Back to Journals » Journal of Pain Research » Volume 16
Evaluation of Gabapentin as a Treatment of Breakthrough Cancer Pain Caused by Metastatic Prostate Adenocarcinoma
Authors Ismy J , Emril DR, Khalilullah SA , Mauny MP
Received 9 June 2023
Accepted for publication 25 September 2023
Published 2 October 2023 Volume 2023:16 Pages 3319—3324
DOI https://doi.org/10.2147/JPR.S422769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amitabh Gulati
Jufriady Ismy,1 Dessy R Emril,2 Said Alfin Khalilullah,1 Muhammad Puteh Mauny1
1Department of Urology, Faculty of Medicine, Universitas Syiah Kuala/Dr. Zainoel Abidin General Hospital, Aceh, Indonesia; 2Department of Neurology, Faculty of Medicine, Universitas Syiah Kuala/Dr. Zainoel Abidin General Hospital, Aceh, Indonesia
Correspondence: Jufriady Ismy, Department of Urology, Faculty of Medicine, Universitas Syiah Kuala/Dr. Zainoel Abidin General Hospital, Teuku Nyak Arief Street, No. 441, Kopelma Darussalam, Aceh, Indonesia, Email [email protected]
Introduction: Breakthrough Cancer Pain (BTcP) is defined as a temporary increase in pain that occurs spontaneously. The use of gabapentin is believed to be able to reduce pain complaints in patients with BTcP. However, research to support the efficacy of gabapentin in relieving pain in patients with BTcP is still limited. This study aims to determine the effectiveness of the use of gabapentin in patients with BTcP caused by metastatic prostate adenocarcinoma.
Methods: The study was conducted by analytic study with a prospective approach. The subjects were all patients with metastatic prostate adenocarcinoma at Zainoel Abidin General Hospital during 2022– 2023 which fulfilled inclusion and exclusion criteria (30 patients). Data analysis was performed in the form of reduction in pain scale in patients with BTcP caused by metastatic prostate adenocarcinoma using gabapentin and the combination of the opioid gabapentin with T-Test.
Results: The results showed that there was no significant difference between the reduction in posttreatment pain in patients with BTcP caused by metastatic prostate adenocarcinoma taking gabapentin alone or taking the opioid gabapentin combination, either on days 3– 4 or on days 5– 6 (p > 0.05). However, based on the results of the evaluation on day 3– 4, it was found that gabapentin was able to reduce pain by 2.2272, whereas the combination of opioid gabapentin was only able to reduce pain by 1.916. The evaluation on days 5– 6 showed that gabapentin was able to reduce pain by 4.1363 and the combination of gabapentin opioids by 3.2083.
Conclusion: The conclusion of this research is that gabapentin is effective in the treatment of BTcP caused by metastatic prostate adenocarcinoma.
Keywords: gabapentin, breakthrough cancer pain, metastatic prostate adenocarcinoma
Introduction
Cancer is still one of the leading causes of death in the world. World Health Organization in 2019 mentions cancer as the first or second cause of death before the age of 70 in 112 of 183 countries.1 The Health Survey by the Ministry of Health in 2018 also showed an increase in the incidence of cancer in Indonesia from 1.4% of cases to 1.8% of cases.2 One of the problems often caused by cancer is pain. Results of a study by Sofyan et al (2019) at Cipto Mangunkusumo and the National Cancer Center Dharmais Hospital showed that out of 57 research subjects with a mean age of 45.91, 31.6% of them complained of neuropathic cancer pain.3
Prostate cancer is a major health problem, accounting for 1.3 million new cases of prostate cancer worldwide each year. Approximately 10 million men are currently living with prostate cancer, and around 700,000 of them have metastases. Metastatic prostate cancer accounts for >400,000 deaths annually, and these deaths are expected to double over by 2040. The same number of men is expected to live with treatment-related morbidity for >10 years after diagnosis. Prostate cancer is most commonly diagnosed in men aged 55–74 years with a median age of 66 years at diagnosis. Many study efforts continue to expand our understanding of prostate cancer.4
Pain felt by patients with cancer can trigger a sudden and uncontrollable spike in pain called breakthrough cancer pain (BTcP). Approximately 70%–80% of BTcP complaints can be felt by patients with cancer.5 An observational study conducted in Spain in 2019 on 3765 patients with cancer who visited the clinic for 1 month obtained about 1117 (30%) patients experiencing cancer pain, and around 539 (48%–95%) patients experiencing BTcP complaints.6
To reduce these complaints, optimal management is needed to improve the patient’s quality of life. Opioids are one of the analgesics that are often used for the treatment of BTcP. However, opioids are not able to provide a good response to pain with short episodes; this is based on drug tolerance and side effects caused by opioids.7 In addition to opioids, currently the use of anticonvulsants is also believed to reduce pain complaints.
This is supported by a study conducted by Smith et al (2020) showing that the use of gabapentin was able to result in a decrease in pain, neurosensory symptoms, and general systemic symptoms in patients with cancer.8 Another study conducted by Bao et al (2021) showed that the use of opioids in combination with gabapentin was also effectively able to reduce complaints of neuropathic cancer pain compared to the use of opioids alone.9
Until now, the management of cancer pain in prostate cancer focuses on NSAIDs, opioids, and radiotherapy, which are quite effective in pain relief. However, many health facilities do not yet have radiotherapy for pain management. To our knowledge, no studies have reported the management of BTcP in metastatic prostate cancer. Moreover, there have been many studies that mention the benefits of anticonvulsants such as gabapentin in the management of cancer pain.6,8
Gabapentin is an antipain that is often used in patients with cancer pain, especially neuropathic cancer pain.10 However, research that discusses further on the effectiveness of gabapentin for the management of patients with BTcP is still very limited. An analysis is needed to assess the effectiveness of gabapentin in the treatment of BTcP caused by metastatic prostate adenocarcinoma.
Method
In this prospective study with double-blind design, we collected data from 30 patients with BTcP metastatic prostate adenocarcinoma at a single institute between January 2022 and March 2023. This study was registered to the Medical and Health Research Ethics Committee (409/EA/FK-RSUDZA/2021) and approved by the appropriate institutes’ ethics committee of Medical Faculty, Universitas Syiah Kuala, Dr Zainoel Abidin General Hospital. This clinical investigation was conducted in compliance with the principles that have their origin in the latest version of the Declaration of Helsinki.
The patients were divided into two group of treatments, gabapentin and the combination of gabapentin with opioids. Inclusion criteria: All patients with metastatic prostate adenocarcinoma who had BTcP and numeric rating scale score (for evaluate pain score) more than seven. In addition, the exclusion criteria: All patients who had comorbidities that caused pain complaints and patients who had decreased consciousness.
All statistical data analyses were performed using Shapiro–Wilk tests to analyze the normality of data. When data distribution was skewed, we analyze the data using a nonparametric test. Differences in baseline or final data between two groups were analyzed using an independent T-test. A p-value < 0.05 was considered statistically significant (confidence interval: 95%).
Results
Characteristics of Patients with BTcP Caused by Metastatic Prostate Adenocarcinoma
The characteristics of patients with BTcP caused by metastatic prostate adenocarcinoma can be seen in Table 1.
 |
Table 1 Characteristics of Patients with BTcP Caused by Metastatic Prostate Adenocarcinoma |
In 30 patients with metastatic prostate adenocarcinoma in this study, 13 of them had BTcP with the highest age range >65 years (56.6%). Treatment with the combined opioid gabapentin is a treatment that is used more in patients with BTcP caused by metastatic prostate adenocarcinoma. Based on the type of pain experienced by BTcP patients, it was found that all patients experienced mixed pain.
Reduction of Pain in Each Class of Painkillers Given to Patients with BTcP Caused by Metastatic Prostate Adenocarcinoma
The description of pain reduction in each antipain group given to patients with BTcP caused by metastatic prostate adenocarcinoma can be seen in Table 2.
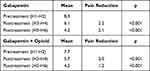 |
Table 2 Pain Reduction in Each Anti-Pain Group |
This study showed that the mean pain before gabapentin administration was 8.3 and decreased to 6.1 (days 3–4) and 4.2 (days 5–6). This difference was significant based on the statistical test (p < 0.001), so it can be concluded that there was a significant difference between pain before treatment and pain after treatment of BTcP patients using gabapentin.
The combined use of the opioid gabapentin also showed significant pain reduction, with pain reduction to 1.9 (days 3–4) and 3.2 (days 5–6) from baseline pain 7.7. The results showed that gabapentin given to patients with BTcP caused by prostate metastatic adenocarcinoma was better at reducing pain (2.2 to 4.1) pain relief than the combination of gabapentin and opioids (1.9–3.2 pain reduction).
Comparison of Pain Scale Reduction for Each Antipain Group in Patients with BTcP Caused by Metastatic Prostate Adenocarcinoma
Comparison of pain scale reduction of each antipain class in patients with BTcP caused by metastatic prostate adenocarcinoma based on T-Test can be seen in Table 3.
 |
Table 3 Comparison of Pain Reduction for Each Antipain Group |
The table shows that there was no significant difference between posttreatment pain reduction in patients with BTcP caused by metastatic prostate adenocarcinoma using gabapentin alone or using the opioid gabapentin combination, both on days 3–4 and 5–6 (p > 0.05). But based on the results of the evaluation on day 3–4, it was found that gabapentin can reduce pain by 2.2, whereas the combination of gabapentin opioids can only reduce pain by 1.9. Evaluation on days 5–6 showed that gabapentin was able to reduce pain by 4.1 and the combined opioid gabapentin by 3.2.
Discussion
This study showed that most patients with BTcP caused by metastatic prostate adenocarcinoma were in the age range >65 years. In a retrospective study conducted by Rahmadi et al (2017), it was stated that most patients who experienced BTcP were in the age range of 45–64 years (51.49%).10 Munoz et al (2018) reported that patients with BTcP in a population of patients with chronic neuropathic pain had an average age of 60.2 years.11 Research conducted by Hjermstad et al (2015) also stated that the average age of patients with BTcP was 62.2 years.12
The gabapentin group and combined opioid gabapentin are the two most commonly used painkillers in patients with BTcP. A study conducted by Yang Jong-Yeun et al (2013) showed that the administration of gabapentin at a dose of 3 times a day was significantly able to reduce the pain scale in patients who had complaints of BTcP.13 The results of Bao Hainan et al (2020) states that the combined use of gabapentin and opioids is believed to increase the analgesic effect, reduce the need for opioids, and reduce the side effects of opioids.9
The results showed that all metastatic prostate adenocarcinoma patients with cancer pain and BTcP had mixed pain complaints. In a study conducted by Mishra et al, it was stated that there are three types of pain that underlie the occurrence of BTcP, namely nociceptive, neuropathic, and mixed pain. Among these types of pain, neuropathic pain and mixed pain are the most dominant.14 In a study conducted by Mercadante et al (2021–) it was stated that mixed pain was the most common type of pain experienced by patients with BTcP, which was 64.1%.15
The results showed that there was no significant difference between the reduction in posttreatment pain in patients with BTcP caused by metastatic prostate adenocarcinoma who used gabapentin alone or using the combination of opioid gabapentin, either on days 3–4 or on days 5–6 but based on the results of the evaluation on days 3–4 found that gabapentin was able to reduce pain by 2.2, whereas the combination of opioid gabapentin was only able to reduce pain by 1.9. The evaluation on days 5–6 showed that gabapentin was able to reduce pain by 4.1 and the combination of gabapentin opioids by 3.2. This proves that gabapentin is more effective in reducing pain complaints in patients with BTcP caused by metastatic prostate adenocarcinoma than the combination of opioid gabapentin.
There are no other studies that discuss the comparison of the two antipain groups for the management of BTcP. However, the results of research on the effectiveness of gabapentin on patients with BTcP are in line with research conducted by Jong-Yeun Yang et al (2013) which showed that giving gabapentin at a dose of 3 times a day was significantly able to reduce the pain scale in patients who had complaints of BTcP. In this case, the use of anticonvulsants is believed to reduce complaints of pain.13
This is supported by a study conducted by Michael Ghiam et al (2020), where 79 patients included in this study showed that the use of gabapentin was able to produce pain reduction.8 So Young Yoon also mentioned that pregabalin and gabapentin have been proposed as first-line treatments for neuropathic cancer pain. Gabapentin has fewer side effects than other drugs, such as valproic acid and carbamazepine. Gabapentin is currently widely used because several clinical trials have shown good results in reducing neuropathic pain either alone or in combination with opioids.10
Gabapentin works in reducing pain by binding to the subunit α2δ-1 voltage gated calcium channel in spinal cord and central nervous system. The binding of gabapentin to these subunits is able to reduce the entry of calcium, which results in a decrease in the release of neurotransmitters that play a role in the process of pain. The alpha subunit is responsible for determining through which calcium ions will enter the cell. Therefore, the presence of gabapentin in binding to the subunit α2δ-1 is believed to be able to destabilize macromolecular complexes that maintain calcium influx at the presynaptic terminal surface. Although gabapentin has no direct effect on calcium influx, it does act by influencing the amount of calcium available in the plasma membrane.16
Gabapentin has a half-life of 5–7 hr and is usually given 3 times a day. Gabapentin reaches plasma concentrations after 2–3 hr of oral administration. The initial dose of gabapentin is 300 mg and is increased by 300 mg daily to a total of 900 mg daily.13 If the patient fails to tolerate an increased dose of gabapentin, the dose is decreased one level and will be continued for the duration of treatment until other pain medications are no longer needed.8
In addition to gabapentin, the combination of opioid gabapentin is also believed to be able to reduce the scale of pain felt by patients. This is in accordance with the research conducted by Hainan Bao et al (2021) by comparing the use of opioids and the combined opioid gabapentin. This study shows that the combination of gabapentin and opioids can significantly reduce neuropathic cancer pain compared to opioids alone. The combination of gabapentin and opioids has been shown to significantly inhibit neuronal responses and reduce pain intensity. In terms of drug interactions, opioids are able to increase the absorption of gabapentin by reducing intestinal motility and increasing the analgesic effect.9
Although the combination of gabapentin opioids is also believed to reduce pain, the side effects are stronger than the administration of gabapentin alone. This is in line with a study conducted by a German group that patients taking a combination of gabapentin and morphine showed higher side effects than patients receiving only one drug. Other studies mention some side effects caused by the use of gabapentin opioids such as drowsiness, chorea, spatiotemporal disorientation, visual hallucinations, and episodes of psychosis.17 The side effects caused by the use of gabapentin, such as dizziness and mild drowsiness, usually occur during the titration phase.
Our study has a limitation due to the single-center study. Future studies with high-quality prospective multicenter and randomized control trials are needed. While there are some limitations, this preliminary study can be an initial scientific basis for the development of gabapentinoid administration in controlling BTcP in patients with metastatic adenocarcinoma of the prostate.
Notably, the findings in this study have a good implication for the knowledge of BTcP cause by metastatic prostate adenocarcinoma protocols. The management of BTcP in prostate cancer with gabapentin can be considered clinically by providing good results in pain control, as found in this study. In addition, gabapentin can also be an alternative where radiotherapy as pain management is not available or in cases where the side effects of opioids are predominant.
Conclusion
Gabapentins are effective as the treatment of BTcP caused by metastatic prostate adenocarcinoma.
Informed Consent
This study was approved by the ethical committee of Dr Zainoel Abidin General Hospital with number 409/EA/FK-RSUDZA/2021. Informed consent was obtained from the study participants prior to study commencement.
Funding
No funding supports this study.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Ministry of Health RI. Results of basic health research in 2018. Ministry Health Republic Indonesia. 2018;53.
3. Sofyan HR. The prevalence of neuropathic pain in patients with cancer pain at the Hospital Dr. Cipto Mangunkusumo and PKN RS Dharmais. Neurona. 2020;37(3):161–167.
4. Jara C, Del Barco S, Grávalos C, et al. SEOM clinical guideline for treatment of cancer pain (2017). Clin Transl Oncol. 2018;20(1):97–107. doi:10.1007/s12094-017-1791-2
5. Pérez-Hernández C, Blasco A, Gándara Á, et al. Prevalence and characterization of breakthrough pain in patients with cancer in Spain: the CARPE-DIO study. Sci Rep. 2019;9(17701). doi:10.1038/s41598-019-54195-x
6. Davies AN, Elsner F, Filbet MJ, et al. Breakthrough cancer pain (BTcP) management: a review of international and national guidelines. BMJ Support Palliat Care. 2018;8(3):241–249. doi:10.1136/bmjspcare-2017-001467
7. Smith DK, Cmelak A, Niermann K, et al. Preventive use of gabapentin to decrease pain and systemic symptoms in patients with head and neck cancer undergoing chemoradiation. Head Neck. 2020;42(12):3497–3505. doi:10.1002/hed.26407
8. Bao H, Wu Z, Wang Q, et al. The efficacy of gabapentin combined with opioids for neuropathic cancer pain: a meta-analysis. Transl Cancer Res. 2021;10(2):637–644. doi:10.21037/tcr-20-2692
9. Yoon SY, Oh J. Neuropathic cancer pain: prevalence, pathophysiology, and management. Korean J Intern Med. 2018;33(6):1058–1069. doi:10.3904/kjim.2018.162
10. Rahmadi M, Madina U, Sulianto I, et al. Study on dosage range evaluation opioid analgesic for breakthrough pain in cancer patients: a retrospective study. Ann Palliat Med. 2021;10(2):1237–1243. doi:10.21037/apm-20-492
11. Munoz MC, Estevez FV, Lopez AJ, Alvarez AC, Lopez BS. Evaluation of quality of life and satisfaction of patients with neuropathic pain and breakthrough pain: economic impact based on quality of life. Pain Res Treat. 2018;2018:1–8. doi:10.1155/2018/5394021
12. Hjermstad MJ, Kaasa S, Caraceni A, et al. Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer. BMJ Support Palliat Care. 2016;6(3):344–352. doi:10.1136/bmjspcare-2015-000887
13. Yang JY, Lee WI, Shin WK, Kim CH, Baik SW, Kim KH. Administration of four different doses of gabapentin reduces awakening from breakthrough pain and adverse effects in outpatients with neuropathic pain during the initial titration. Korean J Anesthesiol. 2013;65(1):48–54. doi:10.4097/kjae.2013.65.1.48
14. Mishra S, Bhatnagar S, Chaudhary P, Rana SP. Breakthrough cancer pain: review of prevalence, characteristics and management. Indian J Palliat Care. 2009;15(1):14–18. doi:10.4103/0973-1075.53506
15. Mercadante S, Caraceni A, Cuomo A, et al. A Longitudinal Study of Breakthrough Cancer Pain: an Extension of IOPS-MS Study. J Clin Med. 2021;10(11):2273. doi:10.3390/jcm10112273
16. Fornasari D. Pharmacotherapy for Neuropathic Pain: a Review. Pain Ther. 2017;6(Suppl 1):25–33. doi:10.1007/s40122-017-0091-4
17. Quintero GC. Review about gabapentin misuse, interactions, contraindications and side effects. J Exp Pharmacol. 2017;9:13–21. doi:10.2147/JEP.S124391
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
