Back to Journals » Infection and Drug Resistance » Volume 16
Evaluating the Efficacy and Safety of EZC Pak, a 5-Day Combination Echinacea-Zinc-Vitamin C Dose Pack with or without Vitamin D, in the Management of Outpatient Upper Respiratory Infections
Authors Radhakrishnan A, Spencer S, Yanamala N, Malepati S
Received 2 November 2022
Accepted for publication 16 March 2023
Published 3 May 2023 Volume 2023:16 Pages 2561—2572
DOI https://doi.org/10.2147/IDR.S392087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Aditya Radhakrishnan,1– 3 Stephanie Spencer,4 Naveena Yanamala,1– 3 Sarath Malepati4
1Department of Medicine, Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ, 08901, USA; 2Department of Medicine, West Virginia University School of Medicine, Morgantown, WV, 26506, USA; 3School of Computer Science, Carnegie-Mellon University, Pittsburgh, PA, 15213, USA; 4The PPC Group, Los Angeles, CA, 90049, USA
Correspondence: Sarath Malepati, The PPC Group, 520 South Sepulveda Blvd, Suite 400, Los Angeles, CA, 90049, USA, Tel +1 310 749-8730, Fax +1 877 705-7327, Email [email protected]
Background: Growing antibiotic resistance is among the most serious threats to public health, with antibiotic misuse considered a leading driver of the problem. One of the largest areas of misuse is in outpatient upper respiratory infections (URIs). The purpose of this research is to evaluate the efficacy of EZC Pak, a combination Echinacea-Zinc-Vitamin C dose pack with or without Vitamin D, on the duration of illness and symptom severity of non-specific URIs as an alternative to antibiotics when none are deemed clinically necessary. A secondary analysis was carried out on patient satisfaction.
Methods: A total of 360 patients across the United States were enrolled and randomized in a double-blind manner across two intervention groups, EZC Pak, EZC Pak+Vitamin D, and one placebo group. The study utilized a smartphone-based app to capture data. Once a participant reported the first URI symptom, they were instructed to take the intervention as directed and complete the daily symptom survey score until their symptoms resolved.
Results: The average EZC Pak participant recovered 1.39 days (90% CI 1.05 to 1.73) faster than the average placebo participant (p=0.017). The average EZC Pak participant reported a 17.43% (90% CI 17.1 to 17.8) lower symptom severity score versus placebo (p=0.029). EZC Pak users reported 2.9 times higher patient satisfaction versus placebo users (p=0.012). The addition of Vitamin D neither benefited nor harmed illness duration or symptom severity.
Conclusion: The findings support the potential use of EZC Pak as an alternative to patient request for antibiotics when none are deemed clinically necessary at the time of initial clinical presentation. The decision to replete vitamin D in the acute phase of URI is an individualized decision left to the patient and their clinician. EZC Pak may play a critical role in improving outpatient URI management and antibiotic stewardship (ClinicalTrials.gov number, NCT04943575).
Keywords: upper respiratory infection, antibiotic stewardship, Echinacea, zinc, vitamin D
Introduction
Growing antibiotic resistance and the concomitant rise of drug-resistant pathogens (superbugs) is among the most serious threats to healthcare systems and public health globally. A UK government-commissioned analysis on rising antimicrobial resistance suggests that current growth rates may lead to more deaths from superbugs than cancer by 2050 at a USD $100 trillion cost.1
While there are a host of factors contributing to this complex, multifaceted problem, the World Health Organization (WHO) considers the inappropriate use of antibiotics when none are necessary to be the leading driver of the growth of superbugs.2 The seriousness of this expanding crisis has reached a stage where the WHO is requesting action across government and the private sector to develop strategies that prioritize the reduction of antimicrobial resistance.2,3
While this problem is pervasive across the healthcare system, one of the biggest areas of antibiotic misuse is in the outpatient management of upper respiratory infections (URIs). URIs are the most common infection in humans. Eighty percent of upper respiratory infections are caused by viruses.4 Antibiotics only treat bacterial infections, not viral infections. Despite this, antibiotic usage without evidence of a bacterial infection remains a critical problem. This problem has been highlighted most recently in the surge of antibiotic overuse globally during the COVID-19 pandemic.5,6
While vaccines and antiviral medications exist, wider adoption remains limited due to low access or low uptake of such interventions in certain geographies and communities, high viral mutation rates rendering treatments potentially ineffective,7,8 and weighing the efficacy and risk benefit ratio of using costly interventions for what amount to in most cases, mild and self-limited disease.9
Vitamins, minerals, and herbs to support the immune system’s clearance of infections have broadly shown mixed benefits. This has been in part due to the lack of uniform standards in preparation, formulation, potency, and actual usage.10 The dosages necessary to confer therapeutic benefit demonstrated in supportive studies are often much higher than the dosages found in standard products commonly found over the counter in pharmacies and drug stores. A key advantage of the potential use of vitamin, mineral, and herbal preparations as a tool in URI management is the reduced risk of antimicrobial resistance, reduced exposure to the potential side effects of drugs, and the long-term preservation of antibiotic and antimicrobial efficacy for when they are critically needed.
In the case of the Western herb Echinacea, the strongest data for its potential use in the treatment of URIs is likely in the form of Echinacea purpurea.11–17 In the case of the mineral zinc, the greatest potential benefit of its usage in the management of URIs may be in ionizable forms of zinc, such as zinc acetate.18–21 The utility of vitamin C supplementation in either the prevention or treatment of URIs has yielded mixed results in randomized clinical trials (RCTs), but may provide more benefit in the prevention of URIs in patients doing heavy exercise and undergoing similar short term physical stress.22–24
There has been increased interest in the potential role of vitamin D in URI management during the COVID-19 pandemic. While data is mixed,25,26 some current data shows there may be potential benefit in vitamin D supplementation in reducing the incidence of URIs.27–29 However, a study evaluating early, acute repletion of vitamin D with high enteral bolus during active COVID-19 illness in intensive care unit patients did not show benefit in reducing 90-day all-cause mortality.30
While there are a number of studies evaluating the use of individual vitamins, minerals, and herbs in the management of URIs, RCTs evaluating the potential role of combinations of herbs, vitamins, and minerals that have individually demonstrated efficacy data remain limited. The author’s interest in examining the potential use of such treatment modalities stems from the WHO’s public request and is derived from a desire to equip clinicians and patients with tools that reduce inappropriate antibiotic use during viral URI. The end goal is to reduce the potential risk of the induction and spread of antibiotic resistance.
The purpose of this specific study is to evaluate the feasibility of using EZC Pak, a 5-day dose pack of Echinacea purpurea, zinc acetate, and vitamin C to reduce the duration of illness and symptom severity in non-specific upper respiratory infection. A secondary endpoint was evaluating patient satisfaction with receipt of the intervention. Given both public and academic interest in a potential role for vitamin D in URI management, a second intervention arm adding vitamin D to the base dose pack of Echinacea purpurea, zinc, and vitamin C was carried out.
Methods
Institutional review board (IRB) approval of the study protocol was carried out by Argus IRB. A total of 360 individuals, male or female over 18 years old, were recruited, informed consent obtained in compliance with CFR 50.25 and the Declaration of Helsinki, and enrolled by Citrus Labs, a third-party clinical research organization (CRO), to participate in the study. The clinical trial data collection period was June 1, 2021 and ended February 28, 2022. The CRO utilized an algorithm to randomize the patients into three different arms with comparable demographics – placebo, EZC Pak, or EZC Pak + Vitamin D (EZC Pak+D) in a double blinded manner. The placebo was composed of rice concentrate.
A total of 165 individuals were enrolled in the placebo control arm. A total of 123 individuals were enrolled in the EZC Pak intervention arm. A total of 72 individuals were enrolled in the EZC Pak+D intervention arm (Figure 1). Enrollment was completed during the initial 90 days and the intervention component was carried out over the subsequent six months.
 |
Figure 1 CONSORT flow diagram. |
Individuals with the following medical conditions were excluded: ragweed allergy, chronic seasonal allergies, liver disease, autoimmune or connective tissue disorder (eg, rheumatoid arthritis, lupus, multiples sclerosis, HIV), alcohol consumption more than 7 drinks per week, or more than 3 drinks per occasion, routine recreational drug use, renal disease, and females that were pregnant, wanted to become pregnant for the duration of the study, or who were breastfeeding.
The study was conducted virtually with the CRO’s technology platform utilized to screen, enroll, and capture study data of the participants. Study enrollees had to actively participate in the study intervention only when they had a URI. Once participants had a URI, they took the double blinded test product as directed and completed the daily symptom survey score until their symptoms resolved.
Participants also recorded any adverse or ill effects any time after taking the test product and for any final adverse events upon completion of the exit form. Participants also recorded if they took any additional medications during the course of their URI.
Once a study participant reported the first symptoms of a URI, they were advised to take the intervention (ie, placebo, EZC Pak, or EZC Pak+D) taper dosed over a five-day period. The participant was instructed to take the intervention 4 times a day (every 6 hours) on Day 1, 3 times a day (every 8 hours) on Day 2, and 2 times a day (every 12 hours) on Day 3 through Day 5 (Figure 2).
 |
Figure 2 Visual representation of the dosing scheme over the five-day treatment period. |
Analysis
In order to evaluate the performance of the intervention, a comparative analysis on the illness of trial participants from the intervention arms EZC Pak and EZC Pak+D was performed versus the placebo control arm. There were 360 subjects enrolled in this study, well distributed across the mainland US (Figure 3). The age range across the sample was between 22 years and 88 years old. The average age for the placebo group was 57 years old, the EZC group was 55 years old, and the EZC+D group was 54 years old. Most participants were White or Caucasian. The other ethnicities represented less than 10% of the sample within each intervention arm (Table 1).
 |
Table 1 Demographic Characteristics of Participants |
 |
Figure 3 Choropleth map of geographic distribution of study participants. |
Two evaluations were carried out. The primary evaluation assessed illness on the basis of daily symptom and vital sign reporting. Secondarily, we performed an analysis on subjective patient satisfaction. In addition to separate comparisons, EZC Pak and EZC Pak+D arms were also combined to include all participants from both pools.
Given that the entire adult population of the United States, or 258.3 million adults,31 can be infected by URIs, a 90% confidence interval was used to select a 360 patient sample size for this initial feasibility study.
We evaluated the performance of each illness via two metrics: Days To Recovery (DTR) and Symptom Severity During Recovery (SSDR). Two separate, parallel analyses were carried out for each to determine the efficacy of the intervention versus the placebo.
Days to Recovery (DTR)
DTR is a metric that measures the total number of days in which a patient is experiencing symptoms of an illness while taking the intervention or placebo. DTR also directly lends itself for use in a log-rank analysis, which is used to compute statistical significance.
The primary limitation of DTR arises from the heterogeneous nature of the illness and the patient’s unique recovery. Despite aggressive daily oversight, some participants were lost in follow up, most particularly, but perhaps not surprisingly, in the placebo group. Interestingly, the 20% dropout rate in the placebo group was comparable to the proportion of patients, approximately 20%, one would expect to have a bacterial infection that may require antibiotics. In these instances of dropout, a DTR score of 14 days was imputed, equivalent to the average number of days a bacterial infection lasts if left untreated.
From the numerical results, the average EZC Pak participant recovers nearly one and a half days sooner than the average placebo participant (Table 2). From the Kernel Density Estimate (KDE) plot (Figure 4), we can similarly observe a higher density of early recoveries as compared to the placebo group, with EZC Pak group peaks coming sooner. For EZC Pak and the EZC Pak Combined cohort, we see that this is a statistically significant improvement (p< 0.1). EZC Pak+D does not achieve the same level of statistical significance in the DTR analysis driven by the small sample size.
 |
Table 2 Mean DTR Score and Improvement over Placebo with Log-Rank test |
 |
Figure 4 Kernel density estimate plot and Kaplan–Meier plot for Days To Recovery (DTR) Score. |
Symptom Severity During Recovery (SSDR)
SSDR is a metric that aims to capture information on how the symptoms of an illness progress during the recovery phase. Unlike DTR, it is intended to be disease agnostic and not influenced by the type of illness.
SSDR is motivated by the idea that the path to recovery provides useful insights into a participant’s disease response. In order to assess this, SSDR is fundamentally based on the area under an illness curve. Such illness curves are generated by measuring daily symptom magnitudes for each illness day.
Daily symptom magnitudes utilized the following questions, are you experiencing: 1) coughing? 2) hoarseness? 3) runny nose? 4) nasal congestion? 5) sneezing? 6) scratchy or sore throat? 7) headache? 8) ear pain? 9) fatigue? 10) chills? 11) shortness of breath or difficulty breathing? 12) new loss of taste or smell? 13) nausea? 14) vomiting? 15) diarrhea? 16) fever?
Subjective responses for each symptom were registered as either “None”, “Mild”, “Moderate”, or “Severe.” Each of these was mapped to a numerical score of 0, 1, 2, and 3, respectively. Additionally, along with the symptoms, the presence of a fever was included, where “No Fever”, “Between 99.9–100.4°F”, “Between 100.5–101.4°F”, “Between 101.5–103°F”, and “More than 103°F” was similarly mapped to 0, 1, 2, and 3, respectively.
The total “symptom severity” for a day was the sum of these numerical scores across all symptoms and temperature. Other vitals including respiratory rate, heart rate, blood pressure, and oxygen saturation were recorded in the study, but ultimately discarded due to the observed high unreliability of participant self-measurement and recording of these vital signs.
From these symptom scores, a sequence of daily symptom severities was generated, the sum of which is the area under the illness curve. In its raw form, the area represents the total discomfort or pain that a patient experiences during an illness. Reducing this is generally a foundational goal of an intervention.
With respect to illness heterogeneity, simply taking the raw area under the illness curve brings the same challenges as DTR, only to a larger extent. As such, a scaling approach is used where the symptom severity is scaled according to the illness peak, and the timesteps are scaled based on the length of the recovery phase. This is also equivalent to the ratio of the observed area under recovery to the area under recovery if the illness had stayed static and not improved at all from the peak.
This results in a theoretical maximum SSDR of 1 and a minimum of 0. The lower the SSDR, the better. SSDR utilizes the area under the recovery phase and not the entire illness. To determine the start of recovery, the greatest one-day decrease in symptom severity was identified and then analyzed backwards until symptom severity stopped improving. In effect, this results in SSDR being a metric that focuses on the severity of symptoms.
SSDR can still be difficult to compute under certain circumstances. For example, in instances where a participant skipped multiple days of data entry, the exact shape of the illness curve becomes unknown. To the extent possible, this was addressed using a linear estimate of nearby datapoints, but such estimates become unreliable if an excess number of data entries are missing.
As such, some basic filters were utilized to assess subject participants with usable and ultimately clinically relevant SSDRs:
- Participants with incomplete end of data entry reporting or more than 30% of their daily data entries missing
- Illnesses that were less than three days or longer than ten days
This results in a SSDR cohort (Table 3). We observe a 15–20% improvement in SSDR when comparing the mean performance of the EZC Pak groups versus placebo (Table 3). In the KDE plot, we also observe the very clear leftward shift in EZC Pak group peaks (Figure 5). Most EZC Pak participants have notably lower SSDRs than placebo participants.
 |
Table 3 Mean SSDR Score and Improvement Over Placebo with T-test |
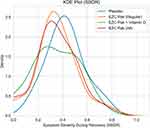 |
Figure 5 Kernel density estimate plot for Symptom Severity During Recovery (SSDR) Score. |
Patient Satisfaction Survey Analysis
At the end of illness, participants were asked the following: “Do you believe the test product sped up your recovery time?” The options they could choose were “Yes”, “Maybe”, and “No.” These responses were mapped to scores 1, 0, and −1 respectively, enabling a scale that ranges [−1, 1]. Negative scores imply a lack of confidence in the product, zero implies ambivalence, and positive scores imply satisfaction. No filters were applied or imputations made.
All EZC Pak groups had a higher mean participant satisfaction than the placebo group, with the base EZC Pak performing approximately three times better than placebo (Table 4).
 |
Table 4 Mean Satisfaction Score with T-test |
Patient Safety Data & Side Effects Analysis
In total, 25 participants reported side effects. The most significant side effect was gastrointestinal (GI) discomfort or nausea. This was reported in 6 patients total in the intervention arms, representing 6.5% of the total participants in EZC Pak Combined. This rate of GI discomfort or nausea side effect was within the normal anticipated range given the known potential side effect of high dose zinc.
Three patients in the placebo group reported loose stool or diarrhea. Rice concentrate can have an osmotic effect, especially if taken without additional food. In all but two cases, only a single side effect was reported. One placebo participant reported nausea as well as muscle aches. Another placebo participant reported headache and drowsiness (Table 5).
 |
Table 5 Participant Side Effects |
Discussion
The primary complexity of studying URIs relates to the heterogeneous nature of the illness and the unique recovery of each patient. URIs vary by pathogen, geography, and seasonality among many factors.32 Intestinal absorption, metabolism, and immune response to EZC Pak and vitamin D may be influenced by numerous factors. These include the patient’s age, sex, health status, diet and nutritional status, medications, and microbiome among others.33 Further, all people get URIs. Taken together, this leads to research conditions in which large sample sizes are required to generate a high degree of generalizability. This becomes technically challenging, as the vast majority of URIs are self-limited diseases.
While this study is demographically and geographically evenly distributed across each arm, females predominated in the study as a whole, which may reflect a self-selection bias for trials of this type. Adjustments in the study recruitment process may be made to address this in future study. Bloodwork analysis including blood counts, vitamins C, D, zinc, and related mineral and micronutrient levels can also be included in future study. Similarly, patient weight, BMI, and dietary patterns should be included in future study. Adequately educating trial participants at the study onset on the meaning of each vital sign and proper use of the vital sign recording equipment may also improve vital sign data collection towards further analysis of disease status and resolution.
The results of this trial of EZC Pak’s potential impact on outpatient URI management yield three intriguing results for further study. One, initiating use of EZC Pak as the first step in patients with non-specific URI symptoms has the potential to reduce the duration of illness. The findings support the use of EZC Pak as a viable alternative to patient request for antibiotics when none are deemed clinically necessary at the time of initial clinical presentation. The benefit of EZC Pak on illness duration is likely highest in viral URI. Whether there is a synergistic benefit to using EZC Pak in combination with an antibiotic when a bacterial URI is suspected or established can be investigated in future studies.
Secondly, there is a clinically meaningful reduction in symptom severity during URI when using EZC Pak. This lends clinical management to consider EZC Pak alone or in combination with adjuvant treatments that can potentially provide a synergistic reduction in symptom severity during URI (eg, nasal rinse, steam inhalation, or symptom specific relieving medications) and can be studied further.
While some epidemiologic data suggests patients with low serum vitamin D levels have a higher incidence of URIs,34,35 similar to the outcomes of other recent vitamin D supplementation trials,36 the addition of vitamin D during the acute phase of illness in this study neither benefited nor harmed outcomes with respect to illness duration or symptom severity. As such, the decision to replete vitamin D in the acute phase of URI remains an individualized decision left to the patient and their clinician.
The patient satisfaction score of EZC Pak compared favorably versus placebo in this double-blind study. This highlights an important potential role EZC Pak can play in maintaining or enhancing patient satisfaction in the clinical management of viral URI. This is particularly important given the predominantly self-limited nature of outpatient cases. EZC Pak may play a critical role in improving outpatient URI management and antibiotic stewardship. Future study should expand the sample size of this initial study to further evaluate these initial key findings.
Data Sharing Statement
The data that underlie the results reported in this study are available from PPC Pharmaceuticals. This data includes deidentified individual participant data. Other study documents including the study protocol, statistical analysis plan, and analytic code are available from PPC Pharmaceuticals. Restrictions apply to the availability of these data, which were used under license for this study. Data are available to researchers who provide a methodologically sound proposal to the corresponding author with the permission of PPC Pharmaceuticals. Proposals can be directed to [email protected]. To gain access, data requestors will need to sign a data access agreement. Data will be available beginning 3 months and ending 36 months following manuscript publication.
Acknowledgments
The authors acknowledge Citrus Labs for their assistance in carrying out the clinical trial.
Funding
This clinical trial was carried out by Citrus Labs with funding support from PPC Pharmaceuticals. The supply of EZC Pak, EZC Pak+D, and placebo for the trial was provided by PPC Pharmaceuticals.
Disclosure
Aditya Radhakrishnan received a stipend from PPC Pharmaceuticals for his participation in the study. Sarath Malepati is a shareholder in PPC Pharmaceuticals and reports a patent (US 63/379,410) pending to PPC Pharmaceuticals. The other authors report no conflicts of interest in this work.
References
1. O’Neill, J. Tackling drug-resistant infections globally: final report and recommendations; 2016. Available from https://apo.org.au/node/63983.
2. World Health Organization. Antimicrobial resistance. World Health Organization; 2023. Available from http://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
3. Sanchez JD. Paho/WHO: antimicrobial resistance. Pan American Health Organization / World Health Organization; 2015. Available from https://www3.paho.org/hq/index.php?option=com_content&view=article&id=11129%3Aamr-antimicrobial-resistance-intro&Itemid=41534&lang=en#gsc.tab=0.
4. Heikkinen T, Järvinen A. The common cold. Lancet. 2003;361(9351):51–59. doi:10.1016/s0140-6736(03)
5. Russell CD, Fairfield CJ, Drake TM, et al. Co-infections, secondary infections, and antimicrobial use in patients hospitalised with COVID-19 during the first pandemic wave from the ISARIC WHO CCP-UK study: a multicentre, prospective cohort study. Lancet Microb. 2021;2(8):e354–65. doi:10.1016/S2666-5247(21)00090-2
6. Langford BJ, So M, Raybardhan S, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(12):1622–1629. doi:10.1016/j.cmi.2020.07.016
7. Hu Y, Lewandowski EM, Tan H, et al. Naturally occurring mutations of SARS-COV-2 main protease confer drug resistance to Nirmatrelvir. bioRxiv. 2022;2022:6.
8. Sedova M, Jaroszewski L, Iyer M, Godzik A. Monitoring for SARS-COV-2 drug resistance mutations in broad viral populations. bioRxiv. 2022;2022:5.
9. FDA. Pfizer reports additional data on paxlovid™ supporting upcoming new drug application submission to U.S. FDA. Pfizer; 2022. Available from: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-reports-additional-data-paxlovidtm-supporting.
10. Melchart D, Linde K, Worku F, Bauer R, Wagner H. Immunomodulation with echinacea — a systematic review of controlled clinical trials. Phytomedicine. 1994;1(3):245–254. doi:10.1016/s0944-7113(11)80072-3
11. Barnes J, Anderson LA, Gibbons S, Phillipson JD. echinacea species (echinacea angustifolia (DC.) hell., echinacea pallida (Nutt.) Nutt, echinacea purpurea (L.) moench): a review of their chemistry, pharmacology and clinical properties. J Pharm Pharmacol. 2005;57(8):929–954. doi:10.1211/0022357056127
12. Barrett B. Medicinal properties of echinacea: a critical review. Phytomedicine. 2003;10(1):66–86. doi:10.1078/094471103321648692
13. Gupta M, Sharma D, Sharma A, Kumari V, Goshain OP. A review on purple cone flower (Echinacea purpurea L. Moench). J Pharm Res. 2012;5(8):4076–4081
14. Mahady GB, Qato DM, Gyllenhaal C, Chadwick L, Fong HHS. Echinacea: recommendations for its use in prophylaxis and treatment of respiratory tract infections. Nutr Clin Care. 2001;4(4):199–208. doi:10.1046/j.1523-5408.2001.00143.x
15. Melchart D, Linde K, Fischer P, Kaesmayr J. Echinacea for preventing and treating the common cold. Cochrane Database Syst Rev. 1999. doi:10.1002/14651858.cd000530
16. Shah SA, Sander S, White CM, Rinaldi M, Coleman CI. Evaluation of echinacea for the prevention and treatment of the common cold: a meta-analysis. Lancet Infect Dis. 2007;7(7):473–480. doi:10.1016/s1473-3099(07)70160-3
17. Woelkart K, Linde K, Bauer R. Echinacea for preventing and treating the common cold. Planta Med. 2008;74(6):633–637. doi:10.1055/s-2007-993766
18. Petrus EJ, Lawson KA, Bucci LR, Blum K. Randomized, double-masked, placebo-controlled clinical study of the effectiveness of zinc acetate lozenges on common cold symptoms in allergy-tested subjects. Curr Ther Res. 1998;59(9):595–607. doi:10.1016/s0011-393x(98)85058-3
19. Prasad AS, Beck FWJ, Bao B, Snell D, Fitzgerald JT. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis. 2008;197(6):795–802. doi:10.1086/528803
20. Eby J. Zinc ion availability-The determinant of efficacy in zinc lozenge treatment of common colds. J Antimicrob Chemother. 1997;40(4):483–493. doi:10.1093/oxfordjournals.jac.a020864
21. Hemilä H, Petrus EJ, Fitzgerald JT, Prasad A. Zinc acetate lozenges for treating the common cold: an individual patient data meta-analysis. Br J Clin Pharmacol. 2016;82(5):1393–1398. doi:10.1111/bcp.13057
22. Hemilä H. Vitamin C and common cold incidence: a review of studies with subjects under heavy physical stress. Int J Sports Med. 1996;17(05):379–383. doi:10.1055/s-2007-972864
23. Hemilä H. Vitamin C supplementation and the common cold-was Linus Pauling right or wrong? Int J Vitam Nutr Res. 1997;67:329–335.
24. Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013;2013(1):CD000980. doi:10.1002/14651858.CD000980.pub4
25. Murdoch DR, Slow S, Chambers ST, et al. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults. JAMA. 2012;308(13):1333. doi:10.1001/jama.2012.12505
26. Jolliffe DA, Holt H, Greenig M, et al. Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: Phase 3 randomised controlled trial (CORONAVIT). BMJ. 2022;e071230. doi:10.1136/bmj-2022-071230
27. Laaksi I, Ruohola JP, Mattila V, Auvinen A, Ylikomi T, Pihlajamäki H. Vitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double‐blinded trial among Young Finnish men. J Infect Dis. 2010;202(5):809–814. doi:10.1086/654881
28. Charan J, Goyal JP, Saxena D, Yadav P. Vitamin D for prevention of respiratory tract infections: a systematic review and meta-analysis. J Pharmacol Pharmacother. 2012;3(4):300–303. doi:10.4103/0976-500x.103685
29. Jolliffe DA, Camargo CA, Sluyter JD, et al. Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet Diabetes Endocrinol. 2021;9(5):276–292. doi:10.1016/s2213-8587(21)
30. National Heart, Lung, and Blood Institute PETAL Clinical Trials Network. Early high-dose vitamin D3 for critically ill, vitamin D–deficient patients. N Engl J Med. 2019;381(26):2529–2540. doi:10.1056/nejmoa1911124
31. Ogunwole SU. Population under age 18 declined last decade. Census.gov; 2022. Available from: https://www.census.gov/library/stories/2021/08/united-states-adult-population-grew-faster-than-nations-total-population-from-2010-to-2020.html.
32. Avendaño Carvajal L, Perret Pérez C. Epidemiology of respiratory infections. In: Bertrand P, Sánchez I editors. Pediatric Respiratory Diseases. Cham: Springer; 2020. doi:10.1007/978-3-030-26961-6_28
33. Mossink JP. Zinc as nutritional intervention and prevention measure for COVID–19 disease. BMJ Nutr Prev Health. 2020;3:111–117. doi:10.1136/bmjnph-2020-000095
34. Ginde AA, Mansbach JM, Camargo CA
35. Katz J, Yue S, Xue W. Increased risk for COVID-19 in patients with vitamin D deficiency. Nutrition. 2021;84:111106. doi:10.1016/j.nut.2020.111106
36. Martineau AR, Cantorna MT. Vitamin D for COVID-19: where are we now? Nat Rev Immunol. 2022;22:529–530. doi:10.1038/s41577-022-00765-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
