Back to Journals » Advances in Medical Education and Practice » Volume 13
Evaluation of Medical Students’ Knowledge on Palliative Care: A Single Institution Cross-sectional Study
Authors Mosalli RM , Mousa AH , Alshanberi AM, Almatrafi MA
Received 1 April 2022
Accepted for publication 4 August 2022
Published 19 August 2022 Volume 2022:13 Pages 893—901
DOI https://doi.org/10.2147/AMEP.S369006
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Rafat Mohammed Mosalli,1,2 Ahmed Hafez Mousa,3 Asim Muhammed Alshanberi,3,4 Mohammed A Almatrafi2
1Department of Pediatrics, Batterjee Medical College, Jeddah, Saudi Arabia; 2Department of Pediatrics, Um Al-Qura University, Makkah, Saudi Arabia; 3College of Medicine, Batterjee Medical College, Jeddah, Saudi Arabia; 4Department of Community Medicine and Pilgrims Health Care, Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence: Ahmed Hafez Mousa, College of Medicine, Batterjee Medical College, Jeddah, Saudi Arabia, Tel +966 548458786, Email [email protected]
Background: Palliative care is the branch of medicine which has a target of setting focus on the improvement of the quality of life of patients, particularly toward their end of life, such as cases of terminal diseases with low prognosis. Despite growing recognition of the importance of palliative care, a gap remains in medical education. Our study aims to evaluate the current level of knowledge of medical students in regard to palliative care.
Methods: A cross-sectional descriptive study was conducted in Batterjee Medical College, Jeddah, Saudi Arabia, through a period of three months from December 2021 to March 2022.
Results: A total of 254 students participated in our study. Psychosocial and spiritual needs of the patient alongside definition of palliative care were perceived the most important by the students with a mean score of 3.9 each.
Conclusion: Our study concludes that there is an overall lack of confidence among medical students in providing palliative care. We recommend further enhancement and implementation of palliative care as part of undergraduate mandatory courses.
Keywords: medical education, palliative care, undergraduate education, end of life care, medical students, curriculum improvement
Introduction
Palliative care is a branch of medicine that focuses on providing a wide range of relief from various sources of disease-related distress.1 Despite growing recognition of the importance of palliative care, a gap remains in medical education.2 Palliative care (PC) provides an essential aspect of clinical management and support to various patients and their families.3 According to the World Health Organization (WHO), palliative care is looked to as an approach that enhances the quality of life for patients and their families.4 During their careers, all doctors will at some point be involved in the care of patients dying, thus future doctors need to be well-prepared for this.5 Our study aims to evaluate the current level of knowledge of medical students in regard to palliative care.
Materials and Methods
Study Design and Setting
A cross-sectional descriptive study conducted in Batterjee Medical College, Jeddah, Saudi Arabia, through a period of three months from December 2021 to March 2022.
Study Population and Sampling Technique
Medical education in Saudi Arabia lasts seven years and consists of a one-year foundation year program (FY1) prior to the first year of medical school (M1). The remaining six years consist of three years (M1, M2, M3) focusing on basic sciences, two years (M4, M5) focusing on clinical sciences, and one year (M6) of obligatory internship. Students from M1 to M5, studying at Batterjee Medical College, not transferred from any other medical institution were included in this study. All students of the faculty of medicine, attending the Batterjee Medical College, were eligible to participate in the study. The minimum sample size was calculated considering a level of confidence of 95%, expected prevalence of 50%, and precision of 0.05 and was found to be 232. To comply with the physical distancing rules in response to the COVID-19 pandemic, recruitment of study participants was done through online invitations on different platforms of social media and in-person interviews conducted with the participants on campus. The survey platform used to administer the survey was Google Forms. Participation was voluntary and participants had the right to withdraw at any time.
Study Tool
The questionnaire used in this research is based on the work of Weber et al.6 The questionnaire contained three components, two of which we utilized in our study. The first component was “perceived importance and education received”. This first part of the questionnaire was based on a translation of the questionnaire done by Weber at al6 and was elaborated with 11 statements concerning various aspects of palliative care. Participants were asked to evaluate these 11 aspects in two ways (as shown in Table 1). The second component was “self-reported confidence”. This part was also based on a translation of the questionnaire by Weber at al.6 Students were asked to report their confidence level with regard to 10 situations in which palliative care was required (as shown in Table 2). The final component was “knowledge”. This portion was evaluated by utilization of the palliative care knowledge questionnaire PEACE-Q.7 Copyright permission for the utilization of the PEACE-Q questionnaire has been purchased and obtained from the original publisher and the authors of the study. No further translation of the questionnaire was needed due to that the primary language used in the medicine program of Batterjee Medical College is English. A pilot study with five M5 students was conducted. The students filled out the questionnaire to establish the comprehensibility, clarity of the questions, handling, and duration. No further changes were needed. A link was then formulated and sent to the study participants. The data were analyzed using SPSS v23. To obtain descriptive results, data were analyzed in line with Weber at al.6 For perceived importance and education, it was reported on a 5-point scale. A score of 3 or below was considered to be an indicator of the item being unimportant and not sufficiently covered, for perceived importance and education respectively. Permission for using the PEACE-Q questioner has been obtained.
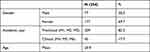 |
Table 1 Characteristics of the Study Participants |
 |
Table 2 Students’ Views on Palliative Care Education and Perception of its Importance (N Students = 254) (Scale 1–5; 1 = Lowest Score; 5 = Highest Score) |
Ethical Considerations
Approvals from Ethics and Scientific Committees (UB-RES-2022) of Batterjee Medical College were obtained before the conduction of the study. Informed online consent was obtained from each participant; the aim of the study was clearly explained and the “Agree to participate” icon was a condition before proceeding in responding to the questionnaire items. Participation was voluntary and participants had the right to withdraw at any time. Data were collected anonymously and the confidentiality of collected data was guaranteed.
Data Analysis
The collected data were statistically analyzed using statistical package for social studies (SPSS) version 23 created by IBM, Chicago, IL, USA. Categorical variables were presented as numbers and percentages. For perceived importance and education, it was reported on a 5-point scale. A score of 3 or below was considered to be an indicator of the item being unimportant and not sufficiently covered, for perceived importance and education respectively. For self-reported confidence levels and the knowledge, scores were calculated within answer categories. The scores for self-reported confidence were coded into “confident” for scores of 3 or more and not “not confident” for scores of 2 or less. For knowledge, several categories were considered and are listed below:
- Philosophy of palliative care (questions 1–3 in Table 4)
- Cancer pain (questions 4–12 in Table 3)
- Side effects of opioids (question 13–15 in Table 4)
- Dyspnea (questions 16–18 in Table 4)
- Nausea and vomiting (questions 19–21 in Table 4)
- Psychological distress (questions 22–24 in Table 4)
- Delirium (questions 25–27 in Table 4)
- Communication (questions 28–30 in Table 4)
- Community-based palliative care (questions 31–33).
 |
Table 3 Self-reported Confidence in the Domains of Palliative Care (N Students = 254) |
 |
Table 4 Knowledge Extrapolated in Relation to Four Topic Scores (%) (N Students = 254) |
Results
Demographics Data
A total of 254 students participated in our study. Among the participants, males 30.3% (77) represented a smaller portion of the sample, whereas the majority were females 69.7% (177). Our participants ranged from first year to senior year medical students in which preclinical students represented 82.3% (209) and clinical year students represented 17.7% (45). The mean age for the participants was 20.9. (Table 1) shows a summary of the demographic data.
Students’ Views
We evaluated the students views on palliative care education and how they perceived its importance (Table 2). Psychosocial and spiritual needs of the patient alongside definition of palliative care were perceived the most important by the students with a mean score of 3.9 each. In addition, the students reported two metrics to be the least for which they received education for, patient-focused work with palliative care patients, psychosocial and spiritual needs of the patient, and knowing what kind of care is available for palliative patients and who plays a role in, each with a mean score of 1.2.
Self-reported Confidence
Self-reported confidence in the domains of palliative care was evaluated (Tables 3 and 4) shows a summary of the knowledge extrapolated in relation to four topic scores. Assessing and examining patients with cancer pain was show to be the most domain in which students reported lack of confidence in 42.9%. In contrast, integrating the psychological aspects of treating and supervising severely ill and dying patients ranked first among the domains which students reported highest confidence in 86.0%. The knowledge extrapolated in relation to four topic scores was assessed and the item which was answered correctly the most was related to the side effects of opioids whereas the item which students showed most wrong answers in was in the questions related to dyspnea. Answers to 33 questions exploring knowledge (%) in responding students is shown (Table 5).
 |
Table 5 Answers to 33 Questions Exploring Knowledge (%) in Responding Students (N Students = 254) |
Discussion
Our study showed that there is a relative lack of confidence towards a wide range of elements related to palliative care. Many elements were shown to not be covered properly in the educational curriculum. Various studies from different countries (Table 6) showed results like ours that shed light on the gap and the lack of preparedness of medical students to provide palliative care. Anneser et al reported that German medical students go through distress frequently in end-of-life care.9 This finding is in line with our results from Table 4 that show the fact the majority of students claim to be unsure about most of the domains related to palliative care. However, among our findings in Table 3, which evaluated self-reported confidence of students, most students reported to be confident, which is an alarming sign shedding light on a false perception the students have toward their levels of confidence.
 |
Table 6 Summary of Key Findings from Other Studies |
Reasons for false perception vary, a specific reason was addressed by Zimmermann et al10 which found that there is a strong stigma attached to palliative care which may persist even after positive experiences with an early palliative care intervention. Another study conducted by Helen B. Miltiades21 found that almost 40% of students reported not having sufficient knowledge. A study conducted by Leung and Wong11 investigated the confidence of students in providing palliative care and their findings showed that 59.5% were non-confident in providing palliative care. Our study while exploring the knowledge of students had three parameters, correct, wrong, and I do not know, the latter showed to be the most utilized answer by our respondents which reflects the lack of confidence, a finding which is consistent with that of Leung and Wong.11
Deficiency in undergraduate medical students’ knowledge is a serious issue which has been highlighted from various perspectives in several studies. A study conducted by Spruit et al12 revealed that the majority of students in the United States stated that they did not get palliative care education whereas just 22% of physicians revealed that they received some form of palliative care education, highlighting a wide gap. Another study conducted in Malaysia including 292 undergraduate medical students and 69 pediatricians found that only a quarter of the respondents thought they have familiarity with fundamentals of palliative care knowledge.13
A specific domain related to the lack of education on certain psychosocial aspects which was a contributor to the relative lack of confidence in knowledge with palliative care. Several studies had findings in line with such a finding. Best et al14 found a confusion present between religious aspects and certain spiritual domains. In their study they investigated and found that such a finding is one of the major contributing factors to reluctance of doctors to discuss palliative care aspects related to spirituality with patients. Another study done by Ellis et al15 found that doctors, on very rare occasions, discuss issues around spirituality with patients in medical consultations. These findings likely stem from the fact the medical school curriculums are primarily based on a biopsychosocial model rather than biopsychosocial-spiritual model.16 Certain studies address challenges in palliative care education in different parts of the world as the Asia-Pacific region has shown interesting findings and a different scope of challenges. An interesting study conducted by Mills et al18 stated there has been progress toward palliative care development in medical education. This progress has been evidenced by many findings including educational preparation, use of medicines, and palliative care services provision in the Asia-Pacific region. International efforts outside the USA have been notable as well. The UK recognized palliative medicine as a core specialty in 1987 and since then massive efforts have been done to constantly and repeatedly update guidelines on palliative care education.19
Limitations
Certain limitations existed in our study. First the inclusion of a single medical school only may have resulted in the generation of results that may not necessarily reflect the overall level of palliative care knowledge of medical students across Saudi Arabia. In addition, the gap present between preclinical and clinical year participants may have led to a somewhat uneven comparison between the different groups due to the varying level of knowledge.
Conclusion
Our study concludes that there is an overall lack of confidence among medical students in providing palliative care. Moreover, an alarming finding was that false perception of good knowledge was present among medical students at an alarming rate evident by most students perceiving themselves as confident with various aspects of providing palliative care yet answering wrongly or being unsure regarding the vast majority of aspects related to palliative care information. Finally, we recommend further enhancement and implementation of palliative care as part of undergraduate mandatory courses.
Data Sharing Statement
Data supporting the findings of the study are available upon request from the corresponding author.
Ethics Approval and Consent to Participate
An informed consent was obtained from all the participating individuals, all the participants had the right to withdraw from the study at any time.
Acknowledgments
The authors would like to thank Reema Dakhilallah Alghanmi, Waqqas Zubair, Nuha Fatima Khan, Taif Mansour, and Bushra Wadi Bin Saddiq who helped in data collection.
Author Contributions
All authors made significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
No funding was provided for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Evangelista CB, Lopes ME, Costa SF, Batista PS, Batista JB, Oliveira AM. Palliative care and spirituality: an integrative literature review. Rev Bras Enferm. 2016. 69(3):591–601. English, Portuguese. PMID: 27355311. doi:10.1590/0034-7167.2016690324i
2. Cowfer B, McGrath C, Trowbridge A. Teaching pediatric palliative care communication skills to fourth-year medical students through role-play. MedEdPORTAL. 2020;16:10991. PMID: 33094157; PMCID: PMC7566222. doi:10.15766/mep_2374-8265.10991
3. Swami M, Case AA. Effective palliative care: what is involved? Oncology. 2018;32(4):180–184. PMID: 29684230.
4. World Health Organisation (WHO). Definition of palliative care. Erişim Linki. Available from: www.who.int/cancer/palliative/deffinition/en.
5. Diver R, Quince T, Barclay S, et al. Palliative care in medical practice: medical students’ expectations. BMJ Support Palliat Care. 2018;8(3):285–288. PMID: 29622688. doi:10.1136/bmjspcare-2017-001486
6. Gibbins J, McCoubrie R, Forbes K. Why are newly qualified doctors unprepared to care for patients at the end of life? Med Educ. 2011;45(4):389-99. PMID: 21401687. doi:10.1111/j.1365-2923.2010.03873.x
7. Chen CA, Kotliar D, Drolet BC. Medical education in the United States: do residents feel prepared? Perspect Med Educ. 2015;4(4):181-5.PMID: 26183246; PMCID: PMC4530539. doi:10.1007/s40037-015-0194-8
8. Storarri ACM, de Castro GD, Castiglioni L, et al. Confidence in palliative care issues by medical students and internal medicine residents. BMJ Support Palliat Care. 2019;9:e1. doi:10.1136/bmjspcare-2017-001341
9. Anneser J, Jox RJ, Thurn T, Borasio GD. Physician-assisted suicide, euthanasia and palliative sedation: attitudes and knowledge of medical students. GMS J Med Educ. 2016;33(1):Doc11. PMID: 26958648; PMCID: PMC4766939. doi:10.3205/zma001010
10. Zimmermann C, Swami N, Krzyzanowska M, et al. Perceptions of palliative care among patients with advanced cancer and their caregivers. CMAJ. 2016;188(10):E217–E227. PMID: 27091801; PMCID: PMC4938707. doi:10.1503/cmaj.151171
11. Leung SY, Wong EL. Assessing medical students’ confidence towards provision of palliative care: a cross-sectional study. Int J Environ Res Public Health. 2021;18(15):8071. PMID: 34360364; PMCID: PMC8345455. doi:10.3390/ijerph18158071
12. Spruit JL, Bell CJ, Toly VB, Prince-Paul M. Knowledge, beliefs, and behaviors related to palliative care delivery among pediatric oncology health care providers. J Pediatr Oncol Nurs. 2018;35(4):247–256. doi:10.1177/1043454218764885
13. Chong L, Khalid F. Paediatric palliative care in Malaysia: survey of knowledge base and barriers to referral. Prog Palliat Care. 2014;22(4):195–200. doi:10.1179/1743291X13Y.0000000074
14. Best M, Butow P, Olver I. Why do we find it so hard to discuss spirituality? A qualitative exploration of attitudinal barriers. J Clin Med. 2016;5(9):77. doi:10.3390/jcm5090077
15. Ellis MR, Vinson DC, Ewigman B. Addressing spiritual concerns of patients: family physicians’ attitudes and practices. J Fam Pract. 1999;48:105–109.
16. Geer J. Learning Spiritual Care in Dutch Hospitals van de Geer. University of Groningen; 2017:12–38.
17. Abuhammad S, Muflih S, Alazzam S, Gharaibeh H, Abuismael L. Knowledge of pediatric palliative care among medical students in Jordan: a cross-sectional study. Ann Med Surg. 2021;64:102246. PMID: 33898025; PMCID: PMC8053886. doi:10.1016/j.amsu.2021.102246
18. Mills J, Kim S, Chan H, et al. Palliative care education in the Asia Pacific: challenges and progress towards palliative care development. Prog Palliat Care. 2021;29(5):251–254. doi:10.1080/09699260.2021.1976951
19. Head BA, Schapmire TJ, Earnshaw L, et al. Improving medical graduates’ training in palliative care: advancing education and practice. Adv Med Educ Pract. 2016;7:99–113. PMID: 26955298; PMCID: PMC4772917. doi:10.2147/AMEP.S94550
20. Yamamoto R, Kizawa Y, Nakazawa Y, Morita T. The palliative care knowledge questionnaire for PEACE: reliability and validity of an instrument to measure palliative care knowledge among physicians. J Palliat Med. 2013;16(11):1423–1428. PMID: 24073719. doi: 10.1089/jpm.2013.0112
21. Miltiades HB. University Students' Attitudes Toward Palliative Care. Am J Hosp Palliat Care. 2020;37(4):300–304. Epub 2019 Sep 19. PMID: 31537081. doi:10.1177/1049909119876911
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
