Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Evaluating the Feasibility and Pretesting the Impact of an Educational and Telemonitoring Program for COPD Patients in Lebanon
Authors Nohra RG , Chaaban T, Sacre H , Salameh P , Aoun Bacha Z , Le Bon Chami B, Abou Rizk F, Makhlouf P , Rothan-Tondeur M
Received 17 September 2021
Accepted for publication 3 April 2022
Published 27 April 2022 Volume 2022:17 Pages 949—965
DOI https://doi.org/10.2147/COPD.S339592
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Rita Georges Nohra,1– 3 Taghrid Chaaban,1,4 Hala Sacre,3 Pascale Salameh,3,5– 7 Zeina Aoun Bacha,8 Beatrice Le Bon Chami,9 Fadi Abou Rizk,10 Paul Makhlouf,11 Monique Rothan-Tondeur1,12
1Chaire Recherche Sciences Infirmières, Laboratoire Educations et Promotion de la santé, LEPS, Université Sorbonne Paris Nord, Villetaneuse, France; 2Faculty of Public Health, Lebanese University, Fanar, Lebanon; 3Institut National de Santé Publique, d’Épidémiologie Clinique et de Toxicologie-Liban, INSPECT-LB, Beirut, Lebanon; 4Faculty of Public Health, Islamic University of Lebanon, Khaldeh - Beirut, Lebanon; 5School of Medicine, Lebanese Amerian University, Byblos, Lebanon; 6Department of Research, Faculty of Pharmacy, Lebanese University, Hadat, Lebanon; 7Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, 2417, Cyprus; 8Department of Pulmonary Disease,Faculty of Medicine, Saint Joseph University, Beirut, Lebanon; 9Department of Pulmonary Disease, Maritime Hospital, Jbeil, Lebanon; 10Department of Pulmonary Disease, American University Medical Center Rizk Hospital, Beirut, Lebanon; 11Department of Pulmonary Disease, Notre Dame du Liban Hospital, Jounieh, Lebanon; 12Chaire Recherche Sciences Infirmières, AP-HP, Paris, France
Correspondence: Rita Georges Nohra, Université Sorbonne Paris Nord, Chaire Recherche Sciences Infirmières, Laboratoire Educations et Promotion de la santé, LEPS, 74 Rue Marcel Cachin, Villetaneuse, 93000, France, Tel +961 76 144 873 ; +33 7 67 23 36 34, Email [email protected]
Purpose: The objective of this study was to investigate the feasibility and pretest the effectiveness of an educational and telemonitoring program in a sample of Lebanese COPD patients to inform the design of a randomized study.
Patients and Methods: This study recruited a convenient sample of 15 patients from the pulmonology departments of four hospitals. Validated questionnaires were adapted to meet the context of this study in terms of adequacy, acceptability, adoption, fidelity, and cost. The impact of this program on quality of life and anxiety was measured by the COPD Assessment Test (CAT), the COPD Clinical Questionnaire (CCQ), and the Hospital Anxiety and Depression Scale (HADS). All measurements were performed before and after the intervention.
Results: All 15 participants who agreed to participate in this intervention found the program adequate and acceptable for addressing COPD-related issues. Regarding adoption, all participants declared having no difficulty explaining to others the content of the education sessions and that they would suggest this program to other COPD patients. In terms of effectiveness, six patients had improving in quality of life scores, and five patients had lower anxiety and depression scores compared to baseline measures. A knowledge assessment was done at the end of each session, showing an increase in knowledge for all participants. Skills were also assessed at the end of the program. Participants made no errors that had an impact on their health. Regarding the cost, it was difficult to evaluate the relative cost of this intervention given the economic situation in the country.
Conclusion: This study is the first to evaluate the application of telehealth to optimize COPD management in Lebanon. The approach proposed gave insights into the different obstacles and facilitating factors for implementing such a project to allow a large-scale work on the adaptation of the COPD patient to his disease in Lebanon.
Keywords: chronic obstructive pulmonary disease, quality of life, telehealth, knowledge, skills
Introduction
Chronic diseases are a major public health problem in Lebanon, contributing to 45% and 38.7% of premature deaths in men and women, respectively.1,2 Patients with a chronic disease such as Chronic Obstructive Pulmonary Disease (COPD) face a double constraint: managing the disease and living with it.3 Quality of life is significantly impaired in COPD patients due to the nature of this chronic, disabling disease, which is not well known by the general public.4 However, understanding COPD makes it easier for patients to accept it and contributes to a better living.5 Therapeutic education has been recognized as an integral and permanent part of the management of patients with chronic diseases.6–8 Nevertheless, to date, there are no standard recommendations on the specific educational topics that should be included in the educational programs offered to COPD patients. Furthermore, there is a lack of educational centers or facilities for COPD patients in Lebanon and a near absence of studies related to the quality of life of Lebanese patients living with COPD.
As lung function may worsen over time, even with the best available care,9 systematic follow-up showed to be essential in COPD patients. However, it requires human resources, time, and high expenses. Hence, telehealth is emerging as a new approach to chronic disease management, despite controversies about its effectiveness. Some studies concluded that telehealth in COPD patients does not produce recognizable or statistically significant improvements in the quality of life of these patients,10 while others reveal a positive outcome in terms of hospitalization rates and stabilization of the clinical status of COPD patients.11 In Lebanon, because of the diversity of the population’s health, educational, and economic needs, some means of collaborative networking and remote interventions used in telehealth may be helpful and even necessary.
Therefore, our study aims to evaluate the feasibility, acceptability, and effectiveness of a therapeutic education program coupled with a telemonitoring system for COPD patients in Lebanon.
Methods
Study Design
This single-group non-randomized feasibility study was conducted to inform the design of a randomized study. Eligible participants were enrolled in a 6-week home-based educational and telemonitoring program. Quantitative data collection methods were used pre, per, and post-intervention.
Patient Involvement
Participants with COPD were not involved in setting the research question, study design development, or choice of outcome measures. However, it is planned to disseminate the main results to study participants and seek patient involvement in refining the study design prior to a full-scale trial.
Study Population
An empirical convenience sample was recruited based on the judgment of the pulmonologists and the willingness of patients to participate.
No formal calculation of the sample size has been performed since this feasibility study involves an intervention that has never been tested before on the Lebanese population.
Participants were considered eligible if they met the following criteria: age ≥ 18 years, a prior diagnosis of COPD, cognitively capable with a suitable health status to participate in the study according to the clinical consensus between nurses and physicians. Exclusion criteria consisted of participants diagnosed with lung cancer or having cognitive problems related to memory loss or speech disorders that would not allow a constructive exchange.
Intervention
Our intervention consisted of a home-based, personalized, therapeutic education program and a telemonitoring system. It was conducted in three phases:12
Phase I: The First Nursing Consultation
Phase I is the diagnostic phase, where the patient received the first home visit from the nurse to elaborate an educational diagnosis and define a personalized program. In this stage, the objectives were to get to know patients, identify their needs and expectations, identify the factors that promote learning and those that may limit it, and formulate the skills to be acquired, mobilized, or maintained, taking into account their priorities to plan an individual program. The nurse explained how the patient should use the oximeter to measure daily the oxygen saturation (SpO2), and how the information collected will be transmitted. The oximeter was connected to each patient phones through Bluetooth and the spO2 was collected through internet to an online health platform that allows for frequent health status updates and rapid response, which can be important.
Phase II: The Education and Telemonitoring Sessions
Phase II is the educational phase, where the patient received one home visit per week from the nurse to encourage him/her to self-assess each of his/her risk factors so that he/she becomes aware that his/ her illness is not inevitable and that he/she can be involved in a behavioral change to reduce the risk of exacerbations plans and implements individual educational sessions. These sessions were conducted face-to-face (with/without the presence of a family caregiver), using educational tools such as PowerPoint presentations and videos. Our program consisted of 6 weekly education sessions. Session 1 was about COPD physiopathology, signs, and symptoms, session 2 included an overview of medications, session 3 was about detecting exacerbations, session 4 covered breathing strategies and exercise, session 5 was about adopting and maintaining a healthy lifestyle (smoking, diet, sleep), and session 6 explained stress and anxiety management. Sessions were individualized and conducted in order of patient preference. A booklet summarizing the content of these sessions was given to each participant. Telemonitoring was conducted throughout the program. Patients transmitted their SpO2 to the nurse every day (usually in the morning) and in case of subjective clinical worsening.
Phase III: The Last Nursing Consultation
Phase III is the evaluation phase, where the nurse assesses, face to face, the skills acquired by the patient during her las visit to patients’ home. This stage enabled the nurse to highlight the changes that occurred in the patient and their maintenance over time. A follow-up by telephone was conducted after one month to assess whether the learning was maintained.
Outcomes Measures
Because an intervention will not be effective if it is not implemented well, it is important to know if the intervention is feasible and effective and if it is deployed correctly.13 Based on Proctor’s lists of outcome variables that can assess program implementation,13 this study evaluated the adequacy, acceptability, adoption, fidelity, and cost of the intervention, using various tools adapted to our context: The pre-referral intervention team inventory (PRITI) to measure the acceptability,14 the adoption of information technology innovation scale to measure the adoption,15 parenting strategies questionnaire for adequacy,16 and the utilization and cost questionnaire to evaluate the total cost of the intervention.17
At phases I and III, several tests were performed to pretesting the impact of the intervention: The COPD assessment test (CAT),18 the COPD clinical questionnaire (CCQ),19 and the Hospital Anxiety and Depression Scale (HADS).20
The skills and expertise of the participants were assessed using questions created for each session.
Adequacy
Adequacy is perceived as the appropriateness, relevance, or compatibility of the innovation or practice.13 Therefore, participants were asked three questions to measure intervention adequacy: 1) Is this program appropriate? 2) Is this program helpful in your daily life? 3) Is this program compatible with your daily life? Responses ranged from 0 (not adequate) to 10 (adequate). The adequacy was assessed the first phase during the educational diagnosis (called D1) and in the third phase during the last consultation (called D2).
Acceptability
Acceptability (or “what” is acceptable) is the perception that a given service is pleasant, acceptable, or satisfying.13 Acceptability is different from the broader concept of satisfaction. Acceptability is more specific and refers to particular steps, whereas satisfaction generally refers to the overall experience. Therefore, we assume that the acceptability assessed is dynamic and evolves with experience so we measured acceptability at all stages of the program. The statements selected to assess the acceptability of the intervention from the participants’ perspective were as follows:
Responses were rated on a 5-point Likert scale from 0 (no opinion) to 4 (strongly agree).
Adoption
Adoption is defined as the intention, initial decision, or action to try or employ an innovation or practice.13 The statements assessing adoption were as follows:
Fidelity
Fidelity is defined as the degree to which an intervention is implemented as prescribed by the original protocol. Achieving and measuring fidelity is subject to a number of challenges. Therefore, a second researcher was asked to assess fidelity in the implementation of this intervention, to evaluate whether the intervention was received and faithful to the original protocol, by comparing the original intervention and the implemented intervention in terms of (1) adherence to the program protocol and (2) the amount of program delivered.
Cost
This intervention was measured in terms of;
(1) general cost of the intervention: materials/patient, (2) Time taken by the nurse to go to the patient, (3) Time spent by the nurse at the patient home, (4) Number of hospitalizations and emergency room visits during the intervention/patient.
Efficacy
COPD Assessment Test (CAT)
The CAT consists of eight questions measured on a 5-point scale, with scores ranging from 0 to 40. Higher scores indicate a higher impact of COPD on the patients’ quality of life.18
Clinical COPD Questionnaire (CCQ)
The CCQ is a 10-item tool used to assess the quality of life of COPD patients. The total score, calculated by summing the scores of the ten questions and dividing the number obtained by ten (the number of items), ranges from 0 (very good health) to 6 (extremely poor health).19
Hospital Anxiety and Depression (HADS)
The HADS aims to measure symptoms of anxiety and depression and consists of 14 items, seven for the anxiety and seven for the depression subscale. Each item is scored on a response-scale with four alternatives ranging between 0 and 3. Recommended cut-off scores are 0–7 for normal, 8–10 for borderline and ≥ 11 for abnormal.20
Assessment of Knowledge and Skills of Participants
Knowledge was assessed at the beginning and the end of each educational session through a 5-item true-false questionnaire set by the researcher and related to the session.
Skills were evaluated at the end of the program through a checklist about the breathing strategies inspired by the technique elaborated by d’Ivernois and Gagnayre, which helps patients master their breathing.21 The criteria sought were whether patients were able to identify the right moment to take the spray, whether they respected the chronology of the gesture, and whether they verified the effectiveness of their gesture. These criteria were evaluated according to the seriousness of the error:
1) the error or omission had health consequences;
2) the error or omission was minor with no consequences;
3) no error or omission; the patient has mastered the quality of the procedure.
Statistical Analysis
Five variables were selected to determine the feasibility of this research program: acceptability, adoption, adequacy, fidelity, cost and impact. Analyses were performed on SPSS version 25 (IBM SPSS Statistics for Windows). The Student’s t-test was used to compare normally distributed continuous variables between two groups, the ANOVA to compare three groups or more, and the Chi-square for binary and/or categorical variables. Data were analyzed according to gender, age, stage of the disease, presence of a caregiver, duration of illness and medical coverage. P value less than 0.05 (≤ 0.05) is considered statistically significant.
Results
Of the 15 patients who agreed to participate in this intervention, 8 lived in the Greater Beirut, 5 in North Lebanon, and 2 in Mount Lebanon. The majority of the participants were females (8/15), with an average age of 77±9.7 years and 9±4 years of COPD diagnosis. Almost half of the respondents had a moderate stage of the disease (6/15), 7 a severe stage, and 2 had a very severe stage of their COPD. Most respondents had a family caregiver (11/15) and were financially responsible for their disease (9/15) (Table 1).
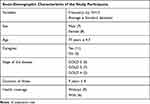 |
Table 1 Sociodemographic Characteristics |
Adequacy
At the end of the program, the mean score for all three adoption questions increased. For the question “Is this program appropriate?”, the average score increased from 7.73±0.57 to 8.6±0.6 (P=0.000). The score for the question “Would this program be helpful in your current life?” increased from 7.26±1.28 to 8.2±0.7 (P=0.004). As for the question “Is this program compatible with your current life?”, the average score increased from 7.2±1.27 to 7.8±0.95 (P=0.004).
Acceptability
All participants found this program an acceptable way to address COPD-related issues. A significant relationship was noted between the age of the participants and the acceptability of this program. Indeed, this program seemed to be more acceptable for participants aged 82 years and younger (3.62±0.51; p=0.05), females (3.57±0.53; p=0.234), those with a severe stage of the disease (3.57±0.53; p=0.368), without a caregiver (3.5±0.57; p=0.662), and without financial coverage for COPD (3.44±0.52; p=0.693) (Table 2). All participants agreed that the educational sessions met their original objective. However, the acceptability, relative to each session, varied. The respiratory strategy and physical exercise session (S4) had a mean score of 3.8±0.4 and the lifestyle session (S5) 3.6±0.47 (Table 3). All participants either strongly agreed (score=4) or agreed (score=3) that education sessions did not negatively impact their daily life. All participants found PowerPoint presentations, videos, and booklet to be quite acceptable tools. As for the telemonitoring system, only eight participants had the necessary equipment for its proper functioning, ie, internet connection and cell phone or IPad. While seven participants agreed to use the telemonitoring system, one patient refused, assuming it would complicate their life. All seven patients who used the telemonitoring system reported that it did not negatively impact their daily lives. One participant was uncompliant in terms of daily monitoring of saturation. None of the participants had an answer to the question “I prefer other methods to help us manage COPD problems”, while five participants mentioned the lack of inhalation devices (treatment) due to the current socioeconomic crisis in the country. Overall, all participants found the program beneficial.
 |
Table 2 Acceptability and Sociodemographic Variables |
 |
Table 3 Acceptability Score Relative to Each Session |
Adoption
All participants declared that their participation in this program was voluntary. All participants agreed that they have no difficulty explaining to others the content of the education sessions and that they would suggest this program to other COPD patients.
As for the question “I am willing to repeat this session if needed” responses varied depending on the educational session. Four participants answered that they would repeat S1 (COPD physiopathology, signs, and symptoms), five participants would repeat S2 (overview of medications), 8 participants would repeat S3 (detecting exacerbations), and almost all participants would repeat S4 (breathing strategies and exercise), S5 (adopting and maintaining a healthy lifestyle), and S6 (stress and anxiety management).
Fidelity
In the protocol, it was planned that the first and last sessions of the intervention take place in the nurse’s office. This clause was not respected. Given the risk of COVID-19 contamination in the hospital, the entire program took place at the participants’ homes while respecting the protective measures. The educational sessions could not be delivered every week, given the situation in Lebanon and the imposed lockdown due to COVID-19. Some sessions were done every two weeks.
Furthermore, the material provided to the patients consisted of the booklet and the monitoring material. It did not include the summary sheet of the educational diagnosis, as foreseen in the protocol to limit the risk of contamination due to COVID-19.
All the educational sessions were completed, except for the telephone follow-up. Only 13 participants could be contacted due to the death of two patients during the month following the intervention.
Cost
The cost of this procedure was measured in terms of time and materials. The total distance traveled by the nurse during the entire intervention period was 5552 Km, each worthing 0.15 USD of gas. The average time spent by the nurse with a patient per eight sessions was 429.56 min. In Lebanon, the wages of a hospital nurse are about 10,000 LBP/60 minutes, equivalent to 6.5 USD/60 minutes at the official rate of 1 USD=1500 LBP. Thus, the cost related to the time the nurse spent per one patient is 46 USD. The cost of materials for educational sessions was 100 USD/patient (cost of booklet, and educational materials), while that for the telemonitoring services was 143 USD/patient (including the cost of the saturomètre). Hence, the overall cost of the intervention was 200 USD/patient (educational sessions only) and 244 USD/patient (including telemonitoring services).
It is noteworthy that, the intervention throughout this study was free of charge. The patients did not cover any cost.
During the intervention, one patient was hospitalized for one week due to a condition not related to COPD.
Impact
CAT
The CAT questionnaire assess the impact of COPD on the patients’ quality of life.18 The scores ranging from 0 to 40 and a higher scores indicate a higher impact. At the end of the program, 8 patients had the same baseline score after the 6 weeks of the intervention (P1, P3, P4, P7, P8, P9, P12, P14), 6 patients had more effective scores than at baseline (P2, P5, P10, P11, P13, P15) while one patient had a deterioration of his quality of life (P6). Participants with improved CAT scores were in the age range ≤82 years, with severe COPD (GOLD 3), diagnosed for ≤10 years, and with a caregiver (Table 4).
 |
Table 4 CAT, CCQ and Sociodemographic Variables |
CCQ
The CCQ tool was also used to assess the quality of life of COPD patients. The score ranges from 0 (very good health) to 6 (extremely poor health).19 At the end of the intervention, a decrease in score was noted in 8 patients (P2, P4, P7, P10, P11, P13, P14, P15), no changes were seen in 4 participants, and a deterioration in health status was identified in 3 patients (P5, P6, P9). Participants with an improvement in the CCQ score belong to the age group ≤ 82 years, female, with severe COPD (GOLD 3), diagnosed for ≤ 10 years, and with a caregiver (Table 4).
HADS
The HADS aims to measure symptoms of anxiety and depression. Scores ranged between 0–7 for normal, 8–10 for borderline and ≥ 11 for abnormal.20 The anxiety score did not change in 6 of the participants after the intervention, 5 patients had an increased score, and 4 patients had a decreased score. Regarding the depression score, the intervention was effective in 5 patients, not effective in 2 patients, and did not induce changes in 8 patients.
SpO2
Seven patients agreed to participate in the telemonitoring system in whom an increase in SaO2 value from baseline was noted with distant desaturation periods. P2 had a saturation limit that varied between 89% and 95%; at the end of the program, this value increased to 91–95% (Figure 1). In P3, the saturation at baseline varied between 89% and 93%, reaching 93–95% at the end of the program (Figure 2). P11 joined the program with a saturation between 87% and 92%; it was about 89–93% at the end of the intervention (Figure 3). For P12, the saturation was between 93% and 96% at the end of the program, higher than the baseline value of 92–95% (Figure 4). After having periods of drops to 91%, the saturation of P13 varied between 93% and 95% at the end of the program (Figure 5). The saturation of P14 reached 97% after having varied between 92% and 95% at the beginning of the program (Figure 6). The lower saturation limit of P15 was 93% at the end of the program, after varying between 90 and 91% at baseline (Figure 7).
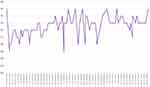 |
Figure 1 SpO2 variation for Patient 2 throughout the program. |
 |
Figure 2 SpO2 variation for Patient 3 throughout the program. |
 |
Figure 3 SpO2 variation for Patient 11 throughout the program. |
 |
Figure 4 SpO2 variation for Patient 12 throughout the program. |
 |
Figure 5 SpO2 variation for Patient 13 throughout the program. |
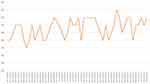 |
Figure 6 SpO2 variation for Patient 14 throughout the program. |
 |
Figure 7 SpO2 variation for Patient 15 throughout the program. |
Assessment of Knowledge and Skills
The knowledge of participants was assessed at the beginning of each educational session and the end of the same session using a 5-item true-false questionnaire. The results showed that all participants had a lack of knowledge related to their disease. At the end of each session, the majority of participants answered all questions correctly (Table 5).
 |
Table 5 Assessment of Participant’s Knowledge |
The skills of participants were evaluated at the end of the program through a checklist created about respiratory strategies. Participants made no errors that had a health consequence, but five of them made errors with no health consequences regarding the timing of the gesture. Also, 11 participants omitted the gesture verification step.
Discussion
The results of this feasibility study show that this program might be feasible and acceptable to the Lebanese population.
A significant relationship was noted between the age of the participants and the acceptability of this program (≥82 years, 3.62 + 0.51; p=0.05). A previous study has shown that younger individuals with COPD reported more symptoms of anxiety and depression, worse health-related quality of life, and more breathlessness only if they were single, suggesting that young individuals, particularly those who are single, have unique needs due to their young age at onset of severe chronic disease.22 This finding can explain the acceptability of our program by younger participants who do not have a caregiver (3.5±0.57; p=0.662).
Studies have shown that COPD management can be more difficult in socioeconomically disadvantaged populations.23 Most participants (9/15) in this study indicated that they were not financially supported in managing their disease and having difficulties in accessing medications and transportation. Furthermore, the results have shown that this program was more acceptable for participants without financial coverage for COPD (3.44±0.52; p= 0.693). Therefore, a more comprehensive chronic disease intervention, involving assistance in accessing treatment, may be more acceptable and beneficial for COPD patients in Lebanon.
The current literature indicates that multidimensional and comprehensive interventions are needed to address the complex and progressive nature of COPD. However, it is unclear which components or combinations of interventions can result in consistent improvements in patient outcomes.23 The results of this study have shown that the respiratory and physical exercises (3.8± 0.4) and lifestyle sessions (3.66±0.47) had the highest acceptability score.
Recruitment appears to be a global problem. It is considered one of the main challenges and recognized as the most considerable barrier.24 In this intervention, of the 50 patients contacted, only 15 agreed to participate. However, despite all the constraints faced during this year, no dropout has been encountered. When analyzing recruitment figures in our study, it appears that there is variability according to the stage of the disease. Indeed, 13 of the 15 participants had a disease stage that varied from moderate to severe, ie, 6 patients GOLD 2 and 7 patients GOLD 3. Therapeutic education is been shown essential at all stages of the disease.25 However, this feasibility study has shown that this therapeutic intervention could be more accepted and effective in Lebanon for patients with moderate (GOLD 2) and severe COPD (GOLD 3).
Furthermore, education showed to have an impact on quality of life.26,27 Indeed, our intervention revealed an improvement in quality of life for half of the participants (6 patients for the CAT score and 8 patients for the CCQ score). The incidence of anxiety and depression also decreased after education sessions. However, anxiety and depression are common psychological problems and are associated with poor prognosis in COPD.28,29 A study has suggested that monitoring of indicators could be improve quality of life and anxiety-depression scores in COPD patients.30
Regarding the telemonitoring system, the use of telehealth in Lebanon is limited.31 Although smartphones (80%) and the internet (76%) are highly used,32 telehealth activities include small-scale interventions for refugees, poor populations,33 and well-defined medical tasks.34 In our study, seven patients used the telemonitoring system and reported that it did not negatively affect their daily life. These patients were satisfied with their participation in this trial. Indeed, the Lebanese population has multiple barriers that can hinder their access to health care. In this context, the adoption of telehealth can help democratize access to health care, increase awareness, and improve education.35 Telehealth services can improve access to health services and reduce health care costs, thus presenting great benefits to all Lebanese residents.35 The widespread adoption and use of telehealth services can also mitigate other social problems, such as traffic and pollution.36 Furthermore, a study has shown that the experience of telehealth during the COVID-19 pandemic appears to have contributed to greater openness and willingness to adopt telehealth in Lebanon.35
Strengths and Limitations
This study was a small-scale, single-group, feasibility study using a convenience sample recruited across four sites. As a result, the generalizability of our results to the broader COPD population is limited. However, the primary objective of this study was to determine the feasibility of a home-based educational program with telemonitoring as a novel way to manage COPD in Lebanon. Hawthorne effect37 (defined as a positive effect observed that is not related to the intervention but is simply due to the fact that this group feels observed, hence the modification of its behavior) can be seen in our study because of the absence of blinding inherent to the design of the protocol. Consequently, a telephone follow-up was conducted one month after the intervention to assess retention. Also, to reduce the effect of confirmation bias, the tendency to favor information that confirms preconceived ideas, a second judge was asked to assess whether the intervention was received and faithful to the original protocol.
Given the current situation in the country and the continuous and rapid change in the value of the Lebanese pound, it was difficult to evaluate the relative cost of this intervention. Therefore, it was decided to keep the official value of 1500 LBP for 1 USD, which may present a bias and an unrealistic view of the current cost of such an intervention in Lebanon.
On the other hand, our intervention included an online health platform that allows for frequent health status updates and rapid response, which can be important.
The innovative aspect of this study lies not only in the use of a telemonitoring system but also in the conduct of education sessions at the participants’ homes. In Lebanon, until now, there is no decree governing the organization and conduct of an educational program for patients living with a chronic disease. Educational programs conducted in Lebanon remain limited to the framework of a study in the hospital; until now, no center or structure of education for patients living with COPD exists in Lebanon. Also, to date, no health insurance in Lebanon covers the use of telehealth systems or even educational programs.
Nerveless, this program is an opportunity for professionals, particularly nurses, to strengthen their capacity. This intervention can be seen as a source of nursing leadership in the care of patients in close cooperation with different health professionals, including physicians, physiotherapists, dieticians, and pharmacists. Also, this intervention could reinforce and make known the importance of the role of the nurse in the out-of-hospital environment, which is not well-recognized in Lebanon.
Results from this study will serve to inform a larger-scale study which can address some of the limitations noted here.
Conclusion
Disease-specific education is an essential part of COPD treatment that affects patients’ quality of life and emotional state. This educational program improved patients’ knowledge of the disease. Furthermore, this feasibility study showed that this intervention could be more accepted and effective in Lebanon among younger patients with COPD stages 2 and 3. The results of this study have shown that the sessions concerning respiratory and physical exercises and lifestyle received the highest acceptability score. Our findings suggest that health insurance initiatives covering education programs and telehealth interventions could be of great interest. In addition, with appropriate support, researcher and patient may be able to work together in a constructive and mutually beneficial manner. The patient could participate in the educational session as a peer education method. This collaboration could contribute to new scientific discoveries.
Abbreviations
COPD, chronic obstructive pulmonary disease; SpO2, oxygen saturation; CAT, COPD assessment test; CCQ, COPD clinical questionnaire; HADS, Hospital Anxiety and Depression scale.
Data Sharing Statement
The dataset may be available from the corresponding author (Rita Georges Nohra) upon reasonable request.
Ethics Statement
This study has been approved by HDF Ethics Committee record (CEHDF 1519, November 4, 2019). All participants were informed about the purpose of the study, that was conducted in accordance with the Declaration of Helsinki. Written consent was obtained from each participant. The study protocol was registered on clinicalTrials.gov 11 December 2019, NCT04196699 and published.12
Acknowledgments
The authors would like to thank the 15 participants of this study and their families for finding the time to participate to our program. Our acknowledgments to Dr Bassem Haber for his advice.
Funding
The budget for this study is supported by the project funding, including a grant from the Lebanese University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ministry of Public Health. Non Communicable Diseases Prevention and Control Plan (NCD-PCP) Lebanon 2016–2020. Published 2016. Available from: http://www.moph.gov.lb/en/DynamicPages/view/3691/non-communicable-diseases-prevention-and-control-plan-ncd-pcp-lebanon-2016-2020-.
2. Yamout R, Adib SM, Hamadeh R, Freidi A, Ammar W. Screening for cardiovascular risk in asymptomatic users of the primary health care network in Lebanon, 2012–2013. Prev Chronic Dis. 2014;11. doi:10.5888/pcd11.140089
3. D’ Ivernois JF, Gagnayre R, les membres du groupe de travail de l’IPCEM. Compétences d’adaptation à la maladie du patient: une proposition. Educ Ther Patient. 2011;3(2):S201–S205. doi:10.1051/tpe/2011103
4. Bahloul N, Kallel N, Moussa N, Gargouri R, Ketata W, Kammoun S. Impact de la BPCO sur la qualité de vie des patients. Rev Mal Respir. 2017;34:A150–A151. doi:10.1016/j.rmr.2016.10.358
5. Le Guillou F, Izadifar A, Piperno D, et al. BPCO et autonomie: impact de la BPCO sur la qualité de vie au quotidien. Rev Mal Respir. 2017;34:A162–A163. doi:10.1016/j.rmr.2016.10.386
6. Autorité de Santé H. Eductaion therapeutique du patient comment la proposer et la realiser? Juin 2007; 2017. Available from: https://www.has-sante.fr/portail/upload/docs/application/pdf/etp_-_comment_la_proposer_et_la_realiser_-_recommandations_juin_2007.pdf.
7. Pétré B, Gagnayre R, De Andrade V, Ziegler O, Guillaume M. From therapeutic patient education principles to educative attitude: the perceptions of health care professionals – a pragmatic approach for defining competencies and resources. Patient Prefer Adherence. 2017;11:603–617. doi:10.2147/PPA.S121892
8. Lagger G, Pataky Z, Golay A. Efficacy of therapeutic patient education in chronic diseases and obesity. Patient Educ Couns. 2010;79(3):283–286. doi:10.1016/j.pec.2010.03.015
9. GOLD. Global Initiative for Chronic Obstructive Lung Disease. GOLD 2017 Global Strategy for the Diagnosis, Management and Prevention of COPD - Global Initiative for Chronic Obstructive Lung Disease - GOLD. https://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/.
10. Vijayan V. Chronic obstructive pulmonary disease. Indian J Med Res. 2013;137:251–269.
11. Esteban C, Moraza J, Iriberri M, et al. Outcomes of a telemonitoring-based program (telEPOC) in frequently hospitalized COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:2919–2930. doi:10.2147/COPD.S115350
12. Nohra RG, Sacre H, Salameh P, Rothan-Tondeur M. Evaluating the feasibility, acceptability and pre testing the impact of a self-management and tele monitoring program for chronic obstructive pulmonary disease patients in Lebanon: protocol for a feasibility study. Medicine. 2020;99(6):e19021. doi:10.1097/MD.0000000000019021
13. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. doi:10.1007/s10488-010-0319-7
14. Yetter G. Assessing the acceptability of problem-solving procedures by school teams: preliminary development of the pre-referral intervention team inventory. J Educ Psychol Consult. 2010;20(2):139–168. doi:10.1080/10474411003785370
15. Moore GC, Benbasat I. Development of an instrument to measure the perceptions of adopting an information technology innovation. Inf Syst Res. 1991;2(3):192–222. doi:10.1287/isre.2.3.192
16. Whittingham K, Sofronoff K, Sheffield JK. Stepping stones triple P: a pilot study to evaluate acceptability of the program by parents of a child diagnosed with an autism spectrum disorder. Res Dev Disabil. 2006;27(4):364–380. doi:10.1016/j.ridd.2005.05.003
17. Kashner MT, Rush JA, Altshuler KZ. Measuring costs of guideline-driven mental health care: the Texas medication algorithm project. J Ment Health Policy Econ. 1999;2(3):111–121. doi:10.1002/(SICI)1099-176X(199909)2:3<111::AID-MHP52>3.0.CO;2-M
18. Al-Moamary MS, Al-Hajjaj MS, Tamim HM, Al-Ghobain MO, Al-Qahtani HA, Al-Kassimi FA. The reliability of an Arabic translation of the chronic obstructive pulmonary disease assessment test. Saudi Med J. 2011;32(10):1028–1033.
19. Ställberg B, Nokela M, Ehrs PO, Hjemdal P, Jonsson E. Validation of the Clinical COPD Questionnaire (CCQ) in primary care. Health Qual Life Outcomes. 2009;7(1):26. doi:10.1186/1477-7525-7-26
20. Al‐Gamal E. Testing of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Int J Nurs Knowl. 2017;28(2):94–99. doi:10.1111/2047-3095.12106
21. Éducation thérapeutique du patient ETP IPCEM; 2021. Available from: https://ipcem.org/.
22. Holm KE, Plaufcan MR, Ford DW, et al. The impact of age on outcomes in chronic obstructive pulmonary disease differs by relationship status. J Behav Med. 2014;37(4):654–663. doi:10.1007/s10865-013-9516-7
23. Collinsworth AW, Brown RM, James CS, Stanford RH, Alemayehu D, Priest EL. The impact of patient education and shared decision making on hospital readmissions for COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1325–1332. doi:10.2147/COPD.S154414
24. Examination of clinical trial costs and barriers for drug development. ASPE. Published April 2, 2015. Available from: https://aspe.hhs.gov/report/examination-clinical-trial-costs-and-barriers-drug-development.
25. Autorité de Santé H. Guide du parcours de soins, Bronchopneumopathie chronique obstructive. [Guide to the care pathway, Chronic obstructive pulmonary disease]. Juin 2014. 2016. Available from: http://www.has-sante.fr/portail/upload/docs/application/pdf/2012-04/guide_parcours_de_soins_bpco_finale.pdf.
26. Oancea C, Fira-Mladinescu O, Timar B, Tudorache V. Impact of medical education program on COPD patients: a cohort prospective study. Wien Klin Wochenschr. 2015;127(9):388–393. doi:10.1007/s00508-015-0712-z
27. López-Campos JL, Quintana Gallego E, Carrasco Hernández L. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis. 2019;14:1503–1515. doi:10.2147/COPD.S170848
28. Cafarella PA, Effing TW, Usmani ZA, Frith PA. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology. 2012;17(4):627–638. doi:10.1111/j.1440-1843.2012.02148.x
29. Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4 Suppl):43S–56S. doi:10.1378/chest.08-0342
30. Van Cauwenberge H, Delroualle A, Hans B, et al. [Telemonitoring of severe COPD patients]. Rev Med Liege. 2019;74(11):566–571. Danish.
31. Saleh S, Khodor R, Alameddine M, Baroud M. Readiness of healthcare providers for eHealth: the case from primary healthcare centers in Lebanon. BMC Health Serv Res. 2016;16(1):644. doi:10.1186/s12913-016-1896-2
32. Lebanon: 2016 TV audience measurement. ipsos. https://www.ipsos.com/en/lebanon-2016-tv-audience-measurement.
33. Saleh S, Farah A, El Arnaout N, et al. mHealth use for non-communicable diseases care in primary health: patients’ perspective from rural settings and refugee camps. J Public Health. 2018;40(suppl_2):ii52–ii63. doi:10.1093/pubmed/fdy172
34. Saleh N, Dirani A, Fadlallah A, et al. Dépistage de la Rétinopathie et de la Maculopathie Diabétique au Liban par Rétinographie et par SD - OCT: intérêt de la Télémédecine. [Screening for Retinopathy and DiabeticMaculopathy in Lebanon by Retinography and SD - OCT: Interest of Telemedicine]. Lebanese Medical. 7–1:(1973)103;2015. doi:10.12816/0012552
35. Helou S, El Helou E, Abou-Khalil V, et al. The effect of the covid-19 pandemic on physicians’ use and perception of telehealth: the case of Lebanon. Int J Environ Res Public Health. 2020;17(13):E4866. doi:10.3390/ijerph17134866
36. Vidal-Alaball J, Franch-Parella J, Lopez Seguí F, Garcia Cuyàs F, Mendioroz Peña J. Impact of a telemedicine program on the reduction in the emission of atmospheric pollutants and journeys by road. Int J Environ Res Public Health. 2019;16(22):E4366. doi:10.3390/ijerph16224366
37. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi:10.1016/j.jclinepi.2013.08.015
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
