Back to Journals » International Journal of General Medicine » Volume 9
Evaluation of immunological indices in HIV-infected patients with chronic hepatitis C in Kazakhstan
Authors Sarsekeyeva N, Kosherova B
Received 25 November 2015
Accepted for publication 28 February 2016
Published 23 May 2016 Volume 2016:9 Pages 147—153
DOI https://doi.org/10.2147/IJGM.S101303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nazgul Sarsekeyeva,1,2 Bakhyt Kosherova3
1Department of Infectious Diseases and Dermatovenerology, Karaganda State Medical University, 2Karaganda Regional Center for the AIDS Prevention and Control, 3Rectorate of Karaganda State Medical University, Karaganda, Kazakhstan
Aim: To evaluate immunological indices in HIV-infected patients with chronic hepatitis C (CHC) who are injecting drug users.
Materials and methods: The study examined 38 patients coinfected with HIV and CHC who were injecting drug users and 36 patients with HIV/CHC who were not injecting drug users. In the study of immune status, the relative and absolute numbers of CD3+, CD4+, CD8+, CD16+, and CD20+ cells were determined by means of flow cytofluorometry of “FACSCount” using monoclonal antibodies of the company Becton Dickinson. The level of circulating immune complexes in blood serum was determined by means of precipitation in polyethylene glycol solution.
Results: It was found that T-cell immunodeficiency was developing in patients coinfected with HIV and CHC. T-cell immunodeficiency was characterized by a decrease in the number of T-helpers, mainly for injecting drug users. At the same time, patients coinfected with HIV and CHC experienced markedly elevated levels of circulating immune complexes, mainly among injecting drug users. The evaluation of immunogram indices in injecting drug users coinfected with HIV and CHC, depending on the stage of HIV infection, revealed a greater degree of immune-suppression of T-helper cells in clinical stage III.
Conclusion: Our comprehensive immunological study of patients coinfected with HIV and CHC revealed a pronounced dysfunction of the immune system. The comparison of the immune system indices in patients with HIV/CHC showed a more pronounced T-cell suppression in injecting drug users than in patients with HIV/CHC but who were not injecting drug users.
Keywords: HIV infection, chronic hepatitis C, immunological indices, injecting drug users
Introduction
The relevance of the problem of HIV and hepatitis C is largely uncovered by common epidemiological, social, and economic indices.1,2
Currently, the activation of the immune system plays the leading role in the pathogenesis of immunological disorders with HIV, manifested by an increased rate of proliferation of T- and B-lymphocytes.3–5
HIV infection exacerbates the severity and progression of liver disease associated with hepatitis C virus (HCV) infection. There is a clear link between disease progression and decreased number of CD4 cells, which is considered as the main feature of the pathogenesis of the disease. The distinguishing characteristic of HIV infection is the profound immunodeficiency as a result of progressive qualitative and quantitative insufficiencies of helper T-lymphocytes.6 Dysfunction of the lymphocyte helper inducers leads to spontaneous B-cell activation and development of polyclonal hypergammaglobulinemia at the cost of nonspecific immunoglobulin (Ig) production.7,8
Immunodeficiency state of HIV accelerates the progression of viral hepatitis. It can be linked with the defects in various parts of the immune system: disturbance of antibody production, cellular immunity disorders, defects in phagocytosis, and the complement system.9
Thus, the study of the immune status of HIV infection and viral hepatitis plays a key role as it largely establishes the clinical approach.
As of January 1, 2015, it was estimated that there were 24,216 cases of HIV infection in Kazakhstan. In particular, on November 1, 2015, Karaganda region of Kazakhstan registered 4,286 HIV-infected patients at its dispensary. Meanwhile, the overall figure of HIV-infected individuals with HCV in Karaganda region comprised 1,098 people.10
In Kazakhstan, the high levels of HCV infection in HIV-infected patients can be explained by a significant prevalence of intravenous drug over a sexual infection route. This fact is explained by the drug epidemic that swept Kazakhstan in the late 1990s, which led to HIV infection by intravenous administration of psychoactive substances in 70%–80% of cases. In this regard, the dominant cause of HIV infection and concomitant infection with HCV was the use of intravenous drugs.
The aim of this research was to evaluate immunological indices in HIV-infected patients with chronic hepatitis C (CHC) who are injecting drug users.
Materials and methods
Study design: open and nonrandomized. The study had been approved by the Karaganda State Medical University Ethics Committee. Written, informed consent was obtained from all patients.
Database research: Karaganda Regional Center for the Prevention and Control of AIDS.
Criteria to assign to the study groups included age, 18 years old and above; a verified diagnosis of HIV infection and CHC; and an informed consent to the examination. Exclusion criteria spelled out the following: age younger than 18 years old, patients with nonviral etiology of liver disease, alcohol abuse, patients with the presence of cancer, and severe mental and neurological pathology.
The study included 38 patients coinfected with HIV and CHC who were injecting drug users. To draw a comparison of immunological indices, 36 patients with HIV/CHC but not injecting drug users were concurrently examined.
In patients who used injecting drugs, only an intravenous injection of drugs was marked; however, the abuse drug by the intranasal route was not defined. The abuse drug by the intranasal route was not marked in patients who were not injecting drug users.
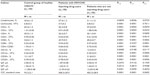
The patients’ description is presented in Table 1. In general, the study groups were comparable (P>0.05).
  | Table 1 Characteristics of coinfected HIV/CHC patients |
The average age of injecting drug users with HIV/CHC was 31.1±0.6 years (median 30.0 years) while the average age of patients with HIV/CHC but not injecting drug users constituted 33.4±0.7 years (median 33.5 years). Sex composition of the group featuring injecting drug users with HIV/CHC consisted of 32 males (84.2%) and six females (15.8%). The sex distribution of the group of patients with HIV/CHC but not injecting drug users had a ratio of 29 (80.6%) versus seven (19.4%), respectively.
Our study was conducted prior to the therapy. Moreover, the patients essentially were in stage I and II of HIV infection without clinical CHC, and they had early stages of fibrosis. It should be noted that patients coinfected with HIV/CHC require individual approach that will take into account their state of immunodeficiency. Patients were followed up in view of their further treatment. Highly active antiretroviral therapy (HAART) was prescribed for HIV/CHC coinfected patients with number of CD4-lymphocytes <350 cells/μL. According to European standards and recommendations, the priority (a first primary) order of antiviral therapy is given to patients with stage F3–F4 of liver fibrosis.
The control group included 20 healthy subjects. In the control group, the mean age was 32.3±1.0 years (median 32.0 years) while sex distribution comprised 16 males (80.0%) and four females (20.0%).
The study involved general clinical research methods (examination of the patient’s medical history, the analysis of peripheral blood). The diagnosis of HIV was verified by immune blotting (Innogenetics, Ghent, Belgium) based on the test system “NEW LAV BLOT”. Verification of hepatitis C was conducted by means of an enzyme immunoassay (anti-HCV) employing the apparatus spectrophotometer Bio-Rad (Bio-Rad Laboratories Inc., Hercules, CA, USA) and using the reagents of Vector-Best (Novosibirsk, Russia; D-0770, D-0771, D-0772). Regarding the RNA detection of HCV and the determination of virus titer and the number of copies, the method of polymerase chain reaction (Rotor-Gene; Corbett Research, Sydney, NSW, Australia) was applied using the reagents with hybridization-fluorescence detection AmpliSens® HCV-FL (InterLabService, Moscow, Russia; D-0798, D-0799).
In the study of immune status, the relative and absolute numbers of CD3+, CD4+, CD8+, CD16+, and CD20+ cells were determined by means of flow cytofluorometry of “FACSCount” using monoclonal antibodies of the company Becton, Dickinson and Company (Franklin Lakes, NJ, USA; reagent kit BD FACSCount™ Reagents # 340167, LOT 41442121). We also have calculated immunoregulatory index (CD4+/CD8+ ratio).11,12 Identification of the serum IgA, IgM, and IgG was conducted through enzyme immunoassay. The level of circulating immune complexes (CIC) in the serum was determined by precipitation in polyethylene glycol solution.
The degree of immunological changes was estimated by the formula by Zemskov.13 For example, in compared groups of HIV/CHC patients who use injecting drugs with control group of healthy subjects: “Patient’s index” divided by “Healthy person’s index” minus 1 multiply by 100%. If the estimated amount had a minus symbol, the immunodeficiency was diagnosed; if there was a plus symbol, hyperactivity of immune system was diagnosed.
Statistical methods
The evaluation of the distribution for normality was carried out using indicators of skewness and kurtosis. The distribution of indices in two groups was normal, and so Student’s t-test was used to assess the differences. Statistical processing of the results was completed with the help of the software package Statistica 6 (Dell Statistica, Tulsa, OK, USA) and determined the arithmetic mean, standard error of the arithmetic mean, standard deviation, and median.
Results
The study conducted a comparative evaluation of immunological indices in injecting drug users coinfected with HIV/CHC and patients with HIV/CHC but not injecting drug users (Table 2).
As a result of the comparative evaluation of the obtained data, it was found that there were marked changes among the majority of immune status indices in injecting drug users with HIV/CHC and in patients with HIV/CHC but not injecting drug users. Similarly, when analyzing the hemograms of patients with HIV/CHC, the number of lymphocytes and leukocytes did not differ significantly as well (P2–3>0.05). The examination of injecting drug users revealed decreased mean values of CD3+ cells and CD4+ cells by 5.39% (P2–3<0.01) and 12.96% (P2–3<0.001). However, injecting drug users showed a reduction in the relative number of CD16+ cells by 15.32% (P2–3<0.05). Injecting drug users with HIV/CHC recorded higher levels of CD8+ cells and CD20+ cells by 8.13% (P2–3<0.001) and 15.60% (P2–3<0.001) compared to the corresponding indices of patients with HIV/CHC but not injecting drug users. At the same time, injecting drug users experienced a decreased value of immunoregulatory index (CD4+/CD8+ ratio) by 20.00% (P2–3<0.001). In addition to the cellular composition, the study investigated the indices of humoral immunity, in particular the levels of IgA, IgM, IgG, and CIC in the blood serum. The average values of IgA, IgM, and IgG in patients with HIV/CHC did not differ significantly (P2–3>0.05). Injecting drug users had a significant increase in the level of CIC by 41.26% (P2–3<0.001).
In the course of further research, the study undertook a comparative evaluation of immunological indices in injecting drug users coinfected with HIV/CHC depending on the clinical stage of HIV infection (Table 3).
The stage of HIV infection was determined according to the clinical classification of World Health Organization.14 In view of this, the distribution among injecting drug users with HIV/CHC depending on the clinical stage of HIV infection was as follows: clinical stage I, 15 (39.5%) patients; stage II, 11 (28.9%); and stage III, 12 (31.6%). Among those surveyed, patients with clinical stage IV were absent.
The comparative evaluation of the immunogram results among injecting drug users with HIV/CHC found no marked differences between indices of clinical stages I and II. The numbers of lymphocytes and leukocytes of patients with stage I or II did not vary significantly (P2–3>0.05). Thus, patients with stage II showed a reduction in the content of CD4+ cells by 14.19% (P2–3<0.05). At the same time, with reference to the immunoregulatory index of (CD4+/CD8+ ratio), a decrease of 15.28% (P2–3<0.05) was recorded for patients with stage II. However, the examination of CD3+, CD8+, CD16+, and CD20+ cells of patients with stage I or II revealed no appreciable differences (P2–3>0.05). Likewise, in both stages, no significant alterations of IgA, IgM, and IgG (P2–3>0.05) in the study of humoral immunity of blood serum were found. In addition, the analysis of indices of the CIC in the two stages did not determine any considerable differences (P2–3>0.05).
The analysis of the immunogram indices of injecting drug users at stages II and III revealed the following changes: patients with stage III in comparison with those with stage II showed a decreased number of lymphocytes and leukocytes by 23.00% (P3–4<0.001) and 16.33% (P3–4<0.05), respectively. It also revealed the increase of 7.18% (P3–4<0.05) in CD8+ cells in patients with stage III when compared with stage II patients. The CD4+/CD8+ ratio in patients with stage III of the disease was reduced by 18.03% (P3–4<0.01). Along with this, there was an increase in the level of the CIC in patients with stage III compared to that of patients in stage II by 34.02% (P3–4<0.05). The assessment of the contents of CD3+, CD4+, CD16+, and CD20+ cells revealed no significant alterations (P3–4>0.05). In the study of IgA, IgM, and IgG in the blood serum at comparable stages, no marked changes were detected (P3–4>0.05).
The greatest changes of immunological indices in injecting drug users were observed between clinical stage I and clinical stage III of HIV infection. Hemogram results revealed that the number of leukocytes and lymphocytes in patients with stages I and III were not notably different (P2–4>0.05). Thus, the relative number of CD3+ and CD4+ cells in patients with stage III as compared with that in patients with stage I was reduced by 9.97% (P2–4<0.01) and 23.10% (P2–4<0.001), respectively. Concurrently, the relative number of CD8+ cells increased by 9.46% (P2–4<0.001) and CD20+ cells went up by 11.34% (P2–4<0.01), accordingly. Moreover, there was a decrease of 30.56% (P2–4<0.001) in CD4+/CD8+ ratio in patients with stage III compared with that of patients with stage I. The average value of CD16+ cells in both stages did not alter drastically (P2–4>0.05). Determination of levels of the three major immunoglobulin classes in the serum showed that the average content of IgA, IgM, and IgG antibodies in patients in both stages did not vary markedly (P2–4>0.05). When evaluating the content of the CIC in patients with stages I and III, no significant distinctions were found (P2–4>0.05).
Discussion
The evaluation of the obtained data revealed significant changes in the number of immune status indices in patients coinfected with HIV/CHC who were injecting drugs users and patients with HIV/CHC who were not injecting drug users. The main immunological marker for monitoring HIV infection remains the level of CD4+ cells.15,16 Development of a helper T-cell immunodeficiency was found in the study of the immune status in patients coinfected with HIV/CHC, especially for injecting drug users. Simultaneously, it was revealed that the relative number of CD8+ cells grew, which denoted immunodeficiency.17,18
An important indicator is the regulatory index, that is, the ratio of the percentage of helper/suppressor (CD4+/CD8+), which is often reduced with immunodeficiency being. Thus, reduction of CD4+ cells and increase of CD8+ cells in patients with HIV/CHC decreased the immunoregulatory index (CD4+/CD8+ ratio), exhibiting a helper immunodeficiency and supporting the findings of other researchers.18,19
The reduction of relative number of CD16+ cells in “injecting drug users” can be regarded as a significant suppression of the natural cytotoxicity, indicating insufficiency of antiviral protection in patients with HIV/CHC.
Infectious process of HIV, occurring as a consequence of disorders of the immune regulation, leads to impaired immunity, which gradually progresses and becomes severe. With the progression of the disease, the number of CD4+ cells is reduced.20,21 In addition to reduction in the number of CD4+ cells in patients coinfected with HIV/CHC, other changes were observed in the immunograms. In particular, there was an increase in the number of CD20+ cells, especially for injecting drug users.
The research of the humoral immunity also involved the measurement of IgA, IgM, and IgG classes of immunoglobulins and CIC in the serum. Through researches, most of the patients with coinfected HIV/CHC were in early clinical stages of HIV infection (68.4%). Alongside with this, an asymptomatic state of the disease, minimal, and medium degree of infection process activity had been noticed in these patients. However, it has been established that immunoglobulin indices in the examined patients changed depending on the stages of HIV infection. Thus, the average values of IgM and IgG rose depending on the clinical stage of HIV infection.
Markedly elevated levels of CIC in the blood serum were the most characteristic changes in the immunograms of patients coinfected with HIV/CHC, especially for injecting drug users. An immunodeficiency state in patients with HIV/CHC occurs not only by impaired cellular immunity but also by deficiency of phagocytic and complement systems. The recruitment of CIC in blood of HIV/CHC patients is determined by decreased functional activity of macrophage phagocytizing system, whereas these particular mechanisms provide CIC elimination from blood flow.21 The cause of CIC level elevation in blood is also a long-lasting persistent infection of CHC in HIV patients.22,23 A wide range of immune system impairments in examined patients worsens as combined with HIV infection and CHC.
Comparative analysis of immunogram results of injecting drug users coinfected with HIV/CHC depending on the stage of HIV infection showed that the greatest changes in indices were observed between asymptomatic clinical stage I and clinical stage III. A large degree of immune-suppression of T-helper cells was herewith observed in clinical stage III.
Currently, a series of similar studies on immune system in patients with HIV monoinfection and HCV monoinfection in comparison with HIV/HCV coinfection are conducted, which predetermine further course of diseases.19,21,24–27 That said, immune status evaluation demonstrates pronounced immunodeficiency state of patients with HIV/HCV coinfection in comparison with HCV monoinfection. Along with this, studies28,29 on patients with HIV/HCV coinfection showed correlation between low level of CD4 cells and later stages of liver fibrosis. In other studies,15,30 it has been established that as quantity of CD4 cells reduces, progression of liver fibrosis in coinfected HIV/HCV patients has been noted.
Conclusion
Our comprehensive immunological study of patients coinfected with HIV and CHC revealed a pronounced dysfunction of immune system. The comparison of the immune system indices in patients with HIV/CHC showed a more pronounced T-cell suppression in injecting drug users than in patients with HIV/CHC but who were not injecting drug users. The degree and range of immune disorders in injecting drug users with HIV/CHC depend on the stage of HIV infection.
Acknowledgment
This work was supported by a research project grant from the Ministry of Health of the Republic of Kazakhstan.
Disclosure
The authors report no conflicts of interest in this work.
References
Andreoni M, Giacometti A, Maida I, Meraviglia P, Ripamonti D, Sarmati L. HIV-HCV co-infection: epidemiology, pathogenesis and therapeutic implications. Eur Rev Med Pharmacol Sci. 2012;16(11):1473–1483. | |
Wandeler G, Gsponer T, Bregenzer A, et al. Hepatitis C virus infections in the Swiss HIV cohort study: a rapidly evolving epidemic. Clin Infect Dis. 2012;55(10):1408–1416. | |
Hyrcza MD, Kovacs C, Loutfy M, et al. Distinct transcriptional profiles in ex vivo CD4+ and CD8+ T cells are established early in human immunodeficiency virus type 1 infection and are characterized by a chronic interferon response as well as extensive transcriptional changes in CD8+ T cells. J Virol. 2007;81(7):3477–3486. | |
Gaiha GD, McKim KJ, Woods M, et al. Dysfunctional HIV-specific CD8+ T cell proliferation is associated with increased caspase-8 activity and mediated by necroptosis. Immunity. 2014;41(6):1001–1012. | |
Dion ML, Poulin JF, Bordi R, et al. HIV infection rapidly induces and maintains a substantial suppression of thymocyte proliferation. Immunity. 2004;21(6):757–768. | |
Balagopal A, Philp FH, Astemborski J, et al. Human immunodeficiency virus-related microbial translocation and progression of hepatitis C. Gastroenterology. 2008;135(1):226–233. | |
Reiche S, Nestler C, Sieg M, et al. Hepatitis C virus (HCV)-specific memory B-cell responses in transiently and chronically infected HIV positive individuals. J Clin Virol. 2014;59(4):218–222. | |
Moir S, Malaspina A, Ogwaro KM, et al. HIV-1 induces phenotypic and functional perturbations of B cells in chronically infected individuals. Proc Natl Acad Sci U S A. 2001;98(18):10362–10367. | |
Shmagel KV, Saidakova EV, Korolevskaya LB, et al. Influence of hepatitis C virus coinfection on CD4+ T cells of HIV-infected patients receiving HAART. AIDS. 2014;28(16):2381–2388. | |
Republican center for the HIV/AIDS prevention and control. The report about AIDS activity for 2014. Almaty. Available from: http://rcaids.kz/ru/publications/page3796/. Accessed January 21, 2015. | |
Yao G, Liang J, Han X, Hou Y. In vivo modulation of the circulating lymphocyte subsets and monocytes by androgen. Int Immunopharmacol. 2003;3(13–14):1853–1860. | |
Zofková I, Kancheva RL. Effect of surgically induced hypoestrinism on immunoregulation in perimenopausal women. Horm Metab Res. 1996;28(4):187–189. | |
Zemskov AM. Clinical Immunology. [The book in Russian]. Moscow: GEOTAR; 2008. | |
World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach; 2013. Available from: http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf?ua=1. Accessed February 11, 2015. | |
Hodowanec AC, Brady KE, Gao W, et al. Characterization of CD4+ T-cell immune activation and interleukin 10 levels among HIV, hepatitis C virus, and HIV/HCV-coinfected patients. J Acquir Immune Defic Syndr. 2013;64(3):232–240. | |
Sajadi MM, Pulijala R, Redfield RR, Talwani R. Chronic immune activation and decreased CD4 cell counts associated with hepatitis C infection in HIV-1 natural viral suppressors. AIDS. 2012;26(15):1879–1884. | |
Barrett L, Gallant M, Howley C, et al. Stronger hepatitis C virus-specific CD8+ T-cell responses in HIV coinfection. J Viral Hepat. 2011;18(3):170–180. | |
Hartling HJ, Gaardbo JC, Ronit A, et al. CD4+ and CD8+ regulatory T cells (Tregs) are elevated and display an active phenotype in patients with chronic HCV mono-infection and HIV/HCV co-infection. Scand J Immunol. 2012;76(3):294–305. | |
Zhuang Y, Wei X, Li Y, et al. HCV coinfection does not alter the frequency of regulatory T cells or CD8+ T cell immune activation in chronically infected HIV+ Chinese subjects. AIDS Res Hum Retroviruses. 2012;28(9):1044–1051. | |
Schnizlein-Bick CT, Spritzler J, Wilkening CL, Nicholson JK, O’Gorman MR. Evaluation of TruCountabsolute-count tubes for determining CD4 and CD8 cell numbers in human immunodeficiency virus-positive adults. Site Investigators and the NIAID DAIDS New Technologies Evaluation Group. Clin Diagn Lab Immunol. 2000;7(3):336–343. | |
Hazenberg MD, Otto SA, van Benthem BH, et al. Persistent immune activation in HIV-1 infection is associated with progression to AIDS. AIDS. 2003;17(13):1881–1888. | |
Dufour DR. Clinical Use of Laboratory Data: A Practical Guide. Baltimore: Williams & Wilkins; 1998. | |
Kondo Y, Ueno Y, Shimosegawa T. Dysfunction of immune systems and host genetic factors in hepatitis C virus infection with persistent normal ALT. Hepat Res Treat. 2011;11:713–716. | |
Ferri S, Lalanne C, Lanzoni G, et al. Redistribution of regulatory T-cells across the evolving stages of chronic hepatitis C. Dig Liver Dis. 2011;43(10):807–813. | |
Bowen DG, Walker CM. Adaptive immune responses in acute and chronic hepatitis C virus infection. Nature. 2005;436:946–952. | |
McCune JM. The dynamics of CD4+ T-cell depletion in HIV disease. Nature. 2001;410:974–979. | |
Hazenberg MD, Hamann D, Schuitemaker H, Miedema F. T cell depletion in HIV-1 infection: how CD4+ T cells go out of stock. Nat Immunol. 2000;1(4):285–289. | |
Glässner A, Eisenhardt M, Kokordelis P, et al. Impaired CD4+ T cell stimulation of NK cell anti-fibrotic activity may contribute to accelerated liver fibrosis progression in HIV/HCV patients. J Hepatol. 2013;59:427–433. | |
Feuth T, van Baarle D, van Erpecum KJ, Siersema PD, Hoepelman AI, Arends JE. CD4/CD8 ratio is a promising candidate for non-invasive measurement of liver fibrosis in chronic HCV-monoinfected patients. Eur J Clin Microbiol Infect Dis. 2014;33:1113–1117. | |
Williams SK, Donaldson E, Van der Kleij T, et al. Quantification of hepatic FOXP3+ T-lymphocytes in HIV/hepatitis C coinfection. J Viral Hepat. 2014;21:251–259. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.