI: 1.82–146.86).
 | Table 2 Genotype frequencies and ORs regarding the association between MET T1010I polymorphism and triple-negative breast cancer risk. Bold values denote statistically significant associations |
The status of rs40239 was not associated with a higher risk for TNBC either at the univariate or at the multivariate analysis (adjusted OR=0.82, 95% CI: 0.46–1.43 for AG; adjusted OR=0.41, 95% CI: 0.03–5.01 for GG vs AA; adjusted OR=0.78, 95% CI: 0.46–1.31 for the allele dose–response model). Subgroup analyses for pre- and postmenopausal women replicated the null associations (Table 3).
 | Table 3 Genotype frequencies and ORs regarding the association between rs40239 polymorphism and triple-negative breast cancer risk. Bold cells denote statistically significant associations |
No significant deviation from HWE was documented for any of the examined polymorphisms (Pearson’s chi2(1) =0.02, p=0.892 for MET T1010I; Pearson’s chi2(1) =2.59, p=0.108 for rs40239). The median follow-up was equal to 9.3 years. The estimated 5-year OS of TNBC patients was equal to 84.6%. The 5-year OS was equal to 84.3% for MET T1010I CC cases vs 88.9% for CT/TT cases; the respective rates were equal to 87.8% for rs40239 AA cases vs 78.7% for AG/GG cases (Figures 1 and 2). None of the examined polymorphisms was associated with overall survival at the univariate or multivariate Cox regression analysis (adjusted HR=1.35, 95% CI: 0.31–5.97 for MET T1010I CT/TT vs CC; adjusted HR=1.78, 95% CI: 0.73–4.35 for rs40239 AG/GG vs AA; Table 4). Figures 1 and 2 present Kaplan–Meier overall survival curves for the studied polymorphisms.
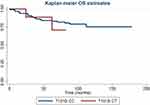 | Figure 1 Kaplan–Meier overall survival (OS) estimates for MET T1010I CC and CT triple-negative breast cancer cases. |
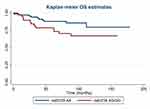 | Figure 2 Kaplan–Meier overall survival (OS) estimates for MET rs40239 AA and AC/GG triple-negative breast cancer cases. |
Discussion
This is the first case–control study that examines the role of MET T1010I and MET rs40239 as potential risk factors and prognostic markers in patients with TNBC. Regarding MET T1010I, our study revealed a significant association between heterozygous genotype CT and an increased risk of TNBC, especially in postmenopausal women. These findings are in agreement with previous results reported by Liu et al, which concerned the role of MET T1010I in breast cancer.21 Collectively, these results indicated that the presence of this polymorphism resulted in undifferentiated tumors with dense cellularity and high mitotic rates in metastatic breast cancer. According to Liu et al study, there were samples where the appearance of MET T1010I induced colony formation independent of HGF existence. This report may suggest that MET T1010I could enhance signaling pathways that are associated with cell abnormal proliferation and development. In this way, MET T1010I could promote breast cancer occurrence. On the other hand, in a study performed by Tilch et al, no significant correlation was presented.25 Although, in the study of Tilch et al, the main point was to screen a large number of Caucasian TNBC and basal like primary breast tumors from Australia to establish the frequency of 238 mutations across 19 oncogenes and not to investigate the association of MET T1010I with TNBC. Furthermore, they used not only FFPE tissue for DNA extraction but also fresh frozen samples in patients with TNBC. Thus, the different purpose, the variant on the origination of cases and the differentiation on biological material that was used for DNA extraction may reflect the discrepancy in the results between the two studies.
Regarding MET rs40239, there was no association with TNBC risk, in contrast with the results reported by Yu Sunakawa et al, who presented a significant association of the polymorphism with gastric cancer risk in Japanese population.22 Although the Kaplan–Meier analysis showed clear separation between AA and AG/GG genotypes and the HR was sizable (adjusted HR=1.78), the sample size and follow-up period did not seem sufficient for establishing a significant association between MET rs40239 and overall survival in TNBC. The variations on biological and molecular features of gastric carcinoma and TNBC, as well as the differences between Caucasians and Japanese population, could reflect the absence of association between MET rs40239 and TNBC in our study.
TNBC is characterized by high biological heterogeneity with increased levels of distal recurrence and poor prognosis, but with a high response rate to chemotherapy, which is the only treatment option. Thus, the discovery of new biomarkers related to TNBC can lead to a better understanding of the disease and may also facilitate the development of new targeted therapies, which will improve patient outcomes. In TNBC, C-Met overexpression coexists with basal markers in numerous trials and has been significantly associated (has a statistically significant association with) with increased risk of recurrence.26–28
An asset of the present case–control study pertains to the fact that no deviation from the HWE was documented in controls’ allele frequencies either for MET T1010I or for MET rs40239. Deviation on HWE may affect the validity of the sample and subsequently, the study, as this fact might indicate selection bias, genotyping errors and population stratification on behalf of the investigation team.
Despite the originality and the statistically significant results, limitations of this case–control study should be acknowledged, hoping to become a stepping stone for improvement. First, this study focused exclusively on the association between the examined polymorphisms and risk of TNBC; these results cannot be extrapolated into non-TNBC carcinomas. Future studies should, therefore, evaluate the assessed polymorphisms in other molecular subtypes (luminal A; luminal B; HER2-enriched) comparing them with the appropriate healthy control subjects. In addition, this study assessed only overall survival, as no details about progression of patients were available; future studies could also evaluate progression-free survival as a surrogate for overall survival.29 Finally, studies with a larger sample size should be designed to confirm results regarding MET T1010I and examine the distinct profiles of homozygous TT carriers that were not present in the study sample. Such larger studies would also allow to examine a possible correlation between MET rs40239 and TNBC survival. Future studies on peripheral blood should be performed, in order to validate our findings, since in the present study the status of polymorphisms was evaluated in paraffin-embedded normal breast tissue.
In conclusion, MET T1010I seems to be a risk factor for TNBC in the Caucasian Greek population, in contrast with MET rs40239, where no correlation was found. Future well-designed studies should be carried out across different races and regions in order to further elucidate the role of these polymorphisms in TNBC.
Acknowledgment
DK received a research grant from Hellenic and the International Society of Molecular Targeted and Personalized Treatments (H.I.S.M.T.P.T.) for the current PhD study.
Disclosure
EK reports grants and personal fees from Amgen, Janssen, and Takeda and personal fees from Genesis Pharma, outside the submitted work. MAD reports personal fees from Amgen, Takeda, Janssen, BMS, and Celgene, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363(20):1938–1948. doi:10.1056/NEJMra1001389
2. Palma G, Frasci G, Chirico A, et al. Triple negative breast cancer: looking for the missing link between biology and treatments. Oncotarget. 2015;6(29):26560–26574. doi:10.18632/oncotarget.5306
3. Rueff J, Gaspar J, Kranendonk M. DNA polymorphisms as modulators of genotoxicity and cancer. Biol Chem. 2002;383(6):923–932. doi:10.1515/BC.2002.099
4. Liu X, Li H, Shao B, et al. Identification of recurrent BRCA1 mutation and its clinical relevance in Chinese triple-negative breast cancer cohort. Cancer Med. 2017;6(3):547–554. doi:10.1002/cam4.1004
5. Vitiello GAF, Guembarovski RL, Hirata BKB, et al. Transforming growth factor beta 1 (TGFβ1) polymorphisms and haplotype structures have dual roles in breast cancer pathogenesis. J Cancer Res Clin Oncol. 2018;144(4):645–655. doi:10.1007/s00432-018-2585-9
6. Li M, Ma F, Wang J, et al. Genetic polymorphisms of autophagy-related gene 5 (ATG5) rs473543 predict different disease-free survivals of triple-negative breast cancer patients receiving anthracycline- and/or taxane-based adjuvant chemotherapy. Chin J Cancer. 2018;37(1):4. doi:10.1186/s40880-018-0268-1
7. Zhai L, Li S, Li H, et al. Polymorphisms in poly (ADP-ribose) polymerase-1 (PARP1) promoter and 3‘ untranslated region and their association with PARP1 expression in breast cancer patients. Int J Clin Exp Pathol. 2015;8(6):7059–7071.
8. Ho-Yen CM, Green AR, Rakha EA, et al. C-Met in invasive breast cancer: is there a relationship with the basal like subtype? Cancer. 2014;120(2):163–171. doi:10.1002/cncr.28386
9. Maroun CR, Rowlands T. The Met receptor tyrosine kinase: a key player in oncogenesis and drug resistance. Pharmacol Ther. 2014;142(3):316–338. doi:10.1016/j.pharmthera.2013.12.014
10. Ponzo MG, Park M. The Met receptor tyrosine kinase and basal breast cancer. Cell Cycle. 2010;9(6):1043–1050. doi:10.4161/cc.9.6.11033
11. Blumenschein GR
12. Zhang Y, Xia M, Jin K, et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol Cancer. 2018;17(1):45. doi:10.1186/s12943-018-0796-y
13. Gaule PB, Crown J, O‘Donovan N, Duffy MJ. cMet in triple-negative breast cancer: is it a therapeutic target for this subset of breast cancer patients? Expert Opin Ther Targets. 2014;18(9):999–1009. doi:10.1517/14728222.2014.938050
14. Wang Q, Yu X, Li Q, et al. Association between miR-199a rs74723057 and MET rs1621 polymorphism and the risk of hepatocellular carcinoma. Oncotarget. 2016;7(48):79365–79371. doi:10.18632/oncotarget.13033
15. Hakimi AA, Ostrovnaya I, Jacobsen A, et al. Validation and genomic interrogation of the MET variant rs11762213 as a predictor of adverse outcomes in clear cell renal cell carcinoma. Cancer. 2016;122(3):402–410. doi:10.1002/cncr.29765
16. Cao X, Hong X, Jia X, Zhang L, Chen G. Single-nucleotide polymorphism rs41736 located in Met was significantly associated with prognosis of small cell lung cancer patients. Med Oncol. 2014;31(12):333. doi:10.1007/s12032-014-0374-0
17. Ma PC, Jagadeeswaran R, Jagadeesh S, et al. Functional expression and mutations of c-Met and its therapeutic inhibition with SU11274 and small interfering RNA in non-small cell lung cancer. Cancer Research. 2005;65(4):1479–1488. doi:10.1158/0008-5472.CAN-04-2650
18. Schmidt L, Junker K, Nakaigawa N, et al. Novel mutations of the MET proto-oncogene in papillary renal carcinomas. Ongogene. 1999;18(14):2343–2350. doi:10.1038/sj.onc.1202547
19. Lee JH, Han SU, Cho H, et al. A novel germ line juxtamembrane Met mutation in human gastric cancer. Ongogene. 2000;19(43):4947–4953. doi:10.1038/sj.onc.1203874
20. Neklason DW, Done MW, Sargent NR, et al. Activating mutations in MET oncogene in familiar colorectal cancer. BMC Cancer. 2011;11:424. doi:10.1186/1471-2407-11-424
21. Liu S, Meric-Bernstam F, Parinyanitikul N, et al. Functional consequence of MET-T1010I polymorphism in breast cancer. Oncotarget. 2015;5(5):2604–2614.
22. Sunakawa Y, Wakatsuki T, Yang D, et al. Prognostic impact of the c-MET polymorphism on the clinical outcome in locoregional gastric cancer patients. Pharmacogenet Genomics. 2014;24(12):588–596. doi:10.1097/FPC.0000000000000091
23. Rohlfs RV, Weir BS. Distribution of Hardy–Weinberg equilibrium test statistics. Genetics. 2008;180(3):1609–1616. doi:10.1534/genetics.108.088005
24. Thakkinstian A, McElduff P, D‘Este C, Duffy D, Attia J. A method for meta-analysis of molecular association studies. Stat Med. 2005;24(9):1291–1306. doi:10.1002/sim.2010
25. Tilch E, Seidens T, Cocciardi S, et al. Mutations in EGFR, BRAF and RAS are rare in triple-negative and basal like cancers from Caucasian women. Breast Cancer Res Treat. 2014;143(2):385–392. doi:10.1007/s10549-013-2798-1
26. Zagouri F, Bago-Horvath Z, Rössler F, et al. High MET expression is an adverse prognostic factor in patients with triple-negative breast cancer. Br J Cancer. 2013;108(5):1100–1105. doi:10.1038/bjc.2013.31
27. Yan S, Jiao X, Zou H, Li K. Prognostic significance of c-Met in breast cancer: a meta-analysis of 6010 cases. Diagn Pathol. 2015;10:62. doi:10.1186/s13000-015-0296-y
28. Gastaldi S, Comoglio PM, Trusolino L. The Met oncogene and basal-like breast cancer: another culprit to watch out for? Breast Cancer Res. 2010;12(4):208. doi:10.1186/bcr2722
29. Li L, Pan Z. Progression-free survival and time to progression as real surrogate end points for overall survival in advanced breast cancer: a meta-analysis of 37 trials. Clin Breast Cancer. 2018;18(1):63–70. doi:10.1016/j.clbc.2017.07.015
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

